Abstract
Literature regarding trends of incidence, mortality, and complications of acute exacerbation of chronic obstructive pulmonary disease (COPD) in the emergency departments (ED) is limited. What are trends of COPD exacerbation in ED? Data were obtained from the Nationwide Emergency Department Sample (NEDS) that constitutes a 20% sample of hospital-owned EDs and inpatient sample in the US. All ED encounters were included in the analysis. Complications of AECOPD were obtained by using ICD codes. Out of 1.082 billion ED encounters, 5,295,408 (mean age 63.31 ± 12.63 years, females 55%) presented with COPD exacerbation. Among these patients, 353,563(6.7%) had AECOPD-plus (features of pulmonary embolism, acute heart failure and/or pneumonia) while 4,941,845 (93.3%) had exacerbation without associated features or precipitating factors which we grouped as AECOPD. The AECOPD-plus group was associated with statistically significantly higher proportion of cardiovascular complications including AF (5.6% vs 3.5%; p < 0.001), VT/VF (0.14% vs 0.06%; p < 0.001), STEMI (0.22% vs 0.11%; p < 0.001) and NSTEMI (0.65% vs 0.2%; p < 0.001). The in-hospital mortality rates were greater in the AECOPD-plus population (0.7% vs 0.1%; p < 0.001). The incidence of both AECOPD and AECOPD-plus had worsened (p-trend 0.004 and 0.0003) and the trend of mortality had improved (p-trend 0.0055 and 0.003, respectively). The prevalence of smoking for among all COPD patients had increased (p-value 0.004), however, the prevalence trend of smoking among AECOPD groups was static over the years 2010–2018. There was an increasing trend of COPD exacerbation in conjunction with smoking; however, mortality trends improved significantly. Moreover, the rising burden of AECOPD would suggest improvement in diagnostics and policy making regarding management.
Abbreviations
| ACS | = | acute coronary syndrome |
| AECOPD | = | acute exacerbation of chronic obstructive pulmonary disease |
| AF | = | atrial fibrillation |
| AMI | = | acute myocardial infarction |
| CABG | = | coronary artery bypass graft |
| CAD | = | coronary artery disease |
| CDC | = | Centers for Disease Control and Prevention |
| CHF | = | congestive heart failure |
| CKD | = | chronic kidney disease |
| COPD | = | Chronic obstructive pulmonary disease |
| ED | = | emergency department |
| HCUP | = | Health Care Utilization Project |
| ICD-9 | = | International Classification of Diseases-9 |
| ICD-10 | = | International Classification of Diseases-10 |
| ICU | = | intensive care unit |
| MI | = | myocardial infarction |
| MV | = | mechanical ventilation |
| NEDS | = | Nationwide Emergency Department Sample |
| NHANES | = | National Health and Nutrition Examination Surveys III |
| NIS | = | National Inpatient Sample |
| NIV | = | noninvasive ventilation |
| NSTEMI | = | non-ST elevated myocardial infarction |
| PCI | = | percutaneous coronary intervention |
| PE | = | pulmonary embolism |
| PVD | = | peripheral vascular disease |
| SID | = | state inpatient database |
| SEDD | = | State Emergency Department Databases |
| STEMI | = | ST elevation Myocardial Infarction |
| TIA | = | transient ischemic attack |
| US | = | United States |
| VTVF | = | ventricular tachycardia ventricular fibrillation |
Introduction
Chronic obstructive lung disease (COPD) is a common condition associated with significant mortality, morbidity, and healthcare burden. According to the American Lung Association, 16.8 million adults, or 6.6% of adults, reported a diagnosis of COPD in 2018 [Citation1], with an additional 12 million being undiagnosed [Citation2]. The Centers for Disease Control and Prevention (CDC) had reported the mortality rate had decreased from 1999 to 2014 from 43.4 per 100,000 to 39.1 per 100,000 in 2014 [Citation3]. Although the decrease in mortality, COPD remains the third major cause of mortality globally [Citation4]. COPD is characterized by irreversible airflow limitation, with persistent respiratory symptoms due to airway abnormalities caused by repeated exposures to noxious stimuli [Citation5]; it affects 5–10% of the United States (US) population [Citation6,Citation7]. Each year in the US, COPD accounts for 15.4 million physician visits and 726,000 hospitalizations [Citation6]. COPD-related ED encounters have increased from the years 1993 to 2014, with 2016 having more than 2 million visits [Citation8]. Given its chronicity and prevalence, the total economic cost in the US is $49.9 billion annually [Citation8]. The economic and social burden caused by COPD will linger due to the inflammatory spillover hypothesis leading to numerous comorbidities [Citation9,Citation10]. In addition to the aging population, use tobacco [Citation11], and known rising healthcare costs [Citation12].
