Abstract
Hospital admissions are common for people with advanced chronic obstructive pulmonary disease (COPD). To provide effective, responsive care, it is important to understand how people experience hospitalization. The aim of this review was to explore the experience of hospitalization in people with advanced COPD, drawing from qualitative research data. Guided by a thematic synthesis approach, a systematic search of databases (n = 13) including PubMed, CINAHL, PsycINFO and ProQuest was undertaken from database inception to May 2020. Inclusion criteria included papers reporting qualitative research focused on any aspect of hospitalization for people with advanced COPD and reported in English language from peer reviewed journals. Following quality appraisal, relevant data were extracted, and a three-stage thematic synthesis method used to develop inductive themes. From 1935 papers, the 11 included studies focused on specific aspects of hospitalization (e.g., care and treatment), rather than the totality of the experience. Four analytical themes were identified: unpredictable hospitalization, benefits and burdens of treatment, overwhelming distress and the communicative attitude of staff. Hospitalization was unpredictable because of the frequent, sudden admissions required for acute breathlessness. Hospital could be perceived both as a safe place, due to immediate symptom relief, but also as a place for experiencing overwhelming distress. Breathlessness was the most difficult symptom experienced, causing physical and psychological distress. Both communication and attitudes of the staff could influence the experience. A holistic approach to the care of hospitalized individuals with advanced COPD is required to improve care.
Supplemental data for this article is available online at https://doi.org/10.1080/15412555.2021.1971186 .
Introduction
People with advanced COPD are frequently hospitalized in the advanced stage of their illness due to a high symptom burden [Citation1]. Acute breathlessness is common, often requiring emergency admission for intensive therapy [Citation2]. People who are hospitalized with COPD have higher unmet needs, including physical, psychological and spiritual aspects compared to those with other chronic illnesses, such as lung cancer [Citation3]. Prolonged symptom burden and high unmet needs cause poor quality of life and suffering during hospitalization [Citation4].
Frequent hospitalization leads to high healthcare cost and causes financial burden to individuals with advanced COPD [Citation5–7]. The number of readmissions, symptom severity, length of hospital stay and associated co-morbidities, such as heart failure and diabetes, influence the cost of hospitalization for those in the advanced stage of COPD [Citation7]. High healthcare utilization and economic burden have implications for developing appropriate healthcare policy to reduce the disease burden of COPD globally [Citation6, Citation8]. Hence, it is important to understand the experience from the individual perspective to improve care.
Qualitative synthesis helps provide insights into individual experience through the integration of data from qualitative studies to provide a formal knowledge synthesis [Citation9]. Many qualitative studies have explored the lived experience of individuals with advanced COPD, studying specific aspects of COPD, such as the experience of breathlessness, care needs and treatment but do not cover these aspects from the perspective of hospitalization [Citation4, Citation10–12]. Careful synthesis of the data in the studies should enable a more comprehensive understanding of the totality of the experience. The aim of this review was to explore the experience of hospitalization in people with advanced COPD, drawing from qualitative studies reporting first person experiences.
Methods
This systematically constructed review utilized a thematic synthesis design [Citation13]. This design enables findings from qualitative studies using different methods to be synthesized while preserving the context to illuminate both the parts and the sum of the phenomenon, such as hospitalization [Citation13]. This review is reported according to the Enhancing Transparency of Reporting the synthesis of Qualitative research (ENTREQ) guidelines [Citation14].
Search strategy
The search was iterative and conducted with the aim to attain conceptual saturation related to the experience of hospitalization [Citation13]. The inclusion and exclusion criteria are set out in Table 1.
The following electronic databases were searched: PubMed, CINAHL, PsycINFO and ProQuest. Gray literature databases included were: theses and dissertations listed on ProQuest, Open Gray, Networked Digital Library of Theses and Dissertations, Open Access Thesis and Dissertation. Finally, citation databases included were: Social Science Citation Index and Conference Proceedings Citation Index on Web of Sciences. No date limits were applied and the search was inclusive up to May 2020. These multiple databases were considered in order to include a wide range of concepts related to the experience of hospitalization. Citation tracking and reference list searching for included papers were conducted to identify potential papers [Citation13]. The search strategy was constructed based on the key topics from the research question, Medical Subject Headings (MeSH) terms identified from the databases and key words identified from relevant papers. A combination of thesaurus terms or MeSH, free text words and the broad-based terms was employed to identify the relevant studies to optimize the search. These combination of terms combined with Boolean operators, such as “AND,” “OR” and truncations were employed to find the relevant studies (). An example search strategy for PubMed is given in Appendix (Supplementary material).
Table 1. Inclusion and exclusion criteria.
Table 2. Search terms for key concepts.
