Abstract
Chronic Obstructive Pulmonary Disease (COPD) is a major cause of morbidity and mortality in Nepal. It is a progressive lung disease and has a significant impact on the quality of life of patients. Health‐related quality of life (HRQOL) reflects the health‐ and disease‐related facets of quality of life. Limited studies have assessed the impact of COPD on HRQOL and associated factors in Nepal. This study is based on a cross-sectional household survey data from a semiurban area of Western Nepal. A validated Nepali version of St George’s Respiratory Questionnaire (SGRQ) was used to measure the HRQOL. COPD was defined together with post-bronchodilator airflow obstruction and the presence of respiratory symptoms. Post-bronchodilator airflow obstruction was defined as Forced Expiratory Volume in 1st second (FEV1) to Forced Vital Capacity (FVC) ratio < 0.70. COPD was diagnosed in 122 participants, and their median (IQR) total score of HRQOL was 40 (26 − 69); the score of symptoms, activity, and impact area were 53 (37 − 74), 57 (36 − 86), and 26 (13 − 62), respectively. The overall HRQOL was significantly different in terms of age, occupational status, physical activity, and comorbidities. Disease severity and the presence of respiratory symptoms had a significant difference in HRQOL (p = 0.0001). Appropriate measures to improve conditions and addressing the associated factors like respiratory symptoms and enhancing physical activity are necessary and important.
Background
Chronic Obstructive Pulmonary Disease (COPD) is an irreversible lung disease characterized by permanent and progressive airway obstruction [Citation1]. It is a common illness affecting millions of people around the world, and in 2017, above 3 million people died globally due to COPD [Citation2]. COPD is one of the most prevalent non-communicable disease (NCD) in Nepal [Citation3]. The estimated prevalence of COPD in Nepal is 8.5%, and prevalence of chronic airflow obstruction (CAO) is 12% [Citation3,Citation4]. Similarly, COPD accounts for 43% of NCDs-related out-patient visits in Nepal [Citation5].
COPD results in a substantial socioeconomic burden to the patients [Citation6,Citation7]. It also impairs physical and mental health and reduces abilities to perform activities of daily living [Citation8]. The symptoms of COPD, including shortness of breath and productive cough, degrade the health status of the patient and may lead to disability [Citation8,Citation9]. It forces patients to give up the basic activities of daily living and discontinuing their work [Citation10]. Furthermore, the treatment of COPD is associated with very high costs, which significantly affects patients’ economic status [Citation11]. The Global Burden of Disease study 2019 estimated COPD as the leading cause of disability-adjusted life years (DALYs) in Nepal, accounting for 7.3% of total DALYs [Citation12].
Measuring health‐related quality of life (HRQOL) is essential for examining the limitations and progression of the disease over time and may support monitoring of treatment [Citation13,Citation14]. Both general and disease-specific instruments have been used to measure quality of life in patients with COPD [Citation15]. Among the disease-specific questionnaires, St. George’s Respiratory Questionnaire (SGRQ) is a frequently used tool to evaluate the HRQOL of COPD patients [Citation16,Citation17].
There are some earlier studies reporting HRQOL of COPD patients in Nepal [Citation18–20]. However, no published evidence on the quality of life of people living with COPD exists from a randomly selected community-based survey in Nepal. Considering the increasing burden of COPD, exploring the HRQOL among patients with COPD will be helpful for health professionals and policymakers. This study aimed to evaluate the HRQOL in COPD patients in a semiurban area of Western Nepal.
Materials and methods
Study design and settings
This cross-sectional study is based on data from the baseline survey of COBIN-P (Community-based Management of Chronic Obstructive Pulmonary Disease: a cluster randomized controlled trial). In the baseline survey of COBIN-P, 1438 subjects (≥40 years of age) were surveyed to determine the prevalence of COPD, magnitude of its risk factors, and HRQOL in a semiurban area of Pokhara metropolitan city (formerly known as Lekhnath Municipality) of western Nepal [Citation21]. According to the latest census, the total population of the study area is 58,816 [Citation22].
