Abstract
Little is known about chronic obstructive pulmonary disease (COPD) patients experience with home-based health treatments, which are currently rapidly evolving. A previous randomized controlled trial investigated the use of long-term oxygen enriched high flow nasal cannula (HFNC) treatment at home. The aim of this study was to explore COPD patients’ experience using home HFNC treatment. Patients in this qualitative study were included from the previous RCT. All patients used long-term oxygen therapy and HFNC, the latter as a primarily nocturnal add-on. Data were collected using semi-structured interviews focused on four themes: ‘Description of daily use’, ‘Experienced changes’, ‘Treatment benefits and disadvantages’ and ‘User-friendliness’. The interviewer played an encouraging, non-normative neutral facilitator role in order to give the participants possibility to explain themselves as fully as possible. Participants were recruited until themes were saturated. A total of 12 patients (5 males, 7 females) and 8 relatives participated. Six themes were identified as important to patient adherence: Perceived lower work of breathing; reduced symptoms; improved quality of sleep; increased activity of daily living; feeling safe; technology use. The results increase our knowledge of patient experience of using HFNC for home treatment, which improved the patients’ experience through reducing symptoms and increase the activity of daily living. Furthermore, they substantiate the necessity of perceived usefulness and ease of use as important factors for adherence to treatment.
Introduction
Chronic obstructive pulmonary disease (COPD) is a common, preventable and treatable disease characterized by persistent respiratory symptoms and airflow limitation. Some of the most common respiratory symptoms are dyspnea, cough and/or sputum production [Citation1–4]. Furthermore, quality of life (QoL) is impaired in COPD patients and it deteriorates with increasing severity of disease [Citation5,Citation6].
Although preventable and treatable, COPD is a slow progressive chronic disease. Patients must learn to live with symptoms that become more severe as the disease progresses [Citation1,Citation2]. Pinnock et al. reported, that COPD patients described their disease as ‘a way of life’ [Citation7]. This is especially relevant with disease flare ups (exacerbations), characterized by worsening of symptoms that can lead to substantial morbidity and mortality [Citation3,Citation8]. COPD exacerbations also contribute to disease progression, therefore the main goal of treatment is to reduce exacerbations and relieve symptoms [Citation3]. In late stage disease patients may suffer from chronic respiratory failure, due to disturbances of gas exchange caused by impairments in either oxygenation or removing carbon dioxide [Citation9]. Data on the prevalence of Chronic hypoxemic failure are sparse, however, the incidence of COPD patients on long-term oxygen therapy (LTOT) in Denmark was relatively stable between 2001 and 2010 [Citation10].
LTOT is an established and well documented treatment for COPD patients with chronic hypoxemic respiratory failure and has been shown to increase survival [Citation11,Citation12]. Despite this, a review by Katsenos et al. showed that only 45–70% of COPD patients are adherent to optimal LTOT [Citation13]. A possible explanation could be side effects caused by LTOT such as nasal dryness, nasal bleeding, dizziness, impaired taste and olfaction, and unpleasant cosmetic effects [Citation13,Citation14]. Another reason for cessation/discontinuing treatment might be a perceived lack of substantial benefits of treatment [Citation13].
Development in home treatment for COPD has evolved over the last two decades with technologies like telemedicine and noninvasive ventilation [Citation15]. A recent published RCT study including 200 COPD patients investigated a new home treatment for COPD patients with chronic hypoxic failure. One hundred patients in the intervention group had a nasal high-flow humidifier device installed at home for complementary use with their standard LTOT. This device can deliver 37C fully humidified respiratory gases between 10 and 60 l/min, with the ability to add supplementary oxygen as required. The above mentioned RCT study presented significant improvements with using high flow nasal cannula (HFNC), including a significant reduction in the number of exacerbations, a decrease in dyspnea (mMRC score) and a positive effect on QoL [Citation16].
Despite the significant treatment effect, half of the patients discontinued treatment within the study period [Citation16]. For future home treatment, it is therefore important to obtain a better understanding of patients’ perspective and the important issues related to treatment adherence.
As health technology for home treatment is evolving, it is important to acknowledge possible obstacles with treatment and meet patients’ needs in order to ensure patients’ adherence to treatment [Citation17,Citation18]. Therefore, knowledge in patients’ experience is of great value for implementing treatment with health technology at home.
The objective of this present study was to explore COPD patients’ experiences with HFNC at home. We focused on patients’ descriptions of use, experienced changes, pros and cons and user-friendliness.