Study selection and quality appraisal
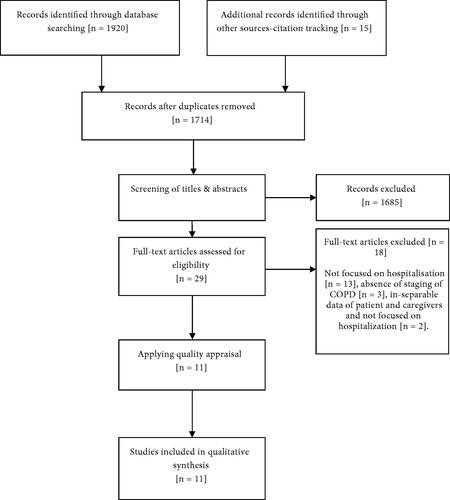
A total of 1935 titles and abstracts were screened and full texts were sought for 29 studies to check their eligibility by applying the inclusion and exclusion criteria. Finally, 11 were included in the review ().
BB screened the title and abstracts of the retrieved studies and these were checked by CW to confirm the consistency of the selection process. The characteristics of included studies are detailed in Supplementary material, Table 1.
The quality of studies was assessed by the appraisal criteria proposed by Thomas and Harden [Citation13] for thematic synthesis. This quality appraisal tool contains 12 criteria under 3 categories: 5 related to the quality of the reporting of a study such as aim and context; 4 criteria related to reliability and validity; and finally 3 criteria related to the appropriateness of the study methods [Citation13]. Each criterion was rated either as present or not (a score of 0 or 1 was given); hence, a maximum score of 12 for each study was possible. Studies scoring below 5 were considered as poor but were not excluded because each study was considered to have some contribution to the synthesis, irrespective of the quality [Citation13]. Overall, the scores ranged from 7 to 12 (see Supplementary material, Table 1).
Appraisal was done by BB and verified by CW to ensure the consistency of the process.
Data extraction and analysis
Data extracted were: study details, demographics and study characteristics, such as the type of data collection, sampling, sample size, findings of the primary study and themes or concepts related to the experience of hospitalization, such as the admission process, treatment and care, and communication with staff. All included studies were imported into NVivo 11 software to aid the analysis. Both direct quotes and the texts related to hospitalization in the findings section were coded. Coding and analysis was done by BB and checked by CW with disagreements resolved by consensus.
Data synthesis was carried out following the three-stage thematic synthesis method [Citation13]. First, line by line coding of the text related to the experience of hospitalization was coded; each code was given a description to maintain the consistency while coding across the studies. Subsequent codes from the rest of the studies were either coded into the existing codes or under a new code, depending on the content of the text. Then, these codes were grouped under appropriate categories and descriptive themes were derived from these categories; until this point, themes were kept closer to the original studies in the context from where they emerged [Citation13]. The final step of analysis involved the interpretive analysis of descriptive themes to develop inductive, analytical themes related to hospitalization.
Findings
Analysis of the findings from 11 studies from Europe (n = 6), the US (n = 1), Australia (n = 1) and Asian countries (n = 3), yielded 4 overarching themes: unpredictable hospitalization, perceived benefits and burdens of treatment, overwhelming distress and the communicative attitude of the staff.
Unpredictable hospitalization
Hospitalizations for people with COPD due to acute breathlessness were frequent. Particularly, emergency admissions were experienced as chaotic, with waits for consultations in the emergency department or for admission [Citation15]. People with COPD could feel a loss of control, with poor communication causing confusion during emergency admissions:
We were whizzed straight into the Medical Emergency or surgical place …I couldn’t tell you. [Citation15, p. 263].
Concurrent with this chaotic experience was a feeling of safety due to the immediate help provided for the acute breathlessness [Citation15–18], with immediate medical attention and appropriate management reducing anxiety and helplessness:
…that’s a feeling of security. Knowing, that you are going away to get help. I just want to be cared for, as there is nothing that I can do. [Citation18, p. 03].
Nevertheless, people preferred to avoid hospitalization because of fear associated with hospitalization due to varied reasons. Firstly, hospitalization itself could be felt to cause a decline in health, occurring after each in-patient episode [Citation17, Citation19], which could cause fear of hospitalization:
Because every time I have a bout…I end up on a short stint in the hospital; I take one step forward and two back so that I’m always starting over again. [Citation19, p. 342].
People could also be fearful of hospitalization because on some occasions severe breathlessness caused near-death experience [Citation17, Citation19, Citation20], and this was associated with uncertainty as prognosis and plans were not clear:
Going to the hospital would bring a lot of unknowns to participants…whether or not they would be admitted, how long they would have to stay…[Citation19, p. 343].
The unclean hospital environment and noise from neighboring patients and machines caused sleep disturbances, which led to avoidance of hospitalization [Citation20]:
No, no I’m fighting the hospital. Geez if I go to the hospital I’ll never come back here…I don’t tell “em the truth. I told” em no (to being short of breath). [Citation19, p. 343].
Repeated hospitalizations caused care burdens that disrupted the family’s routine, and on occasions the care burden itself led to hospitalizations [Citation21]:
My wife begged the doctor to admit me to the hospital. She was too tired to take care of me…I am her burden. [Citation21, p. 1759]
However, hospitalization was perceived as inevitable for accessing treatment for acute symptoms. While hospitalization was perceived as necessary, the burdens of repeated hospitalization caused avoidance of hospitalization where possible.
