Abstract
In this pilot feasibility randomized controlled trial, participants with moderate to severe COPD were randomized to a 12-week tai chi or MBB intervention. Participants were assessed at baseline, 12 weeks, and 24 weeks. Feasibility, as assessed by intervention adherence, was the primary outcome. We also estimated preliminary between-group differences in COPD symptoms and health-related quality of life, cognitive-emotional function, and functional status across three timepoints: baseline, 12, and 24 weeks. A total of 92 participants were randomized 2:1 to tai chi (n = 61) or MBB (n = 31). The overall group adherence in the first 12 weeks was 62% in tai chi and 75% in MBB. From baseline to 12 weeks, tai chi demonstrated greater improvements in depressive symptoms (Cohen’s d effect size (ES) = −.53; adj mean diff = −2.31 [-5.7, 1.07]), 6-minute walk test distance (ES = .47; adj mean diff = 62.04 [2.85, 121.22]), social support (ES = .36; adj mean diff = .19 [-0.11, 0.49]) and chair stand (ES = .44; adj mean diff = .91 [-0.05, 1.86]). Only improvements in social support were maintained at 24-week follow-up. Tai chi and MBB are feasible for individuals with COPD. Preliminary effects suggest that while our mindful breathing intervention may not be sufficient to impact outcomes, tai chi may result in short-term benefits in mood, social support and functional capacity. More work is needed to better understand mindful breathing for COPD and to examine methods for maintaining improvements from tai chi over time.
Supplemental data for this article is available online at https://doi.org/10.1080/15412555.2021.1928037 .
Introduction
Chronic obstructive pulmonary disease (COPD), a progressive respiratory disease characterized by declines in lung function, affects nearly 16 million adults in the USA and is a leading cause of death [Citation1]. Individuals with COPD experience worsening dyspnea, exercise intolerance, and subsequent reductions in physical activity. Notably, lower levels of physical activity, independent of lung function, are associated with a higher risk of hospital admissions and readmissions, acute exacerbations, and death [Citation2–7]. Complicating the clinical picture, individuals with COPD have psychological comorbidities, including higher rates of anxiety and depression than the general population, which contribute to poor disease outcomes, lower levels of quality of life, and poor self-care behaviors [Citation8, Citation9]. There is a well-described interaction between anxiety and dyspnea that contributes to a spiral of disability and functional decline [Citation10].
Mind-body interventions may be well-suited for addressing the complex biopsychosocial effects of COPD on patients. One common component to many mind-body interventions is mindful breathing, which is particularly relevant to patients with COPD. Conventional breathing retraining exercises, which typically do not include an explicit mindfulness focus, are incorporated into conventional pulmonary rehabilitation programs and may include pursed-lip breathing and some elements of diaphragmatic breathing. Pursed lip breathing may improve breathlessness, the mechanical function of the lungs, and exercise capacity [Citation11–13]. However, there is also inconsistent evidence, particularly for diaphragmatic breathing, in terms of benefits to dyspnea, quality of life, and some pulmonary parameters (e.g. ventilation, chest wall motion) [Citation11–14]. Breathing techniques that integrate mindfulness may be particularly helpful for patients with COPD. These techniques include a nonjudgmental awareness of the somatic and psychological processes associated with the breath to help individuals breathe more efficiently. Few studies have examined mindful breathing, specifically. Yogic breathing was shown to be associated with improved exercise tolerance and forced expiratory volume in one second (FEV1) in individuals with COPD [Citation13, Citation15, Citation16], while two studies that combined mindful attention with breathing exercises found no improvements across several physical (e.g. dyspnea, exercise tolerance) and psychological (e.g. emotional function) outcomes [Citation17, Citation18]. More rigorous research is needed to understand the effects of mindful breathing techniques for patients with COPD.
Tai chi is a multimodal mind-body approach that integrates several components relevant to COPD management, including low-impact physical activity, strength training, postural control training, and various mindful breathing techniques. Preliminary research suggests that tai chi may improve both physiological and psychosocial symptoms associated with COPD, including exercise tolerance, anxiety and depressive symptoms, and quality of life [Citation19–21]. In one of the largest studies to date, Polkey and colleagues [Citation22] found that tai chi may be equivalent to pulmonary rehabilitation for dyspnea, strength, and exercise capacity, but not lung function (i.e. FEV1, forced vital capacity [FVC]). While tai chi appears promising for COPD management, the value of the mindful breathing component is not well understood.
Therefore, as a first step toward addressing this research gap, and given the potential relevance of mindful breathing for this pulmonary population, the current study compared tai chi to an intervention comprising the mindful breathing component of tai chi only. Understanding the relative effects of these two approaches may inform the application of mind-body interventions as therapeutic options for COPD management. Indeed, results may provide preliminary information regarding a simplified intervention focused on mindful breathing techniques as a potential stand-alone mind-body approach for individuals with COPD. Moreover, this study may provide preliminary insights regarding active treatment components in tai chi, particularly the relevance of mindful breathing in an overall tai chi program. The aim of the current pilot study was to examine the feasibility (i.e. adherence) and preliminary effect estimates of a mind-body breathing (MBB) intervention, compared to a tai chi program that includes MBB, with respect to COPD symptoms and health-related quality of life (HRQL), cognitive-emotional function, and functional status. Findings from the current study will be used to inform hypotheses and guide the development of a fully-powered randomized controlled trial (RCT) to understand the impact of these mind-body approaches.
