Abstract
The aim of this study was (1) to compare the activities of daily living (ADLs), perceived falling risk and balance in chronic obstructive pulmonary disease (COPD) patients with or without falling history and (2) to investigate the relationship between ADLs and balance. Fourteen patients with COPD with a history of falling whose mean falling frequency was 2.64 ± 0.74 times in the last 12-months (fallers) and 14 age and sex-matched patients with COPD with no history of falling (non-fallers) were included. The outcome measures were the London Chest Activity of Daily Living (LCADL) scale, Activities-Specific Balance Confidence (ABC) scale, Berg Balance Scale (BBS), 6-minute walking test, and quadriceps-femoris strength. Fallers reported increased dyspnoea perception in ADLs, decreased balance confidence, and disturbed balance compared with non-fallers (p < 0.05). A strong correlation was found between the LCADL scale item score (dressing the upper body) and the BBS total score (rho = −0.81, p = 0.001) in fallers. The LCADL scale item score (going out socially) was significantly correlated with the total score of the ABC scale (rho = −0.61, p = 0.001). Moderate correlations were found between the LCADL scale item scores (dressing the upper body, washing hair, and walking up stairs) and the BBS total score (p < 0.003). This study demonstrated that increased severity of dyspnoea perception during ADLs is associated with impaired balance and poor balance confidence, regardless of functional capacity and peripheral muscle strength in patients with COPD. The balance confidence was low in functional mobility-based activities in patients with COPD with a history of falling.
Keywords:
Introduction
Chronic obstructive pulmonary disease (COPD) is characterised by persistent respiratory symptoms and progressive airflow limitation due to airway and/or alveolar abnormalities [Citation1]. The pathologic mechanism and clinical symptoms in COPD limit the respiratory system and cause limited functional status due to systemic inflammation, muscle dysfunction, fatigue, and disturbed balance [Citation2].
Patients with COPD present with limited mobility, muscle weakness, physical inactivity [Citation3], use of supplemental oxygen [Citation4], anxiety, depression [Citation5], impaired postural control [Citation4, Citation6], and balance [Citation2, Citation5] which are associated with older age. Impaired balance leads to a high prevalence of falls, which may cause reduced quality of life and increased mortality in COPD [Citation4]. Older age, increased comorbidities, dyspnoea [Citation7], physical inactivity, muscle weakness [Citation8], fear of falling [Citation8], and reduced balance confidence [Citation9] were reported as possible factors that caused frequent falls in COPD. A recent observational study has pointed out that previous fall history, age, female gender and the presence of coronary heart disease are independent risk factors that predict fall. However, previous falls and diagnosis of coronary heart disease were the most important predictors of falls in COPD patients [Citation7].
Activities of daily living (ADL) such as eating, bathing, dressing, or walking are defined as tasks that people perform daily [Citation10]. The participation of ADL has been limited due to exercise intolerance, muscle weakness, dyspnoea, and impaired postural balance, which may cause poor health-related quality of life in patients with COPD [Citation4, Citation11]. It has been reported that disturbed balance was observed during dynamic activities, but it was similar during static activities in patients with COPD compared with a healthy group [Citation4]. A limited number of studies have reported reduced balance confidence during various mobility-based dynamic activities [Citation2, Citation4, Citation5]. However, ADLs are functional; they are mobility-based activities and also include self-care and domestic activities. Considering that pulmonary rehabilitation programs target increasing the independence level and functional status of patients with COPD, it is vital to understand the possible factors that influence participation in ADLs. To our knowledge, the associations between ADL participation, falling history, and balance have not been investigated in patients with COPD. The primary aim of this study was to compare the ADLs, perceived falling risk and balance in COPD patients with or without falling history. The secondary aim was to investigate the relationship between ADLs and balance.
Methods
Study design
This cross-sectional study was conducted in Istanbul University-Cerrahpasa, Division of Physiotherapy and Rehabilitation, from August 2019 to December 2019. Ethical approval was obtained from the Non-invasive Research Ethics Board of Biruni University (Approval number: 2018/24-15) and conducted in conformity with the Declaration of Helsinki. Verbal and written explanations were provided to participants about the study, and each provided written informed consent. This study was registered in ClinicalTrials.gov (Registration number: NCT04074499).