Perceived benefits and burdens of treatment
In general, treatment offered for breathlessness was considered effective and quick. Noninvasive ventilation (NIV) was one of the treatment options offered for acute breathlessness, which could provide immediate relief and improved independence:
…it gives me back a normal life…to get me back to a normal existence; it helps me breathe… [Citation22, p. 271].
However, NIV caused unpleasant side effects, such as dryness of the throat and difficulties in speaking [Citation17, Citation22–24]. NIV caused anxiety when hot air forcefully pumped into the chest, which was perceived as losing control over breathing. NIV caused total physical restriction that limited daily routines during hospitalization. Nevertheless, participants had to accept NIV, as it seemed to be the treatment of choice for acute breathlessness:
It’s very uncomfortable and awkward…you get anxious and try to avoid the mask, but at the same time you know you need it. [Citation24, p. 1729].
Being on the ventilator in the intensive care unit was perceived to be difficult because being hooked on to the machine increased feelings of losing control [Citation17, Citation24]. Observing other people who did not regain consciousness after intubation caused fear of death and uncertainty:
You need to deal with being cut off from everything and being restrained by the mask… it is really, really tough, but there is no going back, really. [Citation24, p. 173].
Feeling vulnerable and fatigue during acute breathlessness prevented individuals from participating in treatment decision-making [Citation18, Citation19, Citation22, Citation25]. Hence, some preferred their healthcare professionals to decide the treatment of choice:
…perhaps, it is better that they (health personnel) are determined; I was more or less completely gone…[Citation25, p. 3067].
Letting the staff decide treatment options demonstrated trust in staff, on occasions where the treatment decisions were taken by staff without participants’ involvement, this caused uncertainty related to future treatment plan and emotional upset. Time constraints during sudden admissions sometimes led to quick treatment decisions by the staff, which compounded poor explanation of treatment options that could cause a feeling of neglect by staff [Citation17, Citation20, Citation23, Citation25]:
Physicians discussing further treatment above the patient’s head evoked feelings of mistrust in the patient. [Citation23, p. 744].
Both forceful treatment and poor treatment information caused distrust, which are further discussed in the next section.
The communicative attitude of the staff
Friendly staff motivated individuals to remain engaged with treatment during hospitalization. Respecting and listening to concerns encouraged individuals and increased the level of perceived self-control during the acute period of illness [Citation23]. Having an open conversation with staff about the disease and treatment plan helped individuals to cope with the difficult treatment:
I participated all the time and most of them were encouraging and open. They listened to what I had to say – what little I had to say. [Citation23, p. 744].
A friendly chat and a sense of humor displayed by the staff even during critical moments seemed to improve participants’ relationships with staff; they recognized that staff took control during the critical situations and then helped them come back to a more normal balance [Citation23, Citation25]. In particular, being available and proactive to participants’ needs established trust with staff:
That you feel you are in safe hands – that there is control over what is being done… [Citation23, p. 743];
They (staff) saw my needs before I noticed them. [Citation25, p. 3067].
Consequently, trust in staff helped participants tolerate unpleasant situations, such as putting up with difficult treatments.
However, negative behaviors from staff, specifically during the critical time of illness caused loss of trust in treatment. In particular, not listening to participants’ concerns caused feelings of being neglected:
…that she felt she was a nuisance…she said she was put “on hold.” [Citation23, p. 743].
When individuals were not included in the treatment decision-making, it was perceived that difficult treatments were forced on them which caused distrust with staff [Citation20, Citation23, Citation25]. For example, one participant tried to test the nurses by keeping the alarm by her side to see whether nurses would attend when she called out. But nurses tried to manipulate the alarm so that it would not ring which angered the participant and disrupted the relationship between them:
But she (the nurse) threatened (me) a bit with that tablet. I said no. I wanted to be attentive because I might be choked if they do not suck out the slime (in time). I had to be in control… [Citation25, p. 3067].
Treating individuals as a nuisance and without respect created distrust [Citation23, Citation25]. For example, smokers felt that the behavior of the staff made them feel shame and guilty about smoking and that they deserved such unpleasant treatment for their past behavior. Ignoring participants’ opinions and neglecting their presence during treatment discussions were perceived to be unprofessional:
And when a doctor stands over you, at the same time making eye contact with a nurse and smiling, thinking I could not hear anything, well that’s not nice…[Citation25, p. 3067].
These unprofessional behaviors caused distrust and caused a feeling of vulnerability, which had a negative impact on the experience of hospitalization.
Overwhelming distress
Extreme distress was reported during hospitalization, which affected the individuals on the physical, psychological and spiritual aspects.