Materials and method
Study design
This analysis focuses on the exploratory comparison of tai chi versus MBB, within a larger 3-arm pilot RCT examining the effects of a 12-week tai chi program versus an attention-matched education control or a 12-week MBB program. Results from the primary comparison (tai chi versus education control), including a priori benchmarks for overall study feasibility, are presented elsewhere [Citation23]. A randomized subset of tai chi participants also received an additional 12 weeks of tai chi “maintenance” classes. Participants in all groups were assessed at baseline, 12 weeks, and 24 weeks. Research staff performing the assessments were blinded to treatment group.
Eligibility, recruitment, and randomization
Individuals with moderate-severe COPD were eligible to participate. Moderate-severe COPD was defined as: 1) GOLD (Global Obstructive Lung Disease) stage 2, 3 or 4 with symptoms of dyspnea (either FEV1 ≤ 80% and FEV1/FVC <0.70, or computed tomography [CT] evidence of emphysema) and 2) age ≥ 40 years. Individuals were excluded if they had: 1) respiratory failure or GOLD stage 4 and were unable to perform a six-minute walk test (6MWT); 2) a COPD exacerbation in the past two weeks that required steroids, antibiotics, emergency department visit or hospitalization; 3) thoracic surgery within the subsequent 3 months; 4) hypoxemia on cardiopulmonary exercise test or 6MWT (oxygen saturation < 88% on supplemental oxygen at the end of the walk test); 5) vascular or other neuromuscular conditions resulting in an inability to ambulate; 6) indicators of unstable cardiovascular disease (i.e. electrocardiogram [EKG] changes on cardiopulmonary exercise test or chest pain on 6MWT); 7) severe cognitive problems (i.e. Mini-Mental Status Exam ≤ 24); 8) current regular tai chi practice or participation in a pulmonary rehabilitation program; 9) unstable or untreated clinical depression; or 10) non-English speaking status.
All study procedures were approved by each institution’s human subjects review board (BIDMC 2010 P-000412; VA 2540). Potential participants in primary care and pulmonary clinics were identified (August 2011–June 2015) through hospital databases at three large academic medical centers in Boston: Beth Israel Deaconess Medical Center, VABoston Healthcare System, and Boston Medical Center. Individuals deemed potentially eligible through screening were sent a recruitment letter and contacted via telephone. Participants provided written informed consent and were randomized in a 2:1:1 ratio after baseline testing to tai chi, MBB, or education control (data not included here). After week 12 testing, participants in the tai chi group were further randomized to an additional tai chi maintenance class or usual care. A study biostatistician performed the randomization procedures; groups were assigned using a permuted blocks method with randomly varying block sizes of 4 and 8. Group assignments were sealed in sequentially numbered opaque envelopes and study staff randomized each participant by opening the next numbered envelope.
Interventions
The tai chi and MBB classes were held twice per week (1 h per class) for a total of 12 weeks. After the week-12 assessment period, tai chi participants randomized to “maintenance” tai chi attended one additional class per week for 12 more weeks. Three instructors led both the tai chi and MBB classes to minimize the effects of instructor personality and teaching style between groups. Each instructor had previously completed a formal training program, had an average of 19 years of experience teaching tai chi, had prior experience working with medical populations, and were trained (by PMW) in the tai chi and MBB protocols. Treatment fidelity was tracked via an instructor checklist for each class. Participants in each group continued to receive their usual care, which included regularly scheduled provider visits and medications according to American Thoracic Society guidelines for managing COPD [Citation24].
Tai Chi
Complete details regarding the development and content of the tai chi intervention are published elsewhere [Citation25]. Briefly, the 12-week program was designed to meet the needs of older, physically limited adults with COPD. Five core tai chi movements, rooted in the traditional Cheng Man-Ch’ing’s Yang-style short form, were included in the intervention - “raising the power,” “withdraw and push,” “grasp the sparrow’s tail,” “brush knee twist step,” and “cloud hands.” Four mind-body breathing techniques were integrated throughout the interventions: 1) “Renewing the Body with the Breath,” which emphasizes relaxation, body and breath awareness, and imagery to systematically scan the whole body and release tension; 2) “Mindful Breathing,” which emphasizes mental focus, interoception, and awareness of the mechanisms of breathing; 3) “Dan Tien Breathing” or “Ocean Breathing,” which combines diaphragmatic breathing with imagery and simple arm movements mirroring movement of the abdomen; and 4) “Balloon Breathing,” which extends the previous practice by extending the period of exhalation. Each class also included traditional tai chi warm-up and cool-down exercises. Participants were encouraged to practice at home for an additional three times per week for 30 min; they were provided with a 45-minute DVD and audio file to encourage this home practice.
Individuals randomized to receive additional “maintenance” tai chi reviewed and practiced material from the first 12 weeks; no new material was introduced at this time.
Mind-body breathing
The MBB intervention was designed to focus primarily on the four breathing techniques described above, without integrating them with the tai chi movements and warm-up and cool-down exercises. Mindful awareness of breath was emphasized in each of the techniques. The 12-week MBB intervention was matched to tai chi in total class time (1 h weekly); however, the time spent on breathing techniques was relatively increased. In addition to seated practice of the breathing techniques, participants practiced using the techniques in the context of simulated activities of daily living (e.g. having a phone conversation, washing the dishes). Participants in the MBB group were also encouraged to practice at home three additional times per week for 30 min; they were provided with a 45-minute DVD and audio file that mirrored the breathing exercises taught in class to facilitate home practice.
Outcome measures
Intervention feasibility and safety monitoring
The focus of this analysis was on intervention feasibility once enrolled (i.e. class attendance and home practice completion). Results on the overall study feasibility (e.g. willingness to participate, rates of recruitment) are presented elsewhere [Citation23]. Intervention feasibility was assessed via class attendance and home practice. Class attendance in each group was tracked by study staff. Based on class attendance, the a priori benchmark for intervention feasibility was a majority of participants with ≥ 70% class attendance. For the first 12 weeks, adherence to home practice was assessed using home practice logs that tracked the frequency and duration of practice. For the second 12 weeks, home practice continued to be assessed via logs at each class in the tai chi maintenance group, and all other participants (i.e. participants who only completed the first 12 weeks of tai chi and MBB) reported their home practice once a month to study staff via telephone calls.
