Abstract
Chronic Obstructive Pulmonary Disease (COPD) is a progressive but preventable and treatable disease and the third leading cause of death globally. Even though it is evident that physical activity (PA) relieves dyspnea, anxiety, fatigue, and increases quality of life and functional capacity, it is seldom implemented in daily life in people with COPD. The aim of this study was to identify barriers toward PA in people with COPD and to examine the role of FEV1 and smoking status in PA. The study is a quantitative cross-sectional study conducted in Denmark among people with COPD. Data was collected using questionnaires developed by the authors after pilot testing. In total, 493 people with COPD were included. The most significant barrier toward PA was low motivation (p < 0,001 and p = 0,009) and comorbidity (p = 0,035 and p = 0,016). Fear of breathlessness was significantly (p < 0,001) correlated to low motivation. FEV1, and smoking status were not associated with the level of PA. In our study, the main reason why people with COPD did not engage in PA was low motivation, where fear of breathlessness and co-morbidity correlated significantly with low motivation. Studies have shown that doing activities that are enjoyable promotes PA in daily life, indicating that activities that enhance motivation might help people with COPD to see PA as part of their life rather than an obligation. Further exploratory studies are needed.
Introduction
Background
Chronic obstructive lung disease (COPD) is a progressive disease characterized by airflow limitation caused by exposure to noxious particles, which may lead to persistent respiratory symptoms. The primary cause of COPD is tobacco smoking, and the risk of developing COPD among smokers is around 40% [Citation1–3].
The disease is a global health challenge and an extensive socioeconomic burden. World Health Organization (WHO) estimates that 65 million people have moderate to severe COPD. It is a leading cause of morbidity and mortality, and currently the third leading cause of death globally and is predicted to increase even further because of the continued exposure to COPD risk factors and an aging population [Citation1, Citation4]. In Denmark, COPD is also common. Every year 10,048 new cases are diagnosed with COPD, and the disease is the most common reason for hospitalizations among the medical conditions. Every year, treatment and care of COPD accounts for an estimated 1292,9 million Danish crones [Citation5–7].
Physical activity (PA) is an essential aspect of treatment and wellbeing in several medical conditions, and The Global Initiative for Chronic Obstructive Lung Disease (GOLD) [Citation8] recommends regular PA alongside medication for people with COPD. PA is known to relieve dyspnea, anxiety and fatigue, increase exercise and functional capacity, and improve life quality [Citation9]. Several studies have demonstrated that people with COPD are significantly less physically active compared to healthy, age-matched controls [Citation10–13]. Inactivity increases the likelihood of dying from COPD [Citation14–16], and the level of PA in people with COPD is related to lung function decline, hospitalizations and mortality [Citation17–19]. However, despite strong evidence for the beneficial effects of PA, it often fails to get implemented in daily life of people with COPD and in clinical practice [Citation5, Citation20, Citation21]. Data suggests that people with COPD reduce their PA early on and often at the time of diagnosis [Citation22–24], e.g. a controlled multicenter pilot-study by Troosters et al. [Citation22] concluded that PA is reduced early in disease progression. Furthermore, it appears to be challenging to recruit people with COPD to attend - and especially to complete - pulmonary rehabilitation and to do PA on a daily basis [Citation5, Citation15, Citation21, Citation25].
Objectives
We hypothesized that numerous factors/barriers might be associated with a low level of PA, such as reduced lung function, anxiety, dyspnea, low motivation, self-efficacy, not knowing the benefits of PA, socio-environmental factors, exacerbations, and co-morbidities. If the available training possibilities or offers are limited, it could contribute to inactivity as well.
From the sparse number of studies that have explored the association between lung function and PA, the association seems weak [Citation15]. Hayton et al. [Citation26] stated that smoking status is a strong predictor of both attendance and adherence to pulmonary rehabilitation. However, there have not been studies investigating the relationship between smoking status and PA to our knowledge. Therefore, the aim of this study was to identify barriers toward PA in people with COPD and to examine the role of forced expiratory volume during the first second (FEV1) and smoking status in PA.
Methods
Study design
This study is a quantitative questionnaire-based cross-sectional study conducted in Denmark among people diagnosed with COPD.
