Abstract
COPD is a major cause of morbidity and mortality worldwide and carries a huge and growing economic and social burden. Telemedicine might allow the care of patients with limited access to health services and improve their self-management. During the COVID-19 pandemic, patient’s safety represents one of the main reasons why we might use these tools to manage our patients. The authors conducted a literature search in MEDLINE database. The retrieval form of the Medical Subject Headings (Mesh) was ((Telemedicine OR Tele-rehabilitation OR Telemonitoring OR mHealth OR Ehealth OR Telehealth) AND COPD). We only included systematic reviews, reviews, meta-analysis, clinical trials and randomized-control trials, in the English language, with the selected search items in title or abstract, and published from January 1st 2015 to 31st May 2020 (n = 56). There was a positive tendency toward benefits in tele-rehabilitation, health-education and self-management, early detection of COPD exacerbations, psychosocial support and smoking cessation, but the heterogeneity of clinical trials and reviews limits the extent to which this value can be understood. Telemonitoring interventions and cost-effectiveness had contradictory results. The literature on teleconsultation was scarce during this period. The non-inferiority tendency of telemedicine programmes comparing to conventional COPD management seems an opportunity to deliver quality healthcare to COPD patients, with a guarantee of patient’s safety, especially during the COVID-19 outbreak.
Introduction
Chronic obstructive pulmonary disease (COPD) is a complex chronic respiratory condition, usually caused by exposure to toxic gases or particles [Citation1]. Worldwide, COPD is a major cause of morbidity and mortality and carries a huge and growing economic and social burden [Citation2,Citation3]. Through the global digital transformation and using the data from the recently characterized COPD phenotypes, several studies focusing on the effects of different telemedicine programs for patients with COPD have been published.
Telemedicine is defined as the use of electronic information and communication technology by medical personnel to provide and support health care to patients when they are far away from the health care institutions [Citation4,Citation5]. It encompasses a wide range of technologies such as videoconferencing, wearable devices, internet platforms, mobile applications, store-and-forward devices, streaming media, and terrestrial and wireless communication.
Telemedicine can be used for a wide range of purposes, such as to decrease the demand on existing hospital and healthcare services, to promote health education, to reduce the cost of care, to measure and endorse treatment adherence, to quickly identify disease worsening, and to extend the accessibility of services to patients living in remote locations. Telemedicine is therefore a broad concept that involves diagnosis, treatment, monitoring, education and prevention [Citation6].
The global market of telemedicine, particularly during this time of the COVID-19 pandemic, has been emerging as a safer alternative to usual clinical management in chronic respiratory diseases. In addition, the development of new technologies, easy to use and inexpensive, will increase the number of patients requesting telemedicine services.
Nevertheless, details of the implementation of telemedicine interventions in COPD have not been described, and the effectiveness of telemedicine interventions is still unclear. Therefore, with this organized review by topics of recent literature, we attempt to clarify which areas of interest of telemedicine in COPD care have been well appraised, which outcomes we can except from different interventions, and the possible future programs’ changes to achieve better outcomes in COPD home-based care.
Material and methods
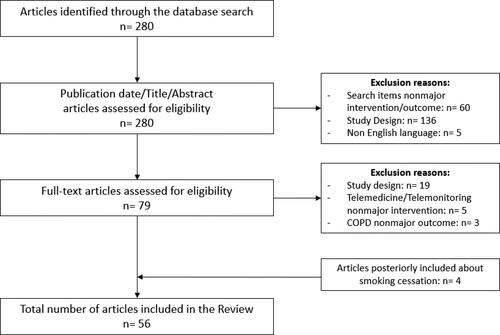
A literature search was carried out in MEDLINE database, for peer-reviewed articles published in English language between January 2015 and June 2020. The retrieval form of the Medical Subject Headings (Mesh) was: ((Telemedicine OR Tele-rehabilitation OR Telemonitoring OR mHealth OR Ehealth OR Telehealth) AND COPD). Two researchers (CSS and MTB) independently extracted data from the abstract of the included studies, being exclusively: systematic reviews, reviews, meta-analysis, clinical trials and randomized-control trials, with the search items in title or abstract. A second assess to eligibility was carried by full-text articles analysis. Any disagreements during the process were resolved by discussion with a third researcher (MMA). An additional search was conducted for relevant recent studies regarding telemedicine assets on smoking cessation. Ultimately, 56 reports were included in this review (detailed information about the search methods is illustrated in the flow chart below—).
