Abstract
Physical activity monitoring technology (e.g. smartphone apps or wearables) can objectively record physical activity levels, potentially support interventions to increase activity levels, and support the self-management of Chronic Obstructive Pulmonary Disease (COPD). Insight into patients’ experiences of monitoring physical activity is needed to inform future healthcare practice and policy utilizing this technology to support long-term positive health behavior change. This scoping review aimed to explore the experiences of using technology for monitoring physical activity among people with COPD. The Joanna Briggs Institute scoping review methodological framework was used. Relevant scientific databases (CINAHL Complete, MEDLINE, PsycINFO, SPORTDiscus, Cochrane Library and Scopus) were searched from 1st January 2016 to 16th March 2021. Thematic synthesis was used to analyze the data. Twelve studies exploring the experiences of people with COPD using technology for monitoring physical activity were included in the synthesis. Seven themes were developed and summarize experiences: 1) Monitoring and keeping track of their activity and health, 2) Supporting motivation to be active, 3) Acceptability of the device, 4) Experiencing technical issues with the device, 5) Setting appropriate and achievable goals for their health condition, 6) Integrating the device into their life and daily routine, and 7) Perceived physical and psychological benefits of using the device. Further high-quality research is needed to understand the experiences of people with COPD using technology to monitor physical activity in everyday life and better self-manage their health condition. Supporting people with COPD to monitor their physical activity could enable them to better self-manage their health condition.
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is the third leading cause of death globally [Citation1]. COPD is a progressive disease characterized by airflow limitation due to airway and/or alveolar abnormalities [Citation2]. Early diagnosis and treatment can slow its progression and help with the management of the disease [Citation3].
Pulmonary rehabilitation is an evidence-based, multidisciplinary, and comprehensive intervention for patients with chronic respiratory diseases, such as COPD [Citation4]. Pulmonary rehabilitation improves health related quality of life, and increases exercise capacity [Citation5]. Although one of the main aims of the intervention is to increase exercise capacity, it is not clear if increased physical activity levels are maintained long term (i.e. one-year post pulmonary rehabilitation) [Citation6]. Therefore, additional support may be needed to integrate daily physical activity into the lives of people with COPD during and after a pulmonary rehabilitation course.
Smartphone applications and wearable devices have been used in interventions with people with COPD to monitor their activity, to investigate if there is an objective improvement over time, and/or to see if the monitor itself can facilitate increases in physical activity levels [Citation7]. Various activity monitors have been used in research to objectively measure physical activity levels. The accuracy, reliability and validity of such devices has been assessed extensively [Citation8–11]. Regardless of their accuracy, commercially available devices for monitory everyday activity are becoming increasingly utilized in everyday life [Citation12, Citation13]. However, evidence on whether activity monitors can support increases in physical activity levels as part of an intervention for people with COPD is mixed and limited [Citation14, Citation15]. Some evidence suggests physical activity promotion interventions using pedometers (either stand alone or alongside pulmonary rehabilitation) can increase steps per day in people with COPD [Citation16–19]. Among people with COPD, using activity trackers can increase motivation to be active and increase awareness of physical activity levels [Citation20]. An online survey of Dutch patients with COPD using activity monitors (i.e. Fitbit, smartphone, pedometer or smartwatch) reported better insights into their daily performance and activity, felt encouraged to accomplish more physical activity, and the activity monitor offered benefits in addition to their medication [Citation21]. Using technology has been found to be acceptable to support physical activity, with the potential to increase physical activity levels, in people with COPD [Citation22–24]. Direct feedback from self-monitoring physical activity using an app or wearable may help patients with COPD to create strategies for and to manage their everyday lives [Citation25, Citation26].
Monitoring technology, such as smartphone apps or wearables, has the potential to support interventions to increase activity levels and awareness of physical activity, and support the self-management of COPD. However, insight into patients’ experiences of using physical activity monitoring devices is needed to inform future healthcare practice and policy utilizing the technology to support long-term positive health behavior change. Therefore, this scoping review aims to qualitatively explore the experiences of people with COPD using technology to monitor physical activity.
Aim and research question
This review aims to qualitatively explore the experiences of people with COPD using physical activity monitors within the published literature. The research question is: what is known about the experiences of using technology for monitoring physical activity among people with COPD? The research aim was developed based on the Joanna Briggs Institute “PCC” mnemonic [Citation27]; Population – people with COPD, Concept – experiences of using technology, and Context – monitoring physical activity.
Methods
The five stages of the Joanna Briggs Institute scoping review methodological framework by Arksey and O’Malley [Citation28] was followed in this study. The stages are: 1) identify the research question, 2) identify relevant studies, 3) study selection, 4) charting the data, 5) collating, summarizing and reporting the results. The Joanna Briggs Institute manual for conducting scoping reviews was used to guide the development of the a-priori protocol and reporting of the review [Citation27] alongside the Enhanced Transparency of Reporting the Synthesis of Qualitative Research framework [Citation29].
Types of sources
Published journal articles, abstracts and conference proceedings were considered for inclusion in the review.
Search strategy
An electronic search of CINAHL Complete, MEDLINE, PsycINFO, SPORTDiscus, Cochrane Library and Scopus was conducted on March 16, 2021. Databases were searched for studies published since January 2016; covering the last 5 years to include the most recent information on experiences of using technology. Technology is a rapidly changing field with usability issues being constantly improved. Exploring experiences over the last 5 years provides an understanding of the current experiences of people with COPD and reflects the most recent developments in technology.
The search strategy (see Supplemental Material A) was adapted from Wilde et al. [Citation30] and Halbert et al. [Citation31]. Adaptations included adding COPD specific terms (e.g. COPD, “chronic obstructive*”, “pulmonary disease*”, etc.). Terms were used to search titles, abstracts, and keywords, except terms searching for studies with children were searched on titles only for exclusion. Searches were restricted by date (01/01/2016 to 16/03/2021) and texts written in English. Reference lists of included studies were also searched for any eligible studies.
