Abstract
The postural imbalance is an extra-pulmonary condition, associated with chronic obstructive pulmonary disease (COPD). COPD affects older individuals and it is unclear whether balance abnormalities can be described as pathophysiological mechanism or aging. The present study aimed to evaluate the influence of age or disease on postural balance of patients with COPD. Patients with COPD over 50 years old were compared with age- and sex-matched healthy adults, and with sex-matched younger healthy adults (n = 30 in each group). The Modified Sensory Organization Test (mSOT) was performed in four different conditions fixed or sway-referenced surface both either with full or no vision. It was analyzed the center of pressure (CoP) variables: amplitude, velocity, root-mean-square and load asymmetry. Three-way ANOVA and post hoc analysis were performed been represented of age (older or COPD compared with younger healthy adults) or disease influences (COPD compared with older healthy groups). Main results were as follows: The CoP excursion was faster, with higher amplitude and variability progressively from COPD vs. older healthy vs. younger healthy adults (p < 0.05) showing age and disease influences (p < 0.05). Age and disease influences were also observed in the sway-referenced surface in both vision conditions. Impairment in postural balance was found related to aging and disease in patients with COPD older than 50 years.
Introduction
Chronic obstructive pulmonary disease (COPD) is a common, preventable, and treatable disease characterized by persistent respiratory symptoms and airflow limitation associated with airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases [Citation1]. The extra-pulmonary consequences of COPD are also well described and include systemic inflammation, weight loss, musculoskeletal dysfunction and increased risks of osteoporosis, depression and cardiovascular disease [Citation2–4]. In addition, recent evidence suggests patients with COPD present deficits in postural balance that increases the risk of falls [Citation5].
Porto et al. [Citation6] reviewed all clinical and experimental tests evaluating postural balance abnormalities in patients with COPD and concluded the impairment of postural control is more frequent in patients with COPD than in healthy age-matched subjects. This impairment is associated with reduced functional capacity and independence during daily tasks that could explain the increased risk of fall. The authors suggested that posturography is the most appropriate tool to evaluate postural control on patients with COPD, probably because it is recognized as the gold standard for the assessment of postural control [Citation7]. The Modified Sensory Organization Test (mSOT) is a posturography test proposed to identify sensorimotor components in the static posture. The components include the evaluation of afferents and efferents pathways as well as the central integration involved in postural stability, that is, the capacity to maintain the center of gravity in the base of support. Consequently, the mSOT allows the discrimination of different sensory systems involved in the postural stability including visual, vestibular, and somatosensory systems. There is an apparently random pattern to determine the stability in the anteroposterior and mediolateral directions not mostly detectable in the clinical examination. However, the center of pressure (CoP) can evaluate such stability using the mSOT in each sensory condition test [Citation8].
Aging is associated with changes in sensory systems because it reduces the appropriate feedback and integration to maintain an adequate balance [Citation9–11]. Patients with COPD present systemic manifestations that become more prominent along with the patient’s life and aging may have even a higher influence in postural control in patients with COPD. However, evidence of the influence of age and sensory components in the postural balance in patients with COPD is still limited [Citation6, Citation12] and it has not been evaluated with computerized dynamic posturography. The mSOT is highly recommended in older adults especially due to the sensory components that may be impaired by aging as proprioception and cutaneous sensation in the lower extremities [Citation10].
The hypothesis to be tested in our study is that aging as well as disease have an influence on postural balance in individuals with COPD. The present study aimed to investigate the influence of age and disease in the postural balance of patients with COPD. This study also aimed to evaluate the influence of sensory components of postural control in patients with COPD taking into consideration the potential influence of aging. These findings are important for the development of new therapeutic approaches concerning the ability of patients to prevent the risk of falls during daily and physical activities.