Study population and sampling
The adult population (≥40 years of age) permanently living in the study area were the study population of the survey. People who were below 40 years of age, severely ill, diagnosed with active pulmonary tuberculosis or a current respiratory infection, with any contraindication for performing spirometry, unlikely to be in the community throughout the intervention period and those who declined to give consent were excluded from the study [Citation23]. The study method of the project COBIN-P baseline survey has been discussed earlier [Citation4].
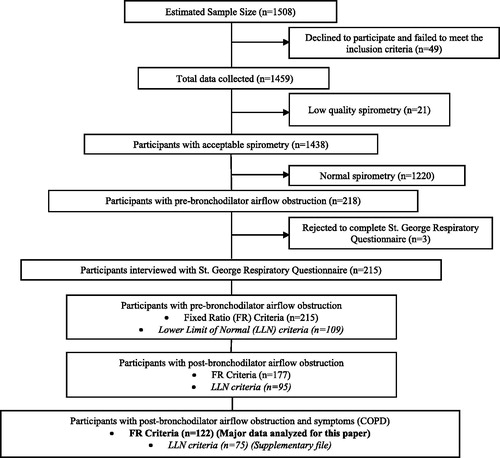
The estimated sample size of the baseline survey was 1508, considering 8% prevalence, 5% margin of error, a design effect of 1.5, and a response rate of 90% [Citation24,Citation25]. The study surveyed the households selected for the Community-based management of non-communicable disease study in Nepal (COBIN) by systematic random sampling [Citation26]. Kish sampling grid was used in households to select one eligible adult per household randomly [Citation27]. Of the surveyed participants, 122 individuals were defined as COPD having symptoms and post-bronchodilator airflow obstruction during spirometry. This study assesses the HRQOL among 122 individuals living with COPD in the study area. The flow diagram of participants’ enrollment and selection is presented in .
Data collection and study tools
Lung function was measured using a portable spirometer (EasyOne Air, ndd Medizintechnik AG, Switzerland) at participants households by the trained data enumerators following American Thoracic Society (ATS) and European Respiratory Society (ERS) task force guidelines for spirometry [Citation23]. Spirometry reports with three acceptable and reproducible graphs according to ATS/ERS guidelines was recorded. The World Health Organization (WHO) STEPwise approach to non-communicable disease risk factor surveillance tool validated in Nepal was used to collect data on physical measurement (height and weight), socio-demographic (age, sex, ethnicity, education, occupation, marital status), and lifestyle-related factors (smoking status, biomass fuel exposure, secondhand smoking, physical activity) [Citation28]. The Body Mass Index (BMI) was calculated as kilogram/meter2 (kg/m2) and classified as underweight (<18.5 kg/m2), normal (18.5–24.9 kg/m2) and overweight/obese (≥25 kg/m2).
The information on respiratory symptoms was collected using an adapted questionnaire from similar studies conducted in Nepal and Uganda [Citation29,Citation30]. A previously validated Nepali version of SGRQ was used to measure the HRQOL [Citation18]. It measures the quality of life connected with the health of patients who have asthma and chronic lung disease [Citation17].
SGRQ measures three areas of functioning of the patients: the sphere of symptoms, activity, and impact of the disease on the patient’s life [Citation17]. The SGRQ symptoms domain estimates the influence of respiratory symptoms, their frequency, and severity. The activity domain evaluates the influence of physical activity, which exacerbates the symptoms of the disease and is connected with the influence of shortness of breath on the patient's physical activity. The impact scores of SGRQ include the aspects connected with the patient's social functioning and estimates the presence of psychological dysfunctions caused by the lung disease. The total score computed presents the influence of the disease on the general health status. The results are presented in percentage, where 100 stands for the worst stage of quality of life.
COPD was defined by the presence of post-bronchodilator airflow obstruction and respiratory symptoms. In the principal analysis, post-bronchodilator airflow obstruction was defined as Forced Expiratory Volume in 1st second (FEV1) to Forced Vital Capacity (FVC) ratio <0.70 according to Global Initiative for Chronic Obstructive Lung Disease (GOLD) fixed ratio (FR) criterion. Due to the absence of lung function reference values for the Nepalese population, an established reference equation for a North Indian population was used [Citation31]. The severity of COPD was defined according to GOLD categorization: grade 1–4. The sensitivity analysis results of the lower limit of normal (LLN) criterion based on FEV1/FVC < LLN are reported in the Supplementary File.