Methods
The methodological approach
The methodological approach of the study was interpretive descriptive inspired by hermeneutics [Citation19]. The focus of the study was on the patients’ perspectives and descriptions of their experiences living with HFNC at home. The study used qualitative semi structured interviews to obtain rich and nuanced descriptions of patients’ experiences. This methodology was adopted as it seeks to understand and explore based on the individual’s own experience [Citation19]. The reporting of the study is in accordance with the Consolidated Criteria for Reporting Qualitative Research (COREQ) [Citation20].
Participants
The participants were purposively and conveniently sampled from the Department of Respiratory Diseases at Aalborg University Hospital in Denmark. All included patients were patients with COPD and chronic hypoxic failure who had been enrolled in the former HFNC study [Citation16]. At time of inclusion, they were treated with HFNC for a minimum of 4 h/day. The length of use ranged from two to 45 months.
At the final 12 months visit in the HFNC study, 12 patients were informed and invited to participate in a qualitative study concerning their experiences with HFNC home treatment by the study nurse. Nine patients from the former intervention group and three patients from the control group were asked for permission to contact them by phone, when the study had been described and approved. Patients from the control group were allowed to start HFNC treatment at the completion of their 1 year within trial period. All patients gave consent. When ready to interview, the study nurse contacted the patients and repeated information and aim of the study. If patients still consented, the interview took place either at the hospital or in the patients’ homes. Patients were also given the option to invite their relatives to participate. All 12 patients, five men and seven women participated. By patients’ choice, eight interviews took place in patients’ homes and four took place at the hospital. In total eight relatives participated in the interview – one daughter, two husbands and five wives. The interviews were carried out from March 2016 till December 2016. Characteristics of patients and the number of relatives participating are presented in .
Table 1. Patient characteristics.
Data collection
Data were collected using interviews [Citation19]. All interviews were conducted by the first author. The interviewer played an encouraging, non-normative neutral facilitator role in order to allow the participants the possibility to explain themselves in their own words as fully as possible [Citation19]. To ensure consistency in the interviews a semi-structured interview guide was developed with open-ended questions. The guide was pilot tested on two COPD patients, and afterwards the first and last author reconsidered content and process. No changes were made, and the interview guide is available in . The semi structured interviews allowed participants to bring up topics or express thoughts that they considered important for their experiences, which were followed up by additional questions if required to fully understand the participants perspective.
Table 2. Semi-structured interview guide.
The interviews lasted from 17 to 44 min and were audiotaped and transcribed verbatim by the first author. The transcriptions of the interviews were completed shortly after the interviews were conducted to determine whether data saturation was reached. As a result, the number of twelve interviews was not determined in advanced but proved to be an adequate number in terms of data saturation as no new insights or nuances emerged during the last interviews [Citation19]. The transcriptions resulted in a total of 89 pages (Calibri size 11).
Ethics
The study was approved by the Danish Data Protection Agency (number 2008-58-0028; 2016-185). Qualitative studies do not need approval from The Ethics Committee (http://www.nvk.dk). All participants were given both oral and written information about the study and informed written consent was obtained from all participants before participation. Confidentiality and anonymity were secured. It was emphasized that participants could withdraw consent at any time without consequences for current or future treatment.
Data analysis
In order to search for meaningful patterns (themes) across the interviews, thematic analysis was performed [Citation19]. Thematic analysis is a method for identifying, analyzing and reporting themes within qualitative data, it is suitable for identifying meaningful themes and patterns across the experiences of patients regarding living with HFNC at home. In accordance with the adaptive approach used in the study, the thematic analysis process was an iterative process. The themes were identified from the data and involved the following steps. The first step of the analysis involved initial reading and precoding in order to get a sense of all data material and to comprehend the overall meaning of the participants’ statements. Preliminary categories and themes were subsequently identified based on the initial coding. The themes were reviewed to check whether they adequately captured the contours of the coded data, which became the basis for theoretical interpretations [Citation19]. The final step in the data analysis involved defining and naming the themes and reporting of the analysis [Citation19].
Results
A total of 12 patients and 8 relatives participated. HFNC was used as an add-on treatment for a mean of 8.5 h/day (self-reported use). The majority of patients were living with their spouse/family, only one patient lived alone. Lung function (FEV1%) at treatment start ranged between 12 and 41%. Furthermore, hypercapnia, defined as PaCO2 > 6.0 kPa was identified in 7/12 (58%) of participants. Patient characteristics are summarized in .