Breathlessness
Breathlessness was the most common reason for hospitalization in the advanced stage of COPD. Severe breathing difficulties were reported which sometimes were perceived as life-threatening [Citation24, Citation25]. Breathlessness was described as a struggle to get enough air, like breathing through a narrow pipe, or as a suffocating feeling and therefore, necessitated an extreme effort to survive. Further, experiencing frequent breathlessness required breathing support such as NIV. Despite using NIV, breathlessness was perceived as the machine tried to blow a significant volume of air against the capacity to inhale; on some occasions, a choking sensation was experienced which caused panic attacks:
…being restrained by the mask was just too much for me, I couldn’t breathe… and suddenly I panicked. [Citation24, p. 173].
Inability to breathe caused a fear of death and anxiety. Experiencing confusion during acute breathlessness and being unable to communicate clearly to staff also caused anxiety. Nevertheless, a few participants tried to keep calm to cope with the dual stress of breathlessness and anxiety during hospitalization, and some used humor to mask their fear:
I remember getting confused, but I’m confused in any case (laughs). But all joking aside it was very scary. [Citation15, p. 263].
An extreme physical weakness accompanied acute attacks of breathlessness and restricted from doing daily activities in hospital [Citation16, Citation17, Citation20, Citation23, Citation24]. Many were bedbound, exhausted and completely dependent on staff to carry out their daily routines:
Being unable to speak, unable to act, not being able to eat, and feeling ill all over. [Citation23, p. 74].
Feelings of isolation caused low self-esteem and helplessness which caused psychological distress.
Psychological distress
Although breathlessness was the main cause for anxiety, nightmares and confusion during acute breathlessness also contributed to anxiety. NIV treatment increased anxiety, as being alone in a hospital room and restrained with the machine caused fear [Citation23–25]. Nightmares were another source of anxiety; several participants were afraid to fall asleep and wanted to keep the lights on even during the day [Citation15–17, Citation19]. Fear of death also caused sleep disturbances during hospitalization. Sleeplessness further worsened fatigue and caused dependency, which disrupted the routines of participants’ families:
My family’s a big factor…I feel as if I’m actually putting on them. [Citation20, p. 752].
Such feelings of helplessness, physical dependency and repeated hospitalizations contributed to considerable psychological distress.
Spiritual concerns
Individuals who were admitted to the intensive care unit expressed a wish to live, despite facing hardships and uncertainty with illness. Surviving previous hospitalizations gave a desire to live, even if that was for a short time. Facing uncertainty with illness helped cherish whatever time that was available to live:
…I learn how to live one day at a time because I do not know whether I can live two days later. [Citation17, p. 4]
Completing family responsibilities and reflecting on their good deeds, gave a feeling of fulfillment of life:
I am at peace with myself because I did nothing purposely in harming others and I did not owe anybody anything that I did not return in my life. [Citation17, p. 138].
In contrast, others were afraid that death may occur soon due to changes in health status and the seasons of weather, particularly winter, as many participants suffered from acute breathlessness during winter. Sensing that life span was short with uncertainties in health caused hopelessness. A strong death wish was reported when repeated hospitalizations did not seem to cure the disease, as expected [Citation17]. However, making do-not-resuscitate decisions reduced fear of death, which then provided some inner peace. Many preferred to have a peaceful death, as if falling into sleep without much suffering:
…my concern is to remain clean and tidy when I die… I only want to die in peace, without causing more trouble. [Citation17, p. 13].
Accepting death rather than confronting it, facilitated decisions around do-not-resuscitate and end-of-life care plans during hospitalization. Expressing death and dying concerns also helped both participants and staff understanding these concerns.
Discussion
This thematic synthesis has provided insight into the experience of hospitalization in people with advanced COPD. Studies focused on specific aspects of hospitalization such as treatment, symptom burden and interaction with staff. Four overarching themes were identified: unpredictable hospitalization, perceived benefits and burdens of treatment, the communicative attitude of the staff and overwhelming distress.
Central to the experience is both the unpredictable nature of hospitalization and that different aspects of the experience can be perceived either negatively or positively, triggered by repeated, acute breathlessness, known to be a feature of the trajectory of COPD and other advanced respiratory illnesses [Citation26–28]. Once in hospital, the immediate attention to ameliorating acute breathlessness could provide a sense of safety and security, similar to the sense of safety seen in other illnesses, such as heart failure and cancer [Citation29, Citation30]. Nevertheless, this sense of safety and security during this acute illness phase did not necessarily mean that hospital was a preferred place of care, as these positive aspects were offset by negative features such as a lack of cleanliness and sleep disturbances [Citation29–34]. Hospitalization could also be associated with the presence of overwhelming physical and psychological distress including spiritual concerns [Citation2, Citation35]. Such spiritual concerns were particularly highlighted in the studies in this review, in contrast to studies focused on different stages of COPD or settings for COPD care [Citation35].