As COPD is one of the leading causes of death, trailing only ischemic heart disease and cerebrovascular disease, it is imperative to continue to report and identify COPD trends to help with policy-making decisions to reduce burden of disease and modify disease management policies to improve patient outcomes. Acute exacerbation of COPD is considered a major determinant in health status in COPD [Citation13]. It is also an independent positive predictor of mortality, and disease progression among all COPD patients [Citation14]. Previous studies from Nationwide Inpatient Sample (NIS) database for the years 2002–2010 and 2005–2014 reported steady rates of hospitalizations related to COPD, with improvement in mortality over the study years [Citation12,Citation15]. However, there is limited available data regarding the recent trends of mortality and incidence from emergency departments in the United States. The objective of this study is to analyze the trends in mortality, incidence, and complications of COPD exacerbation in EDs using the National Emergency Database from 2010 to 2018.
Methods
This is an observational cohort study of patients who had COPD exacerbation encounters created in the emergency departments during the years 2010–2018 in the Nationwide Emergency Department Sample (NEDS) Database. The NEDS constitutes an approximately 20% sample of hospital-owned emergency departments and in-patient sample in the United States. Since the database constitutes only 20% of the population, a weighted analysis is recommended to generalize it for the whole population of the United States [Citation16]. Using a stratified, random sampling design, a sample of hospital-owned emergency departments and in-patient sample from the United States participating in both the State Inpatient Databases (SID) and the State Emergency Department Databases (SEDD) were selected, and 100% of the emergency departments visits from the selected hospital-owned emergency departments were retained. Hospitals were included in the NEDS sample based on geographic region (northeast, mid-west, west, or south), location (urban or rural), teaching status (teaching or non-teaching), ownership (public, private not for profit, private for-profit), and trauma center designation. A total of 950 emergency departments were included in the national emergency department database. From each selected emergency department and in-patient encounter, all visits were included, which amounted to more than 33 million unweighted visits each year. (Detailed information about the database is available from http://www.hcup-us.ahrq.gov/tech_assist/faq.jsp). Patients with age <18 years at the time of presentation were excluded from the study. Furthermore, as per the ethical criteria set up by HCUP, we excluded any numbers less than or equal to 10 in the study as we acknowledge that the risk of identification of individuals is increased when observations (i.e. individual discharge records) in any given cell of tabulated data is less than or equal to 10 [Citation17]. Being a public database, the study was exempt from institutional review board evaluation; however, it was performed according to the ethical criteria established by the Healthcare Cost and Utilization Project (HCUP) [Citation17]. Furthermore, this database cannot see causation, we can only evaluate association. Therefore, we have grouped some of the variables as complications associated with COPD exacerbation as these variables have been related as complications of COPD exacerbation in previously published studies [Citation18–21].
Study definitions
COPD exacerbation was defined by International Classification of Diseases-9 (ICD-9) codes of 491.21 and 493.22 and ICD-10 codes of J44.1 and J47.1. The ICD codes utilized to identify various complications and comorbidities were obtained from online websites, and the information of these websites is given in supplementary file 1 (supplementary material). We have categorized the patients of COPD exacerbation into two groups based on the absence of associated factors like pulmonary embolism, pneumonia, or acute heart failure exacerbation in acute exacerbation of COPD (AECOPD group) and the AECOPD-plus group defined as AECOPD associated with acute heart failure exacerbation, acute pulmonary embolism, or pneumonia. We also extracted data related to cerebrovascular events (transient ischemic attack (TIA) and acute ischemic stroke), cardiac events (ventricular tachycardia or fibrillation (VTVF), atrial fibrillation (AF), cardiogenic shock), ST-elevated Myocardial Infarction (STEMI), and Non-ST-elevated Myocardial infarction (NSTEMI), renal events (acute kidney injury), infectious events (sepsis, septic shock, cellulitis and urosepsis), and pulmonary hypertension (PH) group III using ICD codes.
Patient and hospital characteristics
Baseline patient demographic characteristics (age, sex, insurance payer) were extracted from the database. Diagnostic codes were used to identify hypertension, diabetes mellitus, hyperlipidemia, obesity, smoker, AF, family history of CAD, prior stroke, prior myocardial infarction (MI), prior percutaneous coronary interventions (PCI), prior coronary artery bypass grafting (CABG), peripheral vascular disease (PVD), COPD and chronic kidney injury (CKD) using ICD-9 and ICD-10 codes.
Outcomes
The primary outcome of the study was to evaluate the in-hospital mortality rates between the AECOPD versus the AECOPD-plus group. We also evaluated several important complications associated with both subgroups of patients among all COPD exacerbation population. Additional trends evaluated were mortality and incidence among the AECOPD groups, and the incidence trend of smokers among the patients of the AECOPD group over the study years 2010–2018.