The study was conducted in accordance with the Declaration of Helsinki. Ethical approval was obtained from the ethical review board of the Nepal Health Research Council (Approval number: 30-2019). Written informed consent was obtained from study participants. The study protocol trial registration number of the COBIN-P trial is NCT03797768.
Statistical analysis
Participants’ background/clinical characteristics were summarized as the frequency and percentage for categorical variables and the median and interquartile range (IQR) for continuous variables. As the HRQOL was measured as the continuous variable, the distribution of the HRQOL according to the participants’ characteristics were estimated as the median and IQR; separately estimated for the activity score, impact score, symptoms score, and total score. A non-parametric Kruskal-Wallis test was used to measure the association between the HRQOL scores and categorical background characteristics as the distribution of the scores were not-normal. P-value <0.05 was considered statistically significant throughout the analysis. The analysis was performed using STATA version 15.1 (StataCorp. Texas, USA).
Results
The characteristics of study participants are tabulated in . The median age of the participants was 65 (IQR: 59 − 74) years, and about 60% were male. About 40% were illiterate, and the majority were involved in agriculture. Nearly a quarter of participants were obese/overweight, and above 75% had a low level of physical activity. Approximately 8 out of 10 study participants were either former or current smokers. Among the study participants, nearly 60% had modified medical research council (mMRC) dyspnea scale grade ≥2 ().
Table 1. Study participants characteristics.
SGRQ defined health-related quality of life and airflow obstruction status
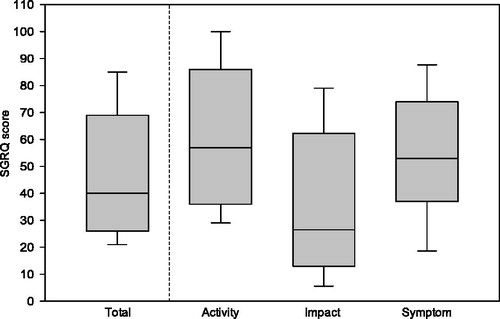
The median (IQR) SGRQ quality of life of people living with COPD was 40 (26 − 69) for overall score, 26 (13 − 62) for impact score, 57 (36 − 86) for activity score, and 53 (37 − 74) for symptom, score (). The overall median SGRQ quality of life for LLN defined COPD was 47 (28 − 73) higher than that of FR defined airflow obstruction (Supplementary File).
SGRQ defined health-related quality of life scores by COPD severity stages
The median SGRQ quality of life level in all the domains gradually worsened with an increase in severity stage of COPD with marked impairment and differences across the stage. There was a significant difference in SGRQ scores between the COPD severity stage (p-value = 0.001) ().
Table 2. SGRQ defined health-related quality of life by COPD severity stages.
Factors associated with SGRQ defined health-related quality of life (HRQOL) in people living with COPD
The median SGRQ activity, symptom and total scores were significantly associated with age groups (). Unemployed and participants with comorbidities had a poor level of HRQOL median scores (p < 0.001). Similarly, level of physical activity and mMRC dyspnea scale were also associated with SGRQ scores (p < 0.001). The presence of respiratory symptoms cough, wheezing, and phlegm production degraded quality of life level across all domains of SGRQ (p < 0.001) (). However, in LLN-based analysis, participants age was not significantly associated with median SGRQ score and the level of HRQOL was observed poor among those exposed to secondhand smoking (p = 0.041) (Supplementary File).
Table 3. Factors associated with HRQOL among people living with COPD.
Discussion
Our study showed that the median SGRQ scores increased as the disease severity increased from I to IV. Similarly, HRQOL was significantly associated with respiratory symptoms, mMRC dyspnea scores, and age. These findings align with the results from earlier studies reporting that respiratory symptoms are associated with impaired HRQOL among people living with COPD [Citation8,Citation19,Citation32]. It was also coherent with earlier reported findings where the quality of life decreased as the severity of COPD increased [Citation33,Citation34].