Literature review
A significant number of reports have been published, evaluating the benefits and limitations of these technologies in managing and monitoring COPD patients in multiple ways. This review is organized by four main topics of telemedicine use in COPD: Tele-rehabilitation, Tele-health education and self-management, Telemonitoring, and other Mobile applications and websites. In addition, we reviewed four major outcomes: exacerbations of COPD and mortality rates; cost-effectiveness; psychosocial support and smoking cessation.
Tele-rehabilitation
The literature about tele-rehabilitation is plentiful when applied to COPD patients (). The majority of the studies obtained in our search showed either potential or positive results in augmenting rehabilitation adherence [Citation7,Citation13] and reduction of healthcare consumption (due to a decrease in number of COPD exacerbations, emergency department visits and hospitalizations) [Citation10,Citation16]. Also, it seems established a gain in quality of life (HRQoL and QoL) and in exercise tolerance (Six minute walk test) [Citation8,Citation13,Citation15,Citation16]. Likewise, it is noted an improvement in reduction of symptoms, increase in exercise capacity or tolerance and sense of social support [Citation8,Citation13,Citation15]. It seems to be established that rehabilitation through telemedicine, especially by video platform, is safe [Citation8,Citation15], and well accepted by the patients that were satisfied with this type of programme [Citation13,Citation15]. A recent review also stated that it is feasible to deliver teleconsultations prior the initiation of pulmonary rehabilitation for rural or remote patients [Citation14].
Table 1. Summary of the studies selected on the topic Tele-rehabilitation applied to patients with COPD.
Tele-health education and self-management interventions
Tele-health education and self-management is characterized by certain interventions that empower patients, giving them the ability to manage by themselves their diseases with confidence [Citation16]. The complexity of the digital health for self-management of COPD has escalated with recent advancement in technology [Citation17]. Many reports attempted to show the short and long-term benefits of these interventions in chronic respiratory diseases (). The majority of studies determined that telemedicine and e-health interventions have a positive impact in self-management, adherence to treatment [Citation22,Citation23], quality of life improvement [Citation16,Citation19] and symptom management ability [Citation22], though a trial by Rixon, L., et al. [Citation19] specified that telehealth only significantly improved quality of life in long term follow-ups (compared to short term follow-ups). These interventions were well accepted by patients and facilitated doctor-patient relationship [Citation23,Citation25] and transition from inpatient to home-based care after an exacerbation [Citation21]. Despite the overall positive outcomes, two studies have shown contradictory results. One RCT did not manage to find a positive effect on global health status even though suggesting there may be benefits in reduced hospital admissions and primary care visits [Citation20] and another RCT found no significant reduction in unplanned all-cause hospitalization days, but showed that the implemented intervention reduced mortality in severe COPD patients [Citation18]. Although, there were no reported main negative effects, further studies are needed to consolidate the possible impact of these technologies in self-management and health education in COPD patients [Citation24,Citation26,Citation27].
Table 2. Studies selected on the topic Tele-health education and self-management in COPD.
Telemonitoring
The definition of this concept implies the transmission of physiologic and other noninvasive data [Citation4]. The literature obtained by our search was extensive on this topic and the monitoring assessment and data alerts differed from study to study as it was already identified [Citation28]. Telemonitoring is not generally accepted yet because of a lack of compelling evidence of its beneficial long-term effects and, once again, the results obtained were mixed (). Studies report improvements in some outcomes assessed: quality of life [Citation12,Citation31], hospital readmissions at three months after discharge [Citation41], and time to readmissions and all cause emergency department or hospital admissions [Citation29,Citation34]. Vianello, A., et al. contradicts this information, with negative results in quality of life and a RCT with 578 patients intervened by Lilholt PH, et al. exposed a non-superior health-related quality of life in a 12-months follow-up [Citation32,Citation33]. Other data suggests it might not have impact in reducing mortality and exacerbation-related outcomes in COPD [Citation35], with others showing reticence regarding the application of these interventions in a generalized way (34), stating that the benefits might come from the fact that patients submitted to clinical trials have more attention and support with the disease than otherwise they would receive. Few reports also established positive results and possibilities for the successful application of telemonitoring interventions: with regard to noninvasive ventilation [Citation38] forced expiratory volume [Citation39], peripheral oxygen saturation [Citation28,Citation29,Citation42] and physical activity [Citation12]. There are also investigations into new technologies and telemonitoring methods with encouraging outcomes, such as, respiratory oscillometry [Citation30,Citation36,Citation43], exhaled breath temperature [Citation37] or telemonitoring machine learning that will enable treatments to be personalized and early detect COPD exacerbations [Citation6,Citation38,Citation40].
