Abstract
Chronic obstructive pulmonary disease (COPD) is frequently associated with a reduced functional exercise capacity. This parameter is usually evaluated using 6-minute walking test (6MWT). New tools appear regularly. The aim of this study was to validate the 3-minute step test (3MStepT) and to compare 3MStepT and 6MWT in stable patients with COPD as a tool to quantify the functional exercise capacity.
Patients with COPD admitted for a pulmonary rehabilitation program in a dedicated center were recruited and randomly performed both tests: 6MWT and 3MStepT. A training test was performed systematically before each test. Walking distance and number of repetitions (3MStepT) were measured. Cardiorespiratory parameters, dyspnea and lower limb fatigue (Borg) were recorded pre and post the tests.
Fifty patients with COPD (FEV1: 45.2 ± 18.3) were included. 6MWT (423.6 ± 96.3 m) was strongly correlated with 3MStepT (62.1 ± 18.0; r = 0.780; p < 0.001). Heart rate and SpO2 were significantly different at the end of the 6MWT and 3MStepT (respectively, 106.2 ± 16.3 vs. 112.9 ± 13.4bpm, p = 0.002; 87.6 ± 5.4 vs. 89.6 ± 5.3bpm, p = 0.001). Lower limb fatigue was significantly higher after the 3MStepT (2.5 ± 2.6 vs. 3.4 ± 2.4, p = 0.01).
The 3MStepT is an alternative to the 6MWT to estimate functional exercise capacity in stable patients with COPD but cardiorespiratory adaptation and lower limb fatigue are not similar between these tests.
Background
Patients with chronic obstructive pulmonary disease (COPD) are often characterized by a reduction of exercise capacity and peripheral muscles weakness that lead to a reduced quality of life [Citation1–6]. Pulmonary rehabilitation is recommended for these patients to improve exercise capacity, muscle strength and physical activity level [Citation7–9]. Pulmonary rehabilitation programs (PRPs) are individualized and required an evaluation [Citation9]. The 6-minute walk test (6MWT) is one of the field tests recommended to measure exercise capacity [Citation10]. It is valid, reliable, responsive to the effects of treatment such as pulmonary rehabilitation and strongly associated with the risk of hospitalization and mortality [Citation10]. However, 6MWT requires a familiarization test, long time and a 30-m corridor. A national survey about the realization of the 6MWT [Citation11] showed limitations related to the 6MWT. According to the results of this survey, it appears that the recommendations of the ATS/ERS task force are not always followed: on many occasions, the corridor is not empty and in most cases, only one 6MWT was performed, suggesting that the learning effect is not taken into account. The time required for the 6MWT was the major problem for the good realization of the 6MWT. Then it seems important to find others submaximal field tests that are less time-consuming. Gloeckl et al. [Citation12] report the same comments in their study comparing 2-minute walk test (2MWT) and 6MWT.
Many other field tests have been proposed (1-minute sit-to-stand test (STST1) [Citation13, Citation14], 6-minute stepper test [Citation15–17], 6-minute step test [Citation18–20], 2MWT [Citation21]) and showed their ability to measure exercise capacity in patients with COPD. Many of these tests are shorter as STST1 or 2MWT. However, 2MWT requires also a 30-m corridor and Gloeckl et al. [Citation12] showed the ability of 2MWT to detect exercise-induced oxygen desaturation only in patients with severe COPD, which were normoxemic at rest. STST1 requires less space but it is not able to detect exercise-induced oxygen desaturation [Citation13–14]. Dal Corso et al. [Citation22] studied the 6-minute step test and suggested that a 2–3-min test would also provide a reasonable estimate of exercise capacity.
Three-minute step test (3MStepT) is another field test consisting to step up and down on a platform during 3 min. Then it is easy to perform and not expensive. The 3MStepT is valuable to measure exercise tolerance in children with pulmonary disease [Citation23, Citation24], but it has never been validated to evaluate functional exercise capacity, exercise-related oxygen desaturation and heart rate response, in patients with COPD.