Methods
Participants
The study included three groups of volunteers: (1) COPD group, (2) older healthy group, and (3) younger healthy group; with 30 participants in each group. Patients with COPD were diagnosed according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria [Citation1]. Consecutive patients with COPD clinical stable (insufficient exacerbation or changes in medication for at least 4 weeks) were invited during a regular medical consultation. Criteria inclusion were: be under optimal medical treatment for, at least, 6 months, range from 50 to 85 years of age and post-bronchodilator forced expiratory volume in one second (FEV1) <80% of predicted and FEV1 to forced vital capacity (FVC) ratio (FEV1/FVC ratio) <0.7. Participants in the older and younger healthy groups were recruited, respectively, among hospital employees and students of the university. Subjects were recruited by an advertisement placed through the hospital internal information board or mail. Inclusion criteria for all participants from the older and younger groups were self-reported being independent for gait and upright bipedal posture and for older healthy group been age and sex-matched and for younger healthy group been sex-matched and aging between 20 and 40 years old. Exclusion criteria for all three groups were: (a) other cardiopulmonary, musculoskeletal or neurological diseases; (b) untreated visual, vestibular and somatosensory diseases; (c) previous engagement in any exercise training routines in the last 2 years; and, (d) current smokers (to avoid the deleterious signs of nicotine on postural balance) [Citation13]. The Hospital Ethics Committee approved the study, and all patients provided written informed consent after being informed about the study in accordance with the Declaration of Helsinki.
Clinical data
Age (years), sex (male and female) and comorbidities were evaluated in all participants.
Pulmonary function, respiratory muscle strength, and functional status were evaluated only in patients with COPD. Pulmonary function was evaluated by forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1) values, and FEV1/FVC ratio [Citation14]. All values were expressed as a percent of the predicted value for the Brazilian population [Citation15]. The maximal respiratory pressures (MIP and MEP) was evaluated by manovacuometry and values were analyzed as predicted percentage [Citation16,Citation17]. Functional status was assessed by Body Composition, Obstruction, Dyspnea and Exercise Capacity (BODE) index [Citation18].
Modified Sensory Organization Test (mSOT)
The mSOT assessment consisted of maintaining quiet balance while standing over an upright bipedal support for one minute. Their feet were positioned in parallel stance, with a symmetrical distance between the medial malleolus, from a middle point of reference in the platform. Participants were asked to keep their arms relaxed and parallel to their trunk. In the full vision condition, participants were instructed to stare at a black screen on the top of a pole positioned 80 cm away from their eye level. For the no vision condition, participants were asked to close their eyes and instructed to keep their head in the same position and to maintain the attitude they adopted in the full vision condition. Both full vision and no vision conditions were performed with participants standing on a force platform which could be fixed or on sway-referenced surface (Pro Balance Master System, NeuroCom PRO 8.4.0, Oregon, USA).
The posturography performance was evaluated through the “Modified Sensory Organization Test” (mSOT) that assesses balance stability on postural sway in a Cartesian plane under four sensorial conditions: fixed surface with full vision or no vision (two conditions), and sway-referenced surface with full vision and no vision (two conditions). The sway-referenced surface condition was in a tilt direction “up and down” movement using the servo-driving of the equipment on the frontal axis as previously described [Citation19]. During the sway-referenced surface, the surface input is reduced, and a sensory conflict is induced leading to the re-weighting of the sensory systems to maintain postural control [Citation19]. The sampling frequency of the collected data was 100 Hz obtained in three 20-second trials.
Kinetic measures
Stance stability data was collected from the CoP excursion, measured as linear dislocation of CoP amplitude (AMP; cm), root-mean-square (RMS; cm), and mean velocity (MV; cm/s). All these variables were considered in both anteroposterior (AP) and mediolateral (ML) directions. Load asymmetry (Asy) was measured. It is defined as the normalized difference between anterior and posterior vertical ground reaction force according to the location of the cell force load of the platform to quantify the weight transferred by the feet in the anteroposterior direction [Citation20].
The data extraction and processing were made using Matlab (Mathworks®, 2015) routine following visual data inspection for anomalous or spurious values. CoP data were low-pass filtered through a fourth-order Butterworth filter with a cutoff frequency of 100 Hz. Trials for each condition were individually averaged for statistical analysis.
