Abstract
The Glittre ADL-test (TGlittre) is a multiple-task test designed to assess functional limitation in patients with chronic obstructive pulmonary disease (COPD). Although few studies have investigated the TGlittre learning effect, the results are still conflicting. This study aimed to investigate the test-retest reliability and learning effect on TGlittre and to identify predicting factors of the learning effect in patients with COPD. Patients performed the TGlittre twice with a 30-minutes resting period between trials. TGlittre consists in measuring the time to complete five laps of a multiple ADL-like activities circuit: walking stairs, carrying a backpack, lifting objects, bending down and rising from a seated position. 124 patients with COPD were assessed [81 men; 66 ± 8 years, forced expiratory volume in one second (FEV1) 37.1 ± 15.0%pred; TGlittre 120 ± 60%pred; six-minute walking test 75.5 ± 17.4%pred]. The time spent in TGlittre presented excellent reliability (ICC = 0.96; 95%CI 0.92 − 0.98; p < 0.001; SEM 0.46 min; MDC 1.28 min) and decreased in the retest (5.24 ± 2.31 min to 4.85 ± 2.02 min; p < 0.001). Patients presented a learning effect of 6.11 ± 11.1% in TGlittre. A lower FEV1 (r2=0.10; p < 0.001) and a worse performance in the first TGlittre (r2=0.28; p < 0.001) are related to the improvement in performance of the second TGlittre. Although the TGlittre is reliable, patients improve their performance when performing the second test probably because they underestimate their functional capacity. These results should encourage professionals to assess TGlittre twice when using this test as an outcome measure.
Introduction
Patients with chronic obstructive pulmonary disease (COPD) commonly present limitation in performing activities of daily living (ADL), and this limitation is associated with poorer quality of life [Citation1], higher frequency of exacerbations and hospitalizations [Citation2] and increased mortality [Citation3]. Daily activities other than walking, such as lifting, picking up objects, climbing stair, and others, are often perceived as problematic by patients with COPD and their caregivers [Citation4, Citation5]. Therefore, adequate assessment of function limitation is a key issue for understanding the impact of COPD on patient’s life, designing interventions, evaluating disease progression and interventions’ effectiveness [Citation5, Citation6].
Field tests are assessment tools capable of objectively assessing patient functional capacity in common daily tasks [Citation6]. There are several valid tests for patients with COPD, and it is recommended to use those with well-established measurement properties and interpretation criteria [Citation7]. The six-minute walking test (6MWT) is one of the most popular tests to assess functional capacity, presenting well-established measurement properties. This test has high test-retest reliability and the need to perform two tests on patients with chronic respiratory diseases is already well established in the literature, due to the learning effect [Citation8]. However, the 6MWT does not assess other ADL than walking, as well other field tests, in general, only assess one domain of ADL, mostly focusing on lower limbs activities [Citation5].
In this sense, the Glittre-ADL test (TGlittre) was developed as a multiple-task test that requires upper and lower limbs in a set of ADL-like activities known to be difficult for patients with COPD [Citation9]. The TGlittre is valid [Citation9] and reliable for assessing the functional capacity of both clinically stable [Citation9–11] and hospitalized patients [Citation12], it is able to differentiate functional capacity of patients with COPD from healthy subjects [Citation13], it is responsive to pulmonary rehabilitation [Citation9, Citation14] with a known minimal important difference [Citation14]. In addition, TGlittre is associated with other tools for assessing functional [Citation9, Citation15, Citation16] and health status [Citation17] of patients with COPD. Previous studies investigated the test-retest reliability of the TGlittre in patients with COPD [Citation9–12, Citation14], with three of them reporting an intraclass correlation coefficient (ICC) ranging from 0.91 to 0.98 [Citation10,Citation12,Citation14]. However, there is still no consensus on the need to apply the TGlittre more than once when using this test as an outcome measure. Since TGlittre involves a set of different and more complex activities, it is expected to exist an important learning effect when performing the test more than once. The test-retest reliability and the learning effect of a test must be identified to ensure trustworthy outcomes. Thus, we can safely assume that the differences assessed are the result of interventions or the evolution of the patient, and not the variability inherent in the test.