Eligibility criteria
Inclusion and exclusion criteria () were adapted from Wilde et al. [Citation30] to specifically apply to people with COPD.
Table 1. Inclusion and exclusion criteria.
Synthesis of findings
Thematic synthesis was used to analyze the included studies [Citation32]. The three stages of analysis were followed; 1) relevant text in the studies was coded inductively “line-by-line”, 2) codes were organized into “descriptive themes” developed according to meaning and context, and 3) through “going beyond” the findings of the primary studies, “analytical themes” were generated to answer the research question of this review. Analysis was organized using Microsoft Word and Excel and conducted using “traditional tools” (i.e. colored pens and post-it notes) to facilitate interaction and cognition with the data increasing “the opportunity for interpretative insight leading to a more rigorous analysis procedure” ([Citation33], p. 6). Screening and analysis were conducted by LW in consultation with coauthors (LS, CP, GW, CC).
Results
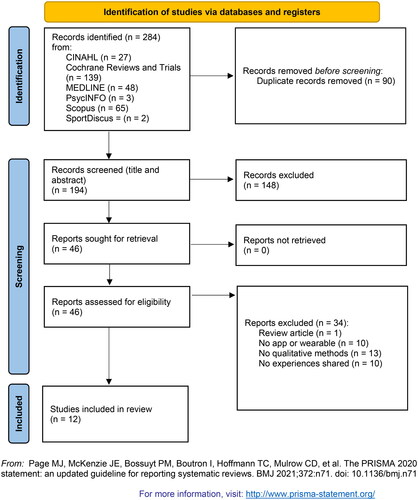
Database searches identified 194 studies for screening following the removal of duplicates. Twelve studies were included in the synthesis (see PRISMA flow diagram [Citation34]). Within the included studies there was a total of 424 qualitative participants.
All but two studies were feasibility studies; one empirical study [Citation35] and one qualitative development study [Citation36]. All but one study [Citation36] involved giving participants activity monitors to use as part of an intervention to increase physical activity levels [Citation35, Citation37–45] or determine whether patients with COPD would, use, wear and maintain use of a smartwatch [Citation36] (see for the type of device used in the included studies and Supplemental Material B for the characteristics of technology used in the included studies). Qualitative data collection methods included open-ended survey questions [Citation38, Citation42, Citation45, Citation46], focus groups [Citation35, Citation42] and semi-structured interviews [Citation35–37, Citation39–41, Citation43–45]. Thematic analysis was the most used qualitative analysis method [Citation36, Citation37, Citation41, Citation42]. Other qualitative analysis methods were content analysis [Citation39, Citation45], constant comparative method [Citation44], Kings Template analysis [Citation43], theory interpreting analysis [Citation35]. Three studies did not report the method of analysis used [Citation35, Citation38, Citation40]. See Supplemental Material C for characteristics of the included studies and Supplemental Material D for details of the participants in the included studies.
Table 2. Type of device used in the included studies.
Seven themes were developed in the synthesis of experiences of using technology for monitoring physical activity among people with COPD: 1) Monitoring and keeping track of their activity and health, 2) Supporting motivation to be active, 3) Acceptability of the device, 4) Experiencing technical issues with the device, 5) Setting appropriate and achievable goals for their health condition, 6) Integrating the device into their life and daily routine, 7) Perceived physical and psychological benefits of using the device.
Theme 1: Monitoring and keeping track of their activity and health
Two studies reported the technology was helpful or useful to participants to monitor and increase their physical activity [Citation41, Citation42].
The step counter was the most useful part and I was a lot more compliant with this than completing the home exercises. (Patient 6, high actual usage score, low contact time; [Citation42], Appendix 8, p. 1)
Many studies reported that participants liked to be able to keep track and see progress on their step counts or physical activity levels, such as through charts or graphs [Citation35, Citation37–39, Citation41, Citation42].
It was neat keeping track of how many steps you take in a day, I had never done that. I thought it was interesting and it regimented me. ([Citation38], p. 138)
Monitoring activity allowed participants to become aware of their activity levels [Citation35, Citation37], develop an understanding of their achievements [Citation35] and pay attention to how their COPD symptoms affected their daily activities [Citation36].
It’s just the way I live. I’ve not done anything different to what I normally do… made me realize how much I was doing, or how little I was doing but I wouldn’t say it increased what I put into it. (Patient [Citation15]; 37, p. 12–13)
One study used a smartwatch to collect objective physical activity data which did not provide feedback to participants [Citation46]. Following the intervention, participants stated they wanted an app and device to provide feedback to them on their activity, heart rate and how better to manage their COPD, rather than a passive monitoring device [Citation46]. Another study attempted to blind participants to their activity levels with a sealed pedometer, however, it became apparent that some participants were accessing their step counts through the Fitbit app installed on the phone required for sending activity data to the researchers [Citation37].
Participants expressed that they wanted an app and a device that could provide more feedback. This feedback would include information about themselves in terms of their heart rate, coughing data, and oxygen saturation. [Citation46, p. 5].
Participants in one study suggested the personalized feedback on activity levels in relation to their goals could be improved by having more variety of messages, sending messages less frequently and making messages more personalized [Citation45]. It was not clear from this study whether the personalized feedback participants referred to was feedback from the wearable device, smartphone app and/or healthcare practitioner.
Only 9% (n = 3) of the patients were not satisfied with the sessions; however, the feedback messages could be improved according to 32% (n = 19) of the patients. Suggestions for improvement of the feedback messages were: more variation (n = 9), send feedback less frequently (n = 6), and to make them more personalized (n = 6). [Citation45, p.13].