Adverse events were systematically tracked in both groups. Throughout the 12-week intervention period, participants were asked about new symptoms and changes in symptoms at each class. At the 12- and 24-week testing visits, participants were asked about emergency department visits, hospitalizations, and medical symptoms in the past 12 weeks. Queried medical symptoms included dizziness, muscle strain, fatigue, shortness of breath or COPD exacerbation, palpitations, falls, and psychological stress. We documented relatedness to the study, severity, change in medications, and additional medical or hospital visits for all events. If a serious adverse event occurred, which was defined by the Institutional Review Board as life-threatening, requiring hospitalization, or resulting in significant disability/incapacity, we conducted medical record reviews to obtain additional details.
Health-related quality of life and dyspnea
Chronic respiratory disease questionnaire (CRQ)
The CRQ is a 20-item self-report measure that assesses disease-specific HRQL. The total score and four subscales (i.e. dyspnea, fatigue, emotional function, mastery) were used in the current study [Citation26, Citation27].
University of California, San Diego shortness of breath questionnaire (USCD SOB)
The UCSD SOB is a 24-item self-report measure that assesses perceived shortness of breath while performing several activities of daily living [Citation28].
Cognitive-emotional
COPD self-efficacy scale (CSES)
The CSES is a 34-item self-report measure that assesses one’s confidence in managing or avoiding breathing difficulties across several different areas: times of negative affect, intense emotions, physical exertion, at-risk behaviors, and adverse weather/environment conditions. Items are rated on a 5-point Likert scale (1 = very confident to 5 = not at all confident) with higher scores reflecting lower confidence. The CSES has demonstrated good psychometric properties [Citation29].
Center of epidemiology studies – depression scale (CES-D)
The CES-D is a well-validated self-report measure that assesses depressive symptoms [Citation30]. Scores > 15 are indicative of significant depressive symptoms. The CES-D has demonstrated good psychometric properties [Citation31, Citation32].
Multidimensional scale of perceived social support (MSPSS)
The MSPSS is a well-validated 12-item self-report measure that assesses one’s perceived social support within their existing social network (i.e. family, friends, significant others) [Citation33].
Functional status
Six-minute walk test (6MWT)
The 6MWT is a standardized measure of exercise capacity that assesses the maximum distance walked in six minutes [Citation34]. The test was performed according to American Thoracic Society (ATS) guidelines, with no practice test administered to minimize participant burden [Citation35]. Participants were able to stop when needed. Participants who were prescribed oxygen with exercise utilized their physician prescribed flow rate during the walk test. The 6MWT is an independent predictor of COPD prognosis and survival [Citation36].
30-second chair stand test
The chair stand test is a validated assessment used to measure lower body strength and endurance. Participants are instructed to fold their arms, rise to a standing position, and return to a seated position as many times as possible in 30 s [Citation37].
Chair sit and reach
Commonly used in older or deconditioned populations, the chair sit and reach was used to assess lower body flexibility, primarily in the hamstrings (distance (inches) from toe to end of fingers) [Citation38].
Patient-Reported Outcome Measurement Information System Fatigue Short Form 7a (PROMIS-Fatigue)
The PROMIS-Fatigue is a well-validated self-report measure used to assess functional fatigue [Citation39].
Community Health Activities Model Program for Seniors Physical Activity Questionnaire for Older Adults (CHAMPS)
The CHAMPS is a well-validated 41-item self-report measure that assesses physical activity across several domains (i.e. leisure, household, occupational) [Citation40]. Participants report weekly frequency and total time spent in physical activities, which is used to estimate caloric expenditure (in kilocalories per week).
Other data collection
Sociodemographic information, spirometry, and lung volumes were collected at baseline. The BODE index (FEV1% predicted, 6MWT distance, modified Medical Research Council dyspnea score, body mass index) [Citation41] and multiple comorbidities from the Charlson Comorbidity Index [Citation42] were calculated at baseline. Spirometry was performed using rolling-seal volume displacement spirometers (Collins GS or CPL) by respiratory therapists or physicians following American Thoracic Society standards [Citation43]. Participants performed three acceptable spirometry efforts; each spirometry effort was repeated after inhalation of two puffs (180 mcg) of albuterol. FEV1 and FEV1/FVC were measured in the current study. Lung volumes were measured via plethysmography, a pressure-based volume measurement technique using Boyle’s law using pressure transducers and a pneumotachograph (Collins Box2). Expiratory reserve volume (ERV), inspiratory capacity (IC), total lung capacity (TLC), and IC/TLC were measured.
Statistical analysis
Adherence and safety
Given the pilot nature of this study, feasibility (i.e. adherence) was the primary outcome. Adherence to each class and home practice were assessed using descriptive statistics. Safety was assessed via the number of reportable and non-reportable adverse events per group.
Preliminary estimates of effects
As part of the larger trial with three arms (tai chi vs. education vs. MBB), the tai chi vs. MBB comparison was a prespecified exploratory comparison and was therefore not fully powered to detect between-group differences. Therefore, in line with guidelines for pilot trials, rather than assess efficacy and statistical significance, analyses focused on effect sizes and confidence intervals to inform the development of future trials [Citation44–47].