As with other studies in chronic illnesses, the overall experience of hospitalization in advanced COPD was a mix of positive and negative experiences, reflecting the treatment aspect of hospitalization [Citation29, Citation30]. The experience seemed to relate mainly to individuals’ varied treatment expectations, such as symptom relief and cost-effective treatment with minimal side-effects; depending on these areas and levels of expectation, the experience of hospitalization was varied. This indicates that the experience could be influenced by individual expectations about treatment and healthcare delivery. Patients’ expectations were an important indicator for measuring patient-satisfaction with treatment, and influence the individual experience related to hospitalization [Citation36–38]. Studying patients’ expectations pertaining to treatment is, therefore, important to understand this mix of experience, both to meet their specific needs, and to improve the quality of care [Citation39, Citation40].
Patients’ expectations related to healthcare are defined as “beliefs about the incidence or non-incidence of a future-directed event or experience” [Citation39, p. 2]. Several theories of patients’ expectations, such as self-efficacy, outcome expectancy and response expectancy theory, focus on certain aspects of patients’ expectations [Citation39, Citation41]. Some of these theories do not sufficiently support the influence on treatment outcome hence, further elaborations were required to address this [Citation42–44]. Nevertheless, there is no unified theory that covers all the aspects of the complex construct of “expectation” in the context of healthcare. Laferton’s integrated model of expectations [Citation39] provides the most comprehensive account, including social learning and cognitive theories that address the main constructs of expectations in the healthcare area [Citation39]. This model is underpinned by four concepts, generalized expectancy, personalized outcome expectancy, treatment outcome expectations and timeline expectations, which are described with the findings of this review.
Generalized expectations are related to the capability of individuals’ self-efficacy, higher levels of which can lead to optimistic self-beliefs that difficult tasks can be achieved [Citation45]. This may or may not be context-specific, such as treatment and illness, which may lead to optimization of treatment [Citation46]. In this review, participants’ expectations around the frequency of hospitalization and type of admission, such as emergency admissions, were context-specific, which influenced the outcome of participants’ expectations around hospitalization. For example, the requirement for frequent hospitalization showed the expectation on the role of hospitalization in providing complete symptom relief remains unmet. COPD studies also showed that patients expected treatment at home, rather than being frequently hospitalized [Citation47]. Similar to this review, symptom relief was the most preferred generalized expectancy while being hospitalized in studies on the early stage of COPD, which was also a major contributor to patient-satisfaction, compared to other domains of expectation [Citation48]. However, varied expectations about symptom relief did not lead to optimization of treatment. Individual expectations could be related to expectation optimization, which improves treatment outcome by reducing maladaptive expectations [Citation49]. Although participants expected breathlessness to recur, they did not expect to be dependent and confined to a hospital bed; this caused dissatisfaction, despite hospitalization providing immediate symptom relief. This mismatch between expectations and treatment outcome could be addressed by explaining the actual impact of acute breathlessness on their dependency, which could reduce participants’ expectation level related to dependency and breathlessness treatment that can lead to optimization of expectation.
Treatment outcome expectations have two components, process and structural expectations, which relate to the nature and course of treatment respectively, covering the benefits and side-effects of treatment [Citation38]. In this review, NIV treatment was considered beneficial because of its ability to provide immediate relief but its associated side-effects caused considerable distress during hospitalization. Studies conducted in the early stages of COPD also showed that expectations are mainly centered on the treatment outcome and communication [Citation47, Citation48, Citation50]. Treatment with minimal side-effects which are also affordable, which could be preferably taken at home are considered helpful [Citation47, Citation48]. Nevertheless, NIV treatment was preferred, despite its side- effects, with the expectation that it would help with breathlessness. This contradicting expectations and behavior outcome are rather complex, as a treatment or a health-changing task is generally abandoned when the desired outcome has not been reached [Citation51]. Here, the sub-domains of self-efficacy and behavior outcome of personalized outcome expectancy seem to have a converse relationship, which is not presented clearly in the integrative model of expectations [Citation39].
Both communicative attitude and treatment information shapes both the past and future expectation of treatment [Citation38, Citation48]. This review showed that communication is an essential part of the treatment which impacted the experience in both a positive and negative manner. For example, if a patient is not given adequate and clear information about treatment, then, this leads to patient dissatisfaction, which is also confirmed in this review [Citation37, Citation48]. Patients’ expectations about the communicative attitude of the staff relates to the process of the treatment [Citation38]. Although the treatment outcome becomes good, if the communicative attitude of staff is perceived as not acceptable, this still could influence the overall treatment outcome negatively, as shown in this review [Citation48]. Discussion of treatment options and listening to their concerns are the most common communicative expectations in people with COPD [Citation48]. Therefore, communication arguably impacts the expectations of both treatment and hospitalization. However, this element of treatment expectations has not been clearly articulated in the existing integrative model, which could be emphasized under the treatment outcome expectancy.
Timeline expectations address temporal factors such as the length of treatment or illness. The need for frequent hospitalization and prolonged treatment with NIV and continued suffering correlates with timeline expectations. Both prolonged suffering and the dependency on treatment lead to loss of personal control over the illness, as well as treatment, which is contrary to the expectation that hospitalization would relieve suffering. In this context, the duration of both illness and treatment contribute to timeline expectancy and also personalized and treatment outcome expectancy. Therefore, these domains seem to be interrelated, rather as distinctive domains, as presented in the integrative model of expectations [Citation39].