Four studies highlighted participants’ frustrations when they perceived that the technology did not accurately monitor or record their activities [Citation35–37, Citation42].
My cycling activities were not well captured by the step counter. (Patient 25, low actual usage, medium contact time; [Citation42], Appendix 8, p. 1)
But, I have the latest Fitbit and it really is quite inaccurate. If you are aware, I drive a motorcycle, if I go on the bike for half an hour it says I’ve climbed like 50 flights of stairs. It misses things like, stairs, my office, where I am sitting right now I am up and down the stairs all day. I would estimate I am up and down the stairs 8–10 times and it typically shows 4–5. And sleep, they try their best to give you your sleep, and that is something I’m really interested in, I’ll give you an example, they disregard periods that could be sleep. If you sit still for 2 h enough it might say you were napping. If I wake up from sleep after 45 min after a disturbance, the next day when I look at my sleep, it threw away that 45 min. (P2; [Citation36], p.8)
Another study found that the monitoring activity was a stressor for some with participants getting annoyed or obsessed with constantly looking at the data or quantifying their activity [Citation35].
I took it off over the Easter holidays. I was wearing it and got annoyed with it because I glanced at it four times a day – it was like being on Facebook. (Dana; [Citation35], p. 1084).
Five studies reported participants wanted to continue using the monitoring technology after the study had finished indicating it would be useful as a long-term tool to monitor and motivate participants to maintain or improve physical activity [Citation35, Citation37, Citation41–43].
It would never have entered my head to go and buy something to improve my condition, never, erm but now I’ve got another Fitbit waiting for me when I go home. (Patient 03; [Citation37], p. 14–15)
I want to go and buy one. I probably will today; go and buy one. Because it must be kept up, right? Also, I need “the whip” (…) so it is about going to the pharmacy and then it will be attached from tomorrow. (Eileen; [Citation35], p. 1083)
The majority of participants planned on continuing to engage in exercise/PA [physical activity] with specific plans including continuing to set goals and use the pedometer or join an exercise class. Participants in both groups were generally quite confident they would continue as the benefits achieved served as motivation. [Citation43, p. 17]
Furthermore, Wu et al. [Citation36] found participants were interested in a device that could monitor symptoms of COPD (e.g. oxygen saturation, heart rate, blood pressure, activity, sleep and coughing) to help them to manage their health and feel safer engaging in activity.
Participants described that the technology would be able to help them make connections between how they are feeling and what their body is doing. People struggled with understanding the relationship of their condition and different triggers to their heart rate and blood pressure. They would put off going to the doctor or starting a treatment plan because they were unable to recognize early symptoms. Real-time monitoring could confirm that there was a need to see a healthcare professional and would be encouragement to get early treatment. It could allow people to better understand their symptoms so they would feel safer engaging in activities. [Citation36, p. 5]
Participants in one study particularly liked the healthcare professional reviewing and monitoring their activity data and discussing progress via the online intervention messaging system [Citation41].
It’s more than just writing it down… reporting…to somebody else is very important… because it meant that you knew someone was monitoring what you were doing. It kept you on your toes. When you have someone ringing saying “How were you going?” you sort of feel that you should be saying “Oh, I will try and do so much more”. (Participant 2; [Citation41], p. 376)
Theme 2: Supporting motivation to be active
Participants in most studies reported they found using the technology motivational [Citation35, Citation37–43, Citation45]. The technology encouraged participants to do more activity by allowing participants to track their activity and receive feedback [Citation35, Citation37–39, Citation41]. Some studies also found the goal setting elements motivating [Citation35, Citation40].
When I started the program… I’d hurt my knee… to look back over three to four weeks and find that “Oh, I’m a lot better than I was”… it just showed you how you’ve progressed and I think that’s important because sometimes you just get bogged down in the mire of not being able to do anything. (Participant 2; [Citation41], p. 376)
Wearing the pedometer was a high motivator. (Subject 02; [Citation40], p. 11)
Participants in some studies found having someone else monitoring or “watching” their physical activity levels remotely (such as a healthcare professional or researcher) externally motivated them to be more active [Citation36, Citation41, Citation42].
If you knew someone was watching you from a distance, even if it was once a fortnight, they would look and say or send you emails and say “What happened?” (Participant 10; [Citation41], p. 377)
The feeling of being monitored motivated me to be more active. (Patient 20, high actual usage score, medium contact time; [Citation42], Appendix 8, p. 2)
However, some participants also highlighted potentially negative health consequences of pushing boundaries of physical activity not taking their COPD into account or paying attention to their own body without support from a healthcare professional [Citation35].
In contrast, the intervention in Loeckx et al., smartphone-based physical activity tele-coaching, was not motivating to increase physical activity [Citation42] and technological issues were demotivating [Citation45].
I wouldn’t use the intervention again. It did not motivate me to be more active. (Patient 14, low actual usage score, high contact time; [Citation42], Appendix 8, p. 2)
One study also reported some participants found the technology “oppressive and consuming” [Citation35].
I have also felt that I had a few days in which I thought: “no, I am fed up with all that exercise. I do not want anything to do with it anymore”, because it was all the time that you had to focus on it. (Sophie; [Citation35], p. 1084)
Another study highlighted the supportive and motivating role of patients achieving goals together with their family [Citation42].
Even my wife bought a step counter so we could reach the goal together. (Patient 85, low actual usage, medium contact time; [Citation42], Appendix 8, p. 2)
Theme 3: Acceptability of the device
Six studies reported participants liked to use the monitoring technology [Citation36, Citation37, Citation41, Citation43–45].