Analysis
Assumptions of parametric statistics were verified through the Shapiro-Wilk test. Statistical analysis was performed by means of a three-way ANOVA, considering 3 groups (COPD, older, and younger) × 2 surfaces (fixed and sway) × 2 conditions (full and no vision) followed by the post hoc comparisons through Newman-Keuls procedures. The level of significance was set at 5%. The age and disease influences were considered significant evaluating the kinetic variables (AMP, RMS, MV, Asy) between groups in the surface (fixed, sway) and vision (full vision, no vision) conditions. The analysis was performed to detect differences between vision (full and no vision), surface (fixed and sway) and groups (COPD, older and younger). The post hoc analysis indicated the age influence considering differences between either older healthy or patients with COPD compared with younger healthy adults, but without difference between the COPD and Older health adults. Disease influence was considered a difference between COPD and older healthy groups.
Results
Ninety-nine patients with COPD were eligible for this study, 37 did not meet inclusion criteria, 15 declined to participate, and 17 were not available, resulting in 30 individuals in the COPD group. Thirty older healthy adults and 30 younger healthy adults comprised healthy groups. depicts the demographic characteristics and comorbidities for all groups and pulmonary function and functional capacity for the COPD group. No significant differences between the groups were observed in the demographic variables (p > 0.05).
Table 1. Demographical and clinical characteristics of the three studied groups: patients with COPD, older healthy adults, and younger healthy adults.
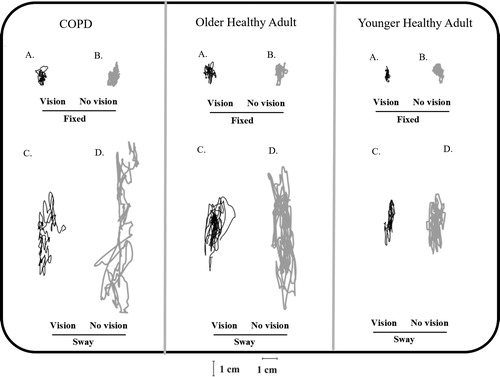
The raw data of the CoP excursion of each group is presented in , in different vision and surface conditions. The kinetics variables from the CoP data were calculated. In this Figure, it is possible to observe that the groups are apparently different considering CoP excursion in general with higher CoP sway in sway surface (conditions C and D) comparatively to fixed surface (conditions A and B) in COPD group. It is possible to observe that the variation of the pattern of the CoP excursion it is progressively increasing from younger healthy group to older adult healthy group to COPD group in AP direction (vertical axis), especially in sway-referenced surface conditions with no vision.
Figure 1. Statokinesiogram for representative individual of each group in the vision and surface condition (COPD, older healthy adults and younger healthy adults); (A) fixed surface/full vision, (B) fixed surface/no vision, (C) sway-referenced surface/full vision, and (D) sway-referenced surface/no vision. The black line represents the full vision and the gray line no vision condition.
presents the significance of the main differences found in the post hoc analysis (AMP, RMS, MV, and Asy). Vision has presented differences in all seven variables, that is, and the surface has presented differences in six of them. Post hoc analysis identifies differences between groups considering factors all together otherwise the condition. Age and disease influence were verified in the post hoc through the interaction between group-vision, group-surface and group-surface-vision indicating in which group vision condition (vision or no vision) or surface condition (sway or fixed) was observed.
Table 2. Evaluation of the main effects and interactions for the center of pressure value among groups (COPD, older healthy adults and younger healthy adults) in different vision (vision and no vision) and surface conditions (fixed, sway-referenced).
General analysis of kinetic variables in mSOT
Mean and standard deviation of the AMP, RMS, and MV in both AP and ML directions in sensory conditions of the mSOT are presented in . Conditions assessed by mSOT were fixed surface with full vision; fixed surface with no vision; sway-referenced surface with full vision, and sway-referenced surface with no vision. The analysis presented that patients with COPD are different from older healthy adults and younger healthy adults in conditions of sway-referenced surface both with vision and no vision. It is described below those differences considering the age and disease influence.
Figure 2. Mean values (standard errors in vertical bars) of amplitude (AMP), root-mean-square (RMS) and mean velocity (MV) of CoP in both directions (anteroposterior, AP; mediolateral, ML), in conditions with support surface (fixed/sway-referenced) and vision (vision/no vision) variations, for all groups (COPD, older healthy adults and younger healthy adults). & age influence; ¶ disease influence.
