 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background: Hypoxemia is currently treated in hospital wards with oxygen, released continuously by “conventional” flow meters. A new type of hybrid flow meter allows to switch between on-demand and continuous mode. The aim of this observational study was to assess whether this new device reduces oxygen expenditure, is well accepted in a hospital setting and improves patient comfort during oxygen therapy. Methods: Oxygen was administered in hypoxemic patients with conventional or hybrid flow meters to maintain an oxygen saturation of ≥ 92% over a 12-week period. Every two weeks conventional and hybrid flow meters were switched. The overall oxygen delivery to the ward was continuously measured with a data logging device installed in the main oxygen pipeline and corrected for multiple confounding factors. Humidity measurements, for which a sensor placed in front of one of the nostrils, and patient questionnaires, were used to assess patient comfort during continuous and on-demand flow. Results: Overall oxygen delivery decreased by 39% when switching from continuous flow to on-demand therapy after correction for confounding factors. Continuous flows significantly decreased relative humidity more than equivalent on-demand settings and the latter tended to increase comfort. Conclusions: Hybrid flow meters cause a significant reduction in oxygen delivery in a hospital ward, which may lead to financial savings. Using the on-demand technology also lowers the dryness of the upper airways (and may increase patient comfort), while maintaining an adequate oxygenation.
Introduction
In a hospital setting, it is current practice to provide oxygen to patients through a nasal cannula, using an oxygen flow meter which delivers a continuous flow. This type of administration has two disadvantages: 1) the oxygen released during the expiratory phase of the respiratory cycle does not contribute to the oxygenation of the patient; 2) continuous flow of oxygen may cause dehydration of the upper airways, particularly at flows exceeding 4 L/min [Citation1]. Currently, cold water humidifiers are often used to improve comfort of continuous flow oxygen therapy. However, it remains a matter of debate whether humidifiers eventually improve patient comfort at oxygen flows below 4 L/min [Citation1–3] and may promote infections [Citation4].
Wada and Tanaka have shown previously that hypoxemia can be adequately corrected if oxygen is only supplied within the first quarter of the inspiration phase [Citation5]. This has led to the development of demand oxygen delivery systems (DODS), which were originally promoted to expand the autonomy of long-term oxygen therapy patients on portable oxygen and/or decrease the weight of portable oxygen sources [Citation6]. Theoretically, this type of technology can reduce the oxygen utilization by more than 80% compared to continuous flow by avoiding the release of oxygen during the expiratory phase and suppress the need for humidification [Citation7,Citation8].
Despite positive evaluations in an ambulatory setting [Citation9], DODS were not commonly used in hospital wards, because they lacked the ability to deliver oxygen both in on-demand and continuous mode. This made their use problematic in patients who may require continuous flow in a phase of worsening of their underlying disorder. Most DODS had only a continuous mode limited to 1 or 2 L/min. A new type of hybrid conserving flow meter has now been developed, that can be used in both the conventional continuous mode (at flow rates between 0.5 and 15 L/min) as in the “on-demand” mode (with settings equivalent to 1 to 5 L/min) ().
This study was primarily designed to determine the clinical and economic feasibility of on-demand delivery of oxygen with a hybrid flow meter in a hospital setting. More specifically, we wanted to compare the difference in oxygen utilization between periods during which oxygen was provided with conventional oxygen flow meters and with the hybrid system (primary outcome). The secondary aim was to investigate whether dryness of the nostrils, mouth and trachea could be attenuated using the on-demand mode. Other outcomes were feasibility, patient tolerance and adequacy of oxygenation.
Method
The present observational study consisted of two sub-studies: an oxygen utilization study conducted at the Department of Respiratory Medicine of Ghent University Hospital, a tertiary teaching hospital and an oxygen comfort study, which was performed at both the former institution and the Department of Respiratory Medicine of Máxima Medical Center Veldhoven, a regional hospital. The study was approved by the ethics committee of Ghent University Hospital (Belgian registration number B670201421371).
The oxygen utilization study was conducted at a ward of 25 beds. Patients admitted to the respiratory ward and in need of oxygen therapy were consecutively invited to participate and sign the informed consent. Reason for hospitalization, age and sex were registered. Patients, doctors, nurses, and physiotherapists of the ward were informed about the aim of the study. Moreover, medical personnel were trained in the correct use of the hybrid flow meter.
All oxygen flow meters on the ward were switched from the conventional (RTM3, Technologie Medical, France) to the new hybrid flow meter (O2COMFORT Flowmeter, Oxypoint, Belgium) and vice versa every two weeks for a total period of three months. Oxygenation of patients was monitored at least 4 times a day by pulse oximetry and flows were adjusted to reach the oxygen saturation (SpO2) prescribed by the physician in charge of the ward. During the hybrid weeks, patients requiring an oxygen flow above 5 L/min were placed in continuous mode. Moreover, the on-demand mode was increased or switched to continuous in patients who failed to maintain the prescribed peripheral SpO2.
Daily oxygen delivery to the ward was measured by installing a mass flow meter (Proline t-mass 65, Endress & Hauser) into the oxygen piping network to the ward and a data logging device (dataTaker DT80, dataTaker) for the duration of the study. Every 2 min, the flow obtained over a 2 min time interval (in L/min) and the cumulative value of consumed O2 were registered and stored.