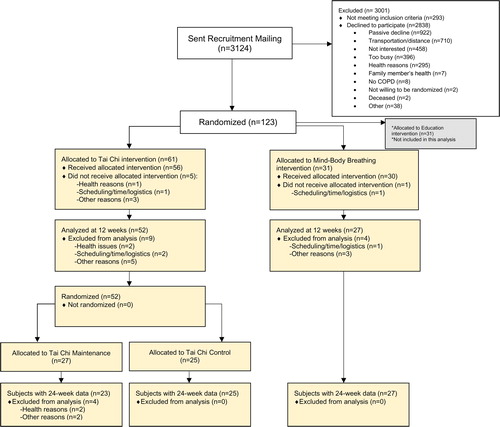
We estimated effect sizes (standardized differences between groups) by comparing change scores between groups (baseline to 12 weeks, 12 to 24 weeks) and calculating Cohen’s d [Citation48]. We calculated confidence intervals (95%) for Cohen’s d using Hedges and Olkin’s [Citation49] formula for confidence intervals for standardized differences. For the 12- to 24-week effect sizes, analyses were separated for the tai chi participants who received and did not receive additional maintenance classes. In these analyses, to match the comparison of 12-week intervention, followed by 12-week follow-up, we included participants who received only 12 weeks of tai chi total (n = 25). To further inform hypotheses regarding the effects of additional tai chi maintenance classes, we also estimated effect sizes by comparing change scores from baseline to 24 weeks between those in the tai chi group who also received additional maintenance classes (i.e. received additional tai chi from 12 to 24 weeks; n = 27) to those in the MBB group. Further, we used generalized estimating equations to estimate the difference in mean changes between groups from baseline and 12 weeks, 12 and 24 weeks, and baseline and 24 weeks, adjusting for baseline values that were imbalanced between the three treatment groups (i.e. tai chi, MBB, education) at baseline: Charlson comorbidity index, CES-D score, and BODE index. We included treatment group assignment, time point, and their interaction in each model as categorical variables. As demonstrated in the CONSORT (), we conducted analyses in subjects with complete data at each of the 12- and 24-week timepoints and we did not impute missing data. We conducted all analyses using SAS statistical software, version 9.4 (SAS Institute Inc., Cary, NC).
Results
Baseline characteristics
The trial CONSORT diagram focused on the tai chi and MBB arms is presented in . Baseline characteristics of each group are presented in . A total of 92 participants were randomized to tai chi (n = 61) or MBB (n = 31). The mean age of participants was 68.2 (SD = 8.7) and 66% were male. Participants had a mean FEV1% predicted of 58.4 (SD = 14.5) and mean tobacco pack years of 50.3 (SD = 37.6). Overall, 24% were GOLD stage 3-4 and 17% were on supplemental oxygen. Comorbidities included coronary artery disease (32%), cancer (21%), chronic musculoskeletal issues or back pain (51%), and significant limitation of an extremity (weakness or paralysis: 21%).
Table 1. Baseline sociodemographic and clinical characteristics.
Baseline values of FEV1% predicted, FEV1/FVC, ERV, IC, TLC are included in in each group. These lung testing parameters were relatively balanced across groups.
Adherence and safety
The overall group adherence (i.e. class attendance) in the first 12 weeks was 62% in the tai chi group and 75% in the MBB group. The majority of participants in both groups attended ≥ 70% of classes (59% in tai chi and 74% in MBB). Class and home practice adherence among those with available data (n = 50 in tai chi and n = 27 in MBB) are presented in . does not include participants who were further randomized to tai chi maintenance in the second 12 weeks. In the first 12 weeks, the tai chi group endorsed an average of 94.4 (SD = 75.8) minutes of home practice per week and the MBB endorsed 116.4 (SD = 117.7) minutes. In the follow-up period, those in the tai chi group logged an average of 68.8 (SD = 58.6) minutes of home practice per week and the MBB logged 88.0 (SD = 72.8) minutes. Those in the tai chi maintenance classes endorsed an average of 52.1 (SD = 50.4) minutes of home practice per week.
Table 2. Tai Chi and Mind-Body Breathing intervention adherence.
Reportable adverse events are summarized in . During the 12-week intervention period, a total of 16 reportable adverse events occurred in the tai chi group and none occurred in the MBB group. In the tai chi group, these included 7 COPD exacerbations and 12/16 (75%) were deemed unrelated to the study. Events that were possibly related in the tai chi group included musculoskeletal flares among those with a prior history of chronic pain and/or osteoarthritis. In the follow-up period, there were three reportable events in the MBB and 21 in the tai chi group. In the MBB group, these included 3 COPD exacerbations. In the tai chi group, these included 11 COPD exacerbations, 1 musculoskeletal flare, and 10 other events (see ). No events were deemed related in the tai chi or MBB groups in the follow-up period. Common expected symptoms that did not meet criteria for reporting to our IRB, including muscle soreness, dizziness/fainting, shortness of breath, fatigue, falls, palpitations, and psychological stress, were reported by 55/61(90%) subjects in tai chi and 28/31 (90%) in MBB.
Preliminary effect estimates
MBB vs. Tai Chi post-intervention (baseline to 12 weeks)
Results on the effects of tai chi and MBB on HRQL, cognitive-emotional measures, and functional status from baseline to 12 weeks are presented in . Overall, there were moderate between-group differences favoring tai chi in CES-D and the 6MWT distance, and small-moderate between-group differences favoring tai chi in chair stand and MSPSS. Calorie expenditure in moderate intensity exercises decreased in both groups, but less so in the tai chi group.
Table 3. Mean changes in health-related quality of life, cognitive-emotional measures, and functional status from baseline to 12 weeks in the Tai Chi and Mind-Body Breathing groups.