The aim of this study was to validate the 3MStepT as a tool to evaluate functional exercise capacity, oxygen desaturation and heart rate response in comparison with 6MWT in patients with COPD.
Methods
Population
All patients admitted in the pulmonary rehabilitation unit of Morlaix Hospital Centre with a diagnosed COPD [Citation25] in order to perform a PRP were potentially eligible. Patients were recruited during summer 2017 (July and August). Patients with clinically instable status, with recent acute exacerbation, with musculoskeletal or joint disorders or contra-indications to perform the tests were not included.
The ethical approval of the study was obtained by the local ethics committee (BE403201317621) and registered on Clinical Trial database (NCT02873780). All patients signed a written inform consent, following the declaration of Helsinki.
Study design
Each patient performed both tests in the same day (crossover design) with the same examiner. An interval of at least 30-min rest between each test was respected. Randomization of the sequences (3MStepT–6MWT or 6MWT–3MStepT) was performed by a computer-generated random number list (www.randomizer.org) and the assessor performing the analysis was blinded regarding the sequence. The routine evaluations currently used before a PRP were also performed (Spirometry, Saint-George respiratory Questionnaire, Hospital Anxiety depressive Scale, Maximal inspiratory pressure…).
The 6-minute walk test (6MWT)
The 6MWT was performed on a 60-m flat corridor. The instructions given to the patient were the ones stemming from ATS/ERS recommendations [Citation26]. As recommended, a familiarization test was performed [Citation26]. The following parameters were recorded: pulsed oxygen saturation (SpO2) and heart rate throughout the test (SpO2 and heart rate were monitored with a pulse-oxymeter (WristOx2 3150 NONIN- BlueNight® Trainer, sleepinnov technology), delta heart rate (heart rate at the end of the test––heart rate at the beginning of the test), delta oxygen saturation (oxygen saturation at the end of the test––oxygen saturation at the beginning of the test), dyspnea (Borg scale) before and at the end of the test, leg discomfort (Borg scale) before and at the end of the test, and the walked distance and the percentage of the predictive value [Citation27].
The 3-minute step test (3MStepT)
The 3MStepT was performed on a 15-cm height platform, which was 67 cm in length and 32 cm in width. The test started from a standing position; the patients had to step up and down a one-step platform (as many times as possible) during 3 min and must straight the legs every step up and down. The platform was placed at 40 cm from a wall, so that the subjects could put a hand on the wall in case of imbalance. Patient was getting up in front of the platform, the 2 feet on the floor. If necessary, patients were authorized to put their hand on the wall in case of imbalance.
We used an adaptation of the instructions from the 6MWT given by the ATS/ERS [Citation26] (standardized encouragement after 1 min, 1 min and a half, and 2 min). A demonstration of the movement was made by a physiotherapist to explain the test. As recommended for the 6MWT [Citation26], a familiarization test was performed in order to limit the variability of the measures due to the apprehension, understanding and realization of the test. The following parameters were recorded: oxygen saturation (SpO2) and heart rate throughout the test, delta heart rate (heart rate at the end of the test––heart rate at the beginning of the test), delta oxygen saturation (oxygen saturation at the end of the test––oxygen saturation at the beginning of the test), dyspnea (Borg scale) before and at the end of the test, leg discomfort (Borg scale) before and at the end of the test, and number of repetitions.
Endpoints
The primary endpoint was the measurement of the functional exercise capacity using the number of repetitions during the 3MStepT and the 6-minute walk distance (6MWD).
The secondary endpoints were the heart rate, SpO2, dyspnea and leg fatigue before and at the end of both tests and the evolution of heart rate and SpO2 during both tests.
We also assessed the reliability of the 3MStepT.
Statistical analysis
The sample size determination was based on the detection of a 0.40 correlation coefficient between both tests with a power of 90% and an alpha level of 0.05 [Citation28]. The number of participants required for the study was determined to be 48.