Statistical methods
Categorical variables were expressed as weighted values along with percentages, and continuous variables were expressed as mean ± standard deviation if the variable was not skewed and as median with 25th and 75th percentiles otherwise. Descriptive statistics were performed for demographics and comorbidities, which were stratified by the AECOPD and AECOPD-plus groups. We used a statistical survey procedure to perform a weighted analysis. Pearson’s chi-square test for categorical variables and t-test for the continuous variables.
Furthermore, we assessed the yearly trends in mortality, the yearly incidence of AECOPD and smokers among patients with AECOPD over the years 2010–2018 and examined their linear trends. All analyses were weighted analyses. Statistical analysis was performed using STATA version 16.1 (College Station, Texas). All p values were two sided, with a significance threshold of p < 0.05.
Results
Out of the total 1,082 billion ED visits from 2010 to 2018, 5,295,408 (mean age 63.31 ± 12.63 years, 55% females) were admitted with a diagnosis of COPD exacerbation. Among these patients, 353,563 (6.7%) had AECOPD-plus while 4,941,845 (93.3%) had strictly AECOPD. The AECOPD subgroup were predominately elderly, females and smokers compared to the AECOPD-plus group who were predominately males; the AECOPD-plus group also had higher comorbidity burden including hypertension, diabetes mellitus, hyperlipidemia, obesity, CKD, prior MI, PCI, or CABG. Additionally, Medicare was the predominant primary payer among both study groups. The baseline characteristics of patients with both groups are presented in .
Table 1. Baseline characteristics associated with AECOPD (defined as AECOPD without any concomitant acute cardiopulmonary disease) and AECOPD plus (defined as AECOPD with a concomitant acute cardiopulmonary disease process, such as acute CHF, pulmonary embolism, or pneumonia)
Other associated complications during hospitalization encounter
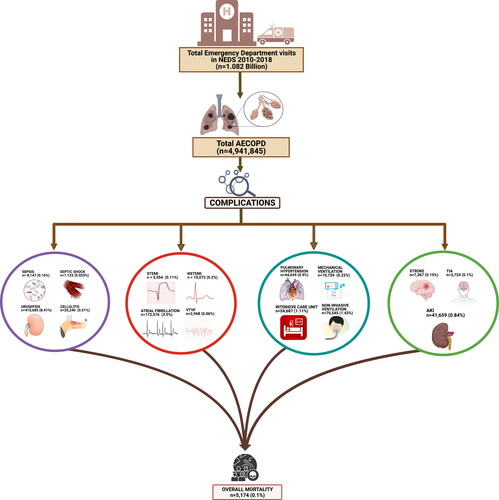
Among the AECOPD group, other major associated complications included acute ischemic stroke (7,367 or 0.15%), TIA (3,725 or 0.1%), AKI (41,659 or 0.84%), AF (172,576 or 3.5%), VT/VF (2,968 or 0.06%), STEMI (5,554 or 0.11%), NSTEMI (10,072 or 0.2%), sepsis (8,147 or 0.16%), septic shock (1,123 or 0.023%), cellulitis (25,240 or 0.51%), urosepsis (415,685 or 8.41%) and pulmonary hypertension (44,649 or 0.9%). Additionally, a significant number of patients (81,304 or 1.6%) developed acute respiratory failure; 70,545 (1.43%) required NIV, 54,687 (1.11%) required ICU admission, and 10,759 (0.22%) required MV. Furthermore, a total of 5,174 (0.1%) had in-hospital deaths. All complications associated with AECOPD are presented in .
Figure 1. Graphical representation for the complications among acute exacerbation of chronic obstructive pulmonary disease (AECOPD) patient population, created using Biorender.com. STEMI, ST-elevation myocardial infarction; NSTEMI, non-ST-elevation myocardial infarction; VTVF, ventricular tachycardia/fibrillation; AKI, acute kidney injury (created with biorender.com).
In the AECOPD-plus group, other major accompanying complications included acute ischemic stroke (959 or 0.27%), TIA (258 or 0.07%), AKI (8,107 or 2.27%), AF (19,753 or 5.6%), VT/VF (502 or 0.14%), STEMI (805 or 0.22%), NSTEMI (2,308 or 0.65%), sepsis (10,091 or 2.85%), septic shock (224 or 0.063%), cellulitis (1,484 or 0.42%), urosepsis (21,064 or 6%) and pulmonary hypertension (12,568 or 3.6%). A significant number of patients (12,303 or 3.5%) developed acute respiratory failure; 9,849 (2.8%) required NIV, 10,507 (3%) required ICU admission, and 2,454 (0.7%) required MV. Additionally, a total of 2,542 (0.7%) had in-hospital related deaths. All complications associated with AECOPD-plus are presented in . All the related complications and mortality rates between the two groups are statistically significant with p-value <0.001. compares the complication rates in AECOPD versus AECOPD-plus groups.
Figure 2. Graphical representation for the complications among acute exacerbation of chronic obstructive pulmonary disease (AECOPD) plus patient population, created using Biorender.com. STEMI, ST-elevation myocardial infarction; NSTEMI, non-ST-elevation myocardial infarction; VTVF, ventricular tachycardia/fibrillation; AKI, acute kidney injury (created with biorender.com).