In this sense, the current study aimed to investigate the relative and absolute test-retest reliability and the learning effect of the TGlittre, as well as identifying the predicting factors of the learning effect in patients with COPD. As a secondary aim, we compared the learning effect of both TGlittre and 6MWT.
Methods
Study population
This study included a convenience sample of patients with COPD (stages 2 to 4 of airflow obstruction)[Citation18], referred to pulmonary rehabilitation program of the Center for Assistance, Teaching and Research in Pulmonary Rehabilitation from the Universidade do Estado de Santa Catarina (NuReab-UDESC) and of the Research Group on Cardiopulmonary Interaction from the Universidade Federal de Ciências da Saúde de Porto Alegre (GPIC-UFCSPA) from August 2013 to December 2019. Participants must have presented clinical stability in the four weeks prior to the study protocol, age ≥ 40 years and not have engaging in any exercise training program at least six months before participating in the study. Patients were excluded when presenting any pulmonary disease other than COPD, current smoking, comorbidities such as heart failure, peripheral arterial disease, and self-reported significant cardiovascular events, or other comorbidities (neurological and orthopaedical) that would compromise the ability to perform any of the study assessments. The present analyses also retrieved data collected at baseline of a previous study of our research group [Citation14].
Expecting an ICC ranging from 0.7 to 0.9, and considering a two-tailed significance level of 5% and a power of 80%, at least 23 participants would be necessary for the test-retest reliability analysis [Citation19]. To investigate the predicting factors of the learning effect, expecting a r2 ≥ 0.1, and considering a two-tailed significance level of 5% and a power of 80%, 76 participants would be needed. Still, we have chosen to present Cohen’s d effect size and calculation of statistical power (1- β).
Study protocol
Participants underwent lung function assessment and, on two separate days, TGlittre and 6MWT. Lung function was assessed with spirometry in accordance with the American Thoracic Society (ATS)/European Respiratory Society (ERS) standardisation [Citation20]. Dyspnea on exertion was assessed by the modified Medical Research Council scale (mMRC) [Citation21].
The TGlittre was performed according to the protocol validated by Skumlien et al. [Citation9], which consists in performing, in the shortest possible time, five laps of a standardized circuit arranged in a 10-m corridor, carrying a backpack (2.5 kg for women and 5.0 kg for men). From the seated position, the subject stands up and walks along a flat corridor, in the middle of which there is a two-step staircase (each step 17 cm high × 27 cm deep) to be climbed up and down. At the end of the corridor, the subject moves three one-kg objects, positioned on a shelf (shoulders’ height), one by one, to another shelf (waist’s height) and then to the floor. Then the objects are placed back on the lower shelf, and finally returned to the upper shelf. The subject returns, in the reverse course, to the initial sitting position. Immediately after sitting down, another lap must be started, following the same circuit [Citation9]. Arterial blood pressure, heart rate (HR), pulse oxyhemoglobin saturation (SpO2) and dyspnea (Borg CR10 scale) [Citation22] were measured at the beginning and at the end of the test. Two tests were performed, with a minimum interval of 30 min or until the vital signs and symptoms returned to baseline. Predicted values for the time to perform the TGlittre were calculated according to Reis et al [Citation23]. Values over 100% of the predicted mean that the subject takes more time to complete the test then the expected. The minimal important difference of −0.38 min was considered [Citation14].
The 6MWT was performed as recommended by the ATS/ERS [Citation8]. Two tests were performed, with a minimum interval of 30 min or until the vital signs and symptoms returned to baseline. At UDESC, the test was performed at a 20-meter [Citation24] aisle and at UFCSPA it was performed at a 30-meter aisle. Before the test, patients were instructed to walk as far as possible, with standardized verbal encouragement every minute. Arterial blood pressure, HR, SpO2 and dyspnea were measured at the beginning and at end of the test. Predicted values for walking distance were calculated according to the equation 1 proposed by Britto et al [Citation25].
This study was approved by the Ethics Committee on Human Research at UDESC (Florianópolis, Santa Catarina, Brazil), UFCSPA (Porto Alegre, Rio Grande do Sul, Brazil), and Irmandade da Santa Casa de Misericórdia de Porto Alegre (Porto Alegre, Rio Grande do Sul, Brazil) (protocol numbers 80831117.5.0000.0118, 1.413.342 and 836.248, respectively). All participants signed the consent form.