Normality of distribution of the variables was verified by Kolmogorov–Smirnov test. Descriptive analyses were expressed as mean with standard deviation and 95% of confidence interval, or median and interquartile range depending on the normality.
Comparisons between results of both best tests were performed by paired Student’s t-test or Wilcoxon’s test depending on the normality. Correlation between results of best 3MStepT and best 6MWT (for validation) and between anthropometric data and results of the tests were calculated by Pearson’s and Spearman correlation coefficient depending on the variable. Intraclass correlation coefficient (ICC) was calculated (for reliability) using a random-effects model for coherence of mean measures to verify reliability between the first and second tests. An ICC value <0.75 was considered as a good reliability [Citation29]. Repeatability between the first and second tests was calculated by paired Student’s t-test and Bland–Altman method. Bias and limits of agreement were calculated.
A value of P < 0.05 was considered as significant. The power of the different tests was calculated.
The data were computed using Statistical Package for the Social Sciences software version 25.0 (IBM, Armonk, NY, USA).
Results
Demographic, clinical and initial spirometric data are reported in .
Table 1. Demographic, clinical and initial spirometric data of patients with COPD.
For the primary endpoint, we found a good correlation between 6MWT (432.6 ± 96.3 m) and 3MstepT (61.2 ± 18.9 steps) (r = 0.78; p < 0.001).
For the secondary endpoints, heart rate and SpO2 were significantly lower at the end of the 6MWT in comparison with the 3MstepT (). The delta heart rate and the delta oxygen saturation were significantly different between 6MWT and 3MStepT ().
Table 2. Comparison of cardiorespiratory variables at the end of 6MWT and 3MstepT.
We found a good correlation between 3MstepT and FEV1 (r = 0.61; p < 0.001).
Dyspnea was not different at the end of each test, but the lower limb fatigue was significantly higher at the end of the 3MstepT in comparison with the 6MWT ().
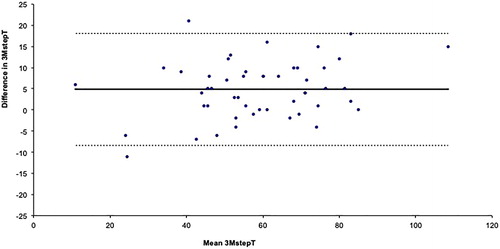
Reliability was excellent for 3MstepT with ICC < 0.9 (ICC = 0.964 (95%CI = 0.936–0.979)). There was a significant difference (p < 0.001) of number of steps between the first (56.4 ± 17.2 steps) and the second 3MstepT (61.2 ± 18.9 steps). First 3MstepT and second 3MstepT agreed with a bias of 4.84 repetitions (95% limits of agreement: –8.4–18.08) ().
Discussion
The aim of this study was to validate the 3MStepT by comparing the 3MStepT and the 6MWT in stable patients with COPD as a tool to quantify the functional exercise capacity.
In this study, we showed a good correlation between 6MWT and 3MstepT (), so the 3MstepT seems to be valid as tool to measure exercise capacity in patients with COPD.
However, we found many differences between both tests. Heart rate and lower limb fatigue were significantly higher at the end of the 3MstepT in comparison with the 6MWT, and SpO2 was significantly lower at the end of the 6MWT in comparison with the 3MstepT ().
The reliability for the 3MStepT was good even if we found a significant difference of number of steps between the first and the second 3MstepT, suggesting a learning effect (+5 steps) for the 3MstepT ().
The 6MWT is a submaximal field test well standardized, which allows the evaluation of exercise capacity with recommendations written by ATS/ERS task force [Citation26]. The 6MWD is responsive to pulmonary rehabilitation [Citation30] and many references equations for 6MWD are available [Citation27, Citation31]. The 6MWT provides information about exercise –induced desaturation [Citation26], and it can be used for the oxygen titration [Citation32]. However, it requires a 30-m corridor so that it can be performed only in hospital unit, which is a limitation for its use in non-hospitalized patients. Another problem is the time required for the realization of the 6MWT [Citation11]. Then it seems important to find others submaximal field tests that require less time and less space, as the 3MstepT.