Participants
All participants, who had been diagnosed as having COPD according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria, were recruited from Istanbul University, Istanbul Medical Faculty, Department of Chest Diseases. The eligibility criteria were as follows: (1) stable disease (no moderate or severe exacerbations in the prior 3 months); (2) ability to walk independently with or without a walking aid; (3) ability to read and write in Turkish; (4) able to follow simple instructions; and (5) no pathology in visual ability and hearing. The exclusion criteria were as follows: (1) a history of specific balance problems (e.g. diagnosed vestibular or neurologic disorder); (2) significant musculoskeletal, neurologic or cardiovascular disorders that limit mobility; (3) use of medication(s) such as sedatives and hypnotics, antidepressants and benzodiazepines; and (4) participation in pulmonary rehabilitation in the last 6 months.
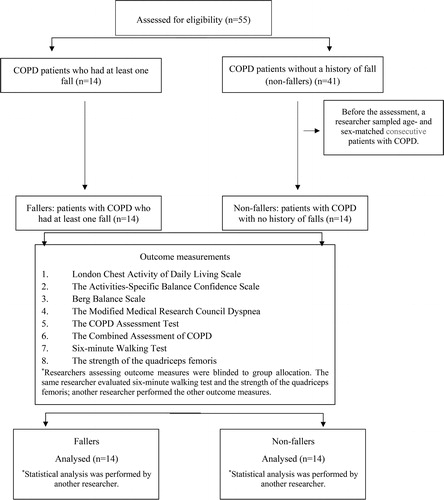
The fallers comprised 14 volunteer patients with COPD who had at least one fall (the mean falling frequency was 2.64 ± 0.74 times in the last 12-months) and non-fallers consisted of 14 volunteers, age- and sex-matched patients with COPD with no history of falling. A researcher questioned details about the circumstances of falls and any resultant injuries, and then sampled age- and sex-matched consecutive patients with COPD to prevent selection bias before the assessments (). The sample size and power calculation were performed using the G*Power 3.1 power analysis program. The calculations were based on a standard deviation of 16.6 points [Citation9], a between-group difference of 19 points [Citation12] (i.e. represents the minimal clinically important difference for the disability of the Activities-Specific Balance Confidence scale), an alpha level of 0.05, a β level of 20%, and the desired power of 80%. These parameters generate a necessary sample size of at least 14 participants for each group. Besides, the calculations were based on an alpha level of 0.05, a β level of 20%, the expected correlation coefficient of 0.50–0.70 (moderate correlation), and the desired power of 80%. These parameters also generate a necessary sample size of at least 7–11 participants for each group. Thus, a total of 28 participants were included in the study.
Outcome measures
The outcome measures for this study were the London Chest Activities of Daily Living (LCADL), the Activities-Specific Balance Confidence (ABC) scale, the Berg Balance Scale (BBS), Six-Minute Walking Test (6MWT), and quadriceps femoris strength. The age, sex, weight, height, body mass index (BMI), dominant extremity, comorbid diseases, smoking status, history of exacerbation in the last year, and falling history were investigated in all eligible participants. The Charlson comorbidity index was used to measure comorbidities [Citation13]. Spirometric data were retrieved from the last one-month clinical records of the patients. The dyspnoea severity was assessed using the Modified Medical Research Council Dyspnoea (mMRC) and impacts of COPD symptoms on health status were assessed using the COPD Assessment Test (CAT). Fall frequency was investigated by asking participants to report any fall events in the last 12 months. The participants were asked: “Have you had any fall, including a slip or trip in which you lost your balance and landed on the floor or ground or a lower level?” [Citation12]. Falls on a slippery road or ice was not accepted as a balance loss-associated fall in patients with COPD.
The mMRC scale is used to determine the level of dyspnoea, according to 5 levels [Citation14]. The CAT is an 8-item questionnaire that evaluates the global impacts of COPD symptoms on overall health status. Each item is scored between 0 to 5, and the total score of CAT ranges from 0 to 40, with higher scores indicating a more severe impact of COPD on health status [Citation15, Citation16]. The COPD severity of the patients was classified according to the new GOLD classification as recommended [this classification is based on spirometric findings and combined symptoms (mMRC and CAT) and exacerbation risk assessment] [Citation1].
