Abstract
Viral infections are known to be the main trigger for Chronic obstructive pulmonary disease (COPD) exacerbations. Face masks are acknowledged for effective viral aerosol shedding reduction. COVID-19 pandemic generated an opportunity to study the impact of face masks and confinement on droplet transmission diseases, usually implicated in acute exacerbations of COPD (AECOPD). We aimed to evaluate the variation on severe AECOPD (sAECOPD) rate in a Portuguese COPD cohort during the first COVID-19 lockdown and following months. This retrospective self-controlled study enrolled 322 adult patients followed at COPD-specialized consultation in a tertiary hospital from February 2016 to July 2020, of whom 286 met inclusion criteria. Severe AECOPD events were registered from March 2020 (beginning of state of emergency) until July 2020. From 2016 to 2019 there was a mean of 38 patients per year with sAECOPD. During 2020, 11 patients experienced sAECOPD. Over the course of 2020 there was a 73.4% (p < 0.001) decrease in sAECOPD events comparing with previous years’ average. After the end of State of Emergency, the rate of sAECOPD events also declined by 74.6% (p < 0.001) comparing with the same timeline of previous years. Results were consistent and statistically significant when comparing 2020 with each of previous years for every period of analysis. Our findings suggest a sustained decrease in the rate of sAECOPD during confinement and in the following months. The widespread use of face mask and social distancing during COVID-19 pandemic may play an important role in preventing the transmission of respiratory infections and consequently reducing sAECOPD.
Introduction
Respiratory viral infections are known to be the main trigger for chronic obstructive pulmonary disease (COPD) exacerbations. The most common isolated viruses in these patients are rhinovirus, influenza virus and respiratory syncytial virus [Citation1]. Severe acute exacerbations of COPD (sAECOPD) are associated with poor quality of life, high mortality and cardiovascular complications [Citation2]. Also, the number of previous exacerbations is known to be one of the best predictors of future exacerbations [Citation3]. Prevention of exacerbations could therefore seriously impact outcomes of COPD patients.
The first outbreak of the COVID-19 pandemic achieved major expression in Europe during March 2020. Initially, most European countries declared State of Emergency and the population was compelled to confinement, in an effort not to overload healthcare institutions. In Portugal, State of Emergency lasted until May 2nd, when most of population resumed their jobs and usual activities. From that date, it was mandatory to wear a mask in all indoor public places, including hospitals, public transports or supermarkets. Recommended use of face mask has been progressively applied by most governments worldwide, as increasing evidence favored its efficacy in preventing SARS-CoV-2 transmission [Citation4]. This generated an opportunity to study the impact of face masks and social distancing on droplet transmission diseases, usually implicated in COPD exacerbations.
According to mid-October 2020 World Health Organization (WHO) influenza update report, influenza activity remained at lower levels than expected during 2020. This is particularly relevant in Australia, New Zealand and tropical countries of South America and Central America [Citation5], since these countries usually have an influenza activity peak around August (June-September) [Citation6]. Nevertheless, influenza virus activity also declined within two weeks of the COVID-19 emergency declaration in the United States of America. Regarding this evidence, the Centers for Disease Control and Prevention (CDC) considered that certain community mitigation measures as face mask might be useful adjuncts to influenza vaccination during influenza seasons, particularly for populations at highest risk for severe disease [Citation7]. This statement reinforces the potential prevention of severe AECOPD caused by viruses inherent to the generalized use of face mask.
This study aims to evaluate variations in sAECOPD rates after the pandemic outbreak and to discriminate between months of exclusive confinement and the following period when face mask may have played a more differentiated role. Therefore, we analyzed the incidence of sAECOPD events during 2020 as compared with 2016, 2017, 2018 and 2019 in a population of COPD patients.