To make a correct estimation of the saving effects of the hybrid vs. the conventional system, data obtained from the logging device were corrected for the following three confounding factors: 1) occupancy rate of the ward, as this may vary from week to week; 2) oxygen flow administered to the patients to maintain the prescribed oxygen saturation, as the overall need for oxygen of all hospitalized patients may fluctuate over time and depend on their disease severity profile; 3) the use of oxygen to aerosolize bronchodilating drugs, as medicinal oxygen is used at the respiratory ward of Ghent University Hospital to aerosolize bronchodilating drugs. These confounding factors were manually collected from the electronic patient records.
Oxygen consumption due to aerosolization was corrected by subtracting the former from the total amount of oxygen delivered. The amount of oxygen delivered during aerosolization was estimated by multiplying the number of sessions of aerosolization by 80 L, the mean amount of oxygen delivered during an aerosol session, since the standard oxygen flow during aerosol administration was 8 L/min and an average session lasted approximately 10 min.
During conventional periods, only continuous flows were noted, during hybrid periods the average flow rate consisted of both on-demand settings and, if applicable, continuous flow. Oxygen flow administered was normalized and corrected by the formula provided in appendix A. This formula uses total average utilization rate as indicated by the datalogger (L/min) during the conventional and hybrid weeks, as well as the average administered oxygen flow rates during these weeks. First, the difference in oxygen flows during the conventional and hybrid weeks was calculated and multiplied with the average delivery of oxygen in the hybrid flow meter weeks (datalogger), normalizing this factor. This was subsequently used to calculate the normalized saving rate.
The percentage of patients using the on-demand mode was recorded during the hybrid weeks. Using the electronic patient files, a distinction was made between the total number of on-demand and continuously prescribed and administered oxygen flow rates. Acceptability, defined by patient tolerance and adequacy of oxygenation, was calculated by dividing the number of patients using on demand therapy by the total number of patients on oxygen.
In the second sub-study, patient comfort was assessed by comparing the relative humidity over 30 min between on demand and continuous oxygen administration for the different flows in patients requiring oxygen supplementation and admitted to the Departments of Respiratory Medicine at both Máxima Medical Center and Ghent University Hospital. The relative humidity was measured directly in front of the nostril without the sensor making direct contact with the nostril itself (to avoid saturation of the sensor) and while sufficient space remained for the nasal cannula which was placed first. The continuous and on-demand settings were tested in a randomized order. The study consisted of the following 3 steps: (1) administration of oxygen via a nasal cannula for 30 min either by continuous or on demand oxygen flow; (2) measurement of SpO2 and relative humidity every 10 min using a pulse oximeter (NellcorTM OXIMAX-N65, Covidien, Colorado, USA) and a humidity sensor (SHT7x of Sensirion AG, Switzerland); and (3) assessment of comfort issues. For the latter, the patient was questioned about the therapy he preferred, while the experienced degree of the irritation was assessed using an adjusted version of the Wong-Baker pain scale varying between 1 (very uncomfortable) and 10 (very comfortable). Previous research comparing the settings of the hybrid and the conventional flow meters had demonstrated that on-demand settings between 1 and 5 largely corresponded with continuous flows between 1 and 5 L/min. Hence, paired comparisons of humidity, comfort and preference were performed at these respective settings and flows.
Statistical analysis
Differences in oxygen utilization data between continuous and on demand weeks were compared using a t-test. Differences in relative humidity levels between the two modes were assessed using a Wilcoxon signed rank test. All statistical analyses were performed with IBM SPSS statistics (version 22; IBM Business Analytics, Armonk, NY, USA). A P value of < 0.05 was considered statistically significant. The potential yearly financial benefits with the hybrid flow meter were based on the oxygen expenses of the preceding year. Prices for oxygen and flow meters were those of 2022.
Results
Oxygen utilization study
Population
139 patients signed to informed consent – none of the invited patients refused to participate – but only 132 (mean age ± SD: 60 ± 16 years and 81 male) patients with acute respiratory failure of different etiology participated in the oxygen delivery study (). Seven of the original 139 patients failed to participate because of unexpected improvement and early dismissal (4), acute deterioration and referral to the ICU (1), referral to the palliative care unit (1), and isolation because of multiresistant bacteria (1) before installation of the hybrid flow meter. Most patients were treated with oxygen for a few days because of a respiratory infection. During the hybrid weeks, a total of 267 flow rates were noted from which a total of 147 flow rates used the on-demand mode. This corresponds with 55% of the patients using the on-demand therapy during the hybrid weeks. The most used on-demand flow rate 2 L/min.
Table 1. Patient population.
Raw data
shows the data of the logger consisting of 60.302 data points obtained over the 12 weeks study period. Oxygen delivery during the hybrid weeks (black) was lower than during the conventional flow meter weeks (gray).
Figure 2. Oxygen delivery in L/min based on the logged flow data of oxygen delivery to the respiratory ward in 132 patients treated with oxygen over a period of 12 weeks. Each data point represents a flow obtained over a 2 min time interval. Black indicates hybrid, gray indicates conventional flow meter periods. The horizontal lines represent the average O2 utilization in the respective periods.
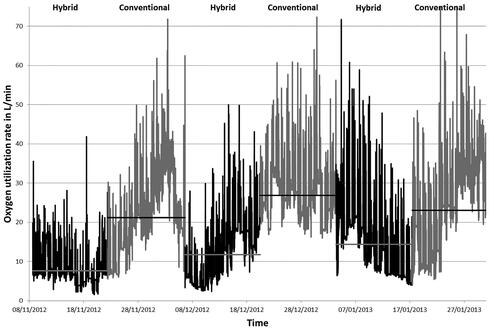
Average oxygen utilