Abstract
Physical inactivity and peripheral muscle dysfunction are considered two of the main contributors to hospitalizations due to exacerbation and, above all, predictors of mortality for these requirements in patients with COPD. Therefore, longitudinal studies are needed to determine the impact of exacerbations during hospitalization on these two factors, especially after three months of hospital discharge. The objectives of the present study were to assess the level of physical activity in daily life (PADL) and isometric muscle strength of the quadriceps in patients hospitalized for exacerbation of COPD and to verify changes after 3 months of hospital discharge. This is a longitudinal observational study that assessed the PADL level with an accelerometer, after 24 h of the hospitalization and the beginning of the drug treatment and assessed the quadriceps muscle strength with a manual dynamometer, after 72 h of hospitalization, in 32 patients with COPD (66 ± 7.61 years), in addition to repeating both assessments with 30 days of hospital discharge and after 3 months of follow-up. Cognition, dyspnea, general health, physical performance and lung function were assessed to characterize the sample. As main results, there was increase in active time (344 ± 260 − 447 ± 199 min; p = 0.04) and number of steps (4.241 ± 374 − 6.216 ± 400 steps; p = 0.02) after three months. In addition, inactive time showed significant reduction 30 days after hospital discharge (1.151 ± 249 − 1.065 ± 198 min; p = 0.02). The level of physical activity showed significant improvement due to the increase in active time and number of steps after three months of hospital discharge and to the reduction of inactive time 30 days after hospital discharge.
Introduction
Chronic obstructive pulmonary disease (COPD) is mainly caused by smoking or inhaling harmful particles/gases, resulting in airflow limitation and persistent respiratory symptoms (cough, dyspnea and secretion). Although COPD is primarily pulmonary, individuals may experience extrapulmonary manifestations caused by the chronic inflammatory process and oxidative stress, as well as nutritional changes [Citation1].
The reduction in physical activity in daily life (PADL) is a striking feature of this population, considered one of the main observed systemic consequences [Citation2] since the beginning of the disease. In COPD, physical and behavioral factors influence physical activity, which is characterized by “any body movement produced by muscles that require energy expenditure.”
Thus, for an individual to be considered physically active, the recommendations proposed by the American College of Sports Medicine (ACSM) suggest at least 30 min/day of moderate to vigorous physical activity, with a frequency of at least 5 times/week or 20 min of vigorous activities, at least 3 time/week. For individuals who have worse physical condition, who have difficulty to perform physical activity continuously, the recommendations suggest physical activity lasting <10 min [Citation3] with a frequency of at least 3 times/week, however, individuals who walk less than 4.500 steps per day are considered physically inactive [Citation4].
For the population with COPD, physical inactivity is currently considered as one of the main contributing factors for cardiovascular morbidities, hospitalizations due to exacerbation and, above all, predictor of the causes of death in this population [Citation5]. Thus, it is important to assess the level of PADL in these individuals in order to characterize the evolution and the damage caused by the disease.
Coupled with the reduction of PADL, peripheral muscle dysfunction (PMD), particularly the quadriceps muscle, is one of the most frequent extrapulmonary manifestations in this population, which can be characterized as loss of muscle strength and/or resistance [Citation6]. The development of PMD is caused by numerous systemic factors such as muscle atrophy due to disuse, energy imbalance, local and systemic inflammation, hypoxia and hypercapnia, electrolyte dysfunction and use of corticosteroids [Citation7].
In addition to the systemic manifestations mentioned above, during the natural course of the disease, COPD is marked by episodes of exacerbations, defined as worsening of baseline respiratory and systemic symptoms, in addition to the expected daily variation, requiring additional therapies [Citation8]. Exacerbations have a negative impact in the short- and long-term on the health system, including higher costs/overload on the health system due to the increase in the number of admissions and hospital readmissions. For patients, impairment in health status includes acceleration of ventilatory decline, muscle strength and level of physical activity [Citation9,Citation10].
During hospitalization due to exacerbation of COPD, the inactive time (sitting/lying down), assessed by an accelerometer, increased to 86.7% [Citation11] and this is justified by numerous factors, including severity of the disease, worsening of symptoms and immobility in the hospital environment [Citation12]. In addition, the constant exacerbations of COPD also worsen the reduced muscle strength of the quadriceps, as in the study by Gayan-Ramirez and Decramer [Citation13], which observed that after the 3rd day of hospitalization quadriceps muscle strength is reduced and quadriceps cross-sectional area is reduced by 5% after the 5th day of hospitalization [Citation14,Citation15].
Corroborating these findings, a review study observed that there is a 20 to 30% reduction in the isometric strength of the quadriceps in patients with COPD when compared to healthy individuals [Citation16]. This reduction can lead to impairment in the performance of physical activities, such as walking or going up and down stairs [Citation17].
However, longitudinal studies are needed to determine the impact of exacerbations during hospitalization on the level of physical activity and quadriceps muscle strength beyond 30 days of hospital discharge [Citation11,Citation14,Citation18,Citation19]. This fact justifies the achievement and relevance of the present study, in order to identify and monitor the recovery of these patients for a period of three months, and thus identify the need for early therapeutic interventions, directed at the detected impairment, avoiding the occurrence of greater functional losses. Thus, the objectives of the present study were to assess the level of PADL and isometric muscle strength of the quadriceps in patients hospitalized for exacerbation of COPD and to verify changes after three months of hospital discharge.
Methods
Study design
This is a longitudinal observational clinical study that encompasses three evaluation moments: Hospitalization, 30 days and three months after hospital discharge. All participants were informed about the research objectives and procedures and signed a free and informed consent form (FICF) to participate in the study. As this is a non-experimental research, this was carried out according to the STROBE checklist – subsidies for the communication of observational studies.
Participants
In total, 42 patients were recruited between January 2018 and December 2019 at the UFSCar University Hospital, in São Carlos - SP, Brazil during hospitalization for exacerbation of COPD (48–72 h of medication). Inclusion criteria were patients COPD, confirmed by clinical diagnosis and performing medical and medication follow-up, with serious exacerbation according to the GOLD (Global Initiative for Chronic Obstructive Lung Disease, 2020) criteria, between 60 and 89 years of age, breathing spontaneously with or without supplemental oxygen, hemodynamic stability, absence of limitations that would not allow evaluations (orthopedic, rheumatological, cardiovascular, neuromuscular, vestibular, severe visual or neurological), BMI between ≤18 and ≥35 kg/m2, not regular drug users, not on mechanical ventilation and no other lung diseases and able to understand the proposed assessments (Mini Mental State Examination with a score ≥13). The following were excluded: patients who had arrhythmias and unstable changes in vital signs during the evaluations and who returned to hospital after 48 h of discharge. This study was approved by the Human Research Ethics Committee of the Federal University of São Carlos (CAAE: 23710519.2.0000.5504) and conducted in accordance with the Declaration of Helsinki.
Procedures
The sample was characterized by collecting the complete anamnesis, data on the history and current status of the disease, smoking history, anthropometric measurements, COPD Assessment Test (CAT) about the general health status related to COPD [Citation20], the modified Medical Research Council (mMRC) scale to evaluate the degree of dyspnea sensation in activities of daily living reported by the patient [Citation21] and the 6-Minute Walk Test (6MWT) to assess the physical performance of the individuals with COPD.
All these variables were colleted after 24 h of hospitalization for exacerbation, except the 6MWT that was colleted after 72 h. As these variables were only part of the characterization of the sample, they were collected only in the initial evaluation.
According to GOLD [Citation1], COPD exacerbations were classified as serious: requiring hospitalization or visits to emergency rooms, which may be related to acute respiratory failure.
One and three months after the hospital discharge the patients were contacted and assessed again all variables describe before. In one month after hospital discharge was also assessed the lung function by trained professionals using a portable spirometer (MicroQuark®) to confirm the spirometric diagnosis of COPD following the techniques recommended by the Brazilian Society of Pulmonology and Tisiology, (2002) for acceptability and reproducibility criteria. The severity of the disease was verified using the criteria after use of a bronchodilator (salbutamol 40 mcg), according to the GOLD classification (2020) [Citation1].