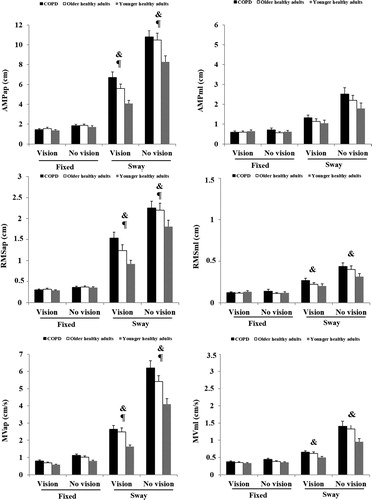
Age influence
Age influence in the postural balance differentiated groups and the significant variables exhibited higher values for COPD (RMSap, RMSml, MVml) and older healthy group (AMPap, MVap) than the younger healthy group. Differences were found in group-surface conditions for sway-referenced surface for AMPap, and for RMS and MV for both AP and ML directions (p values ranging from 0.03 to 0.0001). Age influence also showed differences between groups in vision conditions where differences were found for MVap in full vision and no vision, and MVml no vision (p values ranging from 0.01 to 0.0001). Mean values and significant differences of the variables can be observed in for each condition in each group.
Disease influence
The disease influence in the postural balance showed differences between groups exhibiting higher values for COPD group than the older healthy group. Regarding groups and surface conditions, differences were found only for sway-referenced surface in AMPap (p = 0.04) and MVap (p < 0.0001). Regarding differences between groups and vision conditions was found only for no vision in MVap (p = 0.02). Mean values and significant differences of the variables can be observed in for each condition in each group.
The Asy values found differences between groups showing that the COPD group has a more anterior position of the CoP in the base of support. Differences were consistently for analysis for each group in both vision and surface conditions and are presented in (significant differences considering the age and disease influence is also presented in and is presented below in this section). shows the ground reaction force tends to be found progressively in an anterior location in the young healthy group, followed by older healthy adults and COPD group.
Figure 3. (A) Mean values (standard errors in vertical bars) of asymmetry (Asy) of CoP for groups (COPD, older healthy adults and younger healthy adults). (B) Schematic representation of CoP location for groups regarding the medial malleolus. The square is a schematic representation of the average of CoP location of each group. & age influence; ¶ disease influence.
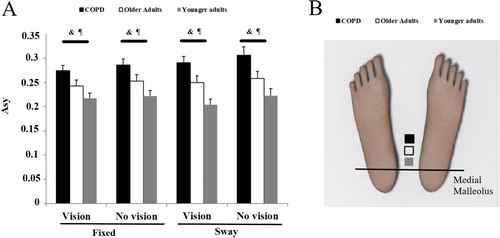
Age and disease influence
The variable Asy showed both age and disease influence, both with higher values for age influence for COPD comparatively to younger (p = 0.0001) and older to younger (p = 0.03); and for disease influence for COPD group to older (p = 0.02) ().
Discussion
Changes in postural balance in patients with COPD have been reported [Citation5, Citation21,Citation22] due to conditions like disease severity, reduced physical activity, reduced muscle strength [Citation5, Citation23], increased levels of anxiety and depression, greater clinical disease influence on lifestyle, and inflammatory markers [Citation22].
The hypothesis of our study was tested using the mSOT for postural balance considering kinetic variables AMP, RMS, and MV in both anteroposterior and mediolateral direction, and Asy only in the anteroposterior direction. Our results showed that patients with COPD presented postural balance compromised due to both age and disease influence.
General analysis of kinetic variables in mSOT
Groups were analyzed taking all mSOT conditions and differences were found for all variables in AP direction and only for MV in ML direction. CoP excursion was faster (MV), with higher amplitude (AMP) and variability (RMS) progressively from patients with COPD, older healthy adults and younger healthy adults.
Age influence
The mSOT allows us to increase the demand to postural control by manipulating sensory components. Sensory impairments in postural control occur in a natural aging process involving functions associated with changes in visual, vestibular and somatosensory systems [Citation9–11]. Sensory manipulation usually discriminates fallers and non-fallers in older adults and the augmented reliance in somatosensory information in fallers is considered a biomarker to these risk conditions [Citation9].