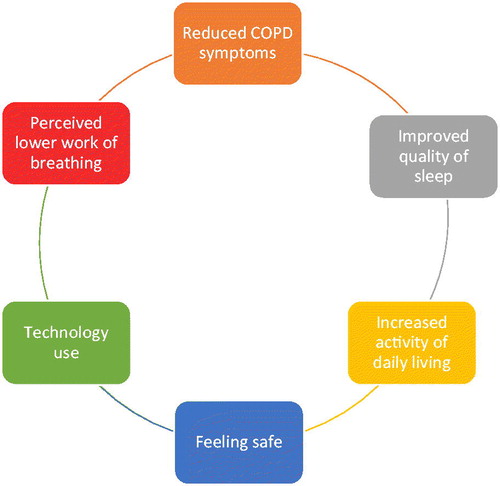
Six themes emerged from the interviews, and these identified that COPD patients and relatives often had the same experiences with HFNC treatment at home. These themes included: ‘Perceived lower work of breathing’, ‘Improved quality of sleep’, ‘Increased activity of daily living’, ‘Reduced COPD symptoms’, ‘Feeling safe’ and ‘Technology use’ (). The findings in each theme are described in the following section substantiated by quotations from interviews with patients and their relatives.
Perceived lower work of breathing
A common experience among patients was that they found it easier to breath and felt more relaxed when using HFNC. Normally their workload of breathing was high, which diminished their energy reserves for other daily living activities. As one patient said:
It’s just getting easier to breathe. Normally, I have to exert myself breathing. I don’t have to with the humidifier on. (PP 12)
When patients feel the difference, it can encourage them to continue their treatment and it reduces their anxieties. Breathing is something most of us take for granted and do automatically. This is not the case for patients with severe COPD. Breathing is on their mind 24/7, but this also changed with the HFNC treatment according to the patients:
I don’t have to think the same way about breathing. I’m more relaxed. (PP 6)
The fact that the HFNC treatment allowed them to relax had a great influence when they go to bed at night. One patient emphasized:
I’m much more relaxed. I spend much less time trying to breathe properly. For instance, when I go to bed at night; earlier I spent a lot of time to get relaxed, I don’t anymore. I can simply just go to bed, lie down with myAirvo on, and I’m relaxed immediately. (PP 1)
Leading on to the next theme ‘Improved quality of sleep’, another patient expanded on her experiences:
I fall asleep faster, maybe because I’m more relaxed. Before I could lie awake for hours, not able to fall asleep. (PP 5)
Improved quality of sleep
The HFNC treatment resulted in a better sleep for most of the patients, as they found it easier to fall asleep, possibly due to the reduced work of breathing. One wife said of her husband’s sleep:
I think he sleeps better, after he began the treatment. His sleep is calmer, and he sleeps longer than before. (PR 2, wife)
Another factor that improved the patients’ sleep was having less interruptions during the night. This might be due to less airway dryness, because of the humidification and the perception of a calmer and easier breathing. Their usual oxygen treatment is not humidified, so it is cool and dry, which causes some patients to wake up with a feeling of dried out airways. Several patients reported that they used to drink water during the night, which could also result in the need for extra toilet visits. All these interruptions can influence the quality of their sleep.
She never complains about dryness anymore, nor is she drinking water during the night as she used to do. (PR 5, husband)
Another common interruption during sleep was patients waking up because they were short of breath. Many patients were in the habit of waking up and sitting on their bedside several times a night to catch their breath. Some patients also needed to use their bronchodilators during the night.
I think he sleeps better, because he doesn’t rouse. He used to sit on his bedside to catch his breath several times during the night, he doesn’t do that anymore. (PR 9, wife)
Being married to a patient with a chronic respiratory condition also disturbed the sleep of the spouse. They are constantly listening to their partners breathing, to check if they are breathing properly. Amelioration of the patients sleep also results in improved sleep quality for the spouses. When the spouses got a good night’s sleep their resourcefulness during the daytime increased.
I also get a better night sleep, when I know my husband is calm and at rest. (PR 12, wife)
Increased activity of daily living
A better sleep can positively influence their level of daily activity. After a good night sleep with HFNC, they felt more rested in the morning. Waking up more energized had a positive effect on their mood and it gave everyone a better start to the day.
When he wakes up in the morning, he tells me that he is feeling so well, he is in a better mood. It’s like he has got more energy. (PR 9, wife)……That’s right, waking up, I feel like a world champion, like I can do everything… (PP 9)
I feel, I have a surplus on energy, and when you do that, it makes you happier. (PP 1)
The increased energy level also affects the patients’ ability to eat. Many COPD patients struggle to maintain a stable weight, due in part, that even chewing and digesting food can cause breathlessness. One patient experienced a weight gain after he started the HFNC treatment.
Before he had trouble gaining weight, the weight only went down. Since he got the humidifier, he gained 5 kilos. It might have been the treatment that gave him more energy to eat. (PR 4, wife)
Another patient and her spouse described a change in the consistency of food she could eat.