Table 3. Studies selected on the topic telemonitoring in COPD.
Mobile applications and websites
Some recent reviews advocate that mobile applications and websites might have positive outcomes (), promoting self-management, health-education and facilitating the way healthcare providers meet their patient’s needs [Citation23,Citation48]. However more research is encouraged so that conclusions can be drawn in the future [Citation47,Citation48] considering that current information about mobile applications and websites in COPD health-education, self-management, and physical activity maintenance after a pulmonary rehabilitation program seems limited [Citation44,Citation45].
Table 4. Studies selected on the topic mobile applications and websites in COPD.
Exacerbations of COPD and mortality rates
Smartphones, artificial intelligence and wearable devices are emerging () and their role for early prediction and prevention of COPD exacerbations has been rising [Citation17]. The studies in our review reported contradictory outcomes regarding exacerbation and mortality rates. Hospitalization and readmissions decreased after implementation of a personalized care delivered through a web-based call center [Citation26]. Acute exacerbations of COPD, emergency department visits and hospital admissions reduced after a tele-rehabilitation programme [Citation10,Citation49] and two other telemonitoring interventions [Citation21,Citation34]. Ding, L., et al. [Citation17] suggested in a recent review a favorable decrease in exacerbation rate but with limited or inconsistent evidence. Other recent report also outlined positive outcomes. Walker, P., et al. [Citation30] stated that telemonitoring by respiratory oscillometry and cardiac parameters reduced hospital readmissions and hospitalization length. Intermediate conclusions were obtained by two systematic reviews: smartphone mediated interventions, when combined with other strategies, might reduce COPD exacerbations [Citation48] and home monitoring by daily spot check SpO2 measurements might be used as a predictor of exacerbation [Citation28]. Nonetheless, more studies are needed to consolidate these suppositions. More self-assured was the conclusion of the paper by Shah, S. et al. that determined pulse oximeter measurements are predictive of COPD exacerbations. Other studies advocated currently insufficient information on how physiological parameters (vital signs and lung function) vary prior to exacerbation to support routine domiciliary monitoring [Citation50]. In severe COPD patients a remote patient management did not reduce emergency room visits or hospital admissions [Citation33] despite reducing the duration of both hospital and ICU stays [Citation29].
Table 5. Summary of the studies selected on the topic exacerbations of COPD.
Concerning mortality rates, a recent 12-months RCT by Kessler, R., et al. [Citation18] revealed a reduced acute care hospitalization days and mortality rate in severe COPD patients. Nevertheless, four reviews stated that telemonitoring and tele-health programs failed to significantly reduce mortality [Citation24,Citation26,Citation35,Citation41].
Cost-effectiveness
Although there are numerous studies about telehealth monitoring interventions, there is still limited evidence about its economic evaluation (). Michaud, T. L., et al. [Citation53] recent systematic review showed a general reduction in costs using telemedicine programs in various chronic diseases management, besides incomplete detailed costs. The existing recent economic analyses from RCTs showed disparity results in cost-effectiveness of telemedicine in COPD care [Citation29,Citation51,Citation52].
Table 6. Summary of the studies selected on the topic cost-effectiveness of telemedicine in COPD.
Psychosocial support
In recent studies, the focus on self-management, telehealth and pulmonary rehabilitation in both physical and mental health preservation is noticeable (). In advanced stages of COPD, chronic respiratory failure often develops, which might undermine mental health and reduce physical activity [Citation55]. Recent outcomes of reviews about psychosocial support and interventions in COPD patients using telemedicine seem contradictory [Citation26,Citation55]. Nonetheless, Mudiyanselage et al., stated an improvement in anxiety and depression and health literacy with telemedicine [Citation51] and another study reported that when a programme of telemedicine in severe COPD involves regular contact with healthcare professionals, patients are more likely to benefit from it [Citation54]. A positive effect on well-being, emotional problems and sense of social support is also described in tele-rehabilitation programmes [Citation15,Citation55].