MBB vs. Tai Chi follow-up (12-24 weeks)
Follow-up effects from 12 to 24 weeks are presented in , including participants who only received the first 12 weeks of tai chi (n = 25). Tai chi continued to demonstrate improvements in MSPSS compared to MBB. However, compared to MBB, after the intervention ended, both COPD self-efficacy and the 6MWT distance declined in the tai chi group. There were small effects of improved CRQ-mastery and an increase in physical activity frequency (moderate-intensity exercise) in tai chi, while small between-group effects favored MBB in measures of fatigue (CRQ-fatigue and PROMIS-fatigue) and lower extremity strength (chair stand).
Table 4. Mean changes in health-related quality of life, cognitive-emotional measures, and functional status from 12 to 24 weeks in the Tai Chi and Mind-Body Breathing groups.
MBB vs. Tai Chi maintenance (baseline to 24 weeks)
Comparing those who received additional tai chi maintenance (24-week intervention total, n = 27) to those who received MBB (12-week intervention, 12-week follow up) from baseline to 24 weeks, there were moderate-large between-group effects favoring tai chi maintenance in CRQ-mastery (ES = 0.74; adjusted mean difference = 0.56) and chair stand (ES = 0.56; adjusted mean difference = 1.38).
Discussion
In the current pilot RCT, we aimed to estimate the feasibility (i.e. adherence) and preliminary effects of time- and attention-matched 12-week tai chi and MBB programs on COPD symptoms and HRQL, cognitive-emotional, and functional outcomes among individuals with moderate-severe COPD. As discussed elsewhere [Citation23], overall study feasibility (e.g. willingness to participate, recruitment rates) was suboptimal due to potential inefficiencies in our recruitment process. Once enrolled, however, class attendance and home practice rates suggest that both interventions were feasible, but overall class adherence and home practice were slightly higher in MBB than the tai chi group. These findings are consistent with previous work, which suggests that once participants are enrolled, tai chi programs adapted for individuals with respiratory diseases are feasible [Citation50, Citation51]. Excellent adherence rates for MBB also suggests that a mindful breathing program is feasible for individuals with COPD. Both interventions were safe with few reportable adverse events deemed related to the study. The four events deemed related or possibly related to tai chi included musculoskeletal flares. The overall percentage of participants reporting common expected symptoms was equal in both groups, which underscores the relatively debilitated and co-morbid population we studied. However, a higher percentage of participants in the tai chi group endorsed common symptoms related to exercise (e.g. muscle soreness, shortness of breath). Therefore, it is possible that class and home practice adherence was slightly lower in tai chi due to musculoskeletal flares and other common and expected symptoms related to exercise. While some symptoms are expected and unavoidable with any form of exercise, future work may consider further adapting tai chi for COPD to minimize uncomfortable exercise-related symptoms.
Nonetheless, at 12 weeks, there were modest improvements in depressive symptoms, exercise capacity, chair stand, and social support for tai chi compared to MBB. We observed minimal within-group improvements across most outcomes in the MBB group, including psychosocial outcomes, which is surprising. Further, there was an apparent small increase in depressive symptoms at 12 weeks. This suggests that mindful breathing alone may not be sufficient to impact these outcomes in 12 weeks among individuals with moderate-severe COPD. Indeed, extant work has demonstrated inconsistent findings on the effects that mind-body breathing interventions or mindfulness interventions with breathing components have in this population [Citation17, Citation18]. It is unclear if the specific breathing techniques chosen were not effective, the incorporation of breathing practice into activities of daily living was not helpful, or the time dedicated to certain exercises was sub-optimal. For example, it is possible that one-hour of breathing exercises was too long or even counterproductive. In contrast to the quantitative results from this analysis, results from qualitative analysis of exit interviews from this same study [Citation52] suggest that those in the tai chi and MBB groups equally endorsed themes related to improved internal locus of control and self-efficacy toward managing anxiety and dyspnea, greater emotion regulation and decreased reactivity, less emotional distress, improved physical function, and greater valuing of social interactions. Therefore, it is also possible that the quantitative outcomes in the current analysis did not effectively capture participants’ experience with the MBB group. Further, other mind-body interventions with a focus on breathing have been shown to be beneficial among individuals with COPD [Citation53]. Given these mixed findings, future work should continue to evaluate mindful and other mind-body breathing programs for individuals with COPD and might consider variables such as intervention dosage, the type of breathing exercises, and the ratio of various breathing exercises.
Once the classes ended, many of the positive effects of tai chi were not maintained in the follow-up period (12 to 24 weeks). Both exercise capacity and chair stand waned in the follow-up period in the tai chi group compared to MBB, suggesting that continued exercise is needed to maintain functional gains. Initial improvements in depressive symptoms for tai chi also did not appear to be maintained over the follow-up period. Of note, COPD self-efficacy and fatigue worsened from 12 to 24 weeks in the tai chi group, whereas there was no change in the MBB group. It is possible that the MBB intervention, while not producing positive gains in the first 12 weeks, acted as a buffer toward progressive declines in self-efficacy and fatigue typically seen in patients with COPD. However, compared to MBB, social support continued to improve in tai chi and there were small trends toward improvements in the mastery subscale of HRQL and the frequency of moderate intensity exercise in the follow-up period (12 to 24 weeks) that were not evident at post-intervention. Together, these results suggest that more than 12 weeks of tai chi may be needed to produce long-term changes in physical and psychosocial outcomes among individuals with moderate-severe COPD. Indeed, results from a separate analysis of data from the current pilot RCT (comparing tai chi with the education control) [Citation23], suggest that tai chi with additional booster or maintenance classes may be protective against decreases in exercise capacity and associated with increases in COPD self-efficacy compared to tai chi with no additional maintenance classes. Furthermore, results from the current analysis demonstrated that those who received an additional 12 weeks of tai chi maintenance improved in HRQL (CRQ-Mastery) and lower extremity strength over 24 weeks with potential improvements in other indices (e.g. depression, exercise capacity) compared to MBB. However, these results may simply be due to the extra time and attention the tai chi maintenance participants received compared to those in MBB (24 weeks vs. 12 weeks intervention). More research is needed to understand the most effective dose of tai chi to sustain effects and to examine whether a longer MBB intervention is needed to detect meaningful change.