I was increasing my walking; demonstrably it had been getting better and better… I love using the pedometer. (Participant 12; [Citation41], p. 376)
However, others found that some participants were not satisfied or did not like the device [Citation38, Citation45]. It was not always possible to discern from the studies exactly what participants’ concerns were about the technology. For example, in Benzo et al. [Citation38] it was not possible to identify the nature of this participant’s complaint (above) about the “armbands” and Garmin.
Is there anything we could do differently or that we need to change? “Can’t think of anything. My main complaint is about the armbands and the Garmin”. ([Citation38], p. 137)
Some participants in one study, who withdrew participation, seemed to find using monitoring technology overwhelming and daunting [Citation37]. Bentley et al. [Citation37] also found some participants had previously thought the monitoring technology was not relevant to them, and instead more suited to athletes, people without severe disease, more technologically knowledgeable and younger.
I wouldn’t have known about that Fitbit cos I weren’t interested in things like that… I never took no notice. I always thought people did it when they went in gym, you know like they bought a Fitbit just to cycle and things like that. (Patient 29; [Citation37], p. 14)
Additionally, to increase engagement with the technology, Bentley et al. [Citation37] highlighted some participants would have preferred to use their own smartphones with the intervention app installed rather than carrying and charging extra equipment. Further, some participants were worried about losing or damaging the device they were responsible for [Citation37].
Theme 4: Experiencing technical issues with the device
Five studies reported most participants found the monitoring technology easy to use [Citation35, Citation37, Citation39, Citation42, Citation44]. However, other studies showed that some participants found the technology difficult to use, reporting technical issues and issues with synchronizing data [Citation36, Citation37, Citation41, Citation42, Citation45, Citation46].
They weren’t getting no data through and I said well I don’t know whether Fitbit what’s not charging or phone what’s not charging. (Patient 25; [Citation37], p. 13]
However, Bentley et al. [Citation37] found participants rarely spoke to the healthcare professionals or researchers when they were experiencing issues. When participants did talk to the healthcare professionals, they found the professional did not know much about the technology or study.
They didn’t know how it worked. They didn’t, you know because I did ask at the beginning I was a bit flummoxed with it all erm and I did ask the physio that was there then and she, she had a look but she couldn’t tell me, but I figured it out myself in the end. (Patient 6; [Citation37], p. 14)
In two studies, technical issues were reported to be reasons for withdrawing or not participating in the study [Citation37, Citation46]. In the study where the technology was not being used as part of an intervention, participants gave up their own personal devices due to technical issues and inaccurate data [Citation36].
One study reported participants found the app connecting with the device slow and time consuming [Citation42].
The smartphone was often slow. I often needed to wait 10 to 15 minutes before I could send my steps in the evening. (Patient 119, low actual usage score, medium contact time; [Citation42], Appendix 8, p. 1)
One study highlighted participants’ prior experience, knowledge and understanding of digital technologies may have influenced their capability to take part in the intervention [Citation37]. Participants with less experience of using technology were more likely to encounter difficulties [Citation37]. Additionally, Wu et al. [Citation36] suggested “mastery of technology” by COPD patients may influence “the use and uptake of wearables and self-management apps” (p. 7).
Theme 5: Setting appropriate and achievable goals for their health condition
Setting achievable goals so they were not “too high” or put “pressure” on patients was mentioned in three studies [Citation35, Citation37, Citation42].
The goal was too high at the end of study. I felt under pressure. (Patient 63, high actual usage, high contact time; [Citation42], Appendix 8, p. 2)
One study identified the monitoring technology as a “personal pacer” for participants as a basis for “setting goals and changing habits” [Citation35].
Prior to this I was employed (…) we could sign up to the pedometer and report on the screen once a month how much we had walked. So I consider the pedometer a “pacer”. (Sophie; [Citation35], p. 1083)
Setting or updating goals was also something patients spoke to their physiotherapist about to ensure it was appropriate and fit with their health condition [Citation35]. Moreover, patients rarely updated their goals because the physiotherapists did not explicitly tell them to increase their goals and they wanted to keep their goals achievable [Citation37].
Well, I also began right away and attached it. But I knew that I would never reach 10,000 [steps] because I have Bechterew’s and therefore have trouble walking and have more than enough with trying to keep myself up. Then I spoke with my physiotherapist about it and he said 4000–5000 and no more than that. That is what I have been trying to keep. (Eileen; [Citation35], p. 1085)
Participants in one study highlighted the device did not take their health condition into account and would not allow goals to be adjusted immediately if patients experienced an exacerbation [Citation42]. Also, the monitoring device or intervention did not provide positive reinforcement for doing activity on days where it is more difficult [Citation35].
Theme 6: Integrating the device into their life and daily routine
Five studies highlighted that participants were able to incorporate the monitoring technology into their lives and daily routines [Citation35, Citation37, Citation42, Citation44], even during short intervention periods [e.g. 2-3 weeks; 44].
Difficulties integrating the technology into participants’ lives included not wanting to walk outside alone, experiencing the technology as a cause of stress, holidays, and having a reason to leave the house and use it [Citation35, Citation37].
I just want to get up and go. If I’m taking my dog out for a walk I’ve got enough trouble getting leads, making sure there’s bags on it and harness on dog and treats to make sure they come back without having to take [the phone]. (Patient 24; [Citation37], p. 13]
One study found as the device was “small and easy to carry”, participants forgot to attach the monitoring device or take the phones everywhere with them [Citation35]. Also, one study reported cases of participants losing the tracker with it catching on clothes and falling off [Citation37].
(…) in the beginning (…) I became annoyed with myself over forgetting it. But then I was able to turn it around so that it was okay. Because even if I forgot it, then I had still walked some (…) and if I had to go out and changed my clothes, and forgot to shift it or didn’t have a pocket so you couldn’t bring it. Well, that was frustrating but after I learned to let go of the numbers and just pulled it in another day if I had not walked that day – then it became alright. [Eileen; 35,p.1085]
Two studies reported participants found the device uncomfortable [Citation37, Citation44] causing itchiness or a rash [Citation37].