Physical performance
The six-minute walk test was evaluated according to the standardized technique established by the European Respiratory Society and American Thoracic Society [Citation22]. Thus, the distance covered was recorded at the end in meters, and to calculate the predicted distance the formula for Men was used: PD = (7.57 × height cm) − (5.02 × age) − (1.76 × weight Kg) − 309 m, and for Women: PD = (2.11 × height cm) − (2.29 × weight Kg) − (5.78 × age) + 667 m) [Citation23]. The percentage of the predicted value was used for the analysis.
Outcome variables
Monitoring the level of physical activity of daily life
The level of physical activity was checked using an accelerometer (activPAL3TM, PALTechnologies Ltd., Glasgow, United Kingdom). This evaluation was carried out 24 h after hospitalization and the beginning of the drug treatment, in which individuals should remain with the equipment for five days and removed in hospital discharge. In addition, it was performed after 30 days and three months of hospital discharge likewise.
Initially, the accelerometer was wrapped in plastic wrap paper and then placed under a transparent waterproof dressing (Tegaderm™ Roll) and fastened by a second transparent dressing (Hydrofilm Roll) in the middle third of the anterior region of the right thigh between the inguinal fold and the patella.
The ActivPALTM Professional software (Pal Technologies Ltd., 2013) was used to download and interpret the data. The data generated by the ActivPALTM Professional software was opened in Excel to calculate the daily time spent sitting/lying down, standing, walking and number of steps.
The data analysis considered the sum of standing and walking time as active time and sitting and lying down time as inactive time. In addition, the analysis considered data for the average of five days and at least 10 h for monitoring the level of physical activity during waking hours were also considered [Citation24].
Quadriceps muscle strength
The quadriceps muscle strength was measured using a manual dynamometer (Microfet 2®, Hoggan - Health Industries, West Jordan, UT, USA) on right lower limb. This evaluation was carried out 48 h after hospitalization. In addition, it was performed during hospitalization, after 30 days of hospital discharge and with 3 months of follow-up.
To perform the measurement, the patients were seated in an adjustable ergonomic chair, with their legs suspended at the edge of the chair, with their hips and knees flexed at 90°. Afterwards, the patients were instructed to keep their arms crossed over the chest during the test to avoid compensation of other muscle groups.
The dynamometer was fastened in the anterior distal portion of the tibia, with a height determined at 2 cm above the malleolus, under an inextensible nylon band fastened to the posterior region of the adjustable ergonomic chair. During the test, the dynamometer was stabilized by the evaluator in order to prevent possible displacements under the band.
The patients were instructed how to perform the test and underwent a maximum voluntary contraction (MVC) for familiarization. After that, the verbal command used during the evaluation was as follows: “breathe in the air and release, force, force, force!” During contraction, exhaling was requested in order to avoid a valsalva maneuver. After familiarizing with the measurement, patients underwent three maximum isometric contractions, each lasting 5 s and 60 s apart. The peak isometric force was expressed in Newton (N) and % of the predicted value [Citation25].
Data analysis
The sample size calculation was performed using the G * Power software (Version 3.1.9.2; Kiel University, Germany). The ANOVA test was used with repeated measures in the post-hoc modality, with the following parameters: Effect size of 0.44, significance level of 0.05, sample size of 24 individuals, resulting in test power of 0.74.
The results of the present study were analyzed using the Statistical Package for Social Sciences for Windows, version 20.0 (SPSS Inc, Chicago, IL). Data distribution was verified by the Shapiro-Wilk normality test. Descriptive statistics (mean ± standard deviation or median and interquartile range) were used to determine patient characteristics. Considering the parametric data, an analysis of variation in repeated measures was performed to compare the results of the three moments, that is, during hospitalization for COPD exacerbation, 30 days after hospital discharge and three-month follow-up. Significance level of p < 0.05 was considered, a post hoc test was performed (Bonferroni test).