Previously she didn’t have the energy to chew meat, vegetables, and she was primary eating blended food and yoghurt. Now she can eat thick slices of bread with cheese, and I don’t have to mash her potatoes anymore. (PR 5, husband)
When patients are able to eat the same food as the rest of the family it has a positive impact on their social life and may lead to patients going out more. In some countries, the socializing culture often includes dining or drinking, which can be one of the reasons why COPD patients stay at home. Eating simply takes too much of their energy, so they are too breathless to talk and socialize while dining. Feeling more energized, several patients explained how they were able to invest more energy in social and physical activities.
I started riding my bike again. When I’m biking, I feel I breathe more freely than I used to. (PP 11)
I’m getting out more…seeing friends. Today I can take my bike and go for coffee at a friends’ house or meet up in town on a café. I didn’t do that before. (PP1)
The fact that patients did have more energy to socialize were also noticed by their relatives and played an important role to the families.
She’s has gained more energy, that’s for sure. She has been out and about more and even participated in birthday parties; she hasn’t done that in years. (PR 3, daughter) …. that’s right, it’s like I have more zest for life….or feel more encouraged. (PP 3)
The majority of patients used HFNC at night, but they still felt it affected their activity levels during the day. One patient also described how she used it extra hours during the day to gain more energy when she had a social event at night.
Despite an increased level of energy, the social activity level remained unchanged for two patients. They argued that the reason for this was a feeling of being stigmatized when going out with their portable oxygen equipment. Even though they felt more energized when using HFNC treatment, they still preferred staying at home. Conversely, another patient felt the way people looked at her had changed after starting the HFNC treatment. Her breathlessness had decreased, and she explained:
Earlier I felt that people were staring after me, I don’t experience that at all today. (PP 1)
Reduced COPD symptoms
This theme describes the participants’ experiences of airway symptoms (i.e. cough, sputum, chest tightness and dyspnea) before and after home HFNC treatment. The symptoms in the morning were the primary focus, as both patients and relatives reported positive changes. Prior to HFNC treatment, most patients said it was normal to start their day coughing. They spent a great deal of time and energy every morning clearing their airways of thick and viscous sputum. Some of the treatments benefits they all experienced were significantly less coughing and sputum production.
It’s been easier to cough and get rid of sputum after I’ve got the humidifier. In the past, I would use a lot more effort and energy on coughing it up. (PP 11)
Earlier, especially in the morning, I had this long, thick mucus, that I couldn’t get rid of. I don’t have that anymore. (PP 12)
HFNC treatment resulted in patients experiencing considerably less cough and sputum symptoms. Another symptom that ameliorated was dryness in both the mouth and airways. Prior to HFNC treatment, all patients described problems with dried out airways.
Waking up, I feel much better now. Earlier I woke up completely dried out in my throat. I never feel this dryness anymore. (PP 9)
Before I got the humidifier, I never left home without a lip balm. I have two unused in the closet, they haven’t been used since. So, in that way it’s been really good. (PP 12)
Reduced airways dryness also seemed to improve patients’ ability to taste and smell. One participant used to work as a chef. For him an important effect of the HFNC treatment was regaining his ability to smell and taste.
One of the first things I noticed after starting the treatment was that I got my taste and smell back. After that the joy of cooking came back. (PP 2)
I actually think I got my taste and smell back. It’s been gone for years, but it’s back now. (PP 5)
Being treated with HFNC truly reduced their airway symptoms. This agrees with the results from the RCT study which also demonstrated that patients treated with HFNC had significantly fewer exacerbations than those treated with LTOT alone [Citation16]. Patients and relatives also noticed the decrease in exacerbations.
The number of exacerbations has decreased enormously. He only had six this year, earlier he had one each month. (PR 4, wife)
It’s great that I don’t have any infections. I picked up some antibiotics nine months ago, but I haven’t taken any of them yet. (PP 6)
Feeling safe
One patient had not felt her symptoms had changed, but in spite of that she had continued to use the HFNC humidifier every day for 45 months. To further understand her reasons for continuing the treatment, she was asked to elaborate. She explained the importance of feeling that you are taking charge and responsibility of a therapy to ameliorate your condition. Another reason for being compliant was the belief in the treatment effect. At each study visit, an arterial puncture was taken both on LTOT, and then after 30 min HFNC treatment [Citation16]. Many COPD patients are already familiar with the risk of hypercapnia when treated with LTOT, and they are therefore paying attention to the blood gas results. In this case, the patient’s knowledge of the positive effects of HFNC treatment in lowering her arterial CO2 levels encouraged her to be persistent.
I hold on to the results from the blood samples. When you can see, that it helps after just 30 min treatment, I believe that it helps. And if not, I can say that I have done something. The humidifier makes me feel safe. It’s the feeling of being able to do something yourself. (PP 10)
Besides her belief in the treatment, she described the importance of being responsible for doing something, kept her safe. Another patient supported this feeling of safety. Having the equipment at home gave them a kind of reassurance that also had benefits for their relatives.
