Abstract
The effects of health literacy in developing self-management skills among people suffering from Chronic Obstructive Pulmonary Disease (COPD) is a topic that has been lightly tread upon. The advent of tobacco smoking and air pollution caused by the industrialisation era has caused a startling increase in the rates of incidence and prevalence of those diagnosed with COPD. Despite advancement in medical treatment, prevention and health care systems COPD poses a great challenge to public health now than ever before. This systematic review examines eight articles that have dealt with the role health literacy plays in developing self-management skills. This study found that there is no relationship between the adequacy of health literacy and the knowledge or learning of a self-management skill. The relationship between heath literacy and developing skills such as correct technique of inhaler use, awareness of an exacerbation, usage of home-based technological support (telehomecare) needs further delving. Remarkably, it also revealed that health literacy sensitive materials improved self-management skills in all the levels of health literacy. More research is required in identifying literacy sensitive methods that would be beneficial to all disregarding of the level health literary. A wider range of self-management skills pertaining to prevention, maintenance and control needs to be explored.
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease with persistent reduction in airflow. It is not curable but its progression could be slowed or controlled with effective treatment. It is characterised by periods of exacerbation which if not approached correctly could warrant hospitalisation or be life threatening [Citation1]. COPD consists of a spectrum of lung conditions such Emphysema, Chronic Bronchitis, Refractory asthma and some forms of Bronchiectasis [Citation2]. Risk factors include smoking and the inhalation of ambient particulate matter (indoor air pollution—use of biomass fuels to cook and heat homes, out-door pollution, occupational dust and chemicals) [Citation1]. In times past the rates of COPD were higher among the population of the developed worlds but is now rapidly increasing in the middle to lower income countries where multinational tobacco companies have crept in and flourished [Citation3].
COPD is a growing burden on the health- system and is the 5th leading cause of death [Citation4] worldwide. The latest data published by Soriano et al. in the Lancet Respiratory Medicine in 2015 estimated that COPD affected 251 million people [Citation5] and caused 3.2 million deaths, accounting for 5% of global deaths [Citation2]. COPD is estimated to become the 3rd leading cause of global deaths by the year 2030 [Citation6].
The health care costs of COPD encumbrances on the economy of countries. In 2010, the US and the EU spent a staggering sum of $36 million [Citation7] and $48.4 billion [Citation8], respectively on the health care of COPD patients. WHO revealed that COPD caused 2.6% of the global disability-adjusted life years [Citation4].This clearly signposts the importance of prevention, treatment, and self-management of COPD.
Prevention of COPD is a path that public health practitioners have trend upon for years and have succeeded in doing so in terms of policy changes such as taxation on tobacco products, tobacco packaging with warning and reduction in passive smoking by promoting smoke free zones [Citation9]. Meanwhile the medical community have invested millions of dollars into the pharmacological treatment for COPD and the self- management techniques. Despite all these efforts the number of people suffering from COPD and health care costs are constantly rising revealing that multiple gaps exist in all sectors in the management of COPD.
Self-management of COPD, has been poorly elucidated but shows significant potential in terms of salvaging quality of life and economic benefits. The former practice of recommendation of merely increasing knowledge about COPD seems to be tipping over to the biomedical aspect and has proved lacking in results. Rightfully Kaptein et al. stated “Knowledge does not impact on illness behaviour” [Citation10]. Wagg, illustrates that action plan and education are just the basic steps in a comprehensive plan for an improved quality of life of those suffering from COPD [Citation11]. On the other hand self-management is the building of self-efficacy by binding both cognition and emotion thereby improving self-management skills which reduces the number of out-patient visits and the rates of hospitalisation in turn this, substantially reduces health related costs and improves the quality of life of patients [Citation12,Citation13]. A pilot randomised control trial conducted by Taylor et al. on self-management support programme in a UK primary care centre concluded that self-management has a scope to be highly cost effective and would be advantageous to the patient and the health care system [Citation14]. This mounting evidence of the benefits of self-management highlights its importance in the treatment of COPD.
WHO defines health literacy as the “ability of individuals to gain access to, understand and use information in ways which promote and maintain good health for themselves, their families and their communities” [Citation15]. Health literate individuals or communities are more likely to follow COPD self-management programmes. For instance, a study conducted by the Geobars et al. demonstrated that adults 75 years and above with low healthy literacy had poor self-management skills suggesting an association between self- management and health literacy [Citation16].