One obvious difference between our two interventions is that the tai chi included integrated physical movement with mindful breathing and other mind-body strategies. While preliminary effects should be interpreted with caution due to the pilot nature of the current study, our results suggest that perhaps multimodal mind-body exercise approaches, which include physical movement, may offer short-term physical and psychosocial benefits for individuals with COPD over a more simplified intervention that focuses mainly on mindful breathing. While mindful breathing is theoretically relevant and promising, the mixed findings point to a more complex picture. Given the effects of interrelated biopsychosocial factors on morbidity in COPD [Citation8–10], integrated approaches (e.g. tai chi) that simultaneously target these factors (e.g. exercise capacity and depressive symptoms) may be particularly valuable. This is in line with research suggesting that other integrated mind-body movement interventions may confer physical and psychosocial benefits for individuals with respiratory diseases (e.g. yoga, dance) [Citation54–56]. Moreover, integrated mind-body exercise approaches may confer advantages over non-movement mind-body interventions for health behavior promotion, particularly physical activity promotion, which is crucial for individuals with COPD. Low-to-moderate intensity activity, combined with other mind-body strategies, may improve exercise capacity, increase self-efficacy for exercise, remove psychosocial barriers to exercise (e.g. depressive symptoms), enhance other self-regulatory processes (e.g. emotion regulation), and ultimately improve downstream physical activity levels [Citation57]. Results from the current study demonstrated potential improvements in the frequency of moderate intensity exercise in tai chi over the course of the 24 weeks. Larger, fully-powered studies are needed to assess the differential effects of mind-body exercise interventions and non-movement mind-body programs for health behavior promotion.
Findings from the current study offer tentative insights regarding active therapeutic ingredients in tai chi. Mindful breathing is one component in a multimodal tai chi intervention. Given the absence of substantive within-group change in the MBB group across most outcomes, it is possible that mindful breathing does not drive change in tai chi interventions. On the other hand, mindful breathing combined with physical activity may additively or synergistically influence outcomes. Consistent with this line of thinking, in studies that compare tai chi to physical activity control conditions, results suggest that tai chi may lead to more improvement across several outcomes (e.g. exercise capacity, positive affect) [Citation58–61]. Future research should further elucidate which components drive change in mind-body exercise interventions, and whether there are additive or synergistic effects of components (e.g. physical activity, mind-body breathing, mindfulness). Multiphase Optimization Strategy (MOST) study designs, which aim to identify active treatment components in multimodal interventions, may be particularly useful in this regard [Citation62].
The primary limitation of the current study was the small sample size. Since the publication of our protocol paper [Citation25], there has been a greater appreciation for the limitations of pilot studies and new guidelines for appropriately reporting results have been issued [Citation44–47]. We acknowledge we may have been underpowered to detect significant differences across multiple outcomes. In addition, the current study included a relatively short follow-up period. It is possible that MBB effects emerge gradually over longer periods of time. Indeed, we observed slightly higher home and total practice in the MBB group, suggesting that MBB is feasible to implement and sustain, which may confer longer-term benefits that were not captured in this study. Further, individuals with moderate-severe COPD without a severe exacerbation in the past two weeks were eligible for the study. Given the relatively short timeframe of two weeks, it is possible that individuals with more unstable disease were enrolled in the study, which may have impacted our results. Lastly, participants did not complete a practice 6MWT at baseline, which may have led to an overestimation of the treatment effect in both groups. However, given that the same 6MWT procedures were used across all participants, the lack of a practice test would not have contributed to differences between group. Despite these limitations, the current study provides rigorous preliminary data to guide future study development and informs hypotheses regarding the differential effects of integrated mind-body exercise and mindful breathing interventions for individuals with moderate-severe COPD.
Disclosure statement
Dr. Wayne reports grants from NIH (K24AT009282) during the conduct of the study. Dr. Yeh reports grants from NIH (R01AT005436; K24AT009465) during the conduct of the study; Dr. Kraemer reports support from NIH (T32AT000051) during the conduct of this study; This work was conducted with support from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL 1TR002541) and financial contributions from Harvard University and its affiliated academic healthcare centers. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, or the National Institutes of Health; All other authors report no conflicts of interest.
References
- Wheaton AG, Cunningham TJ, Ford ES, et al. Employment and activity limitations among adults with chronic obstructive pulmonary disease—United States, 2013. MMWR. Morb Mortal Weekly Rep. 2015;64(11):289.
- Moy ML, Teylan M, Weston NA, et al. Daily step count predicts acute exacerbations in a US cohort with COPD. PloS One. 2013;8(4):e60400. DOI:10.1371/journal.pone.0060400
- Nguyen HQ, Chu L, Amy Liu I-L, et al. Associations between physical activity and 30-day readmission risk in chronic obstructive pulmonary disease. Annals Ats. 2014;11(5):695–705. DOI:10.1513/AnnalsATS.201401-017OC
- Moy ML, Teylan M, Danilack VA, et al. An index of daily step count and systemic inflammation predicts clinical outcomes in chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2014;11(2):149–157. DOI:10.1513/AnnalsATS.201307-243OC
- Wan ES, Kantorowski A, Polak M, et al. Long-term effects of web-based pedometer-mediated intervention on COPD exacerbations. Respir Med. 2020;162:105878. DOI:10.1016/j.rmed.2020.105878
- Moy ML, Gould MK, Liu I-LA, et al. Physical activity assessed in routine care predicts mortality after a COPD hospitalisation. ERJ Open Res. 2016;2(1):00062-2015. DOI:10.1183/23120541.00062-2015
- Waschki B, Kirsten A, Holz O, et al. Physical activity is the strongest predictor of all-cause mortality in patients with COPD: a prospective cohort study. Chest. 2011;140(2):331–342. DOI:10.1378/chest.10-2521
- Yohannes AM, Alexopoulos GS. Depression and anxiety in patients with COPD. Eur Respir Rev. 2014;23(133):345–349. DOI:10.1183/09059180.00007813
- Coventry P, Panagioti M, Scott C, et al. Overview of the prevalence, impact, and management of depression and anxiety in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2014;9:1289–1306.