Data analysis
Results are presented as mean and standard deviation or median and 25th – 75th percentiles, according to the data distribution checked with the Shapiro-Wilk test. Differences between the first and second TGlittre and 6MWT were compared using a paired t-test and the Cohen’s d effect size was calculated [Citation26]. The effect size was considered large (d > 0.80), medium (d > 0.50), small (d ≥ 0.20) or null (d < 0.20) [Citation26]. The relative test-retest reliability of both tests was evaluated using the ICC [Citation27], considering two-way mixed-effects model, absolute agreement, and average measures. Based on the 95% confident interval of the ICC estimate, reliability was classified as poor (ICC < 0.50), moderate (ICC = 0.50 − 0.74), good (ICC = 0.75 − 0.90) and excellent (ICC > 0.90) [Citation28]. The Standard Error of Measurement (SEM) was used as the absolute test-retest reliability measure [Citation27]. The SEM was calculated using the formula [SEM = SD x √ (1 - ICC)], where SD is the standard deviation of the first trial. The minimal detectable change (MDC) was calculated with the formula [MDC = 1.96 x √2 x SEM] [Citation29]. The consistency between the first and second tests were evaluated using Bland-Altman analysis. Due the difference in track length between participating centers, the ICC for the 6MWT of each center was also calculated separately and the absolute and percentual change from the first to the second 6MWT was compared with t-test for independent samples to investigate if the length did not bias the current results. To compare the percentage difference between the first and second TGlittre and 6MWT, the percentage of change on TGlittre was multiplied by −1 then the percentages of change were compared with paired t-test. The changes in HR, SpO2, mean arterial blood pressure (MAP) and dyspnea from the beginning and the end of each test were compared with Wilcoxon test. The associations between the change in time to complete the TGlittre (ΔTGlittre: second test minus first test) and the independent variables (lung function, TGlittre, 6MWT, Δ6MWT: the change between the first and second 6MWT, and the change in HR, SpO2, MAP and dyspnea during the first TGlittre) were analyzed with Pearson correlation test and simple linear regression analysis. The association between TGlittre and 6MWT was also tested with Pearson correlation test. Correlations were considered very weak (r < 0.3), weak (0.3 t 0.49), moderate (0.5 − 0.69), strong (0.7 − 0.89) or very strong (r > 0.9) [Citation30]. Finally, participants were divided in three groups according to severity of airflow obstruction (GOLD stages 2, 3 and 4), then ΔTGlittre and Δ6MWT were compared between groups with GLM and Bonferroni post hoc. The level of significance was set at <0.05 for all statistical tests. Statistical analysis was performed with the SPSS software, version 22.0 (IBM Corporation, Armonk, NY, USA) and the GraphPad Prism software, version 6.0 (GraphPad Inc., San Diego, CA, USA).
Results
A total of 124 patients participated in the study and all performed both TGlittre and 6MWT twice. From those, 81 (65.3%) were from NuReab-UDESC and 43 (34.7%) were from GPIC-UFCSPA. Participants characteristics are described in .
Table 1. Subjects characteristics.
The TGlittre presented excellent test-retest reliability between the first and the second test (), with an ICC = 0.96 (95%CI 0.92 − 0.98; p < 0.001); SEM = of 0.46 min and MDC = 1.28 min. Ninety-eight patients (79%) had a better performance on the second test. In fact, 42.7% of the participants presented a reduction in the time to perform the second test ≥0.38 min. The mean learning effect on TGlittre was −6.11 ± 11.1% (Cohen’s d = 0.18), which is equivalent to a reduction of 24 s on the time taken to perform the second TGlittre. In addition, the mean of the best performances on TGlittre was better than the first test (). The Bland-Altman plot confirmed that most patients showed better performance in the second TGlittre and that patients with better performance in the TGlittre presented greater difference between the two TGlittre ().