I feel safer having it. I don’t panic as before when I get short of breath which is an important factor I think. (PP 9) ….and that feeling of safety also affects me. (PR 9, wife)
Technology use
This theme describes patients’ use and experiences with the equipment. At inclusion, patients were encouraged to use HFNC approximately 8 h/day preferably during the night. All participants in this study were adherent to HFNC treatment which they used between 7 and 10 h/day. The majority of patients (8/12) only used HFNC at night during sleep, two patients only used it during the day, and two patients used it both day and night. One of the day only users felt it was inconvenient to use the device at night.
I think it’s too much of a hassle and there is also a bit of noise. I think I could get used to it at night, but my wife has to endure it too. (PP 7)
When treating patients at home it is important to include the relatives’ perspective on technology acceptance. It is possible that developing the habit of using HFNC was easier for the patient, who felt the improvements on their wellbeing, while their spouse might be more sensitive to the device noise when going to sleep while not getting any improvement in wellbeing.
Disadvantages with daytime use was described by some patients and were mainly related to mobility challenges. Often treatment was interrupted during the day due to other activities, and for some patients this may have resulted in not resuming the therapy afterwards.
There are small disadvantages…you have to disconnect when going to the toilet for instance, and sometimes I forget to put it on afterwards, because I went on doing something else instead. (PP 3)
It’s like you are locked, you can’t just get up and walk. I have to be next to the machine. (PP 9)
The humidified air was delivered to patients at a temperature of 37 °C, which was quite different from their usual LTOT. The warmth was seen as both an advantage and a disadvantage. One patient described the device as ‘a warm friend’ (PP 5) and another experienced trouble adhering to therapy in summer when the weather was warmer (PP 10). On the other hand, patients described the benefits of warm air, with one patient saying:
The heat is an advantage. It also helps on my arthritis. (PP 4)
and another patient described:
Sometimes I actually long for it. (PP 8)
Both patients and relatives described the equipment as simple to use even for people without technical skills. The device settings were locked, which meant that patients could not change the flow rate without consulting their health care professional and technical staff. This made the treatment manageable and safe for everyone.
The ease of use is high and therefore suitable for people without technical skills. You can’t change the settings or break anything. (PP 9)
The low complexity of the device also made the adaption to treatment easy. Treatment became a habit for most patients, and they used the device continuously. Some adapted to it very quickly, others struggled more in the beginning, especially using the nasal cannula.
You just have to get used to the nasal cannula…getting it attached correctly. I did learn it along the way, so today it’s not a problem. But to begin with it could be a bit annoying. (PP 4)
After getting used to treatment, one wife described how her husband had almost developed an addiction to treatment.
I would almost say, that you are addicted to it. (PR 9, wife)
Being almost dependent to treatment also resulted in a number of patients taking their HFNC device when they went on holidays or weekends away. As one patient said:
I always bring it to our summer residence. It’s become like…I can’t do without it. (PP 5)
Another patient described her negative experiences after ceasing treatment for just a couple of days. These experiences of treatment benefits clearly encouraged patients to continue treatment.
I didn’t sleep with it for two nights, and I certainly felt a difference. I had more trouble breathing and getting rid of mucus. The worsening also lasted during daytime, so it’s obviously doing something. (PP 11)
Discussion
Main findings
The aim of this study was to explore COPD patients’ experiences with HFNC at home by focusing on descriptions of use, experienced changes, pros and cons and ease of use of the device. Six themes were identified, and the findings highlights the importance of treating COPD symptoms which have a crucial and negative impact on physical, social and mental factors. Nearly all patients and relatives described an improvement in symptoms after initiating HFNC, primarily a reduction or elimination of cough/mucus and a reduction of dyspnea. As a consequence of symptom reduction patients experienced improved sleep, resulting in more energy for daily activities – both of social and physical nature. All patients found the device easy to use, but the importance of good information about how to use the device and nasal cannula was also emphasized. Both the feeling of symptom relief and the perceived ease of device use was a strong motivator for treatment adherence.
Interpretation of findings in relation to previously published work
Poor quality sleep for COPD patients has previously been described [Citation1,Citation21–23]. In one study that included 2800 patients from five European countries, Price et al. found that 78% of the patients reported nighttime disturbance [Citation21]. Previous research reported a much greater likelihood of sleep disturbance amongst COPD patients with cough and other nighttime symptoms, such as wheezing and shortness of breath, which substantiates the findings in this study [Citation2,Citation21–23]. With HFNC treatment reducing the COPD patients’ perceived work of breathing and symptoms, the participants in this study experienced a better quality of sleep. They fell asleep faster as they were more relaxed, and they were not disturbed due to airway symptoms. Improving sleep quality also has positive benefits for their daytime activities. Consistent with the findings in this study, Price et al. reported that patients with nighttime symptoms experienced more daytime breathlessness and a higher number of exacerbations [Citation21]. Conversely, patients in our study using HFNC experienced reduced breathlessness and fewer exacerbations, as well as reducing their nighttime symptoms.