Table 7. Summary of the studies selected on the topic telemedicine psychosocial support in COPD.
Smoking cessation
Our first literature search did not find results regarding telemedicine assets on smoking cessation. However, a more global search showed some interesting outcomes about mHealth/mobile applications when complementing psychopharmacological therapy (), although with some extra costs [Citation57–59]. In addition, a recent systematic review states that there is a moderate-certainty evidence that automated text message-based smoking cessation interventions can result in superior quit rates than minimal smoking cessation support [Citation60].
Table 8. Summary of the studies selected on the topic telemedicine in smoking cessation.
Literature reviews of telemedicine in COPD
Recent literature reviews regarding a general sight of telemedicine approaches in COPD care () also reported a positive tendency to telehealth interventions, yet inconclusive clinical enhancements and the need for more standardized trials and systematic reviews [Citation6,Citation61–63].
Table 9. Summary of other recent literature reviews about Telemedicine in COPD management.
Discussion
The escalation in complexity and recent advancement in technology and the need for a safe and efficacious follow-up put telemedicine in the spotlight. Therefore, in the past five years, some fallouts have been pointed out regarding telemedicine use in COPD management.
Concerning tele-rehabilitation, our review supports that it seems a feasible and safe alternative to face-to-face pulmonary rehabilitation with an established non-inferiority of major clinical outcomes, such as exercise tolerance, dyspnea level and quality of life [Citation14,Citation15].
Digital health solutions regarding telemonitoring of COPD patients obtained contradictory outcomes, partly because of technical difficulties and low patient compliance. To address these matters, an integrative approach, possibly with continuous improvement and monitoring, seems essential [Citation47]. Another important feature that optimizes the use of telemonitoring is to implement flexible systems that can be customized to individual patients’ requirements, adapted to our diverse healthcare contexts and to correctly identify who the ideal candidates are, at what time they need it, and for how long [Citation6]. Additionally, COPD patients are a very heterogeneous population with different phenotypes, with an overall decline in health status and a variable baseline physiological parameters [Citation40]. Therefore, future research could optimize self-management by using individualized, time-dependent thresholds or predictive algorithms to account for individual differences, diminishing false-alerts, anxiety and lack of compliance [Citation28]. Moreover, artificial intelligence and wearable devices are emerging and finding their way into the health sector and may provide new opportunities for early prediction and prevention of COPD exacerbation, diminishing hospitalizations, emergency room visits and hospital services burden, which would be especially useful during the current pandemic [Citation17,Citation55]. Unexpectedly, none of the reviews assessing mortality in COPD showed a statistically significant improvement within telemedicine programs [Citation24].
COPD is often accompanied by anxiety disturbance, depression, lack of social support, and feeling of isolation. The majority of the reports about psychosocial support interventions or that considered the patients quality of life and general satisfaction about the telemedicine intervention got favorable outcomes, especially with regular contact with healthcare professionals [Citation55,Citation61].
Future clinical trials should include a cost analysis in their reporting to provide financial insights related to the implementation of the intervention [Citation61]. The lack of detailed data on program costs and health-care service savings make it tricky for home-based telemedicine programs to make a solid economic case when considering reimbursement or investment in these programs [Citation53].
Patients’ age, education, experience in technological devices, cognitive, motor and visual abilities or deficits, their families and home environment play an important role in the use of technologies [Citation62]. Therefore, technology-based interventions may not be as effective in some populations, what might limit the wider diffusion of telemedicine programs [Citation64]. In this review the majority of the trials were grounded on high income countries which may not reflect the outcomes in less developed countries/areas. Nevertheless, the tendency for low cost technology, its wide spread throughout the world in different social/age groups and additional training in communication technology of the population, might balance this matter in a near future.
In this COVID-19 pandemic time, we are currently limited in our abilities to diagnose, monitor and manage chronic airway diseases in face-to-face consultations [Citation36]. Surprisingly, none of the included studies intentionally analyzed COPD teleconsultations via telephone or videoconference as first doctor-patient, follow-up or second opinion medical consultations [Citation14]. We consider it is a gap which necessarily should be complemented to the evolution of telemedicine in COPD as a cost-effective and safer health care alternative [Citation65,Citation66].