According to this integrative model, the overall expectations of hospitalization seems to influence the perception of positive and negative experiences, which may vary from time to time; this could be due to a number of factors related to individuals’ previous experience, level and degree of expectation, symptom severity and healthcare delivery [Citation36–38]. These expectations, therefore, are very subjective and could vary depending on the factors which contribute to the overall experience of hospitalization. Although the integrative model provides a unified theory of expectations in the healthcare context, these seem to emphasize more on the distinctness of the individual domains, rather than recognize the causal and/or interrelatedness between the domains of expectations. Also, these domains do not include communication which is an important element of the process of treatment expectations that is crucial in influencing treatment outcomes.
Strengths and limitations
The synthesis process enabled integration across discrete aspects of the hospitalization experience to provide a more holistic account than that offered by individual studies. Including only English language studies may mean that experiences in some cultures and contexts may not be included in the synthesis. Indeed, most included studies were European such that the synthesis is most likely to reflect European culture and contexts, which may not be transferrable [Citation52]. Although most of the studies mentioned physical and emotional distress, spiritual concerns were the least addressed. It was not clear whether this was limited by the study aim, a lack of effort to explore this aspect or that this particular aspect did not develop as a major theme in these studies. This indicates a lack of holistic approach to the care of people with advanced COPD, which has important implications for both policy and practice.
Conclusion
This review showed that hospitalization in people with advanced COPD is a mix of positive and negative experiences. Discordance between patients’ expectations and healthcare delivery plays a role in shaping the experience. This review synthesized specific aspects of hospitalization, such as care, treatment and interaction with staff. As hospitalization seems to be a broad, multi-dimensional experience, it is difficult to know whether these findings represent the experience as a whole. Future research should focus on studying the whole experience, which would enhance our understanding, so we can improve the care for people with advanced COPD.
Disclosure of interest
The authors declare no conflict of interest.
Acknowledgements
The authors sincerely thank Katherine Froggatt for her guidance in conception, design, data analysis and report writing of this study.
Additional information
Notes on contributors
Barathi Bakthavatsalu
Study conception and planning (BB, CW), conducting searches (BB), determining inclusion (BB, CW), synthesis (BB, CW), drafting manuscript (BB), revising it critically for important intellectual content (BB, CW, JS), final approval of the version to be published (BB, CW, JS).
References
- Maddocks M, Lovell N, Booth S, et al. Palliative care and management of troublesome symptoms for people with chronic obstructive pulmonary disease. Lancet. 2017;390(10098):988–1002. DOI:https://doi.org/10.1016/S0140-6736(17)32127-X
- Lovell N, Etkind SN, Bajwah S, et al. Control and context are central for people with advanced illness experiencing breathlessness: a systematic review and thematic-synthesis. J Pain Symptom Manage. 2018;57(1):140–155.e2.
- Luckett T, San Martin A, Currow DC, et al. A systematic review and Meta-analysis of studies comparing burden from lung cancer and chronic obstructive pulmonary disease. Palliat Med. 2020;34(10):1291–1304. DOI:https://doi.org/10.1177/0269216320940153
- Schroedl CJ, Yount SE, Szmuilowicz E, et al. A qualitative study of unmet healthcare needs in chronic obstructive pulmonary disease. A potential role for specialist palliative care? Ann Am Thorac Soc. 2014;11(9):1433–1438. DOI:https://doi.org/10.1513/AnnalsATS.201404-155BC
- Corlateanu A, Covantev S, Mathioudakis AG, et al. Prevalence and burden of comorbidities in chronic obstructive pulmonary disease. Respir Investig. 2016;54(6):387–396. DOI:https://doi.org/10.1016/j.resinv.2016.07.001
- Soriano JB, Abajobir AA, Abate KH, et al. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet Respir Med. 2017;5(9):691–706. DOI:https://doi.org/10.1016/S2213-2600(17)30293-X
- Iheanacho I, Zhang S, King D, et al. Economic burden of chronic obstructive pulmonary disease (COPD): a systematic literature review. Int J Chron Obstruct Pulmon Dis. 2020;15:439–460. DOI:https://doi.org/10.2147/COPD.S234942
- Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management and prevention of chronic obstructive lung disease 2017 report. Respirology. 2017;22(3):575–601. DOI:https://doi.org/10.1111/resp.13012
- Gough D, Thomas J, Oliver S. Clarifying differences between review designs and methods. Syst Rev. 2012;1(1):28. DOI:https://doi.org/10.1186/2046-4053-1-28
- Harb N, Foster JM, Dobler CC. Patient-perceived treatment burden of chronic obstructive pulmonary disease. COPD. 2017;12:1641–1652. DOI:https://doi.org/10.2147/COPD.S130353
- Pooler A, Beech R. Examining the relationship between anxiety and depression and exacerbations of COPD which result in hospital admission: a systematic review. Int J Chron Obstruct Pulmon Dis. 2014;9(315):315–330.