It’s been a bit uncomfortable, because it’s been hot, you know, and I couldn’t put any thin trousers on because I’m wearing it, but it’s been alright, yeah. Maybe a wrist thing would have been better for me. (Female, Feedback 029; [Citation44], p. 8)
Aesthetics and design were important to participants in two studies [Citation36, Citation46]. Participants wanted a more stylish, smaller and less bulky smartwatch [Citation46]. Design was also important, so it did not “stick out” as participants did not want to be able to be identified as having a “medical condition requiring a monitoring device” ([Citation36], p. 8).
Theme 7: Perceived physical and psychological benefits of using the device
Participants in seven studies reported physical and psychological benefits from using the monitoring technology. [Citation35, Citation37, Citation39, Citation41–43, Citation45].
I was increasing my walking; demonstrably it had been getting better and better… I love using the pedometer. (Participant 12; [Citation41], p. 376)
(ActivOnline) and the medication has really helped and that improves my outlook on life… I could see that I was having less “down” days… so (ActivOnline) gave you perspective. (Participant 11; [Citation41], p. 376)
Even though three studies did not find an overall significant or consistent increase in physical activity levels monitored by the technology, participants still reported feeling like it had a positive impact on their physical activity levels [Citation37, Citation41, Citation42].
Patients had varied levels of fitness prior to surgery but overall, almost all reported benefit from using the app. ([Citation39], p. 6)
However, one study found some participants stopped using the technology because they did not think it was beneficial anymore and had reached an appropriate activity level [Citation45].
Discussion
This literature review aimed to synthesize the qualitative literature on experiences of using technology for monitoring physical activity among people with COPD. Accordingly, seven themes were developed during the synthesis of the 12 included studies: (1) Monitoring and keeping track of their activity and health, (2) Supporting motivation to be active, (3) Acceptability of the device, (4) Experiencing technical issues with the device, (5) Setting appropriate and achievable goals for their health condition, (6) Integrating the device into their life and daily routine, and (7) Perceived physical and psychological benefits of using the device.
Overall, people with COPD enjoyed using the technology and found monitoring and keeping track of their activity easy and useful to increase their physical activity levels. This review also found negative experiences of using the monitoring technology among some participants in the studies, such as frustrations with inaccurate monitoring, concerns about being obsessed or stressed with the monitor, the technology being time consuming and experiencing technical issues (i.e. issues with synchronizing data and the app being slow).
Although participants perceived the monitors to have in inaccuracies with monitoring and some studies did not report significant or consistent increases in objectively monitored physical activity, qualitative feedback highlighted participants enjoyed using the activity monitors and felt it had a positive impact on their physical and mental health and wellbeing. Feedback, self-monitoring and setting appropriate goals are important aspects for behavior change and frequently used in interventions to increase physical activity in people with COPD [Citation7, Citation20, Citation47–50]. In support, this review found observing progress through charts, graphs and receiving feedback was motivational to people with COPD and allowed them to become aware of their activity levels. Participants’ feedback in studies where they were blinded to their activity levels notably reported some dissatisfaction and did not want a passive monitoring device. Instead, participants wanted information on their activity and heart rate to help manage their COPD. Setting appropriate and achievable goals was important for people with COPD. However, some participants felt the device, or associated app, did not take their health condition into account or allowed goals to be adjusted automatically if they were experiencing an exacerbation.
Strengths and limitations
To our knowledge, this is the first literature review to synthesize the qualitative literature on experiences of people with COPD using technology for monitoring physical activity. Searches were conducted in seven large academic databases with a comprehensive search strategy. However, it is possible other relevant published research may not have been included in this review due to language restrictions in the search strategy. Other unpublished literature in this area may also be valuable to further understanding experiences of using technology to monitor physical activity.
Another strength is this review followed guidance from the Joanna Briggs Institute manual for conducting scoping reviews [Citation27], alongside the Enhanced Transparency of Reporting the Synthesis of Qualitative Research framework [Citation29] and utilized the PRISMA 2020 flow diagram [Citation34]. Additionally, thematic synthesis was used, similar to other qualitative reviews with people with COPD [Citation20, Citation51–53]. However, the studies included in this review had varied designs and methodological approaches to qualitative analysis. The reporting of qualitative methodologies within studies, including data collection and analysis techniques, were often not reported in detail. Also, the credibility, dependability, transferability, and confirmability of some qualitative findings may have been limited due to the interpretation of the authors and lack of supporting qualitative data reported in the studies, such as including participant quotations. It is possible some studies were biased toward reporting mainly positive aspects of the intervention and technology. Additionally, qualitative analysis techniques used to understand and make sense of the data are seldom reported. Further high-quality research should be conducted with people with COPD to explore experiences of using physical activity monitoring technology. It is recommended future qualitative studies follow the Consolidated Criteria for Reporting Qualitative Research to allow critical appraisal and interpretation [Citation54].
Research included in this review was conducted prior to the COVID-19 global pandemic. During remote delivery of healthcare, the benefits monitoring technology can have to support patients with COPD is uncertain [Citation55]. Further research is needed to determine the impact of the pandemic on technological skills and experience among people with COPD and whether pulmonary rehabilitation centers have increased their use of technology to remotely monitor patients’ health or progress on exercise training programmes.
Implications for future research and practice
There is limited research exploring views and experiences of how people with COPD use and integrate technology into their lives if they have purchased or received a monitor outside of a research project. All but one of the included studies involved giving participants activity monitors as part of the intervention. Therefore, there may be discrepancies in experiences between studies, especially if there were more usability or technical issues with one technology compared to others.