The total SGRQ median score of 40 (26 − 69) also corroborates with the results of earlier SGRQ validation study in Nepal, reporting 41 (± 27) total score for spirometry confirmed COPD patients from the community [Citation18]. It is slightly higher than a community-based research finding from India, with a mean total score of 39 [Citation33].
Among the different domains of SGRQ, the symptoms and activity domain were the most affected, while the impact domain was the least affected aspect of quality of life among individuals with COPD. In line with this findings, previous studies have also reported a higher perceived impact on the quality of life due to symptoms of COPD and limitation in daily activities due to breathlessness rather than hindrances in social functioning and psychological disturbances resulting from COPD [Citation33,Citation35]. This could be attributed to a couple of reasons. Firstly, this is a community-based quality of life survey nested within a community-based prevalence study and, only 3% of study participants reported being clinically diagnosed with COPD before the survey while the vast majority were identified through household spirometry [Citation4]. Since the disease was largely underdiagnosed, the perceived hindrances in psychological and social functioning due to COPD are also not well-understood. It is further supported by findings from the quality of life studies conducted in clinical settings in Nepal with clinically diagnosed COPD that reported higher SGRQ scores [Citation20] compared to our study derived from community-based COPD diagnosis and community-based quality of life survey. Secondly, any psychological effect due to COPD may have been dismissed as ailments of old age hence underestimating the total psychological impact of the disease. The noteworthy patients’ characteristics like mMRC dyspnea scale graded breathlessness, respiratory symptoms like wheezing, phlegm production, cough were significantly associated with HRQOL scores. This supports the findings from previous studies which reported that dyspnea is one of the main factors of the disease specific QOL among patients with COPD. Dyspnea is often regarded as the most distressing COPD symptom affecting QOL [Citation32].
Likewise, the present study showed that demographic factors, such as age and employment status, influenced HRQOL. These findings are consistent with those of Rosińczuk et al. [Citation36]. A hospital-based study from the Chitwan district of Nepal also found a significant difference in the quality of life score among the different age groups [Citation19]. Similar findings were reported by a study conducted in Poland, showing elderly COPD patients had compromised quality of life [Citation37]. In addition, our study illustrated that 60% of study participants had comorbidities of cardiovascular disease and diabetes mellitus. Those with comorbidities had higher (worse HRQOL) median scores in the activity domain and a total score of SGRQ (p < 0.001). Rafii et al. also showed the inverse relationship of comorbidities with HRQOL in COPD patients [Citation37].
Interestingly, the present study found no significant differences in HRQOL based on sex, and this is concurrent with other studies [Citation19,Citation36]. However, sex has also been reported to be associated with HRQOL of COPD patients, showing females having an impaired quality of life level [Citation38]. Other studies have reported a significant positive correlation between smoking packyears [Citation39] and higher SGRQ score for smokers compared to nonsmokers [Citation40]. Although no such significant association was seen between smoking packyears and smoking status with any domains of SGRQ scores for individuals with COPD in our study.
The study also showed that higher physical activity was associated with a better HRQOL as compared to COPD individuals with lower physical activity. Promoting physical activity, especially for the elderly population, which constitutes a majority of COPD patients, can be a potentially effective lifestyle intervention to enhance physical, mental wellbeing and overall quality of life [Citation41]. However, it could possibly also be reverse causality, i.e. people with low impact performed higher physical activity.
To the best of our knowledge, this is a first of its kind study in Nepal that uses the validated tool of SGRQ on a randomly sampled population-based study in a semiurban area of western Nepal, analyzing the results based on both fixed ratio and LLN criteria of CAO. We anticipate a very low selection bias considering a high response rate of 97% [Citation4]. This population-based study findings are more relevant in resource-constrained settings like Nepal, where clinically diagnosed COPD cases underrepresent the total burden of COPD. Along with this, availability, accessibility, and utilization of spirometry for COPD diagnosis and treatment is not optimal due to lack of adequate human resources and technology and poor health-seeking behavior [Citation4,Citation42,Citation43]. Thus, this study conducted at the community level reiterates the importance of identifying COPD in earlier stages, promotion of physical activity with a particular focus on the co-morbid and elderly population is vital to halt the disease progression and enhance the physical, social and mental wellbeing of people living with COPD.