On the contrary, the 3MstepT is easy to perform, needs a small space, needs only 3 min to be realized, is well tolerated by patients with COPD (dyspnea at the end of the 3Mstp Test was not different in comparison with dyspnea at the end of the 6MWT) () and needs only a 15-cm height platform. Then 3MstepT presents many advantages for the evaluation of functional exercise capacity in patients with COPD.
However, heart rate at the end of the best 3MstepT (112.9 ± 13.4) was significantly higher (p = 0.002) in comparison with heart rate at the end of the best 6MWT (106.2 ± 16.3) (), despite the shorter duration of the 3MstepT. So 3MstepT is more soliciting for the heart than 6MWT, which is a submaximal test, even if it can become maximal in severe patients with COPD [Citation33]. It is also possible that during the 3MStepT, we did not reach a steady-state as it is observed in the study by Da Costa et al. [Citation19], even if the increase seems to be less important after 3 min. 3MstepT stay a submaximal test because theoretical maximal heart rate was never reached but we could hypothesize a similar behavior to the 6MWT for severe patients. Our results are in accordance with those obtained by Chirumberro et al. [Citation34] who showed that stair climbing is a submaximal effort for the most sample of patients with COPD with a higher metabolic cost in comparison with maximal cycle exercise test. In the study by Pichon et al. [Citation15], comparing 6-minute stepper test (6MST) and 6MWT, the heart rate was also higher at the end of the 6MST in comparison with the 6MWT. As for the stepper test, we can assume that walking (during the 6MWT) and getting up on a platform (during the 3MstepT) involve different biomechanics and metabolic requirements. That can explain the difference for heart rate and fatigue for the lower limb reached. It seems logical that the fatigue of the leg is significantly more important during the 3MstepT in comparison with the 6MWT, because quadriceps muscles are more solicited during the 3MstepT [Citation35].
At the end of the 3MstepT, oxygen saturation was significantly higher but the difference was clinically not relevant in comparison with the 6MWT. However, both tests objective oxygen desaturation during exercise test. The difference of oxygen desaturation can be due to the difference of time between both tests. The 6MWT is the Gold standard to titrate oxygen at exercise [Citation26]. The results of our study showed significant difference for SpO2 at the end of 6MWT in comparison with the end of the 3MStepT, suggesting that 3MstepT could be less sensitive and not used for oxygen titration at exercise. However, It could be interesting to compare oxygen desaturation during 6MWT and a StepTest with similar duration. The studies about other field tests as 6MST or STST1 are in accordance with our results about the capacity of these tests to measure oxygen desaturation during exercise [Citation13–15]. In our knowledge, no field test, in exception of 6MWT and shuttle walk test has been validated to titrate oxygen at exercise. Then, oxygen titration at exercise must be realized in hospital (necessity of a long corridor) and that is a drawback for patients and healthcare worker who do not work in hospital. In the future, it could be interesting to investigate the capacity of field test requiring small space to titrate oxygen at exercise.
Reliability was excellent for 3MstepT with ICC < 0.9. In comparison with others tests as 6-minute stepper test [Citation17] or STST1 [Citation13], the correlation between 3MstepT and 6MWT was higher. This finding is interesting to show the utility of this new test.