- Halpin D, Hyland M, Blake S, et al. Understanding fear and anxiety in patients at the time of an exacerbation of chronic obstructive pulmonary disease: a qualitative study. JRSM Open. 2015;6(12):2054270415614543. DOI:https://doi.org/10.1177/2054270415614543
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):45. DOI:https://doi.org/10.1186/1471-2288-8-45
- Tong A, Flemming K, McInnes E, et al. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12(1):181. DOI:https://doi.org/10.1186/1471-2288-12-181
- Seamark D, Blake S, Seamark C, et al. Is hospitalisation for COPD an opportunity for advance care planning? A qualitative study. Prim Care Respir J. 2012;21(3):261–266. DOI:https://doi.org/10.4104/pcrj.2012.00032
- Chang Y-Y, Dai Y-T, Chien N-H, et al. The lived experiences of people with chronic obstructive pulmonary disease: a phenomenological study. J Nurs Scholarsh. 2016;48(5):466–471. DOI:https://doi.org/10.1111/jnu.12230
- Pang SM, Tse CY, Chan KS, et al. An empirical analysis of the decision-making of limiting life-sustaining treatment for patients with advanced chronic obstructive pulmonary disease in Hong Kong, China. J Crit Care. 2004;19(3):135–144. DOI:https://doi.org/10.1016/j.jcrc.2004.08.001
- Landers A, Wiseman R, Pitama S, et al. Patient perceptions of severe COPD and transitions towards death: a qualitative study identifying milestones and developing key opportunities. NPJ Prim Care Respir Med. 2015;25:15043. DOI:https://doi.org/10.1038/npjpcrm.2015.43
- Lowey SE, Norton SA, Quinn JR, et al. A place to get worse: perspectives on avoiding hospitalization from patients with end-stage cardiopulmonary disease. J Hosp Palliat Nurs. 2014;16(6):338–345. DOI:https://doi.org/10.1097/njh.0000000000000081
- Harrison SL, Robertson N, Apps L, et al. "We are not worthy"—understanding why patients decline pulmonary rehabilitation following an acute exacerbation of COPD. Disabil Rehabil. 2015;37(9):750–756. DOI:https://doi.org/10.3109/09638288.2014.939770
- Yu DS, Lee DT, Woo J. The revolving door syndrome: the Chinese COPD patients’ perspectives. J Clin Nurs. 2007;16(9):1758–1760. DOI:https://doi.org/10.1111/j.1365-2702.2007.02089.x
- Gale NK, Jawad M, Dave C, et al. Adapting to domiciliary non-invasive ventilation in chronic obstructive pulmonary disease: a qualitative interview study. Palliat Med. 2015;29(3):268–277. DOI:https://doi.org/10.1177/0269216314558327
- Torheim H, Kvangarsnes M. How do patients with exacerbated chronic obstructive pulmonary disease experience care in the intensive care unit?Scand J Caring Sci. 2014;28(4):741–748. DOI:https://doi.org/10.1111/scs.12106
- Sørensen D, Frederiksen K, Groefte T, et al. Striving for habitual well-being in noninvasive ventilation: a grounded theory study of chronic obstructive pulmonary disease patients with acute respiratory failure. J Clin Nurs. 2014;23(11-12):1726–1735. DOI:https://doi.org/10.1111/jocn.12322
- Kvangarsnes M, Torheim H, Hole T, et al. Narratives of breathlessness in chronic obstructive pulmonary disease. J Clin Nurs. 2013;22(21-22):3062–3070. DOI:https://doi.org/10.1111/jocn.12033
- Bartels W, Adamson S, Leung L, et al. Emergency department management of acute exacerbations of chronic obstructive pulmonary disease: factors predicting readmission. COPD. 2018;13:1647–1654. DOI:https://doi.org/10.2147/COPD.S163250
- Karasouli E, Munday D, Bailey C, et al. Qualitative critical incident study of patients’ experiences leading to emergency hospital admission with advanced respiratory illness. BMJ Open. 2016;6(2):e009030. DOI:https://doi.org/10.1136/bmjopen-2015-009030
- Robinson K, Lucas E, van den Dolder P, et al. Living with chronic obstructive pulmonary disease: the stories of frequent attenders to the emergency department. J Clin Nurs. 2018;27(1-2):48–56. DOI:https://doi.org/10.1111/jocn.13842
- Liu T, Kiwak E, Tinetti M. Perceptions of hospital-dependent patients on their needs for hospitalization. J Hosp Med. 2017;12(6):450–453. DOI:https://doi.org/10.12788/jhm.2756
- Spichiger E. Being in the hospital: an interpretive phenomenological study of terminally ill cancer patients’ experiences. Eur J Oncol Nurs. 2009;13(1):16–21. DOI:https://doi.org/10.1016/j.ejon.2008.10.001