Nevertheless, the results of the present study should be interpreted by considering its limitations. This was a cross-sectional study; therefore, the causal relationship between HRQOL and the examined variables could not be established. Likewise, we do not have enough information to rule out reverse causality as the exposure, COPD status, and HRQOL were assessed at the same time. Despite the extensively trained enumerators, who collected the data, we cannot deny the possibilities of miscalculations of self-reported outcomes such as smoking behaviors, physical activity, biomass fuel exposure, and respiratory symptoms. Being a cross sectional study, this study is not free of information bias. For example, smoking behavior could be underreported due to social desirability bias. Also, the people who had a higher stage of COPD might have overestimated their cigarette consumption and exposure to other pollutants compared to less severe patients. This recall bias generally tends to result in lower quality of life among heavy smokers. However, it is difficult to certain the effect of such information bias in the quality-of-life score. Also, we didn’t perform multiple comparisons. Only 1.4% of surveyed data were excluded due to the poor quality of spirometry. These excluded individuals were younger than included participants. This might have slightly exaggerated our findings according to the age category. Likewise, the percentage of ex-smokers and current smokers was observed higher among excluded individuals. This might have resulted in reduced power to detect the statistical difference of HRQOL within the smoking status. Similarly, we lack information on the duration of disease and exacerbations that could have influenced the level of HRQOL.
Conclusion
In conclusion, a higher SGRQ score was observed among people living with COPD and got higher with the grade of disease severity. This implies that people living with COPD in the community experience significant impairment in their quality of life with disease severity and increased breathlessness symptoms. Early identification and treatment of COPD, along with health promotion programs for elderly and co-morbid people living with COPD will not only halt the progression of disease but may also improve the overall quality of life of people living with COPD, thus reducing overall burden of COPD.
| Abbreviations | ||
| BMI | = | Body Mass Index |
| COBIN | = | Community-based Management of Non-communicable Disease in Nepal |
| COBIN-P | = | Community-based Prevention and Management of Chronic Obstructive Pulmonary in Nepal |
| COPD | = | Chronic Obstructive Pulmonary Disease |
| DALYs | = | Disability Adjusted Life Years |
| FEV1 | = | Forced Expiratory Volume in 1st second |
| FVC | = | Forced Vital Capacity |
| GOLD | = | Global Initiative for Chronic Obstructive Lung Disease |
| HRQOL | = | Health-Related Quality of Life |
| IQR | = | Interquartile Range |
| LLN | = | Lower Limit of Normal |
| mMRC | = | Modified Medical Research Council |
| NCDs | = | Non-communicable Diseases |
| SGRQ | = | St. George Respiratory Questionnaire |
| WHO | = | World Health Organization. |
Author’s contribution
TBA, PK and DN conceived and designed the study. TBA collected, analyzed, and interpreted data. AR and PA supported in data analysis. TBA wrote the first draft; incorporated co-authors' suggestions; and prepared the final version for submission. All authors revised the manuscript with substantial contribution and approved the final version for submission.
Acknowledgments
The authors would like to thank all the respondents of the study for providing their time and information on the study questionnaire. We would also acknowledge data enumerators and Nepal Development Society staff at the Project office of Pokhara, Nepal.
Declaration of interest
The authors declare that they have no competing interests in this work.
Additional information
Funding
References
- Global Initiative for Chronic Obstructive Lung Disease Inc. (GOLD). Global Strategy for Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease 2020 (Report). Fontana (CA): Global Initiative for Chronic Obstructive Lung Disease; 2020. https://goldcopd.org/wp-content/uploads/2019/12/GOLD-2020-FINAL-ver1.2-03Dec19_WMV.pdf
- Li X, Cao X, Guo M, et al. Trends and risk factors of mortality and disability adjusted life years for chronic respiratory diseases from 1990 to 2017: systematic analysis for the Global Burden of Disease Study 2017. BMJ. 2020;368:m234.