Methods
Study design
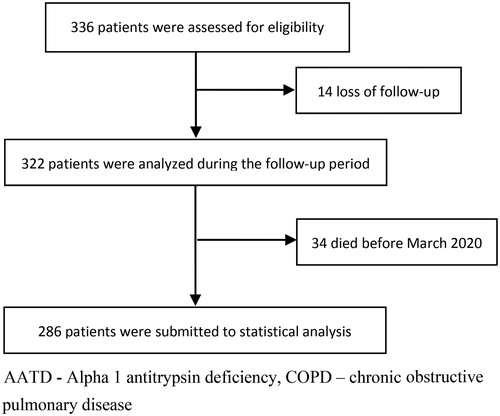
This retrospective self-controlled study enrolled all the 322 adult patients followed at COPD-specialized consultation of the Department of Pulmonology at Centro Hospitalar Universitário do Porto (). The COPD-specialized consultation follows patients whose main pulmonary disease is COPD and who require follow-up in an outpatient hospital setting. Patients were analyzed from February 2016 to July 2020.
Patients were eligible for inclusion in the study if they were at least 18 years old, had diagnosis of COPD and a COPD consultation frequency of at least once a year. Patients were excluded from this study if discharged from COPD-specialized consultation before March 2020 (loss of follow-up).
COPD diagnosis was defined by the presence of a post-bronchodilator FEV1/FVC < 0.70 in patients with appropriate symptoms and significant exposure to noxious stimuli, according to Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2020 report. Among acute exacerbations of COPD (AECOPD), only severe events were registered. Severe AECOPD was defined as an acute worsening of respiratory symptoms that results in additional therapy and requires hospitalization or visiting the emergency room. As recommended by the GOLD 2020 report, we denominated those previously ACO (Asthma and COPD Overlap) as patients with coexisting Asthma characteristics [Citation8].
Patient’s clinical characteristics including symptomatic scores (mMRC - modified Medical Research Council - and CAT - COPD Assessment Test - scores), smoking status, occupational risk and biomass smoke exposure were collected at the beginning of follow-up. The same applies for their functional status (as FEV1% predicted), peripheral eosinophils, immunization status and therapeutic approaches (NIV – noninvasive ventilation -, LTOT - Long-term oxygen therapy - and ICS - Inhaled corticosteroids). Due to the self-controlled nature of the study, patients who died before March 2020 were excluded from analysis.
The COVID-19 pandemic broke out in Portugal on the 2nd of March 2020 and State of Emergency was declared in mid-March. At that time, the majority of the population remained confined to their homes until May 2nd, 2020, the day State of Emergency ended. From that date, it was mandatory to wear a mask in all indoor public places, including hospitals, public transports or supermarkets. Since the start of the pandemic, most of external consultations turned temporarily to a medical teleconsult regimen almost all over the country, allowing to adjust patients’ therapeutics according to their symptoms and recent exacerbation history. Therefore, events of sAECOPD were registered from March 2020 until July 2020 (end of follow-up period). In order to minimize seasonal variation, only events of sAECOPD occurring at the same period (March to July) of previous years (2016 to 2019) were considered for final analysis.
Severe exacerbation events were first collected according to previous patients’ reports and hospital system data. Every COPD-specialized consultation includes a report of previous sAECOPD events for all individual patients, which also applies to any medical teleconsultation performed in 2020. This allowed us to collect a solid database of severe exacerbation events history since 2016. Besides, Portugal has a national inter-hospital system (Registo de Saúde Eletrónico) that automatically records each visit to a hospital or health center and allows to check the clinical record at that other institution. This inter-hospitalar system was checked in end-July for each patient in order to ensure that no hospitalization or emergency room visits data would be missing.
Statistical analysis
Primary outcome was defined as severe AECOPD. All statistical data was processed with IBM SPSS Statistics version 26. Data are presented as the number (percentage) for categorical variables and the median (interquartile range) for continuous variables that are not normally distributed. Paired sample t-test was performed to check the differences of paired data since variables were normally distributed. For all statistical assessment, p < 0.05 was considered statistically significant.