The symptoms of breathlessness, fatigue and cough affect patients in their daily activities and thereby have a major impact on their quality of life [Citation4,Citation24–27]. In line with existing research [Citation2,Citation28], we found that if patients reduced the amount of morning symptoms, it not only improved their physical ability but also their mental state during the day. Several studies have demonstrated that patients considered the morning symptoms of COPD as a key barrier to performing their daily activities [Citation1,Citation2,Citation29–31]. In a review by van Bull et al. it was reported that morning symptoms were associated with a sedentary lifestyle and therefore were negatively related to physical activity [Citation28]. In this present study, patients woke up more energized and felt more positive. Not having to start the day coughing resulted in more energy to physical activities and to eat a proper breakfast.
Maintaining a social life is another important issue affecting quality of life. Social isolation is a well-described problem among COPD patients [Citation4,Citation27,Citation32]. In our study the increased activity of daily living and a reduction of coughing and sputum production seems to have a positive influence on patients’ social life. Several patients and relatives described how they were once again participating in social activities, such as birthdays parties with their relatives. This improvement could be explained by findings from COPD studies reporting that COPD patients perceive visible symptoms such as breathlessness and cough as a barrier to leaving their homes [Citation4,Citation27]. Some find coughing up mucus in front of others to be repulsive and embarrassing, therefore COPD symptoms can severely reduce their social interactions. In a recent qualitative study patients also describe they felt the need to explain and apologize when coughing in public [Citation27]. Other concerns around meal-related social events could also be important. Eating and drinking are often a natural part of a socializing culture, but this can be another barrier for COPD patients. In a qualitative study, Odencrants et al. investigated COPD patient’s experiences with meal-related situations. Patients describe a recurrent problem with having a dry mouth and cough, but also less able to taste food was reported. Breathing and tiredness were their main cause of problems, while coughing before or during meals was their main concern [Citation33]. With the HFNC treatment, these cough related concerns and meal-related problems have been reduced, which might explain why patients’ experience a positive effect on their social behavior.
All participants in this study were adherent to treatment as they used the device between 7 − 10 h/day. The technology acceptance model (TAM) has earlier been used to understand end-users accept of Health IT and Tele-medicine. The model describes two main factors of importance to acceptance of technology – ‘perceived usefulness’ and ‘perceived ease of use’ [Citation34,Citation35]. In this study all patients described benefits of treatment and thereby its usefulness. This was mainly because of the experienced effect on COPD symptoms but also a belief in effect as described by one of the patients. This patient explained that her belief in treatment effect, built upon results from blood samples and the feeling of security, were the reasons for her persistent use. Former studies have presented an association between patients’ belief in the necessity of medical treatment and their treatment adherence [Citation36,Citation37].
The first five themes in our findings: Perceived lower work of breathing; reduced COPD symptoms; improved quality of sleep; increased activity of daily living; feeling safe could be related to patients’ perceiving the usefulness of the device as they experienced an amelioration in their condition.
Former studies on LTOT have indicated side-effects and trouble with equipment as barriers to adherence [Citation13,Citation14]. Kampelmacher et al. found discontent related to equipment as the most common complaint amongst patients in LTOT [Citation14]. This is inconsistent with the findings from our study. Participants – both patients and relatives – described the device as easy to use, even for people without technical skills, which according to TAM is promoting for acceptance and actual use of the device. Furthermore, they did not describe any side-effect from HFNC. Some patients, mainly the day-time users, reported disadvantages related to immobility issues. Former studies focusing on nurses’ acceptance of new technologies have shown that if the usefulness of the technology (e.g. treatment benefit) carries weight over the disadvantages, the acceptance remains [Citation38,Citation39]. This might explain the high level of acceptance and thereby adherence among participants in this study.
Strengths and limitations of this study
This paper reports findings from a qualitative study with twelve COPD patients and eight relatives. Patients were purposively and conveniently sampled from a former RCT study and may therefore not fully represent the diversity of COPD patients, as they had to fit certain eligibility criteria. To ensure a maximum variation sample within the inclusion criteria we included both male and female, husbands, wives and a daughter. As they were asked to participate at their final visit, the majority of patients were persistent users of HFNC. Three included patients were from the control group in the former RCT study meaning they did not have any experiences of HFNC use when asked about participating in this study. As all patients included were adherent to treatment, they may have been more positive and engaged in treatment than those who discontinued use of HFNC during the RCT study. Nevertheless, our findings provide important insight into patients’ experiences with home treatment and crucial aspects in relation to their treatment adherence.