Results
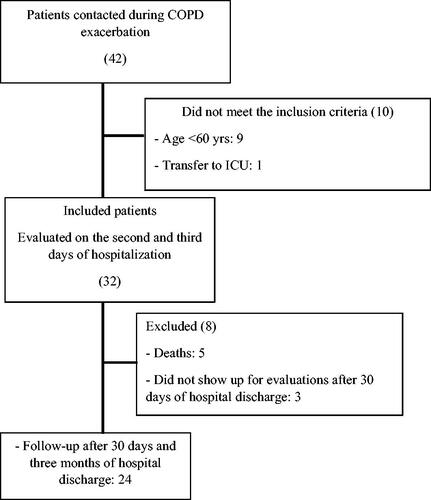
Forty-two patients were admitted for COPD exacerbation. Ten patients did not meet the inclusion criteria due to age <60 years (n = 9) and due to very severe exacerbation requiring intensive care (n = 1). In addition, five patients died and three refused to attend the evaluations after 30 days of hospital discharge. The final sample consisted of 24 patients, all of whom were able to perform tests to assess the levels of PADL and muscle strength. shows the patient inclusion flowchart below.
shows the anthropometric, clinical and functional characteristics.
Table 1. Sample characterization data.
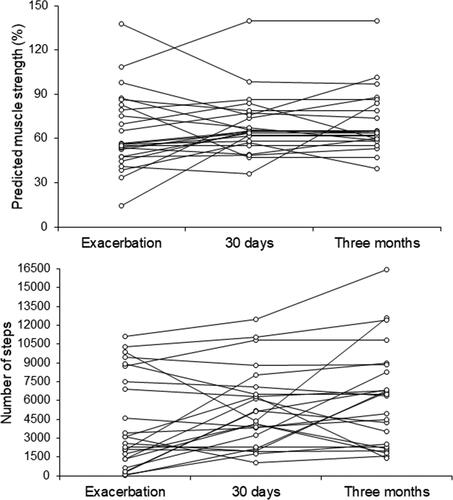
For better visualization of the two study outcome variables at the three evaluation times, patients were dichotomized according to values below and above 80% for predicted quadriceps muscle strength and 4.580 steps, as illustrated in .
Figure 2. Predicted muscle strength values (%) and number of steps dichotomized according to the cutoff values, below and above of 80% e 4580 steps respectively, illustrated in the three moments of evaluation.
shows the results related to the variation in the level of PADL. For inactive time, there was a significant difference between hospitalization and 30 days after hospital discharge. Regarding active time and number of steps, the significant difference was observed only between hospitalization and three months of hospital discharge ().
Table 2. Variation in the level of physical activity in exacerbation, 30 days and three month follow-up.
shows there were no significant differences in quadriceps muscle strength and % of predicted muscle strength between the three moments.
Table 3. Variation in quadriceps muscle strength on exacerbation, 30 days and three month follow-up.
Discussion
The main results of the study showed improvement in the PADL level verified to increased active time and number of steps in three month follow-up. Furthermore, 30 days after hospital discharge there was a reduction of inactive time (sitting/lying down time). Regarding the quadriceps muscle strength, there was no significant difference between the three moments.
Between exacerbation and three months of follow-up, a significant difference in the number of steps was observed (4.241 ± 374 − 6.216 ± 400 steps; p = 0.02). This increase was greater than the minimal clinically significant difference (600–1.000 steps) established by Demeyer et al. [Citation26]. Although we did not control this study, patients received physical therapy interventions during hospitalization, that is, patients were encouraged to walk early on, even though it did not include quadriceps muscle strengthening protocol. Thus, early mobilization, which aims to prevent functional losses and is considered a standard intervention for hospitalized patients due to COPD exacerbation, was indispensable in order to allow observing clinical improvement in the number of steps after hospital discharge [Citation22].
The increase in active time between 30 days of hospital discharge and three months of follow-up reinforces the observed improvement in the number of daily steps. This is relevant because previous evidence revealed that a higher level of physical activity is related to better quality of life, reduced hospitalization and risk of death [Citation27]. In addition, it is also noteworthy that the sample studied did not have any hospitalization for exacerbations in the last year, given that patients with previous hospitalization are considered more inactive before and after exacerbations [Citation11].
The results observed in relation to inactive time (sitting/lying down time) (1.151 ± 249 − 1.065 ± 198 min; p = 0.02), corroborate the results found by Borges and Carvalho [Citation11] (86.7 ± 7.7–69.6 ± 16.1%; p ≤ 0.001) who investigated the effect of hospitalization for COPD exacerbation on PADL in Brazilian patients during hospitalization and after discharge, and observed a significant difference after 30 days of hospital discharge. However, they differ from the results found by Pitta et al. [Citation14] who showed that European patients remained physically inactive 30 days after hospital discharge. This divergence with the present study, which evaluated the Brazilian population, can be explained by factors that prevent them from remaining in inactive periods, such as low socioeconomic conditions and hot temperatures observed in Brazil when compared to European countries [Citation28].