Study setting
Participants were invited via flyers handed out at hospitals, pulmonary out-patient clinics, shops, and cultural centers in all regions of Denmark, and through targeted advertisements via social media and local pulmonary network groups. The flyer briefly explained the study background and the search for people with COPD to participate in a survey about PA concerning behavior and attitude. The flyer also provided contact information to the investigators for further information. The people that responded were screened for eligibility based on whether they self-reported to be diagnosed with COPD or not. Eligible participants would then receive a questionnaire in either electronic or paper format, depending on personal preference. The electronic questionnaire was conducted through Survey Xact [Citation27]. Filled out questionnaires in paper format were returned to the investigators by mail or handed in by post.
Participants
People who self-reported to be diagnosed with COPD were eligible to participate in the study but were excluded if there were uncertainty about the COPD diagnosis: if the participants did not answer the question regarding their lung function and symptoms (question six, Appendix 1, supplementary material) or if they did not state their smoking history (question 15, Appendix 1, supplementary material). If the questionnaire was incomplete the participants were excluded from the study.
Data sources
Data were collected during a one-year period using a questionnaire - composed within the author-group - containing 16 items (Appendix 1, supplementary material) since no validated questionnaire suitable for use in our study was available. The questionnaire was pilot-tested among a group of ten people diagnosed with COPD, comparable with the study population with respect to sex, age, and diagnosis.
The questionnaire is available in full (Appendix 1, supplementary material) and is composed of questions regarding patient demographics, sex, age, geography, and diagnosis, followed by questions that addressed daily level of PA and potential barriers - mainly using a four-point Likert Scale for answers. The extent of information received from the general practitioner (GP) about potential benefits of PA was also addressed. PA is considered as an important non-pharmacology treatment of COPD and in Denmark most patients are referred to pulmonary rehabilitation by their GP. Moreover, data concerning self-reported current or previous attendance in pulmonary rehabilitation was collected.
Data variables
Information about the level of airflow obstruction (FEV1) and symptom score, were solely based on self-reporting.
The authors pre-selected potential barriers to be included in the study. These were: fear of breathlessness, limited availability of training, low airflow obstruction and/or high symptom score, number and/or severity of co-morbidities, low motivation, and lack of information about PA from the GP. The participants then rated to what extent the barriers affected their level of PA.
The threshold defining daily activity level was: being active 20-30 min at an intensity above the talk-limit (sentences get interrupted due to dyspnea). This is in line with the recommendation from the Danish Health Authority [Citation28].
Statistical methods
All data were handled and analyzed using Stata 14.2 (Statacorp. Texas. USA). Descriptive data are given in means with standard deviations or percentages as appropriate. The significance level was set to 0.05 on two-sided tests.
Linear and ordered logistical models were developed to study the impact of the data variables on level of training and possible causes leading to low motivation.
Model building
Linear regression analysis was performed to examine how the level of training correlated with the pre-selected potential barriers. Univariate regressions of each variable were conducted with the number of active days as the dependent variable. Hereafter, a multivariate linear regression model was used to evaluate the contribution of each variable.
An ordered logistical regression model was used to study the effect of variables on causes of low motivation. Both models were built with an a priori selection of relevant variables. Variables were chosen based on our knowledge of the topic. No automated model building methods including forward or backward selection was used.
Ethics approval
Since the study was solely based on questionnaires, ethical approval of the study was not required by regulatory authorities in Denmark [Citation29–31]. The participants were ensured complete anonymity as the questionnaires were anonymous.
Results
Participants
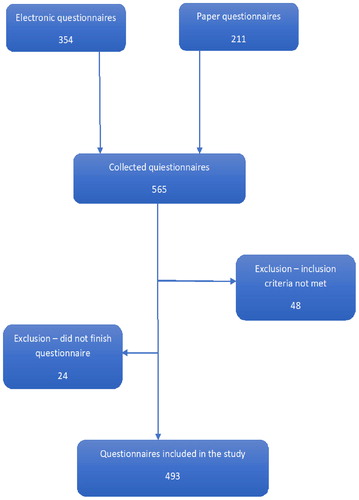
A total of 565 questionnaires were collected. 48 individuals were excluded due to uncertainty of the COPD diagnosis and 24 due to incompletion of the questionnaire. In total, 493 people with COPD were included in the analysis ().