Search methodology
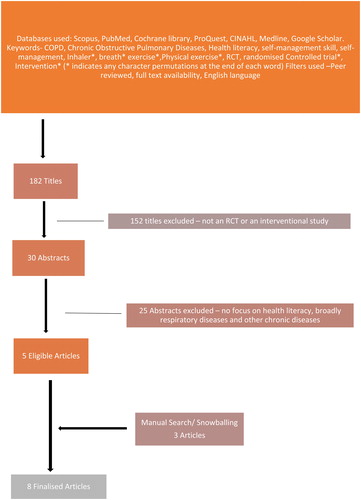
presents the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow chart that was used to identify eligible studies. Well-known databases including Scopus, PubMed, Cochrane library, ProQuest, CINAHL, Medline, Google Scholar were thoroughly searched for eligible papers. Search keywords included Chronic Obstructive Pulmonary Diseases (COPD), COPD, Health literacy, self-management skill, self-management, Randomised Controlled Trial (RCT)*, RCT, Intervention* (* indicates any character permutations at the end of each word). The filters that were used during the search was “Peer reviewed,” “full text availability,” “English language.” No limitations were made to the date of publishment because there was a paucity of articles. Specific inclusion criteria of a randomised control trials and interventional studies were included to attain the highest level in the evidence hierarchy. A broad spectrum of self-management skills such as inhaler techniques, operation of electronic gadjets to detect exacerbatios of COPD, smoking cessation was included. Articles which had no search term “health literacy” were also excluded and so were the articles which had keywords such as “health education” and “education intervention.”
Study selection review
The final selection of the eight articles was done by a dual review process (Cynthia Jeganathan and Hassan Hosseinzadeh). Initially inclusion criteria consisted of randomised controlled trial only which resulted in very few appropriate articles hence “experimental studies” were also included to broaden the search. The abstracts were scanned through for the main themes “COPD” “Self-management”, “Health Literacy” in the English language. There were some articles which had dealt with multiple chronic diseases, of these two studies [Citation17, Citation18] had studied inhaler techniques in both asthma and COPD populations and this was included in this systematic review. To broaden the search further “Self-management” was substituted with specific terms such as “inhaler techniques,” “breathing excersies,” and “recognition of acute exacerbation.” All efforts were made to include all relevant articles because there was a great scarceness of research pertaining to the role of health literacy and COPD. To enhance the body of evidence a manual search via snowballing was also employed. Finally eight RCT and intervention studies met the selection criteria which are outlined in and .
Table 1. Selected articles- Demographics, type of study and self-management technique evaluated.
Table 2. Intervention method used and overall conclusion of selected study articles.
Results
There was a lack of research on the role of health literacy in the self-management of COPD. Only eight studies satisfied the selection criteria of these six are RCTs [Citation17–22] and two are intervention studies [Citation23, Citation24] and only five studies used health literacy as one of the primary outcomes [Citation20–24]. There was no consistency in the self-management skills studied but the most commonly studied skill was the accurate use of inhaler devices. Studies also varied in terms of the type of health literacy being explored such as health literacy as a whole or functional health literacy. Different health literacy tools were used across the studies such as the Danish test of Functional Health literacy in Adults (TOFHLA) [Citation20–22], Short Test of Functional Health Literacy in Adults [Citation19], Rapid Estimate of Adult literacy in Medicine (REALM-SF) [Citation24]. None of the studies had any age restriction which may have introduced bias in the result of these interventions as the younger generation are up-to-date about health issues and technologies hence reaching adequate health literacy.
Five out of the eight studies included correct inhaler skill as the main outcome [Citation17–19, Citation23, Citation24]. However, the types of inhaler techniques being reviewed varied across the studies and included Metered Dose Inhaler (MDI) [Citation17–19, Citation24], MDI with a spacer [Citation19, Citation24], Diskus dry powder inhaler [Citation18, Citation19, Citation23, Citation24], Handihaler dry powder inhaler [Citation17, Citation19, Citation23, Citation24]. Surprisingly health literacy seemed to affect only the Diskus technique in comparison to the others [Citation19] ().Three of the studies were conducted in Denmark [Citation20–22] and the other five in the USA [Citation17–19, Citation23, Citation24]. Of the selected studies 4 recorded the level of education as a baseline measurement [Citation19–22]. Inclusion criteria of participants of most studies were people with an established diagnosis of COPD, not suffering from an episode of acute exacerbation. Alsomali et al. further restricted its inclusion criteria to include participants who had satisfied the GOLD criteria for COPD which requires a post-bronchodilator FEV1/FVC of 70%, making the diagnosis of COPD more definitive. None of the studies included the co-morbidities of the participants as criteria for inclusion but some had added dementia and psychological issues as an exclusion criteria which would have hindered the individuals capacity to absorb, relate and respond to the interventions [Citation23].