Figure 1. Test-retest reliability of Glittre-ADL test and six-minute walking test. A: Scatter plot of first and second Glittre-ADL test (TGlittre). The dashed line shows the line of identity. The bold line is the regression of the second test to the first, with most points under the line of identity (β < 0.01). B: Bland-Altman plot of the difference between the ΔTGlittre (second test – first test) plotted against the mean value of TGlittre performance. The upper dashed line is the upper limit of agreement (ULA = 1.07 min), the lower dashed line is the lower limit of agreement (LLA = 1.85 min) and the dashed line in the middle is the mean ΔTGlittre = -0.39 min. The bold gray line is the regression of ΔTGlittre against mean value, indicating that those who took longer time to complete the test tended to improve more on the second test (r2 = 0.16; p < 0.001). C: Scatter plot of first and second six-minute walking test (6MWT). The dashed line shows the line of identity. The bold line is the regression of the second test to the first, with most points close to the line of identity (β < 0.01). D: Bland-Altman plot of the difference between the Δ6MWT (second test – first test) plotted against the mean value of 6MWT performance. The upper dashed line is the upper limit of agreement (ULA = 79.9 m), the lower dashed line is the lower limit of agreement (LLA = -55.5 m) and the dashed line in the middle is the mean Δ6MWT = 12.2 m. The bold gray line is the regression of Δ6MWT against mean value, indicating no association between the test performance and the improvement in the second test (r2 = 0.006; p = 0.401).
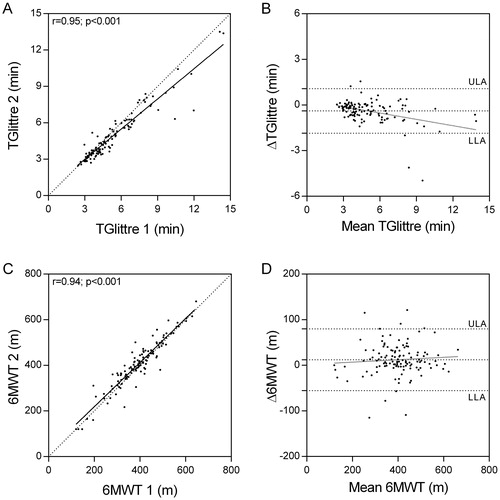
Table 2. Glittre-ADL test and six-minute walking test results.
When analyzing the sample of both centers separately, at UDESC the 6MWT presented excellent test-retest reliability, with an ICC = 0.96 (95%CI 0.94 − 0.98; p < 0.001), as well as at UFCSPA (ICC = 0.97; 95%CI 0.93 − 0.98; p < 0.001). The sample of both centers presented similar learning effect in the second 6MWT (UDESC: 3.34 ± 9.97% vs. UFCSPA: 3.72 ± 11.9%; p = 0.852; Cohen’s d = 0.03). When analyzing the sample of both centers together, the 6MWT also presented excellent test-retest reliability (), with an ICC = 0.97 (95%CI 0.95 − 0.98; p < 0.001); SEM = 17.3 m and MDC = 47.8 m, with a learning effect of 3.48 ± 10.7% (Cohen’s d = 0.12) (). Two (1.6%) participants presented similar performance on both 6MWT, while 83 (66.9%) had a better performance on the second test. The percentage of change between the first and the second test was not significantly different between TGlittre and 6MWT (TGlittre: 6.11 ± 11.1% vs. 6MWT: 3.48 ± 10.7%; p = 0.052; β = 0.24). The Bland-Altman plot confirmed that most patients showed better performance in the second 6MWT. However, there was no association between mean distance walked in the 6MWT with the difference between the two 6MWT ().
The first and the second test induced the same magnitude of physiological change in vital signs and in dyspnea for TGlittre and 6MWT. However, participants presented a slightly higher desaturation on the second test for both TGlittre and 6MWT (). It is important to point out that there were no differences in vital signs and dyspnea in resting conditions at the beginning of the first and the second of both tests (p > 0.05; data not shown).