Age influence compromising postural balance in patients with COPD was shown with higher values for patients with COPD than younger, and older than the younger group. Higher amplitude, variability, and velocity in the excursion of CoP represent greater physical demand to maintain postural balance, and it is especially expected during the aging process [Citation24]. Age influence was revealed in all variables in the anteroposterior direction. RMS in the anteroposterior direction is especially relevant for patients with COPD as it is a biomarker for potential risk of fall [Citation25,Citation26]. The postural assessment in our study raises a concern to the fall risk in patients with COPD due to postural instability. The velocity of CoP in mediolateral direction was revealed as an indicator of age influence in postural balance in the COPD group. It seems that even though older adults present more frequent postural adjustments that do not help reduce the excursion of CoP [Citation24].
Disease influence
Our study discriminates the disease influence in the postural balance of patients with COPD differentiating them from older healthy group. Higher values to the COPD group were observed in the excursion and velocity of CoP in the anteroposterior direction only in the sway-referenced surface and without vision. Janssens et al. [Citation27] reported patients with COPD present a “rigidity” in the postural control strategy in the anteroposterior direction in sway-referenced surface with no vision. According to these authors, this is due to a great reliance on ankle proprioceptive information and to the reduction of the mobility in the trunk that leads to postural instability. In other words, the individual keeps the body rigid following the tilt of the surface without a balance reaction in the counteraction of the sway-referenced surface. The excursion and velocity of CoP in the AP direction observed occurs with the aging influence and was more robust with the disease influence in patients with COPD. This probably is caused due to the clinical, physical and functional components that are worsened in patients with COPD during the aging process.
Age and disease influence
In our study, CoP load (Asy) was showed progressively forward (anterior position) from the younger group, followed by older and patients with COPD, indicating age and disease influence in patients with COPD. According to Engel and Vemulpad [Citation28] this condition of CoP in a forward position in patients with COPD concerns to static forces caused by mass distribution of the body, especially related to chest wall geometry in anteroposterior direction secondary to pulmonary hyperinflation [Citation28]. Hyperinflation can increase thoracolumbar spine hypo-mobility [Citation23] and lead to functional inspiratory muscle weakness [Citation23], reinforcing the possibility that patients with COPD have interdependent low pulmonary and postural control function. Taken together, our results strongly suggest patients with COPD are less able to maintain adequate stability under challenging conditions.
The influence of posture in the respiratory function has been previously described [Citation29]. Considering differences in the static relaxed posture, as posture influences the motor output at rest of the diaphragm. Also, posture influences the synergism between the diaphragm and abdominal muscles, and this can potentially alter airway patency. It is described a series of compensatory mechanisms as increases in firing of upper airway muscles is initiated as a function between this parallel of posture and the respiratory system. In particular, vestibular system participates in adjusting the activity of both upper airway muscles and respiratory pump muscles during movement and changes in body position, which can corroborate our results of the influence of sensory system in the postural control of patients with COPD. The vestibular sensorimotor component, named the vestibulorespiratory responses, do not appear mediated through the brainstem respiratory groups as reflexes of the medulla; otherwise, they may be relayed through neurons in the medial medullary reticular formation, influencing the activity of both abdominal and diaphragm motoneurons. Cerebellum also seems involved in this sensorimotor control as the regions that receive vestibular inputs also influence respiratory muscle activity. The sensorimotor components for posture and respiratory system are correlated in studies of sensorimotor components of postural control in patients with COPD, as the actual study, and this allows some discussion of the role of the sensory system affecting or compensating the disease, as an important functional component. The functional neurophysiological mechanism is important to provide adjustments in ventilation, such that the oxygenation-demand during movement and exercise [Citation29]. The present study corroborates the sensorimotor understanding showing the influence of specific sensorimotor conditions in postural balance in patients with COPD.
Limitations
Some limitations of the current study should be considered. First, the external generalization of our results is limited by the fact that the surface used for posturography allows movements only in the anteroposterior direction. This characteristic could reduce the equipment’s sensitivity to detect CoP displacement in other directions. Second, the pulmonary function was not assessed in the healthy groups (younger and older); however, all of them had no signs of respiratory diseases in their clinicians’ regular exams and no complaints of respiratory function on that and did not report any respiratory symptoms either at rest or during exercise.