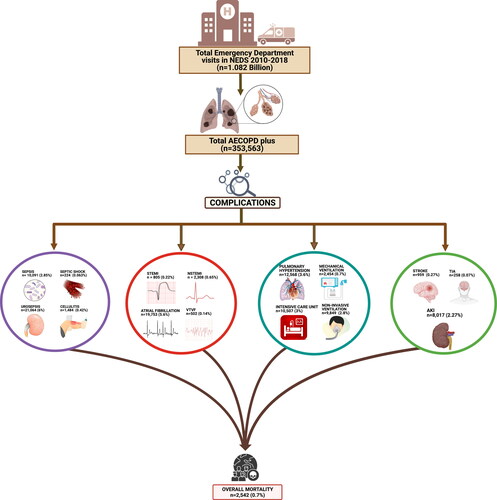
Table 2. Complications associated with AECOPD (defined as AECOPD without any concomitant acute cardiopulmonary disease) and AECOPD plus (defined as AECOPD with a concomitant acute cardiopulmonary disease process, such as acute CHF, pulmonary embolism, or pneumonia)
Disposition
Among the total of 4,941,845 (93.3%) patients with AECOPD, 4,425,692 (89.5%) were discharged home, 54,211 (1.2%) were discharged with home health care, 342,830 (6.9%) were discharged to a skilled care facility or inpatient rehabilitation facility, 110,040 (2.2%) left against medical advice, 5,174 (0.1%) died in the ED. Lastly, 3,897 (0.1%) were admitted to inpatient services.
Of the total AECOPD-plus group 353,563 (6.7%), 247,836 (70.1%) were discharged home, 7,094 (2%) were discharged with home health care, 84,369 (23.9%) were discharged to a skilled care facility or inpatient rehabilitation facility, 10,356 (2.9%) left against medical advice, 1,366 (0.4%) had died in the ED and 2,542 (0.7%) were admitted to inpatient services. Disposition of both groups are illustrated in .
Table 3. Disposition associated with AECOPD (defined as AECOPD without any concomitant acute cardiopulmonary disease) and AECOPD plus (defined as AECOPD with a concomitant acute cardiopulmonary disease process, such as acute CHF, pulmonary embolism, or pneumonia)
Trends
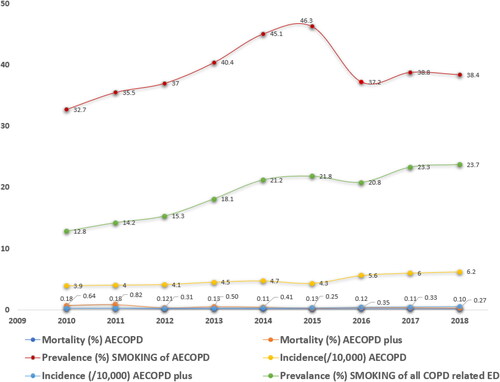
The incidence of AECOPD has increased from 3.9/10,000 in 2010 to 6.2/10,000 in 2018 (linear p-trend 0.004) while the incidence for AECOPD-plus had increased from 0.22/10,000 in 2010 to 0.49/10,000 in 2018 (liner p-trend 0.0003). The mortality trend for AECOPD had decreased from 0.18% in 2010 to 0.10% in 2018 (linear p-trend 0.0055). Meanwhile, the mortality trend for AECOPD-plus had also decreased from 0.64% in 2010 to 0.27% in 2018 (linear p-trend 0.002). The prevalence of smoking among COPD exacerbation encounters had increased from 12.8/10,000 to 23.7/10,000 from 2010 to 2018 (p-value 0.004). However, the prevalence of smoking among AECOPD groups was static over the years 2010–2018 (p-value 0.2). The results are depicted in .
Discussion
The salient findings of our study are as follows: (1) The incidence of AECOPD between both groups had increased significantly while the mortality trend had improved significantly. (2) The overall prevalence of smoking rates among COPD exacerbation had increased significantly. (3) The AECOPD-plus patient population had higher cardiovascular complication burden when compared to the AECOPD group (p-value <0.001). (4) Mortality rates were significantly higher among patients of the AECOPD-plus subgroup (0.7% vs 0.1%; p < 0.001). (5) The AECOPD-plus patient population had higher rates of admission to skilled nursing facility (23.9% vs 6.9%; p-value <0.001) when compared to the AECOPD subgroup.
During the study years of 2010–2018, the overall incidence of total COPD exacerbation had nearly doubled; meanwhile the mortality rates had approximately halved. Previous studies using NEDS had also shown an increase in ED visits for COPD exacerbation, which is concordant with our study [Citation22,Citation23]. One plausible cause of the overall increased incidence of COPD exacerbation can be attributed to the overall increase smoking prevalence seen in the study years given the parallel observation of increasing trends of smoking as depicted in . Moreover, in the last decade, there had been a dramatic increase in the use of e-cigarette with unknown long-term effects, which further contributes to the increase in smoking prevalence [Citation24,Citation25].