In terms of setting, two studies recruited participants just before discharge after an in-patient visit in the hospital setting [Citation25, Citation26]. Both of the studies considered the “time of recovery” at the hospital as the most crucial, to inculcate self-management techniques. There was no consistency in the grading of health literacy levels as each study used different health literacy tool making it very difficult to compare results. Alsomali et al. categorised the participants into inadequate, marginal and adequate literacy levels on the basis of S-TOFHLA. Some the interventions solely depended on the ability of the participant to read and follow instructions given about inhaler and had no other modes such as physical or video demonstration of the use of inhalers which may have affected the results [Citation23].
Two interventions used literacy-sensitive self-management literature [Citation19, Citation23] for instance, RCT conducted by Kiser et al. which studied the effects of literacy sensitive material on the techniques of multiple inhaler usage (diskus, handihaler) and smoking cessation. There was insufficient emphasis upon other aspects of self-management skills such as increase in levels of physical activity, breathing exercises which further objectifies the lack of understanding in the area of self -management skills of COPD.
Three of the five selected RCTs were derived from a very large study called the Danish TeleCare North trial conducted in Denmark. This giant North trial study is very different to the other selected five articles because it studied a very innovative side of the self- management skill of COPD management which directly involved the state of art technological advances. This comprised of a telehomecare technology which entailed the usage of a telekit which comprised of an electronic tablet, oximeter and blood pressure and weight apparatus. This used a sensor based technology located at home that transmitted the vitals of a patient to the health care professional and also enables the latter to give advice to ameliorate the situation hence improving the quality of life of these COPD patients and prevents exacerbation and emergency visits. Several articles have been published in relation to this RCT but only three of its most appropriate and original articles have been included in this study. Another different feature about these three North trials were that they studied Functional Health literacy which is the basic literacy skills needed to utilise health care systems [Citation21, Citation27]. Its short term study had a problematical issue, it lacked a baseline FHL. According to the researchers this step would reduce the possibility of the introduction of a bias during a retest when DTOFHLA is used repeatedly within a short span of time [Citation21], which may have introduced a bias among the other long term studies. Its long-term study conducted after 10 months into the intervention used the FHL data of the short term study as its baseline FHL. It revealed that even though there was an increase in FHL from baseline to the follow-up, there was no statistical significance (p = 0.62) [Citation20]. The drawback of the long-term study was that there was loss of follow up of some participant which caused a mismatch of the baseline characteristics which may have had a confounding effect. Another sub study of this RCT was a cross-sectional study on the self-reported benefits of FHL in the context of the usage of the telekit, but for the purpose of this systematic review this study was considered as a post interventional study as this research was conducted 2 months after the start of using the telekit and like the other studies from the North trial this too concluded that there was no association between increase in their sense of security, freedom, control and awareness of COPD symptoms to the level FHL [Citation22].
Discussion
“Quality of life,” every individual has a different explanation but what would a person suffering from COPD say “ability to breathe freely”? This is a very saddening; one is being robbed of oxygen in air. COPD is an emerging and challenging issue for the public and public health professionals worldwide. Billions and billions of dollars are spent on health care systems, on the treatment and hospitalisation of individuals suffering from COPD. The fact that COPD is a progressive and incurable makes matters even more serious because if no preventive or treatment or control measures are taken, problems at hand would intensify hence warranting a sustainable method for undertaking this issue.
On critically analysing the selected articles, seven out of the eight articles brought to light that participants with higher literacy showed a small margin of improvement in the self-managing skill but did not reach statistical significance hence denied the association between health literacy and self-management skills. This result can be further substantiated by other studies that showed there was no link between the level of knowledge and implementation of a health improving act [Citation25]. Only one study showed that when literacy sensitive measures are used there was statistically significant improvement in the level of self-management skills in both adequate and low health literate participants [Citation19].