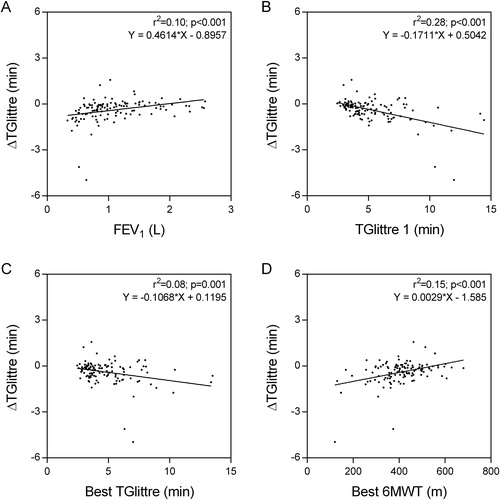
The performance on TGlittre correlated with the performance on 6MWT (r = −0.75; p < 0.001; β < 0.01), but the ΔTGlittre did not correlate with Δ6MWT (r = −0.02; p = 0.8). A longer average time to complete both trials of TGlittre was associated with greater learning effect on TGlittre (). This association was not found on 6MWT (). Also, participants with more severe airway obstruction (), worse performance on the first TGlittre (), on the best TGlittre (), and on the best 6MWT (), tended to present a greater reduction in the time to complete the second TGlittre. In addition, the delta in SpO2 (ΔSpO2) in the first TGlittre presented a very weak correlation with ΔTGlittre (r = −0.25; p = 0.006; β = 0.21). No other correlation was found between ΔTGlittre and the change in vital sings and dyspnea during the tests (p > 0.05).
Figure 2. Associations of the learning effect of the Glittre-ADL test with A) forced expiratory volume in one second (FEV1), β = 0.05; B) the performance on the first Glittre-ADL test (TGlittre 1), β < 0.01; C) the best performance on Glittre-ADL test (Best TGlittre), β = 0.11; and D) the best performance on six-minute walking test (Best 6MWT), β < 0.01.
Patients with very severe airflow obstruction (GOLD 4), presented greater ΔTGlittre (-0.66 ± 0.98 min) when compared to patients with moderate (GOLD 2; −0.17 ± 0.42 min; p = 0.016) and severe (GOLD 3; −0.26 ± 0.53 min; p = 0.026) airflow obstruction (β = 0.43 for the GLM analysis). There was no difference between patients with moderate and severe airflow obstruction (p > 0.05). No statistically significant difference was found between groups regarding the Δ6MWT (19.3 ± 33 m, 17.2 ± 25.8 m, and 2.77 ± 41.3 m for GOLD 2, 3 and 4, respectively; p = 0.057).
Discussion
The current results showed that the TGlittre demonstrates excellent relative test-retest reliability, however presenting a statistically significant learning effect associated with worse airflow obstruction and worse performance in the first TGlittre and on the best 6MWT. Both TGlittre and 6MWT presented similar learning effect, but the changes from the first tests to the second tests (ΔTGlittre and Δ6MWT) were not associated.
Previous studies have reported the test-retest reliability of the TGlittre in patients with COPD, but with conflicting findings about the learning effect. When TGlittre was first described, Skumlien et al. [Citation9] showed a learning effect of 7% (average reduction of 0.37 min on the second test) when the TGlittre was performed in two consecutive days. Further, Tufanin et al. [Citation11] did not find any significant difference between the two tests performed on the same day with a 30-minute interval. José and Dal Corso [Citation12] performed two TGlittre on the same day in hospitalized patients with exacerbation of chronic respiratory diseases, including COPD, and also found high test-retest reliability (ICC: 0.91), however with a greater learning effect (17%). Corroborating our findings, they also found similar values for HR, SpO2 and dyspnea in both TGlittre. When analyzing only the COPD patients (n = 16), the test was less reliable (ICC: 0.75), with a mean reduction of 1.28 min or approximately 20%. Still, the study from dos Santos et al. [Citation10] found a good test-retest reliability (ICC: 0.97) when performing TGlittre twice on the same day, with a learning effect of 6.34%, which was equivalent to a reduction averaging 0.34 min on the second test. Also, the results suggest that patients who perform the first TGlittre in a longer time tend to present a greater reduction in the time to perform the second test, corroborating the current findings. However, in that study, patients performed the TGlittre wearing a face mask, which could have influenced the performance in the test, as well as the test reliability. At last, a previous study of our research group [Citation14] also found a high test-retest reliability of TGlittre (ICC: 0.95), with a learning effect of 7.6% and, moreover, the learning effect reduced to 4.6% after a pulmonary rehabilitation program. In addition, the study showed a MDC of 1.05 min, which is smaller than the one found in the current study and a minimal important difference for TGlittre of −0.38 min (the SEM was considered the minimal important difference), which is similar to the average learning effect of −0.39 ± 0.74 min found in the current study. Furthermore, in the current sample, very severe patients presented a learning effect even higher than the minimal important difference.