Similarly, between 2008 and 2012 there has also been a significant increase in the prevalence of cigar smoking which has further contributed to smoking prevalence trends [Citation26]. We observed a static trend of smoking among AECOPD groups during 2010–2018, compared to previous trends and reports of decreasing smoking prevalence [Citation22,Citation27–29]. Universally, smoking has been notorious as the primary risk factor for developing COPD. As a result, the rate of COPD is 4.3 times higher among current smokers and 3.7 times higher among former smokers [Citation30]. Given the prevalence of smoking seen in developed countries, the prevalence of COPD is projected to increase over the next 40 years and may contribute to 5.4 million annual deaths [Citation11,Citation31]. Despite improvement in primary care and focus on smoking cessation the rates were static for the years 2010–2018. These findings are undoubtedly concerning and clinicians should apply greater emphasis on smoking cessation to alleviate the social and financial burden that COPD has on our healthcare system.
Another explanation for the increased incidence of total COPD exacerbation would be the decreasing COPD-related mortality rate in patients aged 64–75, supplanted by the rising mortality rate in patients 85 and above, with overall trends in mortality improving; these findings are consistent with our own [Citation32]. Despite the increasing incidence trend of COPD exacerbation in both AECOPD groups, we observed an improved mortality trend over the study years as has been reported previously [Citation12,Citation15]. It is reasonable to infer from these data that patients with COPD are living longer. Along with this, studies have also shown that as patients get older, trends of readmission have also been increasing, particularly in ages 70 and above [Citation33]. These studies suggest an explanation for our study findings that perhaps the rise in the incidence of COPD exacerbation is due to readmissions of patients with recurrent COPD exacerbation. The improvement in mortality could be secondary to adherence to inhalation therapy [Citation34] but also to other comprehensive modalities in the management of COPD such as pulmonary rehab, long-term oxygen therapy and use of noninvasive ventilation along with improved early diagnosis [Citation35–38]. The National Health and Nutrition Examination Surveys III (NHANES III) estimated that in 2000 there were 10 million physician-diagnosed COPD cases, while approximately 24 million US adults had impaired lung function without a concomitant diagnosis of COPD, leading to underdiagnosis [Citation27].
The AECOPD-plus patient population had a strong association with cardiovascular complications. In this population, patients were more likely to experience STEMI (0.22% vs 0.11%; p-value <0.001) and NSTEMI (0.65% vs 0.2%; p-value <0.001). It had been reported that the prevalence of COPD among acute coronary syndromes (ACS) can be as high as 7–30% [Citation39]. The higher rates could be secondary to the chronic inflammatory state in these patients, which precipitates ACS. Previous studies have shown an increase in acute phase reactants such as interleukin-6, fibrinogen, and C-reactive protein which can worsen atherosclerosis [Citation40,Citation41]. Our study showed the AECOPD-plus subgroup were more likely to develop AF with rapid ventricular rate (5.6% vs 3.5%; p-value <0.001) and VT/VF (0.14% vs 0.06%; p-value <0.001). Previous studies mirrored our study findings in that AF was the most commonly seen cardiovascular complication, as the risk of developing AF is 28% in patients with COPD [Citation42]. Factors contributing to this risk are reduced forced expiratory volume in 1 s (FEV1), hypercapnia, and higher levels of pulmonary artery pressures [Citation43]. The higher rates of coronary events and arrhythmias seen in AECOPD patient population are concerning and hence call for timely management and proper counseling of patients in the primary care settings may improve patient outcomes.
Our data showed that AECOPD-plus carried a greater risk of mortality and complications than AECOPD. The risk of ICU admission (3.0% vs 1.11%; p < 0.001), in-hospital mortality (0.7% vs 0.1%; p < 0.001), and ED mortality (0.4% vs 0.1%; p < 0.001) were all shown to be greater in the AECOPD-plus group compared to the AECOPD group. The complication rates follow a similar trajectory. Across the board, patients in the AECOPD-plus group had higher risk of developing sepsis (2.85% vs 0.16%). This may be explained by the increased use of systemic steroids as the standard guideline for AECOPD patients leading to immunosuppression [Citation44]. Interestingly, sepsis secondary to urinary infections was found to have lower incidence in the AECOPD-plus group (6.0% vs 8.41%) compared to the AECOPD group. One explanation is that the AECOPD-plus population, especially in conjunction with pneumonia, are treated with broad-spectrum antibiotics which may provide prophylaxis treatment against known pathogens which causes urinary tract infections [Citation45]. Pulmonary Hypertension (PH) is a particularly interesting complication as it is four times more prevalent in the AECOPD-plus group (3.6% vs 0.9; p-value <0.001) compared to the AECOPD group which could partially be attributed to concomitant CHF and PE [Citation46]. Overall, we can infer from this data that AECOPD-plus carries greater morbidity and mortality than AECOPD.