The LCADL is a 15-item scale used for assessing the severity of dyspnoea perception during ADLs. It comprises four domains: self-care (4 items), domestic (6 items), physical (2 items), and leisure (3 items). Each item is scored between 0 (I wouldn't do it anyway) to 5 (I need help in doing this or someone to do it for me) and the total score (LCADLtotal) ranges from 0 to 75, with higher scores indicating a more significant limitation in ADLs. The LCADL scale is a reliable, valid, and responsive instrument for assessing restrictions in performing ADLs in patients with COPD [Citation17, Citation18]. The percentage of the total score (LCADL%total) reflects better outcomes of COPD when compared with LCADLtotal. The cut-off point of 28% is sensitive and specific to distinguish the functional status in patients with COPD, with a lower percentage indicating better clinical outcomes [Citation19]. In this study, the participants were questioned about the occurrence of falls during activities in each item of the LCADL scale. The ADLs may be severely restricted in patients with COPD and evaluation of the perceived risk of falling during performing these activities can provide additional information. Therefore, participants were asked to rate each item of the LCADL in terms of the perceived risk of falling using a 5-point scale, where 1 = very low, 2 = low, 3 = moderate, 4 = high, and 5 = very high (Appendix). The internal consistency of the assessment of the perceived risk of falling by rating each item of the LCADL was strong, with a Cronbach’s alpha (α) of 0.95 in this study.
The ABC scale is a self-administered questionnaire for evaluating confidence in maintaining balance in ADLs. It provides information on the level of concern about falls during 16 community-based and home-based activities. The scale is scored between 0 (unsafe) to 100 (completely safe), and the total score (0–1600) is divided by 16 to obtain an individual's ABC score, with higher scores indicating greater balance confidence [Citation20, Citation21]. In patients with COPD, the ABC scale has demonstrated construct validity as well as criterion validity for falls [Citation9]. The ABC scale is identified as a recommended tool for assessing balance in patients with COPD [Citation8].
The BBS is a measure of balance and consists of 14 items evaluating a patient's ability to balance safely during a series of physical tasks. The scale is scored between 0 (unable/unsafe) to 4 (independent/safe), and the BBS total score ranges from 0 to 56, with higher scores indicating better balance control [Citation22, Citation23]. The cut-off point of 52.5 is sensitive and specific to indicate a risk of falls in patients with COPD [Citation24]. The BBS has demonstrated construct validity in patients with COPD and identified as recommended tools for assessing balance in patients with COPD [Citation8].
The 6MWT is a reliable and valid test for evaluating functional capacity. Two 6MWTs were performed according to the guidelines of the American Thoracic Society (ATS) [Citation25]. During the test, participants were instructed to walk as fast as they could, and standardised encouraging phrases were given to participants during each minute. Arterial oxygen saturation as measured using pulse oximetry (SpO2), blood pressures, heart rate, respiratory rate, perceived dyspnoea, and fatigue (modified Borg scale) were assessed before and after the 6MWTs. The changes in perceived dyspnoea, and fatigue after the 6MWT were calculated (Δ dyspnoea and Δ fatigue, respectively). The distance in metres covered in the 6 min of the test (6MWD) was recorded [Citation26].
The isometric muscle strength of the quadriceps femoris of both sides was measured using a hand-held dynamometer (kg N−1), a Nicholas Manual Muscle Tester (model 01160, The Lafayette Instrument Company, Lafayette, Indiana) [Citation27]. Each participant was informed verbally about the technique of the test before starting. The participants were seated on a raised plinth with their knee flexed at 70°. Resistance was applied to the anterior tibia, 5 cm above the lateral malleolus. Each participant was asked to hold the limb in that position for 4 s while a resistive force was applied with the dynamometer in the opposite direction of the intended movement. The assessor instructed the participant to relax the limb at the end of the test period. Each limb was assessed three times, with a recovery period of 30 s and the mean value was calculated [Citation27].
All assessments were performed on the same day for each patient by two researchers who were blinded to the group allocation. The same researcher evaluated 6MWT and the strength of the quadriceps femoris; another researcher performed the other outcome measures. Outcome measures were performed in the following order: assessment of the quadriceps femoris strength, BBS, 6MWT, and then the other outcomes measures. There were at least 10 min resting period between the assessment of the quadriceps femoris strength, BBS, 6MWT ().