Inclusion criteria are noteworthy when selecting participants for a COPD study. A standardised inclusion criterion would make comparison among similar studies reliable to a greater degree. Spirometrical evaluations at the time of participant selections nullifies any unnecessary confusion with other respiratory diseases. The stage of COPD is also another vital issue as different stages of COPD have differences in the receptivity of that individual to a health instruction disregarding the level of health literacy. For example the revised 2017 Global Initiative for Obstructive lung disease (GOLD) classification grades COPD as follows: Grade A—Low risk, Low symptoms, Grade B—Low risk, high symptom burden, Grade C—High Risk, low symptom burden, Grade D—Higher symptom burden [Citation26, Citation28] was used by only one journal in this current review giving it a well organised systematic approach with a greater standard of evidence [Citation23]. It also came to light that all the studies did not consider the comorbidities of the participants. Some articles had exclusion criteria such as psychological diseases, dementia, critically ill conditions but there was no mention to the comorbidities that the participants were suffering from. This aspect is imperative as the ability of an individual to cultivate a skill depends on that individuals’ prioritisation of specific diseases which may have confounded the results. Effing et al. expressed that solely concentrating on alleviation of COPD symptoms would not be useful on people with comorbidities as they have an overlap of symptoms which they had tackled by introducing an intervention combining individually tailored patient initiated action plan and nursing services [Citation29].
Generalisability is debateable when the sample size is small or the study is conducted specifically on certain ethnic groups or nationality. shows that the sample sizes included in the reviewed article were too small to consider as valid evidence. Some of the studies had numbers as low as 23 participants which makes one doubt the reliability of the study [Citation24]. This current review also noted that most studies were conducted in developed countries such as the US and Denmark and the ethnicity of the people considered in the studies had not been mentioned which may have biased the result.
The two self-management skills that were studied in the eight articles were the use of inhalers and tele-homecare technologies. Inhaler use being the first hand therapeutic strategy necessary to control COPD it was only seeming that five of the eight interventions comprised this. Interventions provided instructions of multiple inhalers like the metered dose inhaler, handihaler and diskus. Overall results showed there is a positive association only between health literacy and diskus method when compared to the other techniques. One needs to consider the bias introduced by instructions that were given over a short span of time or was only given once which was the case in most studies, which may not have been sufficient for the participants to absorb, learn and remember the techniques. The RCT on the telehomecare methods, TeleNorth trial evaluated an innovative aspect of self-management- technological monitoring. A foreseen limitation of this study is the fact that most COPD patients being of the elder generation would find it challenging to learn modern technology for example the use of tablets but if this hurdle is correctly managed, this technology promises a new future for those who suffer from COPD. More research needs to be performed on other skills such as quitting smokes, breathing and physical exercises too. A multicomponent research consisting of both medicinal (inhaler techniques, tele-home care) and physical approach (breathing exercises, yoga, smoking cessation) would yield a more potential outcome. An intervention conducted by Stellefson et al. showed that 70% of the participants with COPD with low health literacy were confident about accessing e-health material but failed to distinguish between the high and low quality sites [Citation30] demonstrating that advancing e-literacy among these individuals shows great promise. Other researchers have mined into the use of social media such as the YouTube and Pinterest with a substantial level of success in transferring knowledge and skills to their low health literate COPD participants which improved their quality of life [Citation31, Citation32].
The abundance of health literacy tools poses a challenge when comparing the outcomes of interventions. The development of a standardised health literacy tool would fill the gaps of missing knowledge and doubt of influence of the different tools. Research also needs to further probe into the aspects of using literacy sensitive knowledge assessment [Citation33]. The use of simple to comprehend, culturally appropriate language seems to have a better effect on individuals of varying health literacy. Another interesting aspect is the use of the “language of heart”—the language the individual is most comfortable where the response would be better [Citation34].
On an overall, seven out the eight studies concluded there is no association between health literacy and the self-management skill but most showed that an increase in self-management skills among health literate group but did not or almost reach statistical significance which shows that this facet needs more investigation. A definitive answer is yet to be found. As highlighted above a larger sample population and a systematic methodology with standardised variables would be beneficial in abstracting the real answer. On the other hand, disease specific low health literacy materials and friendly social media exhibits as an optimistic approach to improve self- management skills.