Descriptive data
169 males and 324 females were included. Data from the study population was compared to existing data from the Danish Registry of COPD [Citation32], resulting in the following findings:
The study population was comparable with data from the Danish Registry of COPD concerning geography (although with some minor variation). Females were overrepresented in the study group (66% vs. 54%) as well as people with moderate COPD (47% vs. 35%) while very severe COPD (12% vs. 22%) was underrepresented. Mild COPD (7% vs 5%) and severe COPD (34% vs. 39%) were comparable. Smoking status was comparable between the study population and the Danish Registry of COPD: never smokers (5% vs. 3%) and previous smokers/current smokers (95% vs. 97%). The demographic characteristics are summarized in .
Table 1. Demography of the study population and the COPD population in Denmark.
Factors related to barriers to PA
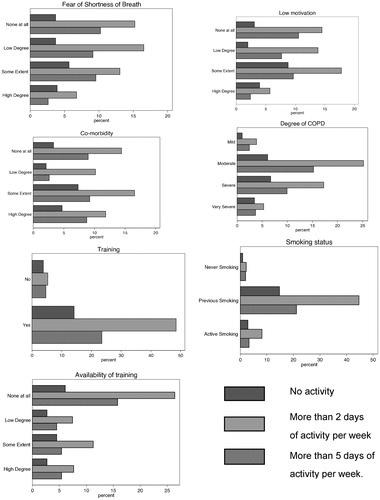
The level of PA among the participants in correlation to each barrier is shown in . In the graphs, each barrier is linked to activity level and to which degree the barriers affect activity level. E.g., the first figure shows to what extent fear of shortness of breath limits daily PA. Previous smokers were more active than never smokers and active smokers.
Regression models
The results of the univariate and multivariate regression analysis are shown in . The models display the number of weekdays the participants are active in correlation to each barrier. The univariate regression found that: Low motivation (p < 0,001), co-morbidity (p = 0,035) and fear of breathlessness (p = 0,009) were statistically associated with activity level in the study population. Low motivation was highly significant. Training availability, the degree of COPD (FEV1), smoking status and current or previous training were not significantly associated with activity level.
Table 2. The results of the univariate and a multivariate regression analysis.
The effect of each barrier for PA - when adjusted for the remaining barriers - is displayed in the multivariate regression. Low motivation (p = 0,009) and co-morbidity (p = 0,016) remained significant, whereas the remaining barriers including fear of breathlessness were insignificant (p = 0,385).
Correlation between barriers and motivation
Low motivation was statistically inversely associated with PA. Consequently, post hoc analysis were conducted to determine the relation between low motivation and each of the remaining barriers. Data were pooled in a univariate ordered logistical regression and a multivariate ordered logistical regression, where the remaining barriers were taken into account. In the univariate logistical regression training availability, co-morbidity, fear of breathlessness and the degree of COPD were all statistically significant correlated with low motivation. This linkage increased the less motivated the participants were. Age, smoking status and self-reported training were not correlated with low motivation. When adjusting for the remaining barriers the same pattern is displayed - although to a lesser degree. However, after adjusting, the degree of COPD was no longer correlated to low motivation. See for details.
Table 3. Correlation between barriers and motivation.
Discussion
PA is a well-documented method to treat COPD and to prevent progression of symptoms. However, in real life it is difficult to motivate to and to maintain PA in patients with COPD. The objectives of this study were to assess potential barriers that were associated with low level of PA in people with COPD and to investigate the roles of FEV1 and smoking status in PA.
The main finding in our study was that low motivation was a key barrier to PA. Secondly, training availability, co-morbidities, and fear of breathlessness were associated with low motivation, with the latter being most pronounced. These findings are not surprising considering the nature of the disease. It is evident that the level of PA decreases as symptoms progresses, leading to decline in physical health status [Citation33]. This vicious circle may cause the development of additional barriers to engage PA [Citation34]. Barriers toward PA are complex, but the patient’s motivation seems essential, which has also been demonstrated by Kosteli et. al [Citation25]. and Hartman et al. [Citation35]. They both conclude that personal barriers such as COPD-related symptoms and lack of drive are significant barriers.
Fear of breathlessness may lead to low motivation and thereby reduce engagement in PA as patients are alarmed by a sensation of breathing difficulty that they are unable to manage. Previous studies have concluded that fear and shame can lead to low level of PA in people with COPD [Citation25, Citation35, Citation36]. COPD contributes to not only physical limitations such as dyspnea but also to psychological limitations such as anxiety, depression, and feeling embarrassed [Citation35, Citation37]. Hence, it seems reasonable to suggest that the psychological impacts of COPD may also affect motivation.