In comparing patient disposition between AECOPD and AECOPD-plus groups, we found that the AECOPD group had lower rates of admission and less discharge needs likely because these patients did not have associated features of PE or CHF. A significantly greater proportion of patients with AECOPD-plus (0.7% vs 0.1%; p-value <0.001) were admitted to inpatient services and required discharge to a skilled nursing facility (23.9% vs 6.9%; p-value <0.001) compared to AECOPD. This is consistent with other studies that showed COPD and CHF are both independent risk factors that have been shown to increase the likelihood of SNF admission [Citation47]. Therefore, we can suggest from our study that AECOPD concomitant with CHF, PE and pneumonia, confers an even higher likelihood of SNF admission. One proposed explanation for this is that patients with AECOPD complicated with acute CHF tend to have longer hospitalization, thus resulting in greater morbidity and rehabilitation needs [Citation48]. It can be surmised from this data that COPD exacerbation concomitant with other cardiopulmonary processes is more debilitating to patients and requires greater healthcare needs. These factors may help suggest that the rising incidence of COPD exacerbation could contribute to the well-documented economic burden of COPD on both patients and the healthcare system [Citation49].
Our study has several limitations. First and foremost, this is a retrospective observational study. These inferences regarding causation should be made with caution. Additionally, we relied on reported ICD-9 and ICD-10 codes to obtain billable diagnoses. NEDS is an administrative database that is subjected to inaccurate coding and underreporting and misclassification of comorbid conditions. Furthermore, there is also lack of inference from objective data such as physical examination findings, imaging, laboratory, and diagnostic studies that can provide insight into the severity of COPD. NEDS database can only extrapolate an association of any variable with the event. However, this database and the codes used in this study have been practical in multiple clinical studies as it provides us with a nationally representative sample and is considered an exceedingly reliable database.
Conclusion
In summary, COPD exacerbation is a common urgent medical condition encountered in the US emergency departments. It is associated with significant rates of morbidity and mortality. Interestingly, the yearly trends of COPD exacerbation had increased annually between 2010 to 2018, however, the yearly mortality trend had improved significantly. AECOPD is associated with decreased morbidity and mortality than AECOPD-plus (associated with acute heart failure, PE, and pneumonia). Furthermore, our data suggest that the rising burden of AECOPD needs urgent attention from physicians and policy makers to improve diagnostics and informed policies regarding management. More research in improvement in primary care, risk stratification, smoking cessation, and vaccination can help in improving the frequent hospitalizations and mortality related to COPD exacerbation.
Authors’ contributions
PN, MMU, TM had substantial contributions to the acquisition, analysis, or interpretation of data for the work. PN, MMU, TM, AK, NR, AP, TH, MAB, and IU also had contributions in drafting the work or revising it critically for important intellectual content. PN, MMU, TM, AK, NR, AP, TH, MAB, IU, PP, PL, GS, PK, and AS had final approval of the version to be published and had agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Tanveer Mir is guarantor.
Declaration of interest
The authors whose names are listed immediately below certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Funding
The author(s) reported there is no funding associated with the work featured in this article.
References
- COPD Prevalence | American Lung Association. Accessed May 1, 2021. https://www.lung.org/research/trends-in-lung-disease/copd-trends-brief/copd-prevalence.
- National Institutes of Health. National Heart, Lung, and Blood, Institute. Morbidity & mortality: 2012 Chart book on cardiovascular, lung, and blood diseases. National Institutes of Health
- CDC. Age-standardized death rates for chronic obstructive pulmonary disease (COPD) – United States, 1999–2014; 1999. Accessed May 1, 2021. http://wonder.cdc.gov.
- Chronic Obstructive Pulmonary Disease – Level 3 cause | Institute for Health Metrics and Evaluation. Accessed September 5, 2021. http://www.healthdata.org/results/gbd_summaries/2019/chronic-obstructive-pulmonary-disease-level-3-cause.
- 2021 GOLD Reports – Global Initiative for Chronic Obstructive Lung Disease – GOLD. Accessed April 10, 2021. https://goldcopd.org/2021-gold-reports/.
- Chronic Obstructive Pulmonary Disease Surveillance –- United States, 1971–2000. Accessed April 10, 2021. https://www.cdc.gov/mmWR/preview/mmwrhtml/ss5106a1.htm.
- Halbert RJ, Isonaka S, George D, et al. Interpreting COPD prevalence estimates: what is the true burden of disease? Chest. 2003;123(5):1684–1692. DOI:https://doi.org/10.1378/chest.123.5.1684
- COPD Burden | American Lung Association. Accessed April 10, 2021. https://www.lung.org/research/trends-in-lung-disease/copd-trends-brief/copd-burden.