As many of the patients had been treated for a longer period when interviewed (mean 23 months), they sometimes experienced trouble remembering exactly how life was before HFNC. Interviewing patients closer to initiation of treatment might have reduced potential recall bias. However, we believe the involvement of relatives was a valuable informative supplement as was including patients from the control group who had been treated for a shorter period at time of the interview. However, further research is needed to detect reasons for patients to discontinue treatment in order to obtain further understanding on how to meet these patients and prevent non-adherence to treatment.
Conclusion
The patients in this study experienced symptom reduction when treated with HFNC, including a perceived lower work of breathing and less cough and sputum. Symptom reduction improved sleep quality, daytime activities, as well as the ability to eat and socialize. Furthermore, important for patients’ adherence is perceived usefulness and perceived ease of use of the device
Contributions
First author (LHS) conducted interviews, undertook all analysis, interpretation and wrote the initial draft of the paper, to which all coauthors (UMW, BLS) contributed. Last author (BSL) contributed to the analysis an interpretation of data.
Disclosure of interest
The authors report no conflict of interest.
Acknowledgement
The authors thanks participants – patients and relatives for spending their time and sharing their valuable experiences.
Additional information
Funding
References
- Miravitlles M, Worth H, Soler Cataluña JJ, et al. Observational study to characterise 24-hour COPD symptoms and their relationship with patient-reported outcomes: results from the ASSESS study. Respir Res. 2014;15(1):1–13. doi:10.1186/s12931-014-0122-1.
- Miravitlles M, Ribera A. Understanding the impact of symptoms on the burden of COPD. Respir Res. 2017;18(1):1–11. doi:10.1186/s12931-017-0548-3.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management and prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease (GOLD) [Internet]. 2019 [cited 2019 Oct 31]. Available from: http://www.goldcopd.org/.
- Williams V, Bruto A, Ellis-Hill C, et al. What really matters to patients living with chronic obstructive pulmonary disease? An exploratory study. Chron Respir Dis. 2007;4(2):77–85. doi:10.1177/1479972307078482.
- Zamzam MA, Azab NY, El Wahsh RA, et al. Quality of life in COPD patients. Egypt J Chest Dis Tuberc. 2012;61(4):281–289. doi:10.1016/j.ejcdt.2012.08.012.
- Budweiser S, Hitzl AP, Jörres RA, et al. Health-related quality of life and long-term prognosis in chronic hypercapnic respiratory failure: a prospective survival analysis. Respir Res. 2007;8(1):9. doi:10.1186/1465-9921-8-92.
- Pinnock H, Kendall M, Murray SA, et al. Living and dying with severe chronic obstructive pulmonary disease: multi-perspective longitudinal qualitative study. BMJ 2011;342(1):d142–d142. doi:10.1136/bmj.d142.
- Wedzicha J, Seemungal T. COPD exacerbations: defining their cause and prevention. Lancet 2007;370(9589):786–796. doi:10.1016/S0140-6736(07)61382-8.
- Budweiser S, Jörres RA, Pfeifer M. Treatment of respiratory failure in COPD. Int J COPD. 2008;3(4):605–618. doi:10.2147/COPD.S3814.
- Ringbaek TJ, Lange P. Trends in long-term oxygen therapy for COPD in Denmark from 2001 to 2010. Respir Med. 2014;108(3):511–516. doi:10.1016/j.rmed.2013.10.025.
- Report of the Medical Research Council Working Party. Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Lancet 1981;317(8222):681–686.
- Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: a clinical trial. Nocturnal Oxygen Therapy Trial Group. Ann Intern Med 1980;93:391–398.
- Katsenos S, Constantopoulos SH. Long-term oxygen therapy in COPD: factors affecting and ways of improving patient compliance. Pulm Med. 2011;2011:1–8. doi:10.1155/2011/325362.
- Kampelmacher MJ, Van Kesteren RG, Alsbach GPJ, et al. Characteristics and complaints of patients prescribed long-term oxygen therapy in The Netherlands. Respir Med. 1998;92(1):70–75. doi:10.1016/S0954-6111(98)90035-X.
- Spencer TR, Barcomb TF. New technologies in COPD management. Curr Emerg Hosp Med Rep. 2014;2(3):143–150. doi:10.1007/s40138-014-0051-9.
- Storgaard LH, Hockey H, Laursen BS, et al. Long-term effects of oxygen-enriched nasal high flow treatment in COPD with chronic hypoxemic respiratory failure. COPD. 2018;13:1195–1205. doi:10.2147/COPD.S159666.