In conclusion, there was a positive tendency toward benefits in tele-rehabilitation, health-education and self-management, early detection of COPD exacerbations, psychosocial support and smoking cessation. Telemonitoring interventions and cost-effectiveness had contradictory results. The extent and significance of benefits to patients and health-care organizations were not always consistent.
An important limitation of this study is that it only included articles written in English. Other important limitations are the short follow-up period, the small sized population studies and the different inclusion criteria of the majority of the RCTs/reviews included in this report which restrict conclusions and clinical recommendations.
Telemedicine itself seems to be not sufficient to yield a significantly better outcome, but it could be a key add-on in COPD care, especially in the COVID-19 pandemic, reducing both inpatient and outpatient health care burden.
In this time of major health services demand and very unique infection control concerns with the COVID-19 pandemic, a non-inferiority in the main outcomes of telemedicine programs presented in this review seems significant. It is quite likely that from now on telemedicine will allow significant changes in our clinical practice.
Support
No funding was received in the publication of this review.
Declaration of interest
The authors report no conflicts of interest.
References
- Global Initiative for Chronic Obstructive Lung Disease (GOLD) . Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2020 report) [Internet]. EUA: GOLD; 2020 [cited 2020 June 6]. Available from: https://goldcopd.org/wp-content/uploads/2019/12/GOLD-2020-FINAL-ver1.2-03Dec19_WMV.pdf
- GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393(10184):1958–1972.
- Steel N , Ford JA , Newton JN , et al. Changes in health in the countries of the UK and 150 English Local Authority areas 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392(10158):1647–1661. DOI:10.1016/S0140-6736(18)32207-4
- Ambrosino N , Vitacca M , Dreher M , et al. Tele-monitoring of ventilator-dependent patients: a European Respiratory Society Statement. Eur Respir J. 2016;48(3):648–663. DOI:10.1183/13993003.01721-2015
- Solli H , Bjørk IT , Hvalvik S , et al. Principle-based analysis of the concept of telecare. J Adv Nurs. 2012;68(12):2802–2815. DOI:10.1111/j.1365-2648.2012.06038.x
- Vitacca M , Montini A , Comini L . How will telemedicine change clinical practice in chronic obstructive pulmonary disease? Ther Adv Respir Dis. 2018;12:1753465818754778. DOI:10.1177/1753465818754778
- Broadbent E , Garrett J , Jepsen N , et al. Using robots at home to support patients with chronic obstructive pulmonary disease: pilot randomized controlled trial. J Med Internet Res. 2018;20(2):e45. DOI:10.2196/jmir.8640
- Bernocchi P , Vitacca M , La Rovere MT , et al. Home-based telerehabilitation in older patients with chronic obstructive pulmonary disease and heart failure: a randomised controlled trial. Age Ageing. 2018;47(1):82–88. DOI:10.1093/ageing/afx146
- Bourne S , DeVos R , North M , et al. Online versus face-to-face pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: randomised controlled trial. BMJ Open. 2017;7(7):e014580. DOI:10.1136/bmjopen-2016-014580
- Vasilopoulou M , Papaioannou AI , Kaltsakas G , et al. Home-based maintenance tele-rehabilitation reduces the risk for acute exacerbations of COPD, hospitalisations and emergency department visits. Eur Respir J. 2017;49(5):1602129. DOI:10.1183/13993003.02129-2016
- Tsai LL , McNamara RJ , Moddel C , et al. Home-based telerehabilitation via real-time videoconferencing improves endurance exercise capacity in patients with COPD: the randomized controlled TeleR Study. Respirology. 2017;22(4):699–707. DOI:10.1111/resp.12966