It is possible that successful adoption of technology among people with COPD depends on the individual’s needs, preferences, intentions and motivations to use the device or associated app [Citation56]. Practitioners and researchers should be aware of altruistic motivations for taking part in research and possibly self-interest in technology and/or physical activity [Citation57]. Additional in-depth qualitative research is needed to further understand how incorporating technology for monitoring physical activity affects the lives of people with COPD.
Some interventions also involved participants needing to manually enter their daily step counts into an app or website after looking at their pedometer at the end of each day. This added process, compared to other interventions which sync automatically, may add another layer of frustration engaging with the intervention, or conversely increased monitoring and awareness of their physical activity levels having to pay attention and make a record of it each day. Over time, people may become more passive with their monitoring, not looking at their steps as often as they become habituated or used to their daily/weekly physical activity routine [Citation58]. Therefore, high quality research is essential to understand the experiences of people with COPD in integrating technology for monitoring physical activity into their everyday lives. Also, further in-depth qualitative research is needed to identify the experiences that are a product of a) specific device/app characteristics, b) the monitoring or wear requirements from participants within research studies, c) the type of data collected (e.g. behavioral, physiological, etc.), d) the extent of sharing/collaborative use of the data and e) duration of device use and if they become obsolescent. Wearables have the potential to increase levels of physical activity, however, we need to understand more about patients’ experiences of integrating these devices into their lives. Addressing any issues with, and success of, integrating technology into the lives of people with COPD can facilitate the development and evaluation of monitoring physical activity.
This review found in some studies, healthcare practitioners (e.g. physiotherapists) supported patients with their activity goals to ensure it was appropriate and fit with their health condition. However, further details would be useful on the support provision from healthcare practitioners to understand how practitioners can support patients with using technology to maintain or increase activity levels in other contexts, such as in pulmonary rehabilitation programmes. Based on the available evidence, further research should consider interventions to promote aiding healthcare practitioners to support people with COPD to engage with technology to monitor their physical activity. Further research is also needed to understand how healthcare practitioners could suitably support patients to adjust their goals appropriately depending on how they feel, including if they are experiencing an exacerbation. Robust, co-created guidelines are needed for healthcare practitioners to implement wearable technology in practice for people with COPD [Citation14, Citation37]. Optimizing opportunities for patients to monitor their activity, set appropriate physical activity goals and recognize improvements or maintenance on physical activity levels with COPD could enable them to take control and better self-manage their health condition.
This review furthers our understanding of people with COPD using technology for monitoring physical activity and provides evidence for researchers, healthcare professionals and technology developers of their experience. This review provides insight for healthcare practitioners to consider supporting patients to increase physical activity levels through using technology to monitor activity levels outside clinical settings or during remote pulmonary rehabilitation courses. Researchers can use the knowledge gained from this review to develop effective health interventions utilizing monitoring technology to increase or maintain physical activity levels in people with COPD. Furthermore, developers of monitoring technology may wish to embed functions to tailor monitoring and automatic goal setting to be appropriate to people with COPD or other restricting chronic health conditions.
Conclusion
This review increases our understanding of experiences of people with COPD using technology for monitoring physical activity. Despite the fact that some studies found people with COPD experienced frustrations with technical issues and highlighted some concerns about participants responses to data from the device, many studies found participants embraced the technology and experienced important benefits to their physical and mental health and wellbeing. Further high-quality research is needed to understand the experiences of people with COPD using different types and different aspects of technology to monitor physical activity in everyday life. Additional insight into monitoring technology will be invaluable to the development of robust, co-created guidelines on how healthcare practitioners can support patients to increase physical activity levels and use monitoring technology. Supporting people with COPD to monitor their physical activity could enable them to better self-manage their health condition.
Authors’ contributions
LW drafted the review protocol with support from coauthors (LS, CP, GW and CC). LW conducted the searches, screening and analysis. Coauthors (LS, CP, GW and CC) contributed to the development of the final themes. LW wrote and finalized the manuscript with substantial contributions to the final manuscript from coauthors (LS, CP, GW and CC). All authors reviewed the manuscript.
Supplemental Material
Download Zip (1.2 MB)Data availability statement
The authors agree to make their data available upon reasonable request.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- World Health Organization. The top 10 causes of death fact sheet 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. 2020.