The degree of self-reported air flow limitation did not correlate with the level of PA in our study. The literature shows conflicting results on this topic, varying from weak or insignificant to significant correlation. Watz et al. [Citation14] state that daily activity decreases according to GOLD stage, and Schönhofer et al. [Citation38] showed a correlation between FEV1 and daily movement. However, in another study, a positive correlation between PA and FEV1 was found [Citation39]. Garcia-Aymerich et al. [Citation40] concluded that FEV1 was not associated with PA level, which is further supported in studies by Pitta et al. [Citation13, Citation41]. These findings support the present study that indicate that a low level of PA in people with COPD does not solely depend on airflow limitation measured by FEV1. Garcia-Rio et al. [Citation42] explored the effect of dynamic hyperinflation in the level of PA in people with moderate to severe COPD. They concluded that the decrease in PA is partially explained by dynamic hyperinflation, regardless of the severity of airflow limitation/GOLD stages. This suggests that future studies should include measurements of dynamic hyperinflation when exploring the association between lung function and PA in daily life in people with COPD.
In our study, no direct association between smoking status and PA was found. The existing body of evidence is limited. Most studies have been focusing on the association between attending physical rehabilitation and smoking. In 2013 Hayton et al. [Citation26] investigated the barriers toward pulmonary rehabilitation. They found that smoking status was a strong predictor of both attendance and adherence - smokers tended to be non-adherent. Similar results are found in other studies [Citation43–46]. The questionnaire used in our study only addressed self-reported smoking status and did not register total pack years. Knowledge on pack years may have provided valuable information that could have allowed for a better understanding of the association between smoking and PA. In future studies the focus on the smoking status and the association to PA in daily life needs to be explored in detail.
Engagement in PA is enhanced if PA is considered beneficial by the patients. This attitude toward PA is influenced by the degree of patient knowledge about the impact of COPD [Citation25, Citation47]. Better information about PA's positive effect on the management of breathing difficulties is needed, so the motivation for being physically active will be enhanced. Based on the barriers and enablers toward PA in daily life, it seems essential that people with COPD gain control over their disease, learn to cope and manage their symptoms, and make meaningful and achievable goals [Citation20, Citation47]. Studies have shown that doing activities that are perceived as fun and enjoyable promote PA in daily life, indicating that intrinsic motivation is the most critical factor [Citation48]. Our results support this approach, and activities that keep up motivation might help patients with COPD to see PA as a part of their lifestyle rather than an obligation.
Biking or Nordic walking, which is walking with specially designed poles, could be some examples where hobbies and PA could be combined. Breyer et al. [Citation49] investigated the effect of Nordic walking as a PA in people with COPD. The activity showed to be a simple, safe and effective training modality for people with COPD. Supervised exercise and self-efficacy enhancing exercise is shown to be effective in promoting PA [Citation50]. Cycle ergometer training significantly improves exercise performance, dyspnea, and quality of life [Citation51] why biking could be an activity that could benefit people with COPD. Studies are lacking in this area.
Hobbies like choral singing and dancing could be attractive to some patients. In previous studies, it has been explored whether singing has a positive effect on physical health, quality of life and dyspnea in people with COPD. An effect would be explained by the specified focus on diaphragmic breathing, altered posture, and improvement of breathing co-ordination [Citation52]. Engen et el [Citation53]. showed that singing with vocal instruction and breathing exercises may improve quality of life. Moreover, Skingley et al. [Citation54] demonstrated that singing is perceived as both acceptable and beneficial in people with COPD. Studies have proved an improvement in functional exercise capacity by singing [Citation55–57]. The effect of dancing in people with COPD in literature is limited. Wshah et al. [Citation58] did a feasibility study, where they conclude that dance intervention is enjoyable, safe, and feasible and improved six-minute walking distance, balance, and quality of life. Research in this field is generally limited but needed, especially long-term and randomized controlled studies, to determine the actual effect of singing and dancing on functional capacity, physical health, and dyspnea. The existing studies are mostly of short duration and conducted on small samples.