Data analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 21.0 software package. Descriptive statistics, including frequency, the percentage for nominal variables, and mean and standard deviation for continuous variables were calculated. The Shapiro-Wilk test was used to test the normality of data distribution. Among the groups, demographic and clinical variables were compared using the independent sample t-test for parametric variables, the Mann-Whitney U test for nonparametric variables, and a Chi-square test for categorical variables. The partial Spearman correlation test, adjusting for Charlson comorbidity index and the isometric muscle strength of the quadriceps femoris, was used to explore the relationship between ADLs and balance and balance confidence. The correlation coefficients (rho) were interpreted as: 0.00–0.30 negligible correlation; 0.30–0.50 weak correlation; 0.50–0.70 moderate correlation; 0.70–0.90 strong correlation; and 0.90–1.00 very strong correlation [Citation28]. The significance level was set as p < 0.05. Bonferroni correction was used to reduce the chances of obtaining type I errors. Significance was accepted as p = 0.05/k (number of items) after Bonferroni correction in the comparison of LCADL scale item scores and the ABC scale item scores between groups, and the correlation between ADLs and balance and balance confidence.
Results
Fifty-five participants with a clinical diagnosis of COPD were assessed for eligibility and a total of 28 voluntary participants (mean age, 70.14 ± 9.54 years; 10 females; mean BMI, 28.48 ± 3.53 kg/m2) were included in the study (). The mean falling frequency was 2.64 ± 0.74 times in the last 12-months in fallers. Only seven patients had fallen in the last 1-months, with mean falling frequency was 1.33 ± 0.50 times. Activities that occurred during falls were sitting to standing (64.28%), outdoor walking (50%), climbing stairs (42.85%), dressing (35.71%), standing (21.42%), and taking a bath (14.28%). Only two participants had a fall, which led to a minor injury, and the others reported no harm.
The demographic and clinical characteristics of the groups are shown in . There were no significant differences between the groups in terms of age, sex, BMI, smoking status, pack-years of smoking history, comorbidities, a combined assessment of COPD, FEV1, FEV1/FVC, mMRC, 6MWD, and quadriceps femoris muscle strength (p > 0.05). The interclass correlation coefficient (ICC) for repeated tests was 0.968 [95% confidence interval (CI): 0.940 to 0.984] for the right limb and 0.968 [95% CI: 0.939 to 0.984] for the left limb in this study. The LCADLtotal (95% CI: 2.10 to 13.71, p = 0.02), the LCADL%total (95% CI: 2.76 to 18.39, p = 0.02), the total score of ABC scale (95% CI: 7.59 to 25.60, p = 0.001), BBS (95% CI: 3.70 to 14.79, p = 0.004), and the CAT (95% CI: 2.80 to 9.33, p = 0.001) were significantly different between the groups. LCADL%total was lower than the cut-off point of 28% in both fallers and non-fallers and the BBS total score was lower than the cut-off point of 52.5 in both fallers and non-fallers ().
Table 1. Demographic and clinical characteristics of groups.
The comparison of the LCADL scale between the groups is shown in . The highest mean score belonged to item 11 (walking upstairs), followed by item 12 (bending), item 3 (putting shoes/socks on), and item 14 (going out socially) in terms of the dyspnoea perception in the groups. However, the mean scores of the LCADL items were not significantly different in fallers compared with non-fallers. Also, there was no significant difference between fallers and non-fallers in terms of the perceived risk of falling during ADLs for items (). There was no difference between fallers and non-fallers in terms of the number of participants who lived alone and the extent to which ADL performance was impaired by dyspnoea (p = 0.62 and p = 0.54, respectively).
Table 2. Comparison of the LCADL scale item scores between groups.
The comparison of the ABC scale item scores between the groups is shown in . The lowest mean scores belonged to item 16 (Walking on icy sidewalks), followed by item 6 (standing on a chair to reach something), item 15 (not holding rails on an escalator), and item 11 (going up and down a ramp). However, the mean scores of item 9 (getting in/out of cars) (p = 0.001), item 11 (up and down slopes) (p = 0.001), item 12 (walk in crowded mall) (p = 0.001), item 13 (walk in crowded mall/bumped) (p = 0.002), item 14 (escalator holding rail) (p = 0.001), and item 15 (escalator not holding the rail) (p = 0.001) were significantly lower in fallers compared with non-fallers ().