- Welte T, Vogelmeier C, Papi A. COPD: early diagnosis and treatment to slow disease progression. Int J Clin Pract. 2015;69(3):336–349. []. 2015 /03/01DOI:10.1111/ijcp.12522
- Spruit MA, Singh SJ, Garvey C, ATS/ERS Task Force on Pulmonary Rehabilitation, et al. An official american thoracic society/european respiratory society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–64. DOI:10.1164/rccm.201309-1634ST
- McCarthy B, Casey D, Devane D, Cochrane Airways Group, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2015;2 DOI:10.1002/14651858.CD003793.pub3
- Egan C, Deering BM, Blake C, et al. Short term and long term effects of pulmonary rehabilitation on physical activity in COPD. Respir Med. 2012;106(12):1671–1679. DOI:10.1016/j.rmed.2012.08.016
- Kohlbrenner D, Sievi NA, Senn O, et al. Long-term effects of Pedometer-based physical activity coaching in severe COPD: a randomized controlled trial. Int J Chron Obstruct Pulmon Dis. 2020;15:2837–2846. DOI:10.2147/COPD.S279293
- Evenson KR, Goto MM, Furberg RD. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int J Behav Nutr Phys Act. 2015;12(1):159. DOI:10.1186/s12966-015-0314-1
- Fuller D, Colwell E, Low J, et al. Reliability and validity of commercially available wearable devices for measuring steps, energy expenditure, and heart rate: systematic review. JMIR Mhealth Uhealth. 2020;8(9):e18694. DOI:10.2196/18694
- Straiton N, Alharbi M, Bauman A, et al. The validity and reliability of consumer-grade activity trackers in older, community-dwelling adults: a systematic review. Maturitas. 2018;112:85–93. DOI:10.1016/j.maturitas.2018.03.016
- Van Remoortel H, Giavedoni S, Raste Y, PROactive consortium, et al. Validity of activity monitors in health and chronic disease: a systematic review. Int J Behav Nutr Phys Act. 2012;9(1):84. DOI:10.1186/1479-5868-9-84
- Shin G, Feng Y, Jarrahi MH, et al. Beyond novelty effect: a mixed-methods exploration into the motivation for long-term activity tracker use. JAMIA Open. 2019;2(1):62–72. DOI:10.1093/jamiaopen/ooy048
- Peng W, Li L, Kononova A, et al. Habit formation in wearable activity tracker use among older adults: qualitative study. JMIR Mhealth Uhealth. 2021;9(1):e22488. DOI:10.2196/22488
- Pericleous P, van Staa TP. The use of wearable technology to monitor physical activity in patients with COPD: a literature review. Int J Chron Obstruct Pulmon Dis. 2019;14:1317–1322. DOI:10.2147/COPD.S193037
- Mantoani LC, Rubio N, McKinstry B, et al. Interventions to modify physical activity in patients with COPD: a systematic review. Eur Respir J. 2016;48(1):69–81. DOI:10.1183/13993003.01744-2015
- Armstrong M, Winnard A, Chynkiamis N, et al. Use of pedometers as a tool to promote daily physical activity levels in patients with COPD: a systematic review and Meta-analysis. Eur Respir Rev. 2019;28(154):190039. DOI:10.1183/16000617.0039-2019
- Qiu S, Cai X, Wang X, et al. Using step counters to promote physical activity and exercise capacity in patients with chronic obstructive pulmonary disease: a Meta-analysis. Ther Adv Respir Dis. 2018;12:175346661878738. DOI:10.1177/1753466618787386
- Kawagoshi A, Kiyokawa N, Sugawara K, et al. Effects of low-intensity exercise and home-based pulmonary rehabilitation with pedometer feedback on physical activity in elderly patients with chronic obstructive pulmonary disease. Respir Med. 2015;109(3):364–371. DOI:10.1016/j.rmed.2015.01.008
- Mendoza L, Horta P, Espinoza J, et al. Pedometers to enhance physical activity in COPD: a randomised controlled trial. Eur Respir J. 2015;45(2):347–354. DOI:10.1183/09031936.00084514
- Robinson H, Williams V, Curtis F, et al. Facilitators and barriers to physical activity following pulmonary rehabilitation in COPD: a systematic review of qualitative studies. Prim Care Respir Med. 2018;28(1):1–12.
- Hendriks C, Deenstra D, Elfferich M, et al. Experience with activity monitors of patients with COPD, sarcoidosis and pulmonary fibrosis in The Netherlands Psychol Behav Sci Int J. 2019;12(4):1–6.
- Moy ML, Janney AW, Nguyen HQ, et al. Use of pedometer and internet-mediated walking program in patients with chronic obstructive pulmonary disease. JRRD. 2010;47(5):485–496. DOI:10.1682/JRRD.2009.07.0091
- Moy ML, Weston NA, Wilson EJ, et al. A pilot study of an internet walking program and pedometer in COPD. Respir Med. 2012;106(9):1342–1350. DOI:10.1016/j.rmed.2012.06.013
- Cruz J, Brooks D, Marques A. Impact of feedback on physical activity levels of individuals with chronic obstructive pulmonary disease during pulmonary rehabilitation: a feasibility study. Chron Respir Dis. 2014;11(4):191–198. DOI:10.1177/1479972314552280
- Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. Jama. 2007;298(19):2296–2304. DOI:10.1001/jama.298.19.2296
- Huniche L, Dinesen B, Nielsen C, et al. Patients’ use of self-monitored readings for managing everyday life with COPD: a qualitative study. Telemed J E Health. 2013;19(5):396–402. DOI:10.1089/tmj.2012.0135
- Peters M, Godfrey C, McInerney P, et al. Methodology for JBI scoping reviews. In: Aromataris E, editor. The joanna briggs institute reviewers manual. Adelaide, South Australia: Joanna Briggs Institute; 2015. p. 1–24.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology. 2005;8(1):19–32. DOI:10.1080/1364557032000119616
- Tong A, Flemming K, McInnes E, et al. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12(1):181. DOI:10.1186/1471-2288-12-181
- Wilde LJ, Ward G, Sewell L, et al. Apps and wearables for monitoring physical activity and sedentary behaviour: a qualitative systematic review protocol on barriers and facilitators. Digit Health. 2018;4:2055207618776454. DOI:10.1177/2055207618776454
- Halbert RJ, Natoli JL, Gano A, et al. Global burden of COPD: systematic review and Meta-analysis. Eur Respir J. 2006;28(3):523–532. DOI:10.1183/09031936.06.00124605