- Barnes PJ. Chronic obstructive pulmonary disease: effects beyond the lungs. PLoS Med. 2010;7(3):e1000220–4. DOI:https://doi.org/10.1371/journal.pmed.1000220
- Naik D, Joshi A, Paul TV, et al. Chronic obstructive pulmonary disease and the metabolic syndrome: Consequences of a dual threat. Ind J Endocrinol Metab. 2014;18(5):608–616. DOI:https://doi.org/10.4103/2230-8210.139212
- Lopez AD, Shibuya K, Rao C, et al. Chronic obstructive pulmonary disease: current burden and future projections. Eur Respir J. 2006;27(2):397–412. DOI:https://doi.org/10.1183/09031936.06.00025805
- Jinjuvadia C, Jinjuvadia R, Mandapakala C, et al. Trends in outcomes, financial burden, and mortality for acute exacerbation of chronic obstructive pulmonary disease (COPD) in the United States from 2002 to 2010. J Chronic Obstr Pulm Dis. 2017;14(1):72–79. DOI:https://doi.org/10.1080/15412555.2016.1199669
- Wedzicha JA, Singh R, Mackay AJ. Acute COPD exacerbations. Published online 2014. DOI:https://doi.org/10.1016/j.ccm.2013.11.001
- Donaldson GC, Seemungal TAR, Bhowmik A, et al. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002;57(10):847–852. DOI:https://doi.org/10.1136/thorax.57.10.847
- Goel K, Bailey M, Borgstrom M, et al. Trends in chronic obstructive pulmonary disease hospitalization and in-hospital deaths in the United States by sex: 2005 to 2014. Ann Am Thorac Soc. 2019;16(3):391–393. DOI:https://doi.org/10.1513/AnnalsATS.201807-488RL
- NEDS Overview. Accessed May 7, 2021. https://www.hcup-us.ahrq.gov/nedsoverview.jsp.
- HCUP-US Home Page. Accessed May 7, 2021. https://hcup-us.ahrq.gov/.
- Díez J de M, Morgan JC, García RJ. The association between COPD and heart failure risk: a review. Int J Chron Obstruct Pulmon Dis. 2013;8:305–312. DOI:https://doi.org/10.2147/COPD.S31236
- Gautam SS, O’Toole RF. Convergence in the epidemiology and pathogenesis of COPD and pneumonia. J Chronic Obstr Pulm Dis. 2016;13(6):790–798. DOI:https://doi.org/10.1080/15412555.2016.1191456
- Aleva FE, Voets LWLM, Simons SO, et al. Prevalence and localization of pulmonary embolism in unexplained acute exacerbations of COPD: a systematic review and Meta-analysis. Chest. 2017;151(3):544–554. DOI:https://doi.org/10.1016/j.chest.2016.07.034
- Yang M, Du Y, Chen H, et al. Inhaled corticosteroids and risk of pneumonia in patients with chronic obstructive pulmonary disease: a meta-analysis of randomized controlled trials. Int Immunopharmacol. 2019;77 doi:https://doi.org/10.1016/j.intimp.2019.
- Ford ES. Hospital discharges, readmissions, and ED visits for COPD or bronchiectasis among US adults: findings from the nationwide inpatient sample 2001–2012 and nationwide emergency department sample 2006–2011. Chest. 2015;147(4):989–998. DOI:https://doi.org/10.1378/chest.14-2146
- Singh JA, Yu S. Utilization due to chronic obstructive pulmonary disease and its predictors: a study using the U.S. National Emergency Department Sample (NEDS). Respir Res. 2016;17(1):1 DOI:https://doi.org/10.1186/s12931-015-0319-y
- Gentzke AS, Creamer M, Cullen KA, et al. Vital signs: Tobacco product use among Middle and high school students – United States, 2011–2018. Morb Mortal Wkly Rep. 2019;68(6):157–164. DOI:https://doi.org/10.15585/mmwr.mm6806e1
- Cullen KA, Gentzke AS, Sawdey MD, et al. e-Cigarette use among youth in the United States, 2019. J Am Med Assoc. 2019;322(21):2095–2103. DOI:https://doi.org/10.1001/jama.2019.18387
- Patterns of Tobacco Use Among U.S. Youth, Young Adults, and Adults – The Health Consequences of Smoking – 50 Years of Progress – NCBI Bookshelf. Accessed August 24, 2021. https://www.ncbi.nlm.nih.gov/books/NBK294302/?report=reader.
- Mannino DM, Homa DM, Akinbami LJ, et al. Chronic obstructive pulmonary disease surveillance–United States, 1971-2000. Respir Care. 2002;47(10):1184–1199.
- Current Cigarette Smoking Among Adults in the United States | CDC. Accessed May 1, 2021. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm.