- Bosworth H. Improving patient treatment adherence: a clinician’s guide. Bosworth H, editor. Vol. 53. New York (NY): Springer; 2010. p. 160.
- World Health Organization. Adherence to long-term therapies: evidence for action. Vol. 2. Geneva (Switzerland): WHO; 2003.
- Kvale S, Brinkmann S. Interview: Det kvalitative forskningsinterview som håndvaerk. 3rd ed. Copenhagen (Denmark): Hans Reitzels Forlag; 2015.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Heal Care. 2007;19(6):349–357. doi:10.1093/intqhc/mzm042.
- Price D, Small M, Milligan G, et al. Impact of night-time symptoms in COPD : a real-world study in five European countries. Int J Chron Obstruct Pulmon Dis. 2013;8:595–603.
- Omachi T, Blanc P, Claman D, et al. Disturbed sleep among COPD patients is longitudinally associated with mortality and adverse COPD outcomes. Sleep Med. 2012;13(5):476–483. doi:10.1016/j.sleep.2011.12.007.
- Stephenson JJ, Cai Q, Mocarski M, et al. Impact and factors associated with nighttime and early morning symptoms among patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;10:577–586. doi:10.2147/COPD.S76157.
- Deslee G, Burgel PR, Escamilla R, et al. Impact of current cough on health-related quality of life in patients with COPD. Int J COPD. 2016;11(1):2091–2097. doi:10.2147/COPD.S106883.
- Peruzza S, Sergi G, Vianello A, et al. Chronic obstructive pulmonary disease (COPD) in elderly subjects: impact on functional status and quality of life. Respir Med. 2003;97(6):612–617. doi:10.1053/rmed.2003.1488.
- Monteagudo M, Rodríguez-Blanco T, Llagostera M, et al. Factors associated with changes in quality of life of COPD patients: a prospective study in primary care. Respir Med. 2013;107(10):1589–1597. doi:10.1016/j.rmed.2013.05.009.
- Cook N, Gey J, Oezel B, et al. Impact of cough and mucus on COPD patients: primary insights from an exploratory study with an Online Patient Community. COPD. 2019;14:1365–1376. doi:10.2147/COPD.S202580.
- Van Buul AR, Kasteleyn MJ, Chavannes NH, et al. Association between morning symptoms and physical activity in COPD: a systematic review. Eur Respir Rev. 2017;26(143):160033. doi:10.1183/16000617.0033-2016.
- Kessler R, Partridge MR, Miravitlles M, et al. Symptom variability in patients with severe COPD: a pan-European crosssectional study. Eur Respir J. 2011;37(2):264–272. doi:10.1183/09031936.00051110.
- Roche N, Small M, Broomfield S, et al. Real world COPD: association of morning symptoms with clinical and patient reported outcomes. COPD 2013;10(6):679–686. doi:10.3109/15412555.2013.844784.
- Partridge MR, Karlsson N, Small IR. Patient insight into the impact of chronic obstructive pulmonary disease in the morning: an internet survey. Curr Med Res Opin. 2009;25(8):2043–2048. doi:10.1185/03007990903103006.
- Gardiner C, Gott M, Payne S, et al. Exploring the care needs of patients with advanced COPD: an overview of the literature. Respir Med. 2010;104(2):159–165. doi:10.1016/j.rmed.2009.09.007.
- Odencrants S, Ehnfors M, Grobe SJ. Living with chronic obstructive pulmonary disease: part I. Struggling with meal-related situations: experiences among persons with COPD. Scand J Caring Sci. 2005;19(3):230–239. doi:10.1111/j.1471-6712.2005.00345.x.
- Holden RJ, Karsh B-T. The technology acceptance model: its past and its future in health care. J Biomed Inform. 2010;43(1):159–172. doi:10.1016/j.jbi.2009.07.002.
- Legris P, Ingham J, Collerette P. Why do people use information technology? A critical review of the technology acceptance model. Inf Manag. 2003;40(3):191–204. doi:10.1016/S0378-7206(01)00143-4.
- Ding A, Patel JP, Auyeung V. Attitudes and beliefs that affect adherence to provider-based complementary and alternative medicine: a systematic review. Eur J Integr Med. 2018;17:92–101. doi:10.1016/j.eujim.2017.12.002.
- Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47(6):555–567. doi:10.1016/S0022-3999(99)00057-4.
- de Veer A, Fleuren M, Bekkema N, et al. Successful implementation of new technologies in nursing care: a questionnaire survey of nurse-users. BMC Med Inform Decis Mak. 2011;11(1):1–12. doi:10.1186/1472-6947-11-67.
- Strudwick G, McGillis Hall L. Nurse acceptance of electronic health record technology: a literature review. J Res Nurs. 2015;20(7):596–607. doi:10.1177/1744987115615658.