Regarding 30 days and three months after hospital discharge, we did not observe any significant difference in inactive time, however the active time between these moments shows a significant increase. Thus, we can infer that, after 30 days of hospital discharge, factors such as symptoms, systemic inflammation and nutritional depletion were attenuated while the level of physical activity increased, resulting in the return to usual activities [Citation12].
Previous studies showed that the number of daily steps increased from hospitalization to 30 days after hospital discharge (602 to 3.575 steps; ≤0.001), and the same occurred for walking time (1.0 ± 1.1 6.1 ± 4.4%; ≤0,001) [Citation11]. Although the number of daily steps did not show significant difference 30 days after hospital discharge, in our study, patients had an average of 5.351 ± 313 steps, which exceeds the values established for severe physical inactivity (<4.500 steps). In this case, of the 24 patients evaluated, nine were above the values established during hospitalization and 15 were below 4.500 steps.
On the other hand, although the patients in the present study were less inactive 30 days after hospital discharge and more active after three months, we did not observe any significant improvement in quadriceps muscle strength in any of the aforementioned specific times. Regarding the predicted values of quadriceps muscle strength, during hospitalization due to exacerbation patients had an average of 64.21 ± 26.76%, 30 days after hospital discharge an average of 64.62 (57–76)% and three months of follow-up of 63.77 (58–82)%. In addition, of the 24 patients evaluated, 18 patients in the hospitalization period, 20 patients after hospital discharge and three month follow-up had quadriceps muscle weakness, considering they are below 80% of the predicted values [Citation29].
The quadriceps muscle strength generally decreases during exacerbations and partially recovers within three months after hospital discharge [Citation15], however, in this study this did not occur in the COPD patients evaluated. Although we indicated that patients have received physical therapy interventions during the hospitalization period, it is possible that early rehabilitation with a quadriceps muscle strengthening protocol was not applied, which is a more intensive approach than early mobilization. Early rehabilitation employs established principles of pulmonary rehabilitation, including resistance training and/or moderate-to-high intensity strength training [Citation12,Citation22]. Although physical training, both in-hospital and after discharge, presents benefits in the short and long term, in Brazil there are barriers that hinder access to pulmonary rehabilitation such as referral, availability and adherence [Citation30–32].
In addition, the hospital environment causes variations in sleep patterns, cognitive changes and consequent loss of autonomy [Citation12]. The increase in systemic inflammation during COPD exacerbations is related to the worsening of muscle function [Citation15]. Studies in a healthy elderly population have shown significantly reduced lower-limb muscle strength due to the effect of immobility [Citation33]. Especially in COPD patients, this reduction is even greater due to the loss of type I oxidative muscle fibers and mitochondria, hindering the protection capacity against the deleterious effects caused by hospitalization [Citation7].
Therefore, restoring levels of physical activity and muscle strength are important goals for early interventions after hospital discharge or in-hospital, as in the study by Ibrahim, Harvey-Dunstan and Greening [Citation12], for a faster recovery of these patients.
The present study had some limitations that must be considered. The small sample size prevents generalizing the results. Another point was that the sample size was not calculated before the study, the power was estimated with the 24 patients included and resulted in a test power below 0.8. Even so, the analysis generated statistically significant results. Additionally, there was a 25% sample loss at the end of all evaluations due to various justifications. Lastly, longitudinal studies generally present adherence challenges, and in the case of the present study, the elderly population depended on public transport, which made it difficult going to the site to carry out the evaluations.
In contrast, the study showed several strengths. First, as this was a longitudinal study, it allowed to observe and analyze the changes in the levels of physical activity and quadriceps muscle strength up to three months after hospital discharge, which was not common in previous studies with individuals exacerbated by COPD. Second, with the outcomes found, we highlight the importance of specific and early interventions for this population, given that the factors analyzed in the present study can influence important clinical outcomes. Highlighting that a program of peri or post-exacerbation pulmonary rehabilitation, for example, may improve quadriceps muscle strength, improve physical performance and physical activity level, resulting in improved exercise capacity and health-related quality of life, it can contribute to reducing hospital readmissions, reducing costs related to hospitalization of patients with COPD, as well as greater availability of beds.