Ethics
The study was performed in accordance with the Declaration of Helsinki and was approved by the local ethics committee (Comissão de Ética do Centro Hospitalar Universitário do Porto/Instituto de Ciências Biomédicas Abel Salazar). The confidentiality of the participants was ensured throughout the entire research process. Adult participant consent was not required because of the retrospective and observational nature of the study.
Results
A total of 286 patients were analyzed. Demographic and clinical characteristics were similar among patients that exacerbated in different years ().
Table 1. Demographic, clinical and functional characteristics at baseline of the overall COPD population and of individuals with at least one severe acute exacerbation of COPD (sAECOPD) event for each year of follow-up.
Certain characteristics were more common in patients with at least one severe exacerbation than in the overall COPD population. Patients with coexisting asthma manifested a propensity for more sAECOPD episodes, although this was only statistically significant in 2017 (22.5% sAECOPD for asthma characteristics vs 8.5% for non-asthma characteristics; p = 0.008) and 2019 (30.0% vs 12.6%; p = 0.004). Besides, patients under long-term oxygen therapy (LTOT) also exhibited more severe exacerbation episodes, a difference that was only statistically significant in 2016 (22.2% for LTOT vs 8.1% non-LTOT; p = 0.002) and 2019 (25.4% vs 12.1%; p = 0.009).
More symptomatic patients with a higher basal CAT presented more severe exacerbations in every year of follow-up (2016, p = 0.010; 2017, p = 0.011; 2018, p = 0.025; 2019, p = 0.001; 2020, p < 0.001). Greater dyspnea (mMRC ≥2) was also associated with more severe exacerbations in 2017 (14.7% vs 6.3%; p = 0.021), 2018 (22.4% vs 11.2%; p = 0.011) and 2019 (19.6% vs 10.5%; p = 0.031). By contrast, very severe COPD (GOLD 4; FEV1 < 30%) was not correlated with severe exacerbations’ rate in any year of follow-up.
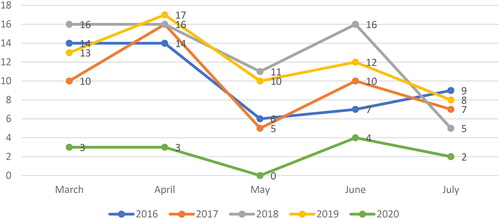
From 2016 to 2019 there was a mean of 38 patients per year with severe exacerbations. During 2020, 11 patients have severely exacerbated (), two of which have died.
Table 2. Number of severe acute exacerbation of COPD (sAECOPD) and of patients with sAECOPD in each year of follow-up.
During the period between 2016 and 2019, each patient presented a mean sAECOPD rate of 0.16 per year, resulting in a paired difference comparing with 2020 of 0.12 per patient (confidence interval [CI] 0.08-0.15, p < 0.001). Over the course of 2020 there was a 73.4% decrease in sAECOPD events comparing with previous years’ average. Results were consistent and statistically significant when comparing 2020s sAECOPD events with each of previous years, as represented in [2016: t(285)=4.02, p < 0.001; 2017: t(285)=3.15, p = 0.002; 2018: t(285)=5.84, p < 0.001; 2019: t(285)=5.51, p < 0.001]. The number of sAECOPD events in 2020 was always lower than in previous years for every month under analysis, as illustrated in .
Table 3. Mean sAECOPD per patient in each year and comparison with 2020.
We also compared the rate of sAECOPD events strictly in the period after the end of State of Emergency (May to July) with the same timeline of previous years (). From May to July 2020 there was a 74.6% decrease in severe AEOPD events comparing with previous years’ average. In fact, each patient presented a mean rate of 0.08 sAECOPD events per year during May to July 2016-2019, a paired difference of 0.06 per patient regarding the same period of 2020 (CI 0.08-0.04, p < 0.001). Similarly, a statistically significant reduction was noted when comparing 2020 with each one of the previous analyzed years [2016: t(285)=3.04, p = 0.003; 2017: t(285)=2.14, p = 0.033; 2018: t(285)=4.03, p < 0.001; 2019: t(285)=3.87, p < 0.001].