Limitations
Two of the selected articles had studied both asthma and COPD and did not differentiate the results for either of the diseases separately hence confounding the results. Three out the selected eight articles were sub-studies conducted from a single large randomised control trial which may have biased the results. The search and selection of articles was done only in the English language. Severity of COPD was not considered by any of the studies. The lack of control over variables such as the gender, level of education, ethnicity may have confounded the results. Most studies mentioned measured health literacy and its effects as a secondary aim or a by-product of a larger study. Most studies lacked information about the co-morbidities the study population had at the time the studies were conducted. All the studies were performed in developed countries which questions its generalizability to developing worlds.
Future research
This evidence based analysis shows that self-management has the potential to improve the quality of life of people who suffer from COPD disregarding the level of health literacy. The rarity of studies of the current topic substantiates the need for further research on the same to arrive at a definite conclusion. An emphasis also needs to be made on the need of future research on innovative skills and disease specific literacy sensitive material to achieve better health for all affected with COPD.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- World Health Organization. Chronic respiratory diseases; 2018 [cited 2018 June]. Available from: http://www.who.int/respiratory/copd/burden/en/.
- Swift D. COPD: 3.2 million deaths worldwide in 2015. Medscape Pulmonary Medicine; 2017 [cited 2018 June]. Available from: https://www.medscape.com/viewarticle/884400.
- Mannino DM, Sonia Buist A. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007; 370:765–773.
- World Health Organization. Chronic respiratory diseases; 2018 [cited 2018 June]. https://www.who.int/respiratory/copd/en/.
- Chronic Respiratory Disease collaborators. Global, regional and national deaths, prevalence, disability adjusted life year and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017;5:691–706.
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. https://doi.org/10.1371/journal.pmed.003044. doi:10.1371/journal.pmed.0030442.
- The American College of Chest Physicians. CDC reports 36 billion in annual financial cost of COPD in US. CHEST; 2014 [cited 2018 June]. Available from: http://www.chestnet.org/News/Press-Releases/2014/07/CDC-reports-36-billion-in-annual-financial-cost-of-COPD-in-US.
- European Lung White Book. The economic burden of lung disease. European Respiratory Society; 2018 [cited 2018 June]. Available from: https://www.erswhitebook.org/chapters/the-economic-burden-of-lung-disease/.
- World Health Organization. Tobacco-key facts. 2018 [cited 2018 June]. Available from: http://www.who.int/mediacentre/factsheets/fs339/en/.
- Kaptein AA, Fischer MJ, Scharloo M. Self-management in patients with COPD: theoratical context, content, outcomes and integration into clinical care. Int J Chron Obstruct Pulmon Dis. 2014;9:907.
- Wagg k. Unravelling self-management for COPD: what next? Chron Respir Dis. 2012;9(1):5–7. doi:10.1177/1479972311435910.
- Bourbeau J, Collet JP, Schwartzman K, et al. COPD: economic benefits of self-management education in COPD. Chest. 2006;130(6):1704–1711. doi:10.1378/chest.130.6.1704.
- Gadoury M, Schwartzman K, Rouleau M, et al. Self-management reduces both short- and long-term hospitalisation in COPD. Eur Respir J. 2005;26(5):853–857. doi:10.1183/09031936.05.00093204.
- Taylor SJ, Sohanpal R, Bremner SA, et al. Self-management support for moderate-to-severe chronic obstructive pulmonary disease: a pilot randomised controlled trial. Br J Gen Pract. 2012;62(603):e687–695. doi:10.3399/bjgp12X656829.
- World Health Organization. Health promotion. 2018 [cited 2018 June]. Available from: www.who.int/healthpromotio/conferenes/9gchp/health-literacy/en/.
- Geboers B, de Winter AF, Spoorenberg SL, et al. The association between health literacy and self-management abilities in adults aged 75 and older, and its moderators. Qual Life Res. 2016;25(11):2869–2877. doi:10.1007/s11136-016-1298-2.
- Press VG, Arora VM, Shah LM, et al. Misuse of respiratory inhalers in hospitalized patients with asthma or COPD. J Gen Intern Med. 2011;26(6):635–642. doi:10.1007/s11606-010-1624-2.