- Dhimal M, Karki KB, Sharma SK, et al. Prevalence of selected chronic non-communicable diseases in Nepal. J Nepal Health Res Counc. 2019;17(3):394–401.
- Adhikari TB, Acharya P, Högman M, et al. Prevalence of chronic obstructive pulmonary disease and its associated factors in Nepal: findings from a community-based household survey. COPD. 2020;15:2319–2331.
- Bhandari GP, Angdembe MR, Dhimal M, et al. State of non-communicable diseases in Nepal. BMC Public Health. 2014;14(1):1–9.
- Iheanacho I, Zhang S, King D, et al. Economic burden of chronic obstructive pulmonary disease (COPD): a systematic literature review. COPD. 2020;15:439–460.
- Srivastava K, Thakur D, Sharma S, et al. Systematic review of humanistic and economic burden of symptomatic chronic obstructive pulmonary disease. Pharmacoeconomics. 2015;33(5):467–488.
- Ioanna T, Kocks J, Tzanakis N, et al. Factors that influence disease-specific quality of life or health status in patients with COPD: a systematic review and meta-analysis of Pearson correlations. Prim Care Respir J. 2011;20(3):257–268.
- Park SK, Larson JL. Symptom cluster, healthcare use and mortality in patients with severe chronic obstructive pulmonary disease. J Clin Nurs. 2014;23(17–18):2658–2671.
- Janson C, Marks G, Buist S, et al. The impact of COPD on health status: findings from the BOLD study. Eur Respir J. 2013;42(6):1472–1483.
- Kirsch F, Schramm A, Schwarzkopf L, et al. Direct and indirect costs of COPD progression and its comorbidities in a structured disease management program: results from the LQ-DMP study. Respir Res. 2019;20(1):215.
- Global Burden of Disease Study (GBD 2019) [Internet]. Washington; 2020 [cited 2020 Nov 17]. Available from: http://www.healthdata.org/gbd/2019
- Kaplan RM, Ries AL. Quality of life: Concept and definition. COPD. 2007;4(3):263–271.
- Treurniet HF, Essink-Bot M-L, Mackenbach JP, et al. Health-related quality of life: an indicator of quality of care? Qual Life Res. 1997;6(4):363–369.
- Engström C, Persson L, Larsson S, et al. Health-related quality of life in COPD: why both disease-specific and generic measures should be used. Eur Respir J. 2001;18(1):69–76.
- Pickard AS, Yang Y, Lee TA. Comparison of health-related quality of life measures in chronic obstructive pulmonary disease. Health Qual Life Outcomes. 2011;9(1):26.
- Jones PW, Quirk FH, Baveystock CM, et al. A self-complete measure of health status for chronic airflow limitation. The St. George’s Respiratory Questionnaire. Am Rev Respir Dis. 1992;145(6):1321–1327.
- Sherpa CT, LeClerq SL, Singh S, et al. Validation of the St. George’s Respiratory Questionnaire in Nepal. Chronic Obstr Pulm Dis. 2015;2(4):281.
- Sharma K, Joshi S. Quality of life of patients with chronic obstructive pulmonary disease in Chitwan, Nepal: a pilot study report. Int J Med Sci Public Health. 2015;4(9):1235–1241.
- Sato A, Kamimura M, Yorimoto K, et al. Evaluation of a chest rehabilitation project in Nepal using the St. George’s Respiratory Questionnaire and Chronic Obstructive Pulmonary Disease Assessment Test. J Phys Ther Sci. 2020;32(12):795–799.
- Adhikari TB. Community-based Management of Chronic Obstructive Pulmonary Disease in Nepal (COBIN-P): U.S. National Library of Medicine 2019. [updated 2019; cited 2020 Oct 26]. Available from: https://clinicaltrials.gov/ct2/show/NCT03797768
- Central Bureau of Statistics. National Population and Housing Census 2011 (National Report). Kathmandu (Nepal): Government of Nepal, National Planning Commission Secretariat, Central Bureau of Statistics; 2012. p. 34.0. https://unstats.un.org/unsd/demographic/sources/census/wphc/Nepal/Nepal-Census-2011-Vol1.pdf
- Graham BL, Steenbruggen I, Miller MR, et al. Standardization of spirometry 2019 update. An official American thoracic society and European respiratory society technical statement. Am J Respir Crit Care Med. 2019;200(8):e70–e88.