Based on that, we raise the importance to perform the TGlittre twice to ensure reliable outcomes when using this test as an outcome measure, even though this learning effect had a null effect size (Cohen’s d < 0.2). This practice will avoid misinterpretations between the result of interventions with the variability of the test. In addition, a single test may underestimate the functional status of patients, especially in those with more severe disease. However, it is important to point out that the TGlittre’s learning effect may vary with the population. Healthy subjects present a learning effect of 5.3% when performing the second TGlittre [Citation23], while obese and post-bariatric surgery subjects present a learning effect of 11.5 − 11.8% [Citation31].
The current study showed a reduction of approximately 6% in the time to perform the second TGlittre. In general, participants with worse lung function and worse functional capacity, both assessed by TGlittre and 6MWT, but especially in the first TGlittre, tended to have a greater reduction in the time to perform the second test. Based on the current findings, the FEV1 can explain only 10% of the change in the time to perform the second TGlittre. This weak association corroborates the evidence that suggests that FEV1 is a relatively poor correlate of the impact of COPD on daily life [Citation32]. Meanwhile, the performance in the first TGlittre explains 28% (moderate association) of the change in the time to perform the second test. A previous study observed similar behavior in the 6MWT performed in two consecutive days, in which a distance ≤350 m in the first test was a determining factor for a clinically significant improvement (greater than 42 m) in the second test [Citation33]. A possible explanation may be that more functionally impaired patients do not perform the first test at their maximum capacity once those patients also presented less desaturation in the first TGlittre. Besides, dyspnea, HR and arterial blood pressure behavior were not associated with the improvement in the second test. Thus, after experiencing the first test, those patients may feel more secure and motivated to perform the second one. Controversially, Sciurba et al. [Citation34] observed that patients with greater distance walked on the first 6MWT tended to improve more on the second test. However, the authors only included severe and very severe patients and as shown by the current results, very severe patients presented a greater variability of learning effect on both tests.
The above-mentioned studies [Citation33, Citation34] found a learning effect of 7% in the second 6MWT, which is a higher learning effect than the one found in the current study. Although both studies have representative samples, it is important to point out that those studies used different course layouts (triangular, oval, circular and straight with different lengths) and the tests were performed in separate days, which might have influenced the learning effect. In the current study, all 6MWT were performed in a straight-course layout and tests were performed on the same day, and, as expected [Citation24], the length of the course did not influence the test-retest reliability and the learning effect.
On the other hand, the 6MWT learning effect found in the current study was not statistically different from the one found for the TGlittre. Still, there was a tendency of a smaller learning effect on the 6MWT, which was expected since TGlittre involves multiple tasks requiring different motor skills. This fact may explain the lack of association between ΔTGlittre and Δ6MWT. However, the comparison of the learning effect between TGlittre and 6MWT was not powered enough, thus it should be considered as a secondary outcome. Anyway, it is important to clarify that to compare the learning effects of both tests, it was necessary to multiply the percentage of change between the two TGlittre by −1, since an improvement in this test means a reduction in the time to perform the test, while an improvement in the 6MWT means an increase in the distance walked.
Although other authors have already studied the test-retest reliability of the TGlittre, our study brings several aspects that strengthen the evidence regarding the learning effect of TGlittre and the need to assess this test more than once. First, the current study has enough statistical power to confirm the difference between the first and the second TGlittre and 6MWT (β = 0.01 and 0.04, respectively). Secondly, we described not only average data for learning effect, but also limits of agreement between assessments as well as an ICC. Thirdly, up to our knowledge, it was the first study that aimed to identify the predicting factors for the TGlittre learning effect. Nevertheless, our study presents some limitations. First, our sample did not include subjects with mild airflow obstruction (GOLD 1), which may impair the representativeness of the COPD population. Still, patients with mild COPD are generally underdiagnosed, so the application of the TGlittre is less frequent. Secondly, the tests were not always executed by the same supervisor. However, all supervisors were strongly familiarized with the tests’ standardization. Thirdly, we acknowledge that participants may be more familiarized with the 6MWT, which is a more popular test in the clinical practice, than with the TGlittre. In addition, the length of the walking course of the 6MWT was different between the two participating centers. Notwithstanding, both centers presented excellent test-retest reliability for the 6MWT and no statistical differences in the learning effect between centers were found. Fourthly, some variables that could have influenced the improvement of the second TGlittre were not studied, such as leg fatigue during the tests, participants’ balance and muscle strength. Finally, the sample size may have been insufficient for the secondary analyzes of comparison between the GOLD classifications and for the comparison of the learning effect between TGlittre and the 6MWT, since the statistical power was below 80%. Therefore, these results should be interpreted with caution.