Table 3. Comparison of the ABC scale item scores between groups.
In fallers, a strong correlation was found between the LCADL scale item score (dressing the upper body) and the BBS total score (rho = −0.81, p = 0.001). In addition, there was a significant relationship between the LCADLtotal and the BBS total score in all participants (rho = −0.57, p = 0.002). Moderate correlations were found between the LCADL scale item scores (dressing the upper body, washing hair, and walking up stairs) and the BBS total score (rho = −0.67, p = 0.001; rho = −0.58 p = 0.002; and rho = −0.58, p = 0.002, respectively). By contrast, there was no significant correlation between the LCADL scale items and the total score of the ABC scale, except for item 14 (going out socially) (rho = −0.61, p = 0.001) ().
Table 4. Partial correlation between the LCADL scale item scores, LCADL total score and the ABC scale score and BBS score.
Discussion
The present study demonstrated that patients with COPD with or without a history of falling present differences in dyspnoea perception during ADLs in addition to balance and balance confidence despite a similar level of functional capacity and peripheral muscle strength. The balance confidence during ADLs was low in functional mobility-based activities in fallers. Furthermore, the balance confidence during ADLs was low in activities that involve the switching of movements, particularly in the vertical orientation. Although both the BBS and the ABC scales were related to ADLs, the BBS was associated with more single-item scores of the LCADL scale than the ABC scale in patients with COPD with or without falling history.
The LCADL scale is a commonly used tool that comprehensively measures dyspnoea perception in ADLs and explicitly assesses the effect of dyspnoea on ADLs [Citation17]. Therefore, we preferred to evaluate the items of the LCADL scale in terms of the perceived risk of falling. The respiratory activity of the diaphragm and other respiratory muscles is normally interrelated with their other functions, such as for postural control of the trunk. Postural and respiratory activities of the diaphragm may be compromised in situations in which respiratory demand is increased, such as chronic respiratory disease; therefore, the postural activity of the diaphragm is reduced in patients with COPD when respiratory demand increases [Citation29]. A recent study concluded that the reduced contribution of the diaphragm to postural control might increase compensation from the abdominal muscles, with the consequence of reduced efficacy of balance recovery [Citation30]. Although there was a difference between the groups in terms of LCADLtotal, the mean scores of the LCADL items were similar in fallers compared with non-fallers. This could be related to the fact that LCADL%total was lower than the cut-off point of 28% in both fallers and non-fallers because the %total score of LCADL correlated better with clinical outcomes such as mMRC, CAT and airflow obstruction [Citation19]. Therefore, both fallers and non-fallers had better functional outcomes.
Our findings showed that the perceived level of dyspnoea experienced during ADLs was high in fallers compared to non-fallers. Although the combined assessment of COPD does not show a significant difference, most of the patients (80%) were GOLD B to C in fallers. This may have an impact on the increased breathlessness on ADLs in fallers group. The LCADLtotal, the severity of dyspnoea perception while dressing the upper body, washing hair, and walking upstairs were associated with the BBS total score. It has been reported that the BBS is an objective quantitative measure for assessing balance while performing functional activities such as reaching, bending, transferring, and standing, which incorporates most components of postural control [Citation22]. Furthermore, the present study showed that the BBS total score was related to the severity of dyspnoea perception while dressing the upper body in fallers. It is well known that upper extremity movements significantly alter ventilatory and postural muscle recruitment, therefore, affecting the mechanics of the ribcage and abdominal compartments [Citation31]. The functional overload of the diaphragm contributes to the appearance of dyspnoea in patients with COPD [Citation32]. Smith et al. [Citation33] indicated that patients with COPD had increased mediolateral centre pressure displacement both at rest and during ADLs and the deficit in balance involves mediolateral rather than anteroposterior control in COPD patients. A possible explanation may be that mediolateral balance is primarily maintained by trunk movement due to the poor efficiency of the ankle muscles to control balance in this direction. Therefore, increased respiratory demand on the trunk muscles may result in a decreased contribution of the trunk to the maintenance of balance in patients with COPD.