- Adhikari TB, Neupane D, Kallestrup P. Burden of COPD in Nepal. COPD. 2018;13:583–589.
- Zhong N, Wang C, Yao W, et al. Prevalence of chronic obstructive pulmonary disease in China: a large, population-based survey. Am J Respir Crit Care Med. 2007;176(8):753–760.
- Neupane D, Shrestha A, Mishra SR, et al. Awareness, prevalence, treatment, and control of hypertension in western Nepal. Am J Hypertens. 2017;30(9):907–913.
- Kish L. A procedure for objective respondent selection within the household. J Am Stat Assoc. 1949;44(247):380–387.
- Aryal KK, Mehata S, Neupane S, et al. The burden and determinants of non communicable diseases risk factors in Nepal: findings from a nationwide STEPS survey. PLoS One. 2015;10(8):e0134834.
- van Gemert F, Kirenga B, Chavannes N, et al. Prevalence of chronic obstructive pulmonary disease and associated risk factors in Uganda (FRESH AIR Uganda): a prospective cross-sectional observational study. Lancet Glob Health. 2015;3(1):e44–e51.
- Nepal Health Reserach Council. Report of indoor air pollution and its effects on human health in Ilam District of Eastern Nepal, 2015. Kathmandu (Nepal): University of Delhi; 2016.
- Chhabra S, Kumar R, Gupta U, et al. Prediction equations for spirometry in adults from northern India. Indian J Chest Dis Allied Sci. 2014;56(4):221–229.
- Miravitlles M, Ribera A. Understanding the impact of symptoms on the burden of COPD. Respir Res. 2017;18(1):67.
- Ahmed MS, Neyaz A, Aslami AN. Health-related quality of life of chronic obstructive pulmonary disease patients: results from a community based cross-sectional study in Aligarh, Uttar Pradesh, India. Lung India. 2016;33(2):148.
- Ståhl E, Lindberg A, Jansson S-A, et al. Health-related quality of life is related to COPD disease severity. Health Qual Life Outcomes. 2005;3(1):56.
- Farag T, Sobh E, Elsawy S, et al. Evaluation of health-related quality of life in patients with chronic obstructive pulmonary disease. Egypt J Bronchol. 2018;12(3):288–294.
- Rosińczuk J, Przyszlak M, Uchmanowicz I. Sociodemographic and clinical factors affecting the quality of life of patients with chronic obstructive pulmonary disease. COPD. 2018;13:2869–2882.
- Grochans E, Bak A, Reczynska A, et al. Socio-demographic contributors to quality of life of patients with asthma and chronic obstructive pulmonary disease. Fam Med Prim Care Rev. 2013;15(4):536–539.
- Merino M, Villoro R, Hidalgo-Vega Á, et al. Health-related quality of life of patients diagnosed with COPD in Extremadura, Spain: results from an observational study. Health Qual Life Outcomes. 2019;17(1):189–189.
- Zamzam MA, Azab NY, El Wahsh RA, et al. Quality of life in COPD patients. Egypt J Chest Dis Tuberc. 2012;61(4):281–289.
- Ferrer M, Villasante C, Alonso J, et al. Interpretation of quality of life scores from the St George's Respiratory Questionnaire. Eur Respir J. 2002;19(3):405–413.
- Vagetti GC, Barbosa Filho VC, Moreira NB, et al. Association between physical activity and quality of life in the elderly: a systematic review, 2000-2012. Rev Bras Psiquiatr. 2014;36(1):76–88.
- Bolton CE, Binaya K, Koju R, et al. Challenges of chronic obstructive pulmonary disease in rural Nepal. Lancet Respir Med. 2019;7(6):476–478.
- Meghji J, Mortimer K, Agusti A, et al. Improving lung health in low-income and middle-income countries: from challenges to solutions. Lancet. 2021;397(10277):928–940