- Franke KJ , Domanski U , Schroeder M , et al. Telemonitoring of home exercise cycle training in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:2821–2829. DOI:10.2147/COPD.S114181
- Marquis N , Larivée P , Saey D , et al. In-home pulmonary telerehabilitation for patients with chronic obstructive pulmonary disease: a pre-experimental study on effectiveness, satisfaction, and adherence. Telemed J E Health. 2015;21(11):870–879. DOI:10.1089/tmj.2014.0198
- Selzler AM , Wald J , Sedeno M , et al. Telehealth pulmonary rehabilitation: a review of the literature and an example of a nationwide initiative to improve the accessibility of pulmonary rehabilitation. Chron Respir Dis. 2018;15(1):41–47. DOI:10.1177/1479972317724570
- Almojaibel AA . Delivering pulmonary rehabilitation for patients with chronic obstructive pulmonary disease at home using telehealth: a review of the literature. Saudi J Med Med Sci. 2016;4(3):164–171. DOI:10.4103/1658-631X.188247
- Murphy LA , Harrington P , Taylor SJ , et al. Clinical-effectiveness of self-management interventions in chronic obstructive pulmonary disease: an overview of reviews. Chron Respir Dis. 2017;14(3):276–288. DOI:10.1177/1479972316687208
- Ding H , Fatehi F , Maiorana A , et al. Digital health for COPD care: the current state of play. J Thorac Dis. 2019;11(Suppl 17):S2210–S2220. DOI:10.21037/jtd.2019.10.17
- Kessler R , Casan-Clara P , Koehler D , et al. COMET: a multicomponent home-based disease-management programme versus routine care in severe COPD. Eur Respir J. 2018;51(1):1701612. DOI:10.1183/13993003.01612-2017
- Rixon L , Hirani SP , Cartwright M , et al. A RCT of telehealth for COPD patient's quality of life: the whole system demonstrator evaluation. Clin Respir J. 2017;11(4):459–469. DOI:10.1111/crj.12359
- Farmer A , Williams V , Velardo C , et al. Self-management support using a digital health system compared with usual care for chronic obstructive pulmonary disease: randomized controlled trial. J Med Internet Res. 2017;19(5):e144. DOI:10.2196/jmir.7116
- Ritchie CS , Houston TK , Richman JS , et al. The E-Coach technology-assisted care transition system: a pragmatic randomized trial. Transl Behav Med. 2016;6(3):428–437. DOI:10.1007/s13142-016-0422-8
- Niznik JD , He H , Kane-Gill SL . Impact of clinical pharmacist services delivered via telemedicine in the outpatient or ambulatory care setting: a systematic review. Res Social Adm Pharm. 2018;14(8):707–717. DOI:10.1016/j.sapharm.2017.10.011
- Morrison D , Mair FS , Yardley L , et al. Living with asthma and chronic obstructive airways disease: using technology to support self-management—an overview. Chron Respir Dis. 2017;14(4):407–419. DOI:10.1177/1479972316660977
- Hanlon P , Daines L , Campbell C , et al. Telehealth interventions to support self-management of long-term conditions: a systematic metareview of diabetes, heart failure, asthma, chronic obstructive pulmonary disease, and cancer. J Med Internet Res. 2017;19(5):e172. DOI:10.2196/jmir.6688
- Morton K , Dennison L , May C , et al. Using digital interventions for self-management of chronic physical health conditions: a meta-ethnography review of published studies. Patient Educ Couns. 2017;100(4):616–635. DOI:10.1016/j.pec.2016.10.019
- Ko FW , Chan KP , Hui DS , et al. Acute exacerbation of COPD. Respirology. 2016;21(7):1152–1165. DOI:10.1111/resp.12780
- Kruse C , Pesek B , Anderson M , et al. Telemonitoring to manage chronic obstructive pulmonary disease: systematic literature review. JMIR Med Inform. 2019;7(1):e11496. DOI:10.2196/11496
- Buekers J , De Boever P , Vaes AW , et al. Oxygen saturation measurements in telemonitoring of patients with COPD: a systematic review. Expert Rev Respir Med. 2018;12(2):113–123. DOI:10.1080/17476348.2018.1417842
- Soriano JB , García-Río F , Vázquez-Espinosa E , et al. A multicentre, randomized controlled trial of telehealth for the management of COPD. Respir Med. 2018;144:74–81. DOI:10.1016/j.rmed.2018.10.008