Conclusion
In summary, although the TGlittre is reliable, there is a statistically significant improvement, averaging 6% when the test is repeated a second time on the same day. Patients improve their performance on the second test probably because they underestimate their functional capacity. These results should encourage professionals to assess TGlittre twice when using this test as an outcome measure.
Diclosure of interest
No potential conflict of interest was reported by the author(s).
Acknowledgements
The authors would like to thank those who supported the data acquisition, to the Irmandade da Santa Casa de Misericórdia de Porto Alegre, to all the pulmonologists who referred their patients to the study protocol, to the Coordenação de Aperfeiçoamento de Pessoal de Ensino Superior (CAPES/Brazil), to the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq/Brazil) and to the Fundação de Amparo à Pesquisa e Inovação do Estado de Santa Catarina (FAPESC/Brazil).
Additional information
Funding
References
- Dechman G, Scherer SA. Outcome measures in cardiopulmonary physical therapy: Focus on the Glittre ADL-Test for people with chronic obstructive pulmonary disease. Cardiopulm Phys Ther J. 2008;19:115–118.
- Pitta F, Troosters T, Probst VS, et al. Physical activity and hospitalization for exacerbation of COPD. Chest. 2006;129:536–544. DOI:10.1378/chest.129.3.536
- Garcia-Aymerich J, Lange P, Benet M, et al. Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population based cohort study. Thorax. 2006;61(9):772–778. DOI:10.1136/thx.2006.060145
- Nakken N, Janssen DJA, van den Bogaart EHA, et al. Patient versus proxy-reported problematic activities of daily life in patients with COPD. Respirology. 2017;22:307–314. DOI:10.1111/resp.12915
- Bui KL, Nyberg A, Maltais F, et al. Functional tests in chronic obstructive pulmonary disease, Part 1: Clinical relevance and links to the international classification of functioning, disability, and health. Ann Am Thorac Soc. 2017;14:778–784.
- Spruit MA, Singh SJ, Garvey C, et al. An official american thoracic society/european respiratory society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13-64–e64. DOI:10.1164/rccm.201309-1634ST
- Singh SJ, Puhan MA, Andrianopoulos V, et al. An official systematic review of the European Respiratory Society/American Thoracic Society: Measurement properties of field walking tests in chronic respiratory disease. Eur Respir J. 2014;44:1447–1478. DOI:10.1183/09031936.00150414
- Holland AE, Spruit MA, Troosters T, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014;44:1428–1446. DOI:10.1183/09031936.00150314
- Skumlien S, Hagelund T, Bjortuft O, et al. A field test of functional status as performance of activities of daily living in COPD patients. Respir Med. 2006;100(2):316–323. DOI:10.1016/j.rmed.2005.04.022
- dos Santos K, Gulart AA, Munari AB, et al. Reproducibility of Ventilatory parameters, dynamic hyperinflation, and performance in the glittre-ADL Test in COPD Patients. COPD J Chronic Obstr Pulm Dis. 2016;13(6):700–705. DOI:10.1080/15412555.2016.1177007
- Tufanin A, Souza GF, Tisi GR, et al. Cardiac, ventilatory, and metabolic adjustments in chronic obstructive pulmonary disease patients during the performance of Glittre activities of daily living test. Chron Respir Dis. 2014;11:247–255. DOI:10.1177/1479972314552805
- José A, Dal Corso S. Reproducibility of the six-minute walk test and Glittre ADL-test in patients hospitalized for acute and exacerbated chronic lung disease. Braz J Phys Ther. 2015;19(3):235–242. DOI:10.1590/bjpt-rbf.2014.0092
- Corrêa KS, Karloh M, Martins LQ, et al. Can the Glittre ADL test differentiate the functional capacity of COPD patients from that of healthy subjects? Rev Bras Fisioter. 2011;15(6):467–473. DOI:10.1590/S1413-35552011005000034