Final considerations
Despite these limitations, our study suggests that postural balance-enhancing treatments can be beneficial for these patients. Recent studies demonstrated improvement in clinical balance measures after balance-specific training associated with pulmonary rehabilitation in patients with COPD [Citation22, Citation30]. Schaffer and Harrison [Citation10] discuss the importance of providing older adults with some compensatory strategies that increase sensory information during function such cutaneous and proprioceptive feedback and visual demonstrative input to enhance balance when impaired due to aging. Sensory feedback is usually part of balance-specific treatments [Citation22]. The treatments should focus on muscular strength training in sway-referenced surfaces in different visual conditions (vision and no vision), to reestablish stability and orientation for postural control. Also, it must be considered that beyond challenging postural control in patients with COPD, it is needed to improve capacities and sensorimotor strategies, so treatment approaches should be designed as progressive but, simultaneously, safe regarding postural stability, physical demand and respiratory function. It has been shown in the literature that specific sensory strategies to enhance vestibular and visual input, as well as the central integration of them, can minimize the deficit of surface information on the postural balance [Citation31]. So far, this approach was not tested in patients with COPD.
Conclusion
In conclusion, the mediolateral imbalance in patients with COPD is related to an age influence, and the anteroposterior imbalance observed in these patients is related to both age and disease influence. These results strongly suggest that impaired postural control is presented in patients with COPD and is more relevant when compared to healthy individuals older than 50 years of age.
Declaration of interest
The authors do not have any conflicts of interest to report
References
- Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2018 Report). Global Initiative for Chronic Obstructive Lung Disease; 2018.
- Agusti A, Soriano JB. COPD as a systemic disease. COPD. 2008;5(2):133–138. doi:10.1080/15412550801941349.
- Dourado VZ, Tanni SE, Vale SA, et al. Systemic manifestations in chronic obstructive pulmonary disease. J Bras Pneumol. 2006;32(2):161–171. doi:10.1590/S1806-37132006000200012.
- Eisner MD, Blanc PD, Yelin EH, et al. COPD as a systemic disease: impact on physical functional limitations. Am J Med. 2008;121(9):789–796. doi:10.1016/j.amjmed.2008.04.030.
- Butcher SJ, Meshke JM, Sheppard MS. Reductions in functional balance, coordination, and mobility measures among patients with stable chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 2004;24:274–280. doi:10.1097/00008483-200407000-00013.
- Porto EF, Castro AA, Schmidt VG, et al. Postural control in chronic obstructive pulmonary disease: a systematic review. Int J Chron Obstruct Pulmon Dis. 2015;10:1233–1239.
- Ruhe A, Fejer R, Walker B. The test-retest reliability of center of pressure measures in bipedal static task conditions–a systematic review of the literature, Gait Posture 2010;32:436–445. doi:10.1016/j.gaitpost.2010.09.012.
- Kristjansson E, Treleaven J. Sensorimotor function and dizziness in neck pain: implications for assessment and management. J Orthopaedic Sports Phys Therapy. 2009;39(5):364–377. doi:10.2519/jospt.2009.2834.
- Ishiyama G. Imbalance and vertigo: the aging human vestibular periphery. Semin Neurol. 2009; 29(5):491–499. doi:10.1055/s-0029-1241039.
- Shaffer SW, Harrison AL. Aging of the somatosensory system: a translational perspective. Phys Ther. 2007;87(2):193–207. doi:10.2522/ptj.20060083.
- Sturnieks DL, St George R, Lord SR. Balance disorders in the elderly. Neurophysiol Clin. 2008;38(6):467–478. doi:10.1016/j.neucli.2008.09.001.
- Oliveira CC, Lee A, Granger CL, et al. Postural control and fear of falling assessment in people with chronic obstructive pulmonary disease: a systematic review of instruments, international classification of functioning, disability, and health linkage, and measurement properties. Arch Phys Med Rehabil. 2013;94(9):1784–1799 e1787. doi:10.1016/j.apmr.2013.04.012.