Conclusion
It is concluded that the level of physical activity showed significant improvement due to the increase in active time and number of steps three months after hospital discharge and to the reduction of inactive time 30 days after hospital discharge. However, there was no significant improvement in quadriceps muscle strength at 30 days and three months after hospital discharge. This reinforces the importance of specific strategies and early interventions to enhance the improvement of these two aspects, optimizing the management of the disease during and after COPD exacerbations.
Acknowledgements
The authors would like to thank the Federal University of São Carlos where this study was developed, the financing of scholarships to researchers involved in this study by the funding agencies Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (Number: 167871/2019-6) and the colleagues of the Spirometry and Respiratory Physiotherapy Laboratory.
Disclosure statement
The authors declare that there is no conflict of interest.
References
- GOLD. GOLD (global initiative for chronic obstructive lung disease). Pneumologie. 2020;71:9–14.
- Troosters T, Sciurba F, Battaglia S, et al. Physical inactivity in patients with COPD, a controlled multi-center pilot-study. Respir Med. 2010;104(7):1005–1011. DOI:https://doi.org/10.1016/j.rmed.2010.01.012
- Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–1359. DOI:https://doi.org/10.1249/MSS.0b013e318213fefb
- DePew ZS, Novotny PJ, Benzo RP. How many steps are enough to avoid severe physical inactivity in patients with chronic obstructive pulmonary disease. Respirology. 2012;17(6):1026–1027. DOI:https://doi.org/10.1111/j.1440-1843.2012.02207.x
- Vaes AW, Garcia-Aymerich J, Marott JL, et al. Changes in physical activity and all-cause mortality in COPD. Eur Respir J. 2014;;44(5):1199–1209. DOI:https://doi.org/10.1183/09031936.00023214
- Maltais F, Decramer M, Casaburi R, et al. An official american thoracic society/european respiratory society statement: Update on limb muscle dysfunction in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2014;189(9):e15–62. DOI:https://doi.org/10.1164/rccm.201402-0373ST
- Abdulai RM, Jensen TJ, Patel NR, et al. Deterioration of limb muscle function during acute exacerbation of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;197(4):433–449. DOI:https://doi.org/10.1164/rccm.201703-0615CI
- Hurst JR. Consolidation and exacerbation of COPD. Med Sci. 2018;6:44. DOI:https://doi.org/10.3390/medsci6020044
- McGhan R, Radcliff T, Fish R, et al. Predictors of rehospitalization and death after a severe exacerbation of COPD. Chest. 2007;132(6):1748–1755. DOI:https://doi.org/10.1378/chest.06-3018
- Halpin DMG, Miravitlles M, Metzdorf N, et al. Impact and prevention of severe exacerbations of COPD: a review of the evidence. Int J Chron Obstruct Pulmon Dis. 2017;12:2891–2908. DOI:https://doi.org/10.2147/COPD.S139470
- Borges RC, Carvalho CRF. Physical activity in daily life in Brazilian COPD patients during and after exacerbation. COPD J Chronic Obstr Pulm Dis. 2012;9(6):596–602. DOI:https://doi.org/10.3109/15412555.2012.705364
- Ibrahim W, Harvey-Dunstan TC, Greening NJ. Rehabilitation in chronic respiratory diseases: in-hospital and post-exacerbation pulmonary rehabilitation. Respirology. 2019;24(9):889–898. DOI:https://doi.org/10.1111/resp.13516
- Gayan-Ramirez G, Decramer M. Mechanisms of striated muscle dysfunction during acute exacerbations of COPD. J Appl Physiol. 2013;114(9):1291–1299. DOI:https://doi.org/10.1152/japplphysiol.00847.2012
- Pitta F, Troosters T, Probst VS, et al. Physical activity and hospitalization for exacerbation of COPD. Chest. 2006;129(3):536–544. DOI:https://doi.org/10.1378/chest.129.3.536
- Spruit MA, Gosselink R, Troosters T, et al. Muscle force during an acute exacerbation in hospitalised patients with COPD and its relationship with CXCL8 and IGF-I. Thorax. 2003;58(9):752–756. DOI:https://doi.org/10.1136/thorax.58.9.752
- Donaldson AV, Maddocks M, Martolini D, et al. Muscle function in COPD: a complex interplay. Int J COPD. 2012;7:523–535.