- Christensen HM, Titlestad IL, Huniche L. Development of non-invasive ventilation treatment practice for patients with chronic obstructive pulmonary disease: results from a participatory research project. SAGE Open Med. 2017;5:2050312117739785. DOI:https://doi.org/10.1177/2050312117739785
- Wang K, Zhang B, Li C, et al. Qualitative analysis of patients’ intensive care experience during mechanical ventilation. J Clin Nurs. 2009;18(2):183–190. DOI:https://doi.org/10.1111/j.1365-2702.2008.02518.x
- Oyesanya T. The experience of patients with ABI and their families during the hospital stay: a systematic review of qualitative literature. Brain Inj. 2017;31(2):151–173. DOI:https://doi.org/10.1080/02699052.2016.1225987
- Brereton L, Gardiner C, Gott M, et al. The hospital environment for end of life care of older adults and their families: an integrative review. J Adv Nurs. 2012;68(5):981–993. DOI:https://doi.org/10.1111/j.1365-2648.2011.05900.x
- Gardener AC, Ewing G, Kuhn I, et al. Support needs of patients with COPD: a systematic literature search and narrative review. Int J Chron Obstruct Pulmon Dis. 2018;13:1021–1035. DOI:https://doi.org/10.2147/COPD.S155622
- Berhane A, Enquselassie F. Patient expectations and their satisfaction in the context of public hospitals. Patient Prefer Adherence. 2016;10:1919–1928. DOI:https://doi.org/10.2147/PPA.S109982
- Bjertnaes OA, Sjetne IS, Iversen HH. Overall patient satisfaction with hospitals: effects of patient-reported experiences and fulfilment of expectations. BMJ Qual Saf. 2012;21(1):39–46. DOI:https://doi.org/10.1136/bmjqs-2011-000137
- El-Haddad C, Hegazi I, Hu W. Understanding patient expectations of health care: a qualitative study. J Patient Exp. 2020;7(6):1724–1731.
- Laferton JA, Kube T, Salzmann S, et al. Patients’ expectations regarding medical treatment: a critical review of concepts and their assessment. Front Psychol. 2017;8:233. DOI:https://doi.org/10.3389/fpsyg.2017.00233
- Friele RD, Sluijs EM. Patient expectations of fair complaint handling in hospitals: empirical data. BMC Health Serv Res. 2006;6(1):1–9. DOI:https://doi.org/10.1186/1472-6963-6-106
- Barron CJ, Klaber Moffett JA, Potter M. Patient expectations of physiotherapy: definitions, concepts, and theories. Physiother Theory Pract. 2007;23(1):37–46. DOI:https://doi.org/10.1080/09593980601147843
- Diefenbach MA, Leventhal H. The common-sense model of illness representation: Theoretical and practical considerations. J Soc Distress Homeless. 1996;5(1):11–38. DOI:https://doi.org/10.1007/BF02090456
- Kirsch I. Response expectancy theory and application: a decennial review. Appl Prev Psychol. 1997;6(2):69–79. DOI:https://doi.org/10.1016/S0962-1849(05)80012-5
- Eastman C, Marzillier JS. Theoretical and methodological difficulties in Bandura’s self-efficacy theory. Cogn Ther Res. 1984;8(3):213–229. DOI:https://doi.org/10.1007/BF01172994
- Schwarzer R. Optimism, vulnerability, and self-beliefs as health-related cognitions: a systematic overview. Psychol Health. 1994;9(3):161–180. DOI:https://doi.org/10.1080/08870449408407475
- Kube T, D’Astolfo L, Glombiewski JA, et al. Focusing on situation-specific expectations in major depression as basis for behavioural experiments—development of the depressive expectations scale. Psychol Psychother. 2017;90(3):336–352. DOI:https://doi.org/10.1111/papt.12114
- Haughney J, Partridge M, Vogelmeier C, et al. Exacerbations of COPD: quantifying the patient’s perspective using discrete choice modelling. Eur Respir J. 2005;26(4):623–629. DOI:https://doi.org/10.1183/09031936.05.00142704
- Bulcun E, Ekici M, Ekici A. Assessment of patients’ preferences regarding the characteristics associated with the treatment of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2014;9(363):363–368.
- Kube T, Glombiewski JA, Rief W. Using different expectation mechanisms to optimize treatment of patients with medical conditions: a systematic review. Psychosom Med. 2018;80(6):535–543. DOI:https://doi.org/10.1097/PSY.0000000000000596
- Wortz K, Cade A, Menard JR, et al. A qualitative study of patients’ goals and expectations for self-management of COPD. Prim Care Respir J. 2012;21(4):384–391. DOI:https://doi.org/10.4104/pcrj.2012.00070
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Adv Behav Res Ther. 1978;1(4):139–161. DOI:https://doi.org/10.1016/0146-6402(78)90002-4
- Hartog J, Hartog EA. Cultural aspects of health and illness behavior in hospitals. West J Med. 1983;139(6):910–916.