Consistent with previous literature, in our study, confidence in maintaining balance in community-based activities was significantly lower in patients with COPD with a history of falling compared with those with no history of falling. A detailed examination of each activity in the ABC scale indicated that there was a significant difference in balance confidence in terms of the activities related to vertical orientation and activities that involved movement switching in the vertical orientation. Vertical orientation and switching in the vertical orientation, dyspnoea, limited mobility, and muscle weakness are the associated factors that contribute to impaired postural control. Thus, walking and climbing up and down ramps could contribute to the decreased balance confidence in patients with COPD [Citation34, Citation35].
A significant result of this study was that balance and balance confidence decreased, and dyspnoea perception with ADLs increased in patients with COPD with a history of falling compared with patients with COPD with no history of falling. However, the difference in the perceived level of dyspnoea during ADLs, in addition to balance and balance confidence, is a result that needs to be interpreted with caution. This result may indicate that patients with functional balance impairment are more restricted in daily life, regardless of breathlessness, than patients without compromised balance [Citation36]. Furthermore, a recent study demonstrated that there was a negative relationship between impaired balance and low levels of physical activity, which is an important predictor of COPD outcome [Citation3]. It is, therefore, essential to identify activities associated with a decreased balance confidence in relation to participation in daily living tasks, thereby preventing the harmful consequences of COPD, including physical inactivity, peripheral muscle dysfunction, and dyspnoea.
This study has some limitations that should be highlighted. First, considering that LCADL is the most used ADLs scale in chronic respiratory diseases, we prefer to add a 5-point scale to the LCADL for the assessment of the perceived risk of falling. Although we found that the internal consistency of the perceived risk of falling assessment by rating each item of the LCADL was strong (Cronbach’s alpha of 0.95), this scale is not a valid and reliable measurement as yet. Second, the history of falling was asked to the patients for the last year; a prospective observation of the patients in terms of falls may provide better objectivity. Third, this study was based on cross-sectional data collection. Hence, it is difficult to conclude causal relations among the study variables. Lastly, the study sample size was relatively small to detect differences between patients with COPD with a history of falling and age sex matched patients with COPD with no history of falling for most outcomes. However, Bonferroni correction was used to reduce the chances of obtaining type I errors in this study.
To our knowledge, this is the first study to investigate ADLs in relation to falls and balance with a comprehensive design in patients with COPD. The methodologic strength of our research includes that the ABC scale and the BBS were used, which were identified as recommended tools for assessing balance in patients with COPD [Citation8]. These results showed that the BBS was a good clinical measure that reflected the relation between perceived dyspnoea levels while performing ADLs and balance. As a practical implication of this finding, the BBS may provide information about balance status related to ADLs in patients with COPD. It is also known that individuals with COPD have worse static and functional balance in comparison with healthy controls. However, there is no information regarding which daily activities are related to decreased balance confidence in patients with COPD. In our study, we identified daily activities in relation to falls using the LCADL scale, which is a disease-specific scale, to comprehensively measure the dyspnoea perception in ADLs.
Conclusion
This cross-sectional study conducted in patients with COPD with or without falls demonstrates that patients with COPD with increased severity of dyspnoea perception during ADLs appear to have a decreased balance and balance confidence while performing ADLs, regardless of functional capacity and peripheral muscle strength. The balance confidence was low during community-based activities, especially those with vertical orientation and functional mobility in patients with COPD with a history of falling. Moreover, the BBS was associated with more single-item scores of the LCADL scale, which predominantly include upper extremity movements, than the ABC scale in patients with COPD with or without a history of falling. Our study, revealing the relationship between daily life activities and balance and balance confidence should be considered when aiming to increase the level of independence and functional status of patients with COPD through exercise-based pulmonary rehabilitation programs. Future research with larger sample sizes is warranted to explore fall prevention strategies including physical therapy interventions that are targeted at these high-risk activities, home environmental adaptation, and proper use of assisted devices to increase the independence level and functional status of patients with COPD.
Author contribution statements
TB: Literature search, Data collection, Study design, Manuscript preparation, Review of manuscript. EPK: Data collection, Study design, Manuscript preparation, Review of manuscript. BA: Literature search, Analysis of data, Manuscript preparation, Review of manuscript. GKA: Literature search, Study design, Manuscript preparation, Review of manuscript. EK: Study design, Manuscript preparation, Review of manuscript
Ethical statement
Ethical approval for this study was obtained from the Non-invasive Research Ethics Board of Biruni University with a decision number 2018/24-15.