The results from our study may help professionals to guide people with COPD to enhance PA and incorporate it as part of daily life. More studies of a grander scale that will investigate the effect of the creative activities, both the short- and long-term effects, with measurements of their pulmonary capacities with, e.g. six-meter walking test, shuttle walk, hyperinflation, is needed. Such studies may contribute knowledge on how to increase daily PA.
The major limitation of this study is the cross-sectional design that does not allow conclusions about the causal effect from motivation on PA. Moreover, data were self-reported and based on questionnaire (no interview, medical records or visit at pulmonary clinics) which introduces a risk of information bias potentially partly due to recall issues [Citation59]. Participants self-reported their lung function, symptom-score and activity level, which could have led to an inaccurate estimation. Furthermore, participants could only report from a list of pre-selected barriers when answering question 7 (barriers that influence daily PA). An open question that would have allowed writing down factors perceived as barriers to PA would have been preferable.
In addition, the participants self-reported if they felt comorbidities influenced their level of PA. Unfortunately, we do not have any specific knowledge about the actual comorbidities – number, severity.
We did not get any beneficial results regarding information from GP on PA (question 7 and 14) - an open question would have been desirable.
The methods for selection of the study sample and distributing questionnaires may have contributed to selection bias as people with interest in healthy lifestyle may have been more likely to participate in the study. People with a reading impairment or without social network and limited resources would probably not have answered the questionnaire.
The impact of the results found in this study underlines the importance of gaining a high level of motivation for PA in patients with COPD. Planning of future pulmonary rehabilitation interventions should focus on activities that increase participants' motivation, which will likely increase willingness to start and adhere to training programs.
In conclusion, this cross-sectional study found that for patients with COPD, low motivation was the key barrier to being physically active. Fear of breathlessness and co-morbidity correlated significantly with low motivation.
| Abbreviations | ||
| COPD | = | chronic obstructive pulmonary disease |
| WHO | = | World Health Organization |
| PA | = | physical activity |
| GOLD | = | global initiative for chronic obstructive lung disease |
| FEV1 | = | forced expiratory volume in one second |
| GP | = | general practitioner |
Declaration of interest
The authors declare that there is no conflict of interest.
Additional information
Funding
References
- Gold Reports for Personal Use - Global Initiative for Chronic Obstructive Lung Disease - GOLD. Available from: https://goldcopd.org/gold-reports/.
- WHO | Diagnosis of COPD. Available from: https://www.who.int/respiratory/copd/diagnosis/en/.
- Lundbäck B, Lindberg A, Lindström M, et al. Not 15 but 50% of smokers develop COPD?–Report from the obstructive lung disease in Northern Sweden Studies. Respir Med. 2003;97(2):115–122. http://www.ncbi.nlm.nih.gov/pubmed/12587960 DOI:10.1053/rmed.2003.1446
- WHO | Burden of COPD. Available from: https://www.who.int/respiratory/copd/burden/en/.
- Østergaard EB, Sritharan SS, Kristiansen AD, et al. Barriers and motivational factors towards physical activity in daily life living with COPD – an interview based pilot study. Eur Clin Respir J. 2018;5(1):1484654. DOI:10.1080/20018525.2018.1484654
- Authority TDH. SYGDOMSBYRDEN I DANMARK. 2015. Available from: https://www.sst.dk/da/sygdom-og-behandling/∼/media/00C6825B11BD46F9B064536C6E7DFBA0.ashx.
- Løkke A, Hilberg O, Tønnesen P, et al. Direct and indirect economic and health consequences of COPD in Denmark: a national register-based study: 1998-2010. BMJ Open. 2014;4(1):e004069. http://www.ncbi.nlm.nih.gov/pubmed/24394800 DOI:10.1136/bmjopen-2013-004069
- Global Initiative for Chronic Obstructive Lung Disease - Global Initiative for Chronic Obstructive Lung Disease - GOLD. Available from: https://goldcopd.org/.
- McCarthy B, Casey D, Devane D, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;2015(2):1465. http://doi.wiley.com/10.1002/14651858.CD003793.pub3.