- Walker PP , Pompilio PP , Zanaboni P , et al. Telemonitoring in chronic obstructive pulmonary disease (CHROMED). A randomized clinical trial. Am J Respir Crit Care Med. 2018;198(5):620–628. DOI:10.1164/rccm.201712-2404OC
- Tupper OD , Gregersen TL , Ringbaek T , et al. Effect of tele-health care on quality of life in patients with severe COPD: a randomized clinical trial. COPD. 2018;13:2657–2662. DOI:10.2147/COPD.S164121
- Lilholt PH , Witt Udsen F , Ehlers L , et al. Telehealthcare for patients suffering from chronic obstructive pulmonary disease: effects on health-related quality of life: results from the Danish 'TeleCare North' cluster-randomised trial. BMJ Open. 2017;7(5):e014587. DOI:10.1136/bmjopen-2016-014587
- Vianello A , Fusello M , Gubian L , et al. Home telemonitoring for patients with acute exacerbation of chronic obstructive pulmonary disease: a randomized controlled trial. BMC Pulm Med. 2016;16(1):157. DOI:10.1186/s12890-016-0321-2
- Ho TW , Huang CT , Chiu HC , et al. Effectiveness of telemonitoring in patients with chronic obstructive pulmonary disease in Taiwan—a randomized controlled trial. Sci Rep. 2016;6:23797 DOI:10.1038/srep23797
- Li X , Xie Y , Zhao H , et al. Telemonitoring interventions in COPD patients: overview of systematic reviews. Biomed Res Int. 2020;2020:5040521. DOI:10.1155/2020/5040521
- Zimmermann SC , Tonga KO , Thamrin C . Dismantling airway disease with the use of new pulmonary function indices. Eur Respir Dis. 2019;28(151). DOI:10.1183/16000617.0122-2018
- Popov TA , Kralimarkova TZ , Labor M , et al. The added value of exhaled breath temperature in respiratory medicine. J Breath Res. 2017;11(3):034001. DOI:10.1088/1752-7163/aa7801
- Arnal JM , Texereau J , Garnero A . Practical insight to monitor home NIV in COPD patients. COPD. 2017;14(4):401–410. DOI:10.1080/15412555.2017.1298583
- Baroi S , McNamara RJ , McKenzie DK , et al. Advances in remote respiratory assessments for people with chronic obstructive pulmonary disease: a systematic review. Telemed J E Health. 2018;24(6):415–424. DOI:10.1089/tmj.2017.0160
- Tomasic I , Tomasic N , Trobec R , et al. Continuous remote monitoring of COPD patients-justification and explanation of the requirements and a survey of the available technologies. Med Biol Eng Comput. 2018;56(4):547–569. DOI:10.1007/s11517-018-1798-z
- Yang F , Xiong ZF , Yang C , et al. Continuity of care to prevent readmissions for patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. COPD. 2017;14(2):251–261. DOI:10.1080/15412555.2016.1256384
- Shah SA , Velardo C , Farmer A , et al. Exacerbations in chronic obstructive pulmonary disease: identification and prediction using a digital health system. J Med Internet Res. 2017;19(3):e69. DOI:10.2196/jmir.7207
- King GG , Bates J , Berger KI , et al. Technical standards for respiratory oscillometry. Eur Respir J. 2020;55(2):1900753. DOI:10.1183/13993003.00753-2019
- Vorrink SN , Kort HS , Troosters T , et al. Efficacy of an mHealth intervention to stimulate physical activity in COPD patients after pulmonary rehabilitation. Eur Respir J. 2016;48(4):1019–1029. DOI:10.1183/13993003.00083-2016
- Ahern DK , Parker D , Eaton C , et al. Patient-facing technology for identification of COPD in primary care. J Innov Health Inform. 2016;23(2):824. DOI:10.14236/jhi.v23i2.824
- Marcolino MS , Oliveira JAQ , D’Agostino M , et al. The impact of mHealth interventions: systematic review of systematic reviews. JMIR Mhealth Uhealth. 2018;6(1):e23. DOI:10.2196/mhealth.8873
- Hallensleben C , van Luenen S , Rolink E , et al. eHealth for people with COPD in the Netherlands: a scoping review. Int J Chron Obstruct Pulmon Dis. 2019;14:1681–1690. DOI:10.2147/COPD.S207187
- Alwashmi M , Hawboldt J , Davis E , et al. The effect of smartphone interventions on patients with chronic obstructive pulmonary disease exacerbations: a systematic review and meta-analysis. JMIR Mhealth Uhealth. 2016;4(3):e105. DOI:10.2196/mhealth.5921