- Gulart AA, Araujo CLP, de Munari AB, et al. The minimal important difference for Glittre-ADL test in patients with chronic obstructive pulmonary disease. Brazilian J Phys Ther. 2020;24:54–60. DOI:10.1016/j.bjpt.2018.11.009
- Karloh M, Karsten M, Pissaia FV, et al. Physiological responses to the Glittre-ADL test in patients with chronic obstructive pulmonary disease. J Rehabil Med. 2014;46(1):88–94. DOI:10.2340/16501977-1217
- Karloh M, Araujo CLP, Gulart AA, et al. The Glittre-ADL test reflects functional performance measured by physical activities of daily living in patients with chronic obstructive pulmonary disease. Braz J Phys Ther. 2016;20(3):223–230. DOI:10.1590/bjpt-rbf.2014.0155
- Gulart AA, Munari AB, Queiroz AD, et al. Does the COPD assessment test reflect functional status in patients with COPD. Chron Respir Dis. 2017;14(1):37–44. DOI:10.1177/1479972316661924
- Agarwal R, Chakrabarti A, Denning DW, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. COPD J Chronic Obstr Pulm Dis. 2020;1:105–141.
- Bonett DG. Sample size requirements for estimating intraclass correlations with desired precision. Stat Med. 2002;21:1331–1335.
- Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. DOI:10.1183/09031936.05.00034805
- Kovelis D, Segretti NO, Probst VS, et al. Validation of the modified pulmonary functional status and dyspnea questionnaire and the medical research council scale for use in Brazilian patients with chronic obstructive pulmonary disease. J Bras Pneumol. 2008;34(12):1008–1018. DOI:10.1590/S1806-37132008001200005
- Borg GA. Psychophysical bases of perceived exertion. Med Sci Sport Exerc. 1982;14:377–381.
- dos RC, Karloh M, Fonseca FR, et al. Functional capacity measurement: reference equations for the Glittre Activities of Daily Living test. J Bras Pneumol. 2018;44:370–377.
- Klein SR, Gulart AA, Venâncio RS, et al. Performance difference on the six-minute walk test on tracks of 20 and 30 meters for patients with chronic obstructive pulmonary disease: validity and reliability. Brazilian J Phys Ther. 2020;25:40–47.
- Britto RR, Probst VS, de Andrade AFD, et al. Reference equations for the six-minute walk distance based on a Brazilian multicenter study. Braz J Phys Ther. 2013;17(6):556–563. DOI:10.1590/S1413-35552012005000122
- Cohen J. Statistical power analysis for the behavioural sciences. Hillside. NJ Lawrence Earlbaum Assoc.;1988.
- Bruton A, Conway JH, Holgate ST. Reliability: What is it, and how is it measured? Physiotherapy. 2000;86(2):94–99. DOI:10.1016/S0031-9406(05)61211-4
- Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. DOI:10.1016/j.jcm.2016.02.012
- Walton D, Macdermid J, Nielson W, et al. Reliability, standard error, and minimum detectable change of clinical pressure pain threshold testing in people with and without acute neck pain. J Orthop Sports Phys Ther. 2011;41(9):644–650. DOI:10.2519/jospt.2011.3666
- Mukaka MM. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24:69–71.
- Monteiro F, Ponce DAN, Silva H, et al. Validity and reproducibility of the Glittre ADL-Test in obese and post-bariatric surgery patients. Obes Surg. 2017;27(1):110–114. DOI:10.1007/s11695-016-2244-7
- Jones P, Miravitlles M, van der Molen T, et al. Beyond FEV1 in COPD: A review of patient-reported outcomes and their measurement. Int J COPD. 2012;7:697–709.
- Hernandes NA, Wouters EFM, Meijer K, et al. Reproducibility of 6-minute walking test in patients with COPD. Eur Respir J. 2011;38:261–267.
- Sciurba F, Criner GJ, Lee SM, et al. Six-minute walk distance in chronic obstructive pulmonary disease: reproducibility and effect of walking course layout and length. Am J Respir Crit Care Med. 2003;167(11):1522–1527. DOI:10.1164/rccm.200203-166OC