Declaration of Interest
All authors declare no conflicts of interest.
Funding
This research did not receive any specific grant in the public, commercial, or not-for-profit sectors.
References
- Global Strategy for the Diagnosis MaPoC, Global initiative for chronic obstructive lung disease (GOLD). 2020. Revision. Available from: http://www.goldcopd.org. (accessed 24 December, 2020).
- de Castro LA, Ribeiro LR, Mesquita R, et al. Static and functional balance in individuals with COPD: comparison with healthy controls and differences according to sex and disease severity. Respir Care. 2016;61(11):1488–1496. DOI:https://doi.org/10.4187/respcare.04749
- Iwakura M, Okura K, Shibata K, et al. Relationship between balance and physical activity measured by an activity monitor in elderly COPD patients. COPD. 2016;11:1505–1514. DOI:https://doi.org/10.2147/COPD.S107936
- Porto EF, Castro AA, Schmidt VG, et al. Postural control in chronic obstructive pulmonary disease: a systematic review. Int J Chron Obstruct Pulmon Dis. 2015;10:1233–1239. DOI:https://doi.org/10.2147/COPD.S63955
- Crişan AF, Oancea C, Timar B, et al. Balance impairment in patients with COPD. PLoS One. 2015;10(3):e0120573. DOI:https://doi.org/10.1371/journal.pone.0120573
- Porto EF, Pradella CO, Rocco CM, et al. Comparative postural control in COPD patients and healthy individuals during dynamic and static activities. J Cardiopulm Rehabil Prev. 2017;37(2):139–145. DOI:https://doi.org/10.1097/HCR.0000000000000246
- Roig M, Eng JJ, MacIntyre DL, et al. Falls in people with chronic obstructive pulmonary disease: an observational cohort study. Respir Med. 2011;105(3):461–469. DOI:https://doi.org/10.1016/j.rmed.2010.08.015
- Oliveira CC, Lee A, Granger CL, Miller KJ, et al. Postural control and fear of falling assessment in people with chronic obstructive pulmonary disease: a systematic review of instruments, international classification of functioning, disability and health linkage, and measurement properties. Arch Phys Med Rehabil. 2013;94(9):1784–1799. DOI:https://doi.org/10.1016/j.apmr.2013.04.012
- Beauchamp MK, Hill K, Goldstein RS, et al. Impairments in balance discriminate fallers from non-fallers in COPD. Respir Med. 2009;103(12):1885–1891. DOI:https://doi.org/10.1016/j.rmed.2009.06.008
- Paes T, Machado FVC, Cavalheri V, et al. Multitask protocols to evaluate activities of daily living performance in people with COPD: a systematic review. Expert Rev Respir Med. 2017;11(7):581–590. DOI:https://doi.org/10.1080/17476348.2017.1335198
- Ozsoy I, Ozcan Kahraman B, Acar S, et al. Factors influencing activities of daily living in subjects with COPD. Respir Care. 2019;64(2):189–195. DOI:https://doi.org/10.4187/respcare.05938
- Beauchamp MK, Harrison SL, Goldstein RS, et al. Interpretability of change scores in measures of balance in people with COPD. Chest. 2016;149(3):696–703. DOI:https://doi.org/10.1378/chest.15-0717
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. DOI:https://doi.org/10.1016/0021-9681(87)90171-8
- Bestall JC, Paul EA, Garrod R, et al. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586. DOI:https://doi.org/10.1136/thx.54.7.581
- Jones P, Harding G, Berry P, et al. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34(3):648–654. DOI:https://doi.org/10.1183/09031936.00102509
- Yorgancıoğlu A, Polatlı M, Aydemir Ö, et al. Reliability and validity of Turkish version of COPD assessment test. Tuberk Toraks. 2012;60:314–320.
- Garrod R, Bestall JC, Paul EA, et al. Development and validation of a standardized measure of activity of daily living in patients with severe COPD: the London Chest Activity of Daily Living scale (LCADL). Respir Med. 2000;94(6):589–596. DOI:https://doi.org/10.1053/rmed.2000.0786
- Saka S, Savcı S, Kütükcü EC, et al. Validity and reliability of the Turkish version of the London chest activity of daily living scale in obstructive lung diseases. Turk Thorac J. 2020;21:116–121.