- Liu F , Jiang Y , Xu G , et al. Effectiveness of telemedicine intervention for chronic obstructive pulmonary disease in China: a systematic review and meta-analysis. Telemed J E Health. 2020. DOI:10.1089/tmj.2019.0215
- Al Rajeh AM , Hurst JR . Monitoring of physiological parameters to predict exacerbations of chronic obstructive pulmonary disease (COPD): a systematic review. J Clin Med. 2016;5(12):108. DOI:10.3390/jcm5120108
- Bohingamu Mudiyanselage S , Stevens J , Watts JJ , et al. Personalised telehealth intervention for chronic disease management: a pilot randomised controlled trial. J Telemed Telecare. 2019;25(6):343–352. DOI:10.1177/1357633X18775850
- Witt Udsen F , Lilholt PH , Hejlesen O , et al. Cost-effectiveness of telehealthcare to patients with chronic obstructive pulmonary disease: results from the Danish 'TeleCare North' cluster-randomised trial. BMJ Open. 2017;7(5):e014616. DOI:10.1136/bmjopen-2016-014616
- Michaud TL , Zhou J , McCarthy MA , et al. Costs of home-based telemedicine programs: a systematic review. Int J Technol Assess Health Care. 2018;34(4):410–418. DOI:10.1017/S0266462318000454
- Barken TL , Söderhamn U , Thygesen E . A sense of belonging: a meta-ethnography of the experience of patients with chronic obstructive pulmonary disease receiving care through telemedicine. J Adv Nurs. 2019;75(12):3219–3230. DOI:10.1111/jan.14117
- Rzadkiewicz M , Nasiłowski J . Psychosocial interventions for patients with severe COPD—an up-to-date literature review. Medicina. 2019;55(9):597. DOI:10.3390/medicina55090597
- Brunton L , Bower P , Sanders C . The contradictions of telehealth user experience in chronic obstructive pulmonary disease (COPD): a qualitative meta-synthesis. PLoS One. 2015;10(10):e0139561. DOI:10.1371/journal.pone.0139561
- Carrasco-Hernandez L , Jódar-Sánchez F , Núñez-Benjumea F , et al. A mobile health solution complementing psychopharmacology-supported smoking cessation: randomized controlled trial. JMIR Mhealth Uhealth. 2020;8(4):e17530. DOI:10.2196/17530
- Richter KP , Shireman TI , Ellerbeck EF , et al. Comparative and cost effectiveness of telemedicine versus telephone counseling for smoking cessation. J Med Internet Res. 2015;17(5):e113. DOI:10.2196/jmir.3975
- Cupertino AP , Cartujano-Barrera F , Perales J , et al . “Vive Sin Tabaco… ¡Decídete!" Feasibility and acceptability of an e-Health smoking cessation informed decision-making tool integrated in primary healthcare in Mexico. Telemed J E Health. 2019;25(5):425–431. DOI:10.1089/tmj.2017.0299
- Whittaker R , McRobbie H , Bullen C , et al. Mobile phone text messaging and app-based interventions for smoking cessation. Cochrane Database Syst Rev. 2019;10(10):CD006611. DOI:10.1002/14651858.CD006611.pub5
- Gaveikaite V , Grundstrom C , Winter S , et al. A systematic map and in-depth review of European telehealth interventions efficacy for chronic obstructive pulmonary disease. Respir Med. 2019;158:78–88. DOI:10.1016/j.rmed.2019.09.005
- Ambrosino N , Fracchia C . The role of tele-medicine in patients with respiratory diseases. Expert Rev Respir Med. 2017;11(11):893–900. DOI:10.1080/17476348.2017.1383898
- Ambrosino N , Makhabah DN , Sutanto YS . Tele-medicine in respiratory diseases. Multidiscip Respir Med. 2017;12(1):9. DOI:10.1186/s40248-017-0090-7
- Witry M , Comellas A , Simmering J , et al. The association between technology use and health status in a chronic obstructive pulmonary disease cohort: multi-method study. J Med Internet Res. 2018;20(4):e125. DOI:10.2196/jmir.9382
- Bauer KA . The ethical and social dimensions of home-based telemedicine. Crit Rev Biomed Eng. 2000;28(3–4):541–544. DOI:10.1615/critrevbiomedeng.v28.i34.330
- Stanberry B . Legal and ethical aspects of telemedicine. J Telemed Telecare. 2006;12(4):166–175. DOI:10.1258/135763306777488825