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews [journal article. ].BMC Med Res Methodol. 2008;8(45):45– 2288. DOI:10.1186/1471-2288-8-45
- Maher C, Hadfield M, Hutchings M, et al. Ensuring rigor in qualitative data analysis: a design research approach to coding combining NVivo with traditional material methods. Int J Qual Methods. 2018;17(1):160940691878636. DOI:10.1177/1609406918786362
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. DOI:10.1136/bmj.n71
- Wienroth M, Lund Holm Thomsen L, Høstgaard AM. Health technology identities and self. Patients’ appropriation of an assistive device for self-management of chronic illness . Sociol Health Illn. 2020;42(5):1077–1094. DOI:10.1111/1467-9566.13079
- Wu RC, Ginsburg S, Son T, et al. Using wearables and self-management apps in patients with COPD: a qualitative study. ERJ Open Res. 2019;5(3):00036-2019. DOI:10.1183/23120541.00036-2019
- Bentley CL, Powell L, Potter S, et al. The use of a smartphone app and an activity tracker to promote physical activity in the management of chronic obstructive pulmonary disease: Randomized controlled feasibility study. JMIR Mhealth Uhealth. 2020;8(6):e16203. DOI:10.2196/16203
- Benzo RP, Kramer KM, Hoult JP, et al. Development and feasibility of a home pulmonary rehabilitation program with health coaching. Respir Care. 2018;63(2):131–140. DOI:10.4187/respcare.05690
- Kadiri SB, Kerr AP, Oswald NK, et al. Fit 4 surgery, a bespoke app with biofeedback delivers rehabilitation at home before and after elective lung resection. J Cardiothorac Surg. 2019;14(1)DOI:10.1186/s13019-019-0951-6
- Larson JL, Webster KE. Feasibility and acceptability of active for life with COPD, an intervention to increase light physical activity in people with COPD. Heart Lung. 2020;49(2):132–138. DOI:10.1016/j.hrtlng.2020.01.002
- Liacos A, Burge AT, Cox NS, et al. Promoting physical activity using the internet: is it feasible and acceptable for patients with chronic obstructive pulmonary disease and bronchiectasis? J Aging Phys Act. 2018;26(3):372–381. DOI:10.1123/japa.2017-0123
- Loeckx M, Rabinovich RA, Demeyer H, et al. Smartphone-based physical activity telecoaching in chronic obstructive pulmonary disease: mixed-methods study on patient experiences and lessons for implementation. JMIR Mhealth Uhealth. 2018;6(12):e200. DOI:10.2196/mhealth.9774
- O’Neill B, O’Shea O, McDonough S, et al. Clinician-Facilitated physical activity intervention versus pulmonary rehabilitation for improving physical activity in COPD: a feasibility study. COPD. 2018;15(3):254–264. DOI:10.1080/15412555.2018.1486396
- Orme MW, Weedon AE, Saukko PM, et al. Findings of the chronic obstructive pulmonary Disease-Sitting and exacerbations trial (COPD-SEAT) in reducing sedentary time using wearable and mobile technologies with educational support: Randomized controlled feasibility trial. JMIR Mhealth Uhealth. 2018;6(4):e84. DOI:10.2196/mhealth.9398
- Verwey R, van der Weegen S, Spreeuwenberg M, et al. Process evaluation of physical activity counselling with and without the use of mobile technology: a mixed methods study. Int J Nurs Stud. 2016;53:3–16. DOI:10.1016/j.ijnurstu.2015.10.008
- Wu R, Liaqat D, de Lara E, et al. Feasibility of using a smartwatch to intensively monitor patients with chronic obstructive pulmonary disease: Prospective cohort study. JMIR Mhealth Uhealth. 2018;6(6):e10046. DOI:10.2196/10046
- de Blok BMJ, de Greef MHG, ten Hacken NHT, et al. The effects of a lifestyle physical activity counseling program with feedback of a pedometer during pulmonary rehabilitation in patients with COPD: a pilot study. Patient Educ Couns. 2006;61(1):48–55. DOI:10.1016/j.pec.2005.02.005
- Michie S, Abraham C, Whittington C, et al. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28(6):690–701. DOI:10.1037/a0016136
- Cindy Ng LW, Mackney J, Jenkins S, et al. Does exercise training change physical activity in people with COPD? A systematic review and meta-analysis. Chron Respir Dis. 2012;9(1):17–26. DOI:10.1177/1479972311430335
- Cheng SWM, Alison J, Dennis S, et al. A behaviour change intervention to reduce sedentary time in people with chronic obstructive pulmonary disease: protocol for a randomised controlled trial. J Physiother. 2017;63(3):182. DOI:10.1016/j.jphys.2017.04.001
- Disler RT, Green A, Luckett T, et al. Experience of advanced chronic obstructive pulmonary disease: Metasynthesis of qualitative research. J Pain Symptom Manage. 2014;48(6):1182–1199. DOI:10.1016/j.jpainsymman.2014.03.009
- O’Connell S, McCarthy VJC, Savage E. Self-management support preferences of people with asthma or chronic obstructive pulmonary disease: a systematic review and Meta-synthesis of qualitative studies. Chronic Illn. 2019;17(3).
- Ora L, Mannix J, Morgan L, et al. Chronic obstructive pulmonary disease and advance care planning: a synthesis of qualitative literature on patients’ experiences. Chronic Illn. 2021. DOI:10.1177/1742395321990109
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. DOI:10.1093/intqhc/mzm042
- Ilowite J, Lisker G, Greenberg H. Digital health technology and Telemedicine-Based hospital and home programs in pulmonary medicine during the COVID-19 pandemic. Am J Ther. 2021;28(2):e217–e223. DOI:10.1097/MJT.0000000000001342
- Ferreira JJ, Fernandes CI, Rammal HG, et al. Wearable technology and consumer interaction: a systematic review and research agenda. Compu Hum Behav. 2021;118:106710. DOI:10.1016/j.chb.2021.106710
- Olsen L, DePalma L, Evans JH. Self-Interested and altruistic motivations in volunteering for clinical trials: a more complex relationship. J Empir Res Hum Res Ethics. 2020;15(5):443–451. DOI:10.1177/1556264620914463
- Sporrel K, Nibbeling N, Wang S, et al. Unraveling mobile health exercise interventions for adults: Scoping review on the implementations and designs of persuasive strategies.JMIR Mhealth Uhealth. 2021;9(1):e16282. DOI:10.2196/16282