- Janssens T, De Peuter S, Stans L, et al. Dyspnea perception in COPD: association between anxiety, dyspnea-related fear, and dyspnea in a pulmonary rehabilitation program. Chest. 2011;140(3):618–625. DOI:10.1378/chest.10-3257
- Borge CR, Hagen KB, Mengshoel AM, et al. Effects of controlled breathing exercises and respiratory muscle training in people with chronic obstructive pulmonary disease: results from evaluating the quality of evidence in systematic reviews. BMC Pulm Med. 2014;14(1):184. DOI:10.1186/1471-2466-14-184
- Dechman G, Wilson CR. Evidence underlying breathing retraining in people with stable chronic obstructive pulmonary disease. Phys Ther. 2004;84(12):1189–1197. DOI:10.1093/ptj/84.12.1189
- Holland AE, Hill CJ, Jones AY, et al. Breathing exercises for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;(10): CD008250. doi:10.1002/14651858.CD008250.pub2
- Cahalin LP, Braga M, Matsuo Y, et al. Efficacy of diaphragmatic breathing in persons with chronic obstructive pulmonary disease: a review of the literature. J Cardiopulm Rehabil Prev. 2002;22(1):7–21.
- Cramer H, Haller H, Klose P, et al. The risks and benefits of yoga for patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Clin Rehabil. 2019;33(12):1847–1862. DOI:10.1177/0269215519860551
- Kaminsky DA, Guntupalli KK, Lippmann J, et al. Effect of yoga breathing (pranayama) on exercise tolerance in patients with chronic obstructive pulmonary disease: a randomized, controlled trial. J Altern Complement Med. 2017;23(9):696–704. DOI:10.1089/acm.2017.0102
- Chan RR, Giardino N, Larson JL. A pilot study: mindfulness meditation intervention in COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:445–454.
- Mularski RA, Munjas BA, Lorenz KA, et al. Randomized controlled trial of mindfulness-based therapy for dyspnea in chronic obstructive lung disease. J Altern Complement Med. 2009;15(10):1083–1090. DOI:10.1089/acm.2009.0037
- Ding M, Zhang W, Li K, et al. Effectiveness of t’ai chi and qigong on chronic obstructive pulmonary disease: a systematic review and meta-analysis. J Altern Complement Med. 2014;20(2):79–86. DOI:10.1089/acm.2013.0087
- Guo C, Xiang G, Xie L, et al. Effects of Tai Chi training on the physical and mental health status in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. J Thorac Dis. 2020;12(3):504. DOI:10.21037/jtd.2020.01.03
- Wu W, Liu X, Wang L, et al. Effects of Tai Chi on exercise capacity and health-related quality of life in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2014;9:1253–1263.
- Polkey MI, Qiu ZH, Zhou L, et al. Tai Chi and pulmonary rehabilitation compared for treatment-naive patients with COPD: a randomized controlled trial. Chest. 2018;153(5):1116–1124. DOI:10.1016/j.chest.2018.01.053
- Yeh GY, Litrownik D, Wayne PM, et al. BEAM study (Breathing, Education, Awareness, Movement): a randomised controlled feasibility trial of tai chi exercise in patients with COPD. BMJ Open Resp Res. 2020;7(1):e000697. DOI:10.1136/bmjresp-2020-000697
- Qaseem A, Wilt TJ, Weinberger SE, et al. Disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179–191. DOI:10.7326/0003-4819-155-3-201108020-00008
- Yeh GY, Wayne PM, Litrownik D, Roberts DH, et al. Tai chi mind-body exercise in patients with COPD: study protocol for a randomized controlled trial. Trials. 2014;15(1):337. DOI:10.1186/1745-6215-15-337
- Guyatt GH, Berman LB, Townsend M, et al. A measure of quality of life for clinical trials in chronic lung disease. Thorax. 1987;42(10):773–778. DOI:10.1136/thx.42.10.773
- Schünemann HJ, Puhan M, Goldstein R, et al. Measurement properties and interpretability of the Chronic respiratory disease questionnaire (CRQ). COPD: J Chron Obstruct Pulmon Dis. 2005;2(1):81–89. DOI:10.1081/copd-200050651
- Eakin EG, Resnikoff PM, Prewitt LM, et al. Validation of a new dyspnea measure: the UCSD Shortness of Breath Questionnaire. Chest. 1998;113(3):619–624. DOI:10.1378/chest.113.3.619
- Wigal JK, Creer TL, Kotses H. The COPD self-efficacy scale. Chest. 1991;99(5):1193–1196. DOI:10.1378/chest.99.5.1193
- Radloff LS, The CES. D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. DOI:10.1177/014662167700100306
- van Manen JG. Risk of depression in patients with chronic obstructive pulmonary disease and its determinants. Thorax. 2002;57(5):412–416. DOI:10.1136/thorax.57.5.412
- Himmelfarb S, Murrell SA. Reliability and validity of five mental health scales in older persons. J Gerontol. 1983;38(3):333–339. DOI:10.1093/geronj/38.3.333
- Zimet GD, Powell SS, Farley GK, et al. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. 1990;55(3–4):610–617. DOI:10.1207/s15327752jpa5503&4_17
- Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;15(8):919–923.