- Tobacco Trends Brief | American Lung Association. Accessed May 1, 2021. https://www.lung.org/research/trends-in-lung-disease/tobacco-trends-brief/overall-tobacco-trends.
- COPD Risk Factors and Patient Characteristics | American Lung Association. Accessed April 12, 2021. https://www.lung.org/research/trends-in-lung-disease/copd-trends-brief/copd-risk-factors.
- WHO | Projections of mortality and causes of death, 2016 to 2060. WHO. Published online 2018. Accessed April 12, 2021. http://www.who.int/healthinfo/global_burden_disease/projections/en/.
- Ford ES. Trends in mortality from COPD among adults in the United States. Chest. 2015;148(4):962–970. DOI:https://doi.org/10.1378/chest.14-2311
- Genao L, Durheim MT, Mi X, et al. Early and long-term outcomes of older adults after acute care encounters for chronic obstructive pulmonary disease exacerbation. Ann Am Thorac Soc. 2015;12(12):1805–1812. DOI:https://doi.org/10.1513/AnnalsATS.201504-250OC
- Vestbo J, Anderson JA, Calverley PMA, et al. Adherence to inhaled therapy, mortality and hospital admission in COPD. Thorax. 2009;64(11):939–943. DOI:https://doi.org/10.1136/thx.2009.113662
- Puhan MA, Gimeno-Santos E, Scharplatz M, et al. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. In: Cochrane database of systematic reviews. Wiley; 2011. DOI:https://doi.org/10.1002/14651858.cd005305.pub3
- Murphy PB, Rehal S, Arbane G, et al. Effect of home noninvasive ventilation with oxygen therapy vs oxygen therapy alone on hospital readmission or death after an acute COPD exacerbation: a randomized clinical trial. J Am Med Assoc. 2017;317(21):2177–2186. DOI:https://doi.org/10.1001/jama.2017.4451
- Kvale PA, Conway WA, Coates EO. Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: a clinical trial. . Ann Intern Med. 1980;93(3):391–398. DOI:https://doi.org/10.7326/0003-4819-93-3-391
- Qaseem A. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179. DOI:https://doi.org/10.7326/0003-4819-155-3-201108020-00008
- Rothnie KJ, Yan R, Smeeth L, et al. Risk of myocardial infarction (MI) and death following MI in people with chronic obstructive pulmonary disease (COPD): a systematic review and Meta-analysis. BMJ Open. 2015;5(9):e007824 DOI:https://doi.org/10.1136/bmjopen-2015-007824
- Mannino DM, Thorn D, Swensen A, et al. Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur Respir J. 2008;32(4):962–969. DOI:https://doi.org/10.1183/09031936.00012408
- Sin DD, Paul Man SF. Why are patients with chronic obstructive pulmonary disease at increased risk of cardiovascular diseases? The potential role of systemic inflammation in chronic obstructive pulmonary disease. Circulation. 2003;107(11):1514–1519. DOI:https://doi.org/10.1161/01.CIR.0000056767.69054.B3
- Grymonprez M, Vakaet V, Kavousi M, et al. Chronic obstructive pulmonary disease and the development of atrial fibrillation. Int J Cardiol. 2019;276:118–124. DOI:https://doi.org/10.1016/j.ijcard.2018.09.056
- Terzano C, Romani S, Conti V, et al. Atrial fibrillation in the acute, hypercapnic exacerbations of COPD. Eur Rev Med Pharmacol Sci. 2014;18:2908–17.
- Barshes NR, Goodpastor SE, Goss JA. Pharmacologic immunosuppression. Front Biosci. 2004;9:411–420. DOI:https://doi.org/10.2741/1249
- Boersma WG. Antibiotics in acute exacerbations of COPD: the good, the bad and the ugly. Eur Respir J. 2012;40(1):1–3. DOI:https://doi.org/10.1183/09031936.00211911
- Frost A, Badesch D, Gibbs JS, et al. Diagnosis of pulmonary hypertension. Eur Resp J. 2019;53:1801904.. DOI:https://doi.org/10.1183/13993003.01904-2018
- McAvay GJ, Vander Wyk B, Allore H. Individual heterogeneity in the probability of hospitalization, skilled nursing facility admission, and mortality. J Gerontol Ser A. 2021;76(9):1668–1677. DOI:https://doi.org/10.1093/gerona/glaa314
- Hawkins NM, Petrie MC, Jhund PS, et al. Heart failure and chronic obstructive pulmonary disease: diagnostic pitfalls and epidemiology. Eur J Heart Fail. 2009;11(2):130–139. DOI:https://doi.org/10.1093/eurjhf/hfn013
- Iheanacho I, Zhang S, King D, et al. Economic burden of chronic obstructive pulmonary disease (COPD): a systematic literature review. Int J Chron Obstruct Pulmon Dis. 2020;15:439–460. DOI:https://doi.org/10.2147/COPD.S234942