The last finding of this study is the utility to perform a training 3MstepT. For the 6MWT, the authors of the recommendations specify the necessity to conduct two tests for the 6MWT, due to the learning effect. For this study, we conducted two tests for the 6MWT and two tests for the 3MstepT to evaluate the learning for the 3MstepT. We found a significant increase of the number of steps during the second 3MstepT, in comparison with the first 3MstepT (), suggesting a learning effect for the 3MstepT. In interstitial lung disease, Dal Corso et al. [Citation22] did not find significant between-tests difference on the total number of steps climbed. However, Dal Corso et al. studied the 6MStepT (and not the 3MStepT) and compared physiological responses to 6MStepT and maximal cardiopulmonary exercise test. They showed that physiological responses were maximal in the 6MStepT that can explain the absence of difference in number of steps between the two 6MStepT. Then, when 3MstepT is used to evaluate exercise capacity in patients with COPD, we recommend to conduct two tests.
Some limitations need to be addressed. Patients who performed the tests were addressed for pulmonary rehabilitation, and then maybe they were not representative of all patients with COPD. Furthermore, we did not measure the sensitivity and specificity of this test. It is necessary to conduct other study to measure the responsiveness of the 3Mstept after pulmonary rehabilitation and to determine the MCID for this test.
In conclusion, the 3MStepT is reliable, and is an alternative to the 6MWT to estimate functional exercise capacity in stable patients with COPD but cardiorespiratory adaptation and lower limb fatigue are not similar between these tests. The 3MstepT should not be used to titrate oxygen at exercise. We recommend to conduct two 3MstepT to measure exercise capacity. Further studies are needed to investigate sensitivity and determine the MCID for the 3MstepT.
Disclosure statement
The authors for this manuscript disclose no relevant, real or apparent financial interest or affiliation with content discussed in this article.
Additional information
Funding
Notes on contributors
Marc Beaumont
MB, AL, LP, ACB, FC, CLB, and GR contributed to the conception or design of the work. MB, AL, LP, ACB, and GR contributed to the acquisition, analysis, or interpretation of data. MB, AL, LP, ACB, FC, CLB, and GR contributed to the drafting the work or revising it. MB, AL, LP, ACB, FC, CLB, and GR given the final approval of the version to be published and agreement to be accountable for all aspects of the work.
Antoine Losq
MB, AL, LP, ACB, FC, CLB, and GR contributed to the conception or design of the work. MB, AL, LP, ACB, and GR contributed to the acquisition, analysis, or interpretation of data. MB, AL, LP, ACB, FC, CLB, and GR contributed to the drafting the work or revising it. MB, AL, LP, ACB, FC, CLB, and GR given the final approval of the version to be published and agreement to be accountable for all aspects of the work.
Loic Péran
MB, AL, LP, ACB, FC, CLB, and GR contributed to the conception or design of the work. MB, AL, LP, ACB, and GR contributed to the acquisition, analysis, or interpretation of data. MB, AL, LP, ACB, FC, CLB, and GR contributed to the drafting the work or revising it. MB, AL, LP, ACB, FC, CLB, and GR given the final approval of the version to be published and agreement to be accountable for all aspects of the work.
Anne-Cécile Berriet
MB, AL, LP, ACB, FC, CLB, and GR contributed to the conception or design of the work. MB, AL, LP, ACB, and GR contributed to the acquisition, analysis, or interpretation of data. MB, AL, LP, ACB, FC, CLB, and GR contributed to the drafting the work or revising it. MB, AL, LP, ACB, FC, CLB, and GR given the final approval of the version to be published and agreement to be accountable for all aspects of the work.
Francis Couturaud
MB, AL, LP, ACB, FC, CLB, and GR contributed to the conception or design of the work. MB, AL, LP, ACB, and GR contributed to the acquisition, analysis, or interpretation of data. MB, AL, LP, ACB, FC, CLB, and GR contributed to the drafting the work or revising it. MB, AL, LP, ACB, FC, CLB, and GR given the final approval of the version to be published and agreement to be accountable for all aspects of the work.
Catherine Le Ber
MB, AL, LP, ACB, FC, CLB, and GR contributed to the conception or design of the work. MB, AL, LP, ACB, and GR contributed to the acquisition, analysis, or interpretation of data. MB, AL, LP, ACB, FC, CLB, and GR contributed to the drafting the work or revising it. MB, AL, LP, ACB, FC, CLB, and GR given the final approval of the version to be published and agreement to be accountable for all aspects of the work.