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–117.
- Cote CG, Casanova C, Marin JM, et al. Validation and comparison of reference equations for the 6-min walk distance test. Eur Respir J. 2008;31(3):571–578. DOI:10.1183/09031936.00104507
- Jones CJ, Rikli RE, Beam WC. A 30-s Chair-Stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport. 1999;70(2):113–119. DOI:10.1080/02701367.1999.10608028
- Jones CJ, Rikli RE, Max J, et al. The reliability and validity of a chair sit-and-reach test as a measure of hamstring flexibility in older adults. Res Q Exerc Sport. 1998;69(4):338–343. DOI:10.1080/02701367.1998.10607708
- Rose M, Bjorner JB, Becker J, Fries JF, et al. Evaluation of a preliminary physical function item bank supported the expected advantages of the Patient-Reported Outcomes Measurement Information System (PROMIS). J Clin Epidemiol. 2008;61(1):17–33. DOI:10.1016/j.jclinepi.2006.06.025
- Stewart AL, Mills KM, King AC, et al. CHAMPS Physical Activity Questionnaire for Older Adults: outcomes for interventions. Med Sci Sports Exerc. 2001;33(7):1126–1141.
- Celli BR, Cote CG, Marin JM, et al. The body-Mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(10):1005–1012. DOI:10.1056/NEJMoa021322
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40(5):373–383. DOI:10.1016/0021-9681(87)90171-8
- Miller MR, Hankinson J, Brusasco V, ATS/ERS Task Force, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–338. DOI:10.1183/09031936.05.00034805
- Eldridge SM, Chan CL, Campbell MJ, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ. 2016;355:i5239. DOI:10.1136/bmj.i5239
- Kistin C, Silverstein M. Pilot studies: A critical but potentially misused component of interventional research. JAMA. 2015;314(15):1561–1562. DOI:10.1001/jama.2015.10962
- Kraemer HC, Mintz J, Noda A, et al. Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry. 2006;63(5):484–489. DOI:10.1001/archpsyc.63.5.484
- Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011;45(5):626–629. DOI:10.1016/j.jpsychires.2010.10.008
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale (NJ): Erlbaum; 1988.
- Hedges LV, Olkin I. Statistical methods for meta-analysis. Orlando: Academic Press; 1985.
- Lewis A, Hopkinson NS. Tai Chi Movements for Wellbeing–evaluation of a British lung foundation pilot. Perspect Public Heal. 2020;140(3):172–180. DOI:10.1177/1757913919872515
- Yeh GY, Roberts DH, Wayne PM, et al. Tai chi exercise for patients with chronic obstructive pulmonary disease: a pilot study. Respir Care. 2010;55(11):1475–1482.
- Gilliam EA, Cheung T, Kraemer K, et al. The impact of Tai Chi and mind-body breathing in COPD: Insights from a qualitative sub-study of a randomized controlled trial. Plos One. 2021;16(4):e0249263. DOI:10.1371/journal.pone.0249263
- Lewis A, Cave P, Stern M, et al. Singing for Lung Health—a systematic review of the literature and consensus statement. NPJ Prim Care Respir Med. 2016;26(1):1–8.
- Philip KE, Lewis A, Williams S, et al. Dance for people with chronic respiratory disease: a qualitative study. BMJ Open. 2020;10(10):e038719. DOI:10.1136/bmjopen-2020-038719
- Philip KE, Akylbekov A, Stambaeva B, et al. Music, dance, and Harmonicas for people with COPD. Respir Care. 2019;64(3):359. DOI:10.4187/respcare.06701
- Wu LL, Lin ZK, Weng HD, Qi QF, et al. Effectiveness of meditative movement on COPD: a systematic review and meta-analysis. Int J Chron Obstruct Pulm Dis. 2018;13:1239. DOI:10.2147/COPD.S159042
- Kraemer KM, Luberto CM, Hall DL, et al. The role of mind–body approaches in promoting healthcare engagement and positive behavior change. In: Moy M, Blackstock F, Nici L, editors. Enhancing patient engagement in pulmonary healthcare. Cham: Humana; 2020. p. 157–182.
- Chan AW, Chair SY, Lee DT, et al. Tai Chi exercise is more effective than brisk walking in reducing cardiovascular disease risk factors among adults with hypertension: a randomised controlled trial. Int J Nurs Stud. 2018;88:44–52. DOI:10.1016/j.ijnurstu.2018.08.009
- Cox AE, Roberts MA, Cates HL, et al. Mindfulness and affective responses to treadmill walking in individuals with low intrinsic motivation to exercise. Int J Exerc Sci. 2018;11(5):609–624.
- Streeter CC, Whitfield TH, Owen L, et al. Effects of yoga versus walking on mood, anxiety, and brain GABA levels: a randomized controlled MRS study. J Altern Complement Med. 2010;16(11):1145–1152. DOI:10.1089/acm.2010.0007
- Yeh GY, Wood MJ, Wayne PM, et al. Tai chi in patients with heart failure with preserved ejection fraction. Congest Heart Fail. 2013;19(2):77–84. DOI:10.1111/chf.12005
- Collins LM, Murphy SA, Strecher V. The multiphase optimization strategy (MOST) and the sequential multiple assignment randomized trial (SMART): New methods for more potent eHealth interventions. Am J Prev Med. 2007;32(5):S112–S118. DOI:10.1016/j.amepre.2007.01.022