Table 4. Mean sAECOPD per patient between May and July of each year and comparison with 2020.
Discussion
Our study demonstrated a significant reduction in the number of severe AECOPD in March-July 2020, comparing to the same months in 2016-2019. This is in agreement with the worldwide decrease of influenza infections in the same period [Citation7] and the expected reduction in overall airborne virus transmission with the use of face mask [Citation4].
During March and April 2020 patients were mainly confined to their homes, so the decrease in severe AECOPD events could mostly be explained by self-confinement. However, a statistically significant fall in severe exacerbation events was also observed between May and July, a time where most people resumed their jobs and frequented at least the supermarket, health and other essential services with the mandatory face mask on. It is not possible though to dissociate the use of face mask from other changes in people's daily lives such as the restriction of social events, the increase in teleworking and the decrease in commuting.
COVID-19 pandemic effect would also expectably have a negative impact on emergency department visits for both patient’s moral conscience of not overloading health services and avoidance of exposure to hospital microorganisms as SARS-CoV-2. According to CDC’s report, emergency department visits were substantially lower specially during an early 4-week interval in the pandemic, followed by an increase of pneumonia and unspecified lower respiratory tract infections [Citation9]. Considering Portugal’s National Health Service preliminary data concerning general emergency department visits per month, the number fell abruptly in April (243626 episodes in 2020 vs 492684 in April 2019), with a progressive recovery in the following months but not to similar numbers reported in previous years. In fact, if we analyze the period between March and July, the mean number of emergency department visits was 321203 in 2020, against 522441 in 2019 [Citation10]. The fact that our population is followed-up regularly in our consultation (including medical teleconsultation during 2020) and the double-checking with national inter-hospital system warrants that we would acknowledge any eventual patient that exacerbated severely, including death events.
A recent study that assessed AECOPD rate until the end of March 2020 in China reported a decline in AECOPD (including hospitalizations) during the pandemic [Citation11]. Analyzing a similar period in Hong Kong, King Chan and colleagues also described a decrease of AECOPD admissions, a finding they associated with increased face mask usage and social distancing [Citation12]. These results are in line with what we observed in our study. On the other hand, a study involving one hundred COPD patients in Spain reported a 13% rate of self-treated at home exacerbations in the 2 months following the beginning of lockdown. [Citation13]. Mild or moderate exacerbations were not assessed in our study. Therefore, it is not possible to assess whether the decrease in sAECOPD may have been due to a corresponding increase in mild to moderate AECOPD.
Since our study is self-controlled, time-invariant confounders are minimized. Regarding study limitations, we used a time span of 5 months since the pandemic has only broke out in Portugal on March 2020. However, we acknowledge that a greater period of comparison would result in more robust evidence. Less than 4% of patients changed ICS, LTOT or NIV prescription status since mid-2016 and this did not seem to affect statistical analysis throughout the article. However, we assume that the self-controlled design does not allow for a therapeutic change weight evaluation in final outcome impact. Also, we have not differentiated the type of mask usually worn by each patient. Surgical masks are acknowledged for effective viral aerosol shedding reduction [Citation14]. Due to shortage of surgical masks for mass population use, cloth masks appeared as an alternative in the market during the pandemic. Although not as effective as surgical masks, cloth masks are a suitable choice for community virus spread prevention when medical masks are unavailable [Citation15]. Therefore, we believe the type of face mask used did not play a major role in our results. Finally, we recognize that we did not control the use of social mask in a patient-to-patient basis nor the activities of daily living that each one performed and this is a design limitation of our article. However, in Portugal it was mandatory for citizens to wear a mask in all hospitals, primary health care and commercial areas during our period of experimental follow-up (March to July 20, 2020), which gives us confidence that this premise was applied in most situations.