Grégory Reychler
MB, AL, LP, ACB, FC, CLB, and GR contributed to the conception or design of the work. MB, AL, LP, ACB, and GR contributed to the acquisition, analysis, or interpretation of data. MB, AL, LP, ACB, FC, CLB, and GR contributed to the drafting the work or revising it. MB, AL, LP, ACB, FC, CLB, and GR given the final approval of the version to be published and agreement to be accountable for all aspects of the work.
References
- Man WDC, Hopkinson NS, Harraf F, et al. Abdominal muscle and quadriceps strength in chronic obstructive pulmonary disease. Thorax. 2005;60:718–722. doi:10.1136/thx.2005.040709.
- Gosselink R, Troosters T, Decramer M. Peripheral muscle weakness contributes to exercise limitation in COPD. Am J Respir Crit Care Med. 1996;153:976–980. doi:10.1164/ajrccm.153.3.8630582.
- Bernard S, LeBlanc P, Whittom F, et al. Peripheral muscle weakness in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;158:629–634. doi:10.1164/ajrccm.158.2.9711023.
- Pitta F, Troosters T, Spruit M, et al. Characteristics of physical activities in daily life in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;171:972–977. doi:10.1164/rccm.200407-855OC.
- Polkey MI, Moxham J. Attacking the disease spiral in chronic obstructive pulmonary disease. Clin Med. 2006;6:190–196. doi:10.7861/clinmedicine.6-2-190.
- Miller J, Edwards LD, Agustí A, et al. Comorbidity, systemic inflammation and outcomes in the ECLIPSE cohort. Respir Med. 2013; Sep107:1376–1384. doi:10.1016/j.rmed.2013.05.001.
- Lacasse Y, Goldstein R, Lasserson TJ, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane database Syst Rev. 2006;4:CD003793.
- McCarthy B, Casey D, Devane D, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;2015:1–209.
- Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European respiratory society statement: Key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188:e13–64. doi:10.1164/rccm.201309-1634ST.
- Holland AE, Wadell K, Spruit M. A. How to adapt the pulmonary rehabilitation programme to patients with chronic respiratory disease other than COPD. Eur Respir Rev. 2013; Dec 122:577–586. doi:10.1183/09059180.00005613.
- Cabillic M, Rass-Roumeguere D, Peron T, et al. [A survey on the performance of the six-minute walk test] . Rev Mal Respir. 2011;28:1111–1123. doi:10.1016/j.rmr.2011.03.018.
- Gloeckl R, Teschler S, Jarosch I, et al. Comparison of two- and six-minute walk tests in detecting oxygen desaturation in patients with severe chronic obstructive pulmonary disease––a randomized crossover trial. Chron Respir Dis. 2016; 13:256–263. doi:10.1177/1479972316636991.
- Reychler G, Boucard E, Peran L, et al. One minute sit-to-stand test is an alternative to 6MWT to measure functional exercise performance in COPD patients. Clin Respir J. 2018;12:1247–1256. doi:10.1111/crj.12658.
- Vaidya T, de Bisschop C, Beaumont M, et al. Is the 1-minute sit-to-stand test a good tool for the evaluation of the impact of pulmonary rehabilitation? Determination of the minimal important difference in COPD. COPD. 2016;Volume 11:2609. doi:10.2147/COPD.S115439.
- Pichon R, Couturaud F, Mialon P, et al. Responsiveness and minimally important difference of the 6-minute stepper test in patients with chronic obstructive pulmonary disease. Respiration. 2016;91:367–373. doi:10.1159/000446517.
- Borel B, Fabre C, Saison S, et al. An original field evaluation test for chronic obstructive pulmonary disease population: the six-minute stepper test. Clin Rehabil. 2010; 24:82–93. doi:10.1177/0269215509343848.