- Swallow EB, Reyes D, Hopkinson NS, et al. Quadriceps strength predicts mortality in patients with moderate to severe chronic obstructive pulmonary disease. Thorax. 2007;62(2):115–120. DOI:https://doi.org/10.1136/thx.2006.062026
- Torres-Sánchez I, Cabrera-Martos I, Díaz-Pelegrina A, et al. Physical and functional impairment during and after hospitalization in subjects with severe COPD exacerbation. Respir Care. 2017;62(2):209–214. DOI:https://doi.org/10.4187/respcare.04597
- Wageck B, Cox NS, Holland AE. Recovery following acute exacerbations of chronic obstructive pulmonary disease - a review. COPD. 2019;16(1):93–103. DOI:https://doi.org/10.1080/15412555.2019.1598965
- Jones PW, Harding G, Berry P, et al. Development and first validation of the COPD assessment test. Eur Respir J. 2009;34(3):648–654. DOI:https://doi.org/10.1183/09031936.00102509
- Bestall JC, Paul EA, Garrod R, et al. Usefulness of the medical research council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586. DOI:https://doi.org/10.1136/thx.54.7.581
- Holland AE, Spruit MA, Troosters T, et al. An official european respiratory society/american thoracic society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014;44(6):1428–1446. DOI:https://doi.org/10.1183/09031936.00150314
- Britto RR, Probst VS, Dornelas De Andrade AF, et al. Reference equations for the six-minute walk distance based on a Brazilian multicenter study. Braz J Phys Ther. 2013;17(6):556–563. DOI:https://doi.org/10.1590/S1413-35552012005000122
- Aguilar-Farias N, Martino-Fuentealba P, Salom-Diaz N, et al. How many days are enough for measuring weekly activity behaviours with the ActivPAL in adults?J Sci Med Sport. 2019;22(6):684–688. DOI:https://doi.org/10.1016/j.jsams.2018.12.004
- Andrews AW, Thomas MW, Bohannon RW. Normative values for isometric muscle force measurements obtained with hand-held dynamometers. Phys Ther. 1996;76(3):248–259. DOI:https://doi.org/10.1093/ptj/76.3.248
- Demeyer H, Burtin C, Hornikx M, et al. The minimal important difference in physical activity in patients with COPD. PLoS One. 2016;11(4):e0154587–11. DOI:https://doi.org/10.1371/journal.pone.0154587
- Garcia-Aymerich J, Lange P, Benet M, et al. Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population based cohort study. Thorax. 2006;61(9):772–778. DOI:https://doi.org/10.1136/thx.2006.060145
- Pitta F, Breyer MK, Hernandes NA, et al. Comparison of daily physical activity between COPD patients from Central Europe and South america. Respir Med. 2009;103(3):421–426. DOI:https://doi.org/10.1016/j.rmed.2008.09.019
- Nellessen AG, Donária L, Hernandes NA, et al. Analysis of three different equations for predicting quadriceps femoris muscle strength in patients with. COPD. 2014;41:305–312.
- Amorim PB, Stelmach R, Carvalho CRF, et al. Barreiras associadas à menor atividade física em portadores de DPOC. J Bras Pneumol. 2014;40(5):504–512. DOI:https://doi.org/10.1590/S1806-37132014000500006
- Egan C, Deering BM, Blake C, et al. Short term and long term effects of pulmonary rehabilitation on physical activity in COPD. Respir Med. 2012;106(12):1671–1679. DOI:https://doi.org/10.1016/j.rmed.2012.08.016
- Iepsen UW, Munch GDW, Rugbjerg M, et al. Effect of endurance versus resistance training on quadriceps muscle dysfunction in COPD: a pilot study. COPD. 2016;11:2659–2669. DOI:https://doi.org/10.2147/COPD.S114351
- Kortebein P, Ferrando A, Lombeida J, et al. Effect of 10 days of bed rest on skeletal muscle in healthy older adults. J Am Med Assoc. 2007;297:1772–1774.