- Vorrink SNW, Kort HSM, Troosters T, et al. Level of daily physical activity in individuals with COPD compared with healthy controls. Respir Res. 2011;12(1):1–8. https://pubmed.ncbi.nlm.nih.gov/21426563/ DOI:10.1186/1465-9921-12-33
- Walker PP, Burnett A, Flavahan PW, et al. Lower limb activity and its determinants in COPD. Thorax. 2008;63(8):683–689. https://pubmed.ncbi.nlm.nih.gov/18487318/ DOI:10.1136/thx.2007.087130
- Hernandes NA, Teixeira D de C, Probst VS, et al. Profile of the level of physical activity in the daily lives of patients with COPD in Brazil. J Bras Pneumol. 2009;35(10):949–956. https://pubmed.ncbi.nlm.nih.gov/19918626/ DOI:10.1590/S1806-37132009001000002
- Pitta F, Troosters T, Spruit MA, et al. Characteristics of physical activities in daily life in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;171(9):972–977. http://www.atsjournals.org/doi/abs/10.1164/rccm.200407-855OC DOI:10.1164/rccm.200407-855OC
- Watz H, Waschki B, Meyer T, et al. Physical activity in patients with COPD. Eur Respir J. 2009;33(2):262–272. DOI:10.1183/09031936.00024608
- Watz H, Pitta F, Rochester CL, et al. An official European Respiratory Society statement on physical activity in COPD. Eur Respir J. 2014;44(6):1521–1537. http://www.ncbi.nlm.nih.gov/pubmed/25359358 DOI:10.1183/09031936.00046814
- Waschki B, Kirsten A, Holz O, et al. Physical activity is the strongest predictor of all-cause mortality in patients with COPD: a prospective cohort study. Chest. 2011;140(2):331–342. http://www.ncbi.nlm.nih.gov/pubmed/21273294 DOI:10.1378/chest.10-2521
- Garcia-Aymerich J, Lange P, Benet M, et al. Regular physical activity modifies smoking-related lung function decline and reduces risk of chronic obstructive pulmonary disease: A population-based cohort study. Am J Respir Crit Care Med. 2007;175(5):458–463. http://www.ncbi.nlm.nih.gov/pubmed/17158282 DOI:10.1164/rccm.200607-896OC
- Garcia-Aymerich J, Farrero E, Félez MA, Estudi del Factors de Risc d'Agudització de la MPOC investigators, et al. Risk factors of readmission to hospital for a COPD exacerbation: A prospective study. Thorax. 2003;58(2):100–105. DOI:10.1136/thorax.58.2.100
- Garcia-Aymerich J, Lange P, Benet M, et al. Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: A population based cohort study. Thorax. 2006;61(9):772–778. DOI:10.1136/thx.2006.060145
- Thorpe O, Kumar S, Johnston K. Barriers to and enablers of physical activity in patients with COPD following a hospital admission: a qualitative study. Int J COPD. 2014;9:115–128. https://pubmed.ncbi.nlm.nih.gov/24489465/.
- Batista Amorim P, Stelmach R, Ricardo Fernandes Carvalho C, et al. Barriers associated with reduced physical activity in COPD patients* Barreiras associadas à menor atividade física em portadores de DPOC. J Bras Pneumol. 2014;40(5):504–512. DOI:10.1590/S1806-37132014000500006
- Troosters T, Sciurba F, Battaglia S, et al. Physical inactivity in patients with COPD, a controlled multi-center pilot-study. Respir Med. 2010;104(7):1005–1011. https://pubmed.ncbi.nlm.nih.gov/20167463/ DOI:10.1016/j.rmed.2010.01.012
- Van Remoortel H, Hornikx M, Demeyer H, et al. Daily physical activity in subjects with newly diagnosed COPD. Thorax. 2013;68(10):962–963. https://pubmed.ncbi.nlm.nih.gov/23604460/ DOI:10.1136/thoraxjnl-2013-203534
- Gouzi F, Préfaut C, Abdellaoui A, et al. Evidence of an early physical activity reduction in chronic obstructive pulmonary disease patients. Arch Phys Med Rehabil. 2011;92(10):1611–1617.e2. https://pubmed.ncbi.nlm.nih.gov/21861985/ DOI:10.1016/j.apmr.2011.05.012
- Kosteli M-C, Heneghan N, Roskell C, et al. Barriers and enablers of physical activity engagement for patients with COPD in primary care. Int J Chron Obstruct Pulmon Dis. 2017;12:1019–1031. https://www.dovepress.com/barriers-and-enablers-of-physical-activity-engagement-for-patients-wit-peer-reviewed-article-COPD DOI:10.2147/COPD.S119806
- Hayton C, Clark A, Olive S, et al. Barriers to pulmonary rehabilitation: characteristics that predict patient attendance and adherence. Respir Med. 2013;107(3):401–407. DOI:10.1016/j.rmed.2012.11.016
- Ramboll RMCS by. SurveyXact. Available from: https://www.surveyxact.dk/.