- Tewari A, Hasan M, Sahai A, et al. Nicotine-mediated microcystic edema in the white matter of cerebellum: possible relationship to postural imbalance. Ann Neurosci. 2011;18(1):14–16.
- Wanger J, Clausen JL, Coates A, et al. Standardisation of the measurement of lung volumes. Eur Respir J. 2005;26(3):511–522. doi:10.1183/09031936.05.00035005.
- Pereira CA, Sato T, Rodrigues SC. New reference values for forced spirometry in white adults in Brazil. J Bras Pneumol. 2007;33(4):397–406. doi:10.1590/s1806-37132007000400008.
- American Thoracic Society/European Respiratory Society. ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166(4):518–624.
- Neder JA, Andreoni S, Lerario MC, et al. Reference values for lung function tests. II. Maximal respiratory pressures and voluntary ventilation. Braz J Med Biol Res. 1999;32(6):719–727. doi:10.1590/S0100-879X1999000600007.
- Puhan MA, Garcia-Aymerich J, Frey M, et al. Expansion of the prognostic assessment of patients with chronic obstructive pulmonary disease: the updated BODE index and the ADO index. Lancet. 2009; 374(9691):704–711. doi:10.1016/S0140-6736(09)61301-5.
- Boffino CC, de Sa CS, Gorenstein C, et al. Fear of heights: cognitive performance and postural control. Eur Arch Psychiatry Clin Neurosci. 2009;259(2):114–119. doi:10.1007/s00406-008-0843-6.
- Prado JM, Dinato MC, Duarte M. Age-related difference on weight transfer during unconstrained standing. Gait Posture. 2011;33(1):93–97. doi:10.1016/j.gaitpost.2010.10.003.
- Crisan AF, Oancea C, Timar B, et al. Balance impairment in patients with COPD. PLoS One. 2015;10(3):e0120573. doi:10.1371/journal.pone.0120573.
- Beauchamp MK, Janaudis-Ferreira T, Parreira V, et al. A randomized controlled trial of balance training during pulmonary rehabilitation for individuals with COPD. Chest. 2013;144(6):1803–1810. doi:10.1378/chest.13-1093.
- Kuznetsov NA, Riley MA. Effects of breathing on multijoint control of center of mass position during upright stance. J Mot Behav. 2012;44(4):241–253. doi:10.1080/00222895.2012.688894.
- Baltich J, von Tscharner V, Nigg BM. Degradation of postural control with aging. Proc Inst Mech Eng H. 2015;229(9):638–644. doi:10.1177/0954411915596013.
- Piirtola M, Era P. Force surface measurements as predictors of falls among older people - a review. Gerontology. 2006;52(1):1–16. doi:10.1159/000089820.
- Tisserand R, Robert T, Chabaud P, et al. Comparison between investigations of induced stepping postural responses and voluntary steps to better detect community-dwelling elderly fallers. Neurophysiol Clin. 2015;45(4-5):269–284. doi:10.1016/j.neucli.2015.07.003.
- Janssens L, Brumagne S, McConnell AK, et al. Proprioceptive changes impair balance control in individuals with chronic obstructive pulmonary disease. PLoS One. 2013;8(3):e57949. doi:10.1371/journal.pone.0057949.
- Engel R, Vemulpad S. The role of spinal manipulation, soft-tissue therapy, and exercise in chronic obstructive pulmonary disease: a review of the literature and proposal of an anatomical explanation. J Altern Complement Med. 2011; 17(9):797–801. doi:10.1089/acm.2010.0517.
- Yates BJ, Billig I, Cotter LA, et al. Role of the vestibular system in regulating respiratory muscle activity during movement. Clin Exp Pharmacol Physiol. 2002;29:112–117
- Mkacher W, Mekki M, Tabka Z, et al. Effect of 6 months of balance training during pulmonary rehabilitation in patients with COPD. J Cardiopulm Rehabil Prev. 2015;35(3):207–213. doi:10.1097/HCR.0000000000000109.
- Whitney SL, Jacob RG, Sparto PJ, et al. Acrophobia and pathological height vertigo: indications for vestibular physical therapy? Phys Ther. 2005;85(5):443–458. doi:10.1093/ptj/85.5.443.