- Press VG, Arora VM, Trela KC, et al. Effectiveness of interventions to teach metered-dose and Diskus inhaler techniques. A randomized trial. Ann Am Thorac Soc. 2016;13(6):816–824. doi:10.1513/AnnalsATS.201509-603OC.
- Kiser K, Jonas D, Warner Z, et al. A randomized controlled trial of a literacy-sensitive self-management intervention for chronic obstructive pulmonary disease patients. J Gen Intern Med. 2012;27(2):190–195. doi:10.1007/s11606-011-1867-6.
- Haesum LKE, Ehlers LH, Hejlesen OK. The long-term effects of using telehomecare technology on functional health literacy: results from a randomized trial. Public Health. 2017;150:43–50. doi:10.1016/j.puhe.2017.05.002.
- Korsbakke Emtekaer Haesum L, Ehlers L, Hejlesen O. Interaction between functional health literacy and telehomecare: short-term effects from a randomized trial Health literacy and telehomecare. Nurs Health Sci. 2016;18(3):328–333. doi:10.1111/nhs.12272.
- Lilholt PH, Haesum LK, Ehlers LH, et al. Specific technological communication skills and functional health literacy have no influence on self-reported benefits from enrollment in the TeleCare North trial. Int J Med Inform. 2016; 91:60–66. doi:10.1016/j.ijmedinf.2016.04.010.
- Alsomali HJ, Vines DL, Stein BD, et al. Evaluating the effectiveness of written dry powder inhaler instructions and health literacy in subjects diagnosed With COPD. Respir Care. 2017;62(2):172–178. doi:10.4187/respcare.04686.
- Beatty CR, Flynn LA, Costello TJ. The impact of health literacy level on inhaler technique in patients with chronic obstructive pulmonary disease. J Pharm Pract. 2017;30(1):25–30. doi:10.1177/0897190015585759.
- Varekojis SM, Miller L, Stein D, et al. Functional health literacy and smoking cessation outcomes. Health Educ. 2011;111(6):464–475. doi:10.1108/09654281111180463.
- Global Initiative for Obstructive Lung Disease. New 2017 GOLD guidelines for COPD released. PulmCCM; 2016 [cited 2018 June]. Available from: https://pulmccm.org/copd-review/new-2017-gold-guidelines-copd-released/.
- Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15(3):259–267. doi:10.1093/heapro/15.3.259.
- Lee B. The 2011 gold classification for COPD: old GOLD vs. new GOLD guidelines. PulmCCM; 2013 [cited 2018 June]. Available from: https://pulmccm.org/review-articles/new-gold-guidelines-2013-better-than-the-old-gold/.
- Effing TW, Lenferink A, Buckman J, et al. Development of a self-treatment approach for patients with COPD and comorbidities: an ongoing learning process. J Thorac Dis. 2014;6(11):1597–1605. doi:10.3978/j.issn.2072-1439.2014.11.14.
- Stellefson ML, Shuster JJ, Chaney BH, et al. Web-based health information seeking and eHealth literacy among patients living with chronic obstructive pulmonary disease (COPD). Health Commun. 2018;33(12):1410–1424. doi:10.1080/10410236.2017.1353868.
- Stellefson M, Chaney B, Ochipa K, et al. YouTube as a source of chronic obstructive pulmonary disease patient education: a social media content analysis. Chron Respir Dis. 2014;11(2):61–71. doi:10.1177/1479972314525058.
- Paige SR, Stellefson M, Chaney BH, et al. Pinterest as a resource for health information on chronic obstructive pulmonary disease (COPD): a social media content analysis. Am J Health Educ. 2015;46(4):241–251. doi:10.1080/19325037.2015.1044586.
- Maples P, Franks A, Ray S, et al. Development and validation of a low-literacy chronic obstructive pulmonary disease knowledge questionnaire (COPD-Q). Patient Educ Couns. 2010;81(1):19–22. doi:10.1016/j.pec.2009.11.020.
- Poureslami I, Kwan S, Lam S, et al. Assessing the effect of culturally specific audiovisual educational interventions on attaining self-management skills for chronic obstructive pulmonary disease in Mandarin- and Cantonese-speaking patients: a randomized controlled trial. Int J Chronic Obstruct Pulm Dis. 2016;11:1811–1822. doi:10.2147/COPD.S105408.