- Klarlund BA. Fysisk aktivitet Håndbog om forebyggelse og behandling. 2018. Available from: https://www.sst.dk/-/media/Udgivelser/2018/Fysisk-aktivitet-håndbog-og-traening/Fysisk-aktivitet-–-håndbog-om-forebyggelse-og-behandling.ashx.
- Forsøgstyper uden anmeldelsespligt//Videnskabsetisk Komite - Region Syddanmark. Available from: https://komite.regionsyddanmark.dk/wm428123.
- Retsinformation. Available from: https://www.retsinformation.dk/eli/lta/2020/1338.
- Hvad skal jeg anmelde? | National Videnskabsetisk Komité. Available from: https://www.nvk.dk/forsker/naar-du-anmelder/hvilke-projekter-skal-jeg-anmelde.
- Årsrapport A til N. Dansk Register for Kronisk Obstruktiv Lungesygdom. 2016.
- Donaire-Gonzalez D, Gimeno-Santos E, Balcells E, et al. Physical activity in COPD patients: Patterns and bouts. Eur Respir J. 2013;42(4):993–1002. http://ow.ly/nug7kwww.erj.ersjournals.comThisarticlehassupplementarymaterialavailablefromwww.erj.ersjournals.com DOI:10.1183/09031936.00101512
- Pitta F, Troosters T, Probst VS, et al. Quantifying physical activity in daily life with questionnaaires and motion sensors in COPD. Eur Respir J. 2006;27(5):1040–1055. https://pubmed.ncbi.nlm.nih.gov/16707399/ DOI:10.1183/09031936.06.00064105
- Hartman JE, ten Hacken NHT, Boezen HM, et al. Self-efficacy for physical activity and insight into its benefits are modifiable factors associated with physical activity in people with COPD: A mixed-methods study. J Physiother. 2013;59(2):117–124. DOI:10.1016/S1836-9553(13)70164-4
- Lewis R, Cramp F. Facilitators and barriers to exercise maintenance in chronic obstructive pulmonary disease: Patient views. Physiother Pract Res. 2010;31(2):19–24. DOI:10.3233/PPR-2010-31205
- Hill K, Geist R, Goldstein RS, et al. Anxiety and depression in end-stage COPD. Eur Respir J. 2008;31(3):667–677. DOI:10.1183/09031936.00125707
- Schönhofer B, Ardes P, Geibel M, et al. Evaluation of a movement detector to measure daily activity in patients with chronic lung disease. Eur Respir J. 1997;10(12):2814–2819. http://www.ncbi.nlm.nih.gov/pubmed/9493666 DOI:10.1183/09031936.97.10122814
- Jakes RW, Day NE, Patel B, et al. Physical inactivity is associated with lower forced expiratory volume in 1 second : European Prospective Investigation into Cancer-Norfolk Prospect… - PubMed - NCBI. Available from: https://www.ncbi.nlm.nih.gov/pubmed/12117705.