Considering the reduction of severe exacerbations of COPD during COVID-19 pandemic observed in our study in accordance with what was reported in China [Citation11] and Hong Kong [Citation12], the use of face masks and social distancing may play a protective role in preventing severe AECOPD by decreasing the transmission of respiratory infectious agents.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- White AJ, Gompertz S, Stockley RA. Chronic obstructive pulmonary disease 6: The aetiology of exacerbations of chronic obstructive pulmonary disease. Thorax. 2003;58(1):73–80. DOI:https://doi.org/10.1136/thorax.58.1.73
- Halpin DM, Miravitlles M, Metzdorf N, et al. Impact and prevention of severe exacerbations of COPD: a review of the evidence. Int J Chron Obstruct Pulmon Dis. 2017;12:2891–2908. DOI:https://doi.org/10.2147/COPD.S139470
- Sadatsafavi M, Xie H, Etminan M, Canadian Respiratory Research Network, et al. The association between previous and future severe exacerbations of chronic obstructive pulmonary disease: Updating the literature using robust statistical methodology. PLoS One. 2018;13(1):e0191243. DOI:https://doi.org/10.1371/journal.pone.0191243
- Liang M, Gao L, Cheng C, et al. Efficacy of face mask in preventing respiratory virus transmission: A systematic review and meta-analysis. Travel Med Infect Dis. 2020;36:101751. DOI:https://doi.org/10.1016/j.tmaid.2020.101751
- World Health Organization. Detailed influenza update - 378. 2020. [cited 2020 Oct 19]. available at https://www.who.int/influenza/surveillance_monitoring/updates/2020_10_12_surveillance_update_378.pdf.
- Caini S, Alonso WJ, Balmaseda A, Global Influenza B Study group–Latin America, et al. Characteristics of seasonal influenza A and B in Latin America: Influenza surveillance data from ten countries. PLoS One. 2017;12(3):e0174592. DOI:https://doi.org/10.1371/journal.pone.0174592
- Olsen SJ, Azziz-Baumgartner E, Budd AP, et al. Decreased influenza activity during the COVID-19 pandemic - United States, Australia, Chile, and South Africa, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(37):1305–1309. DOI:https://doi.org/10.15585/mmwr.mm6937a6
- GOLD 2020 global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease, 2020 report. December 3, 2019. Global Initiative for Chronic Obstructive Lung Disease (GOLD). 2020.
- Hartnett KP, Kite-Powell A, DeVies J, National Syndromic Surveillance Program Community of Practice, et al. Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. DOI:https://doi.org/10.15585/mmwr.mm6923e1
- SNS. Monitorização Mensal de Serviços de Urgência do Serviço Nacional de Saúde, Portugal, November 2020. [updated 10th November 2020]. available at https://www.sns.gov.pt/monitorizacao-do-sns/servicos-de-urgencia/.
- Hu W, Dong M, Xiong M, et al. Clinical courses and outcomes of patients with chronic obstructive pulmonary disease during the COVID-19 epidemic in Hubei, China. Int J Chron Obstruct Pulmon Dis. 2020;15:2237–2248. DOI:https://doi.org/10.2147/COPD.S265004
- Chan KPF, Ma TF, Kwok WC, et al. Significant reduction in hospital admissions for acute exacerbation of chronic obstructive pulmonary disease in Hong Kong during coronavirus disease 2019 pandemic. Respir Med. 2020;171:106085. DOI:https://doi.org/10.1016/j.rmed.2020.106085
- Pleguezuelos E, Del Carmen A, Moreno E, et al. The experience of COPD patients in lockdown due to the COVID-19 pandemic. Int J Chron Obstruct Pulmon Dis. 2020;15:2621–2627. DOI:https://doi.org/10.2147/COPD.S268421
- Milton DK, Fabian MP, Cowling BJ, et al. Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathog. 2013;9(3):e1003205. DOI:https://doi.org/10.1371/journal.ppat.1003205
- Chughtai AA, Seale H, Macintyre CR. Effectiveness of cloth masks for protection against severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(10): e200948. DOI:https://doi.org/10.3201/eid2610.200948