- Grosbois J, Riquier C, Chehere C, et al. Six-minute stepper test: A valid clinical exercise tolerance test for COPD patients. Int J Chron Obstruct Pulmon Dis. 2016;11:657–663.
- Marrara KT, Marino DM, Jamami M, et al. Responsiveness of the six-minute step test to a physical training program in patients with COPD. J Bras Pneumol. 2012; Sep-Oct38:579–587. doi:10.1590/s1806-37132012000500007.
- Da Costa CH, da Silva KM, Maiworm A, et al. Can we use the 6-minute step test instead of the 6-minute walking test? An observational study. Physiotherapy. 2017;103:48–52. doi:10.1016/j.physio.2015.11.003.
- Andrade CH, Cianci RG, Malaguti C, et al. The use of step tests for the assessment of exercise capacity in healthy subjects and in patients with chronic lung disease. J Bras Pneumol. 2012;38:116–124. doi:10.1590/s1806-37132012000100016.
- Leung AS, Chan KK, Sykes K, et al. Reliability, validity, and responsiveness of a 2-min walk test to assess exercise capacity of COPD patients. Chest. 2006;130:119–125. doi:10.1378/chest.130.1.119.
- Dal Corso S, Duarte SR, Neder JA, et al. A step test to assess exercise-related oxygen desaturation in interstitial lung disease. Eur Respir J. 2006; 29:330–336. doi:10.1183/09031936.00094006.
- Balfour-Lynn IM, Ed F, Prasad SA, et al. Diagnostic and therapeutic methods a step in the right direction : assessing exercise tolerance in cystic fibrosis. Pediatr Pulmonol.. 1998;284:278–284. doi:10.1002/(SICI)1099-0496(199804)25:4<278::AID-PPUL8>3.3.CO;2-M.
- Arlaud K, Stremler-Le Bel N, Michel G, et al. [3-min step test: feasibility study for children with bone marrow transplantation] . Rev Mal Respir. 2008; 25:27–32.
- Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report. GOLD Executive Summary. Am J Respir Crit Care Med. 2017;195(5):557–582.
- Holland AE, Spruit M. A, Troosters T, et al. An official European Respiratory Society/American Thoracic Society Technical Standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014;30:1–19. doi:10.1183/09031936.00150314.
- Troosters T, Gosselink R, Decramer M. Six minute walking distance in healthy elderly subjects. Eur Respir J. 1999;14:270–274.
- Hulley S, Cummings S, Browner W, et al. Designing clinical research: an epidemiologic approach. 4th ed. Philadelphia (PA): Wolters Kluwer Health; 2013.
- Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–163. doi:10.1016/j.jcm.2016.02.012.
- Puhan MA, Mador MJ, Held U, et al. Interpretation of treatment changes in 6-minute walk distance in patients with COPD. Eur Respir J. 2008;32:637–643. doi:10.1183/09031936.00140507.
- Enright PL, Duane LS. Reference equations for the six-minute walk in healthy adults. Am J Respir Crit Care Med. 2000;161:1396–1396.
- Poulain M. 6-minute walk testing is more sensitive than maximal incremental cycle testing for detecting oxygen desaturation in patients with COPD. Chest. 2003;123:1401–1407. doi:10.1378/chest.123.5.1401.
- Casas A, Vilaro J, Rabinovich R, et al. Encouraged 6-min walking test indicates maximum sustainable exercise in COPD patients*. Chest. 2005;128:55–61. doi:10.1378/chest.128.1.55.
- Chirumberro A, Ferrali O, Vermeulen F, et al. Is stairclimbing a maximal exercise test for COPD patients? Rev Mal Respir. 2014;31:608–615. doi:10.1016/j.rmr.2013.09.016.
- Dreher M, Walterspacher S, Sonntag F, et al. Exercise in severe COPD: Is walking different from stair-climbing? Respir Med. 2008;102:912–918. doi:10.1016/j.rmed.2008.01.002.