- Garcia-Aymerich J, Félez MA, Escarrabill J, et al. Physical activity and its determinants in severe chronic obstructive pulmonary disease. Med Sci Sports Exerc. 2004;36(10):1667–1673. http://journals.lww.com/00005768-200410000-00002 DOI:10.1249/01.mss.0000142378.98039.58
- Pitta F, Takaki MY, Oliveira N. d, et al. Relationship between pulmonary function and physical activity in daily life in patients with COPD. Respir Med. 2008;102(8):1203–1207. DOI:10.1016/j.rmed.2008.03.004
- Garcia-Rio F, Lores V, Mediano O, et al. Daily physical activity in patients with chronic obstructive pulmonary disease is mainly associated with dynamic hyperinflation. Am J Respir Crit Care Med. 2009;180(6):506–512. https://pubmed.ncbi.nlm.nih.gov/19542481/ DOI:10.1164/rccm.200812-1873OC
- Sabit R, Griffiths TL, Watkins AJ, et al. Predictors of poor attendance at an outpatient pulmonary rehabilitation programme. Respir Med. 2008;102(6):819–824. DOI:10.1016/j.rmed.2008.01.019
- Young P, Dewse M, Fergusson W, et al. Respiratory rehabilitation in chronic obstructive pulmonary disease: Predictors of nonadherence. Eur Respir J. 1999;13(4):855–859. DOI:10.1034/j.1399-3003.1999.13d27.x
- Fischer MJ, Scharloo M, Abbink JJ, et al. Drop-out and attendance in pulmonary rehabilitation: The role of clinical and psychosocial variables. Respir Med. 2009;103(10):1564–1571. DOI:10.1016/j.rmed.2008.11.020
- Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis. 2011;8(2):89–99. http://journals.sagepub.com/doi/10.1177/1479972310393756 DOI:10.1177/1479972310393756
- Miravitlles M, Anzueto A, Legnani D, et al. Patient’s perception of exacerbations of COPD-the PERCEIVE study. Respir Med. 2007;101(3):453–460. DOI:10.1016/j.rmed.2006.07.010
- Salmon J, Crawford D, Owen N, et al. Physical activity and sedentary behavior: a population-based study of barriers, enjoyment, and preference. Health Psychol. 2003;22(2):178–188. DOI:10.1037/0278-6133.22.2.178
- Breyer MK, Breyer-Kohansal R, Funk GC, et al. Nordic Walking improves daily physical activities in COPD: A randomised controlled trial. Respir Res. 2010;11(1):112. DOI:10.1186/1465-9921-11-112
- Lahham A, McDonald C, Holland AE. Exercise training alone or with the addition of activity counseling improves physical activity levels in copd: A systematic review and meta-analysis of randomized controlled trials. Int J Chron Obstruct Pulmon Dis. 2016;11:3121–3136. DOI:10.2147/COPD.S121263
- Spruit MA, Singh SJ, Garvey C, et al. An official American thoracic society/European respiratory society statement: Key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–e64. https://pubmed.ncbi.nlm.nih.gov/24127811/ DOI:10.1164/rccm.201309-1634ST
- Mcnamara RJ, Epsley C, Coren E, et al. Singing for adults with chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. 2017;12:CD012296. https://pubmed.ncbi.nlm.nih.gov/29253921/.
- Engen RL. The singer’s breath: Implications for treatment of persons with emphysema. J Music Ther. 2005;42(1):20–48. https://pubmed.ncbi.nlm.nih.gov/15839731/ DOI:10.1093/jmt/42.1.20
- Skingley A, Page S, Clift S, et al. “Singing for Breathing”: Participants’ perceptions of a group singing programme for people with COPD. Arts Health 2014;6(1):59–74. https://www.tandfonline.com/doi/abs/10.1080/17533015.2013.840853 DOI:10.1080/17533015.2013.840853
- Holland AE, Hill CJ, Jones AY, et al. Breathing exercises for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;10:CD008250. https://pubmed.ncbi.nlm.nih.gov/23076942/.
- Lewis A, Cave P, Stern M, et al. Singing for Lung Health - A systematic review of the literature and consensus statement. Npj Prim Care Resp Med. 2016;26(1):26. www.nature.com/npjpcrm DOI:10.1038/npjpcrm.2016.80
- McNaughton A, Weatherall M, Williams M, et al. Sing Your Lungs Out - A community singing group for chronic obstructive pulmonary disease: A 1-year pilot study. BMJ Open. 2017;7(1):e014151. http://bmjopen.bmj.com/ DOI:10.1136/bmjopen-2016-014151
- Wshah A, Butler S, Patterson K, et al. “let’s Boogie”: FEASIBILITY of A DANCE INTERVENTION in PATIENTS with CHRONIC OBSTRUCTIVE PULMONARY DISEASE. J Cardiopulm Rehabil Prev. 2019;39(5):E14–E19. https://pubmed.ncbi.nlm.nih.gov/31465308/ DOI:10.1097/HCR.0000000000000428
- Ward DS, Evenson KR, Vaughn A, et al. Accelerometer Use in Physical Activity: Best Practices and Research Recommendations. Med Sci Sports Exerc. 2005;37(11 Suppl):S582–S588. http://journals.lww.com/00005768-200511001-00011 DOI:10.1249/01.mss.0000185292.71933.91