- Gulart AA, Munari AB, Klein SR, et al. The London Chest Activity of Daily Living scale cut-off point to discriminate functional status in patients with chronic obstructive pulmonary disease. Braz J Phys Ther. 2020;24(3):264–272. DOI:https://doi.org/10.1016/j.bjpt.2019.03.002
- Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) scale. J Gerontol A Biol Sci Med Sci. 1995;50A(1):M28–34. DOI:https://doi.org/10.1093/gerona/50a.1.m28
- Ayhan C, Büyükturan Ö, Kırdı N, et al. The Turkish version of the activities specific balance confidence (ABC) scale: Its cultural adaptation, validation and reliability in older adults. Turk J Geriatr. 2014;17(2):157–163.
- Berg KO, Maki BE, Williams JI, et al. Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil. 1992;73(11):1073–1080.
- Sahin F, Yılmaz F, Ozmaden A, et al. Reliability and validity of the Turkish version of the Berg Balance Scale, J Geriatr Phys Ther. 2008;31:32–37.
- Jácome C, Cruz J, Oliveira A, et al. Validity, reliability, and ability to identify fall status of the Berg Balance Scale, BESTest, Mini-BESTest, and Brief-BESTest in patients with COPD. Phys Ther. 2016;96(11):1807–1815. DOI:https://doi.org/10.2522/ptj.20150391
- Laboratories ACoPSfCPF. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–117.
- Holland AE, Hill CJ, Rasekaba T, et al. Updating the minimal important difference for six-minute walk distance in patients with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2010;91(2):221–225. DOI:https://doi.org/10.1016/j.apmr.2009.10.017
- O’Shea SD, Taylor NF, Paratz JD. Measuring muscle strength for people with chronic obstructive pulmonary disease: retest reliability of hand-held dynamometry. Arch Phys Med Rehabil. 2007;88(1):32–36. DOI:https://doi.org/10.1016/j.apmr.2006.10.002
- Hinkle DE, Wiersma W, Jurs SG. Applied statistics for the behavioral sciences. Boston: Houghton Mifflin Company; 1988.
- Hodges PW, Heijnen I, Gandevia SC. Postural activity of the diaphragm is reduced in humans when respiratory demand increases. J Physiol. 2001;537(Pt 3):999–1008. DOI:https://doi.org/10.1111/j.1469-7793.2001.00999.x
- Smith MD, Chang AT, Hodges PW. Balance recovery is compromised and trunk muscle activity is increased in chronic obstructive pulmonary disease. Gait Posture. 2016;43:101–107. DOI:https://doi.org/10.1016/j.gaitpost.2015.09.004
- Cerny FJ, Ucer C. Arm work interferes with normal ventilation. Appl Ergon. 2004;35(5):411–415. DOI:https://doi.org/10.1016/j.apergo.2004.05.001
- Ottenheijm CA, Heunks LM, Dekhuijzen PR. Diaphragm muscle fiber dysfunction in chronic obstructive pulmonary disease: toward a pathophysiological concept. Am J Respir Crit Care Med. 2007;175(12):1233–1240. DOI:https://doi.org/10.1164/rccm.200701-020PP
- Smith MD, Chang AT, Seale HE, et al. Balance is impaired in people with chronic obstructive pulmonary disease. Gait Posture. 2010;31(4):456–460. DOI:https://doi.org/10.1016/j.gaitpost.2010.01.022
- Butcher SJ, Meshke JM, Sheppard MS. Reductions in functional balance, coordination, and mobility measures among patients with stable chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 2004;24(4):274–280. DOI:https://doi.org/10.1097/00008483-200407000-00013
- Tudorache E, Oancea C, Avram C, et al. Balance impairment and systemic inflammation in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;10:1847–1852.
- Cruz J, Marques A, Jacome C, et al. Global functioning of COPD patients with and without functional balance impairment: an exploratory analysis based on the ICF framework. COPD. 2015;12(2):207–216. DOI:https://doi.org/10.3109/15412555.2014.933793
Appendix
LONDON CHEST ACTIVITY OF DAILY LIVING SCALE
NAME:
DATE OF BIRTH:
DO YOU LIVE ALONE? YES □ NO □
How much does your breathing affect you in your normal activities of daily living?
A lot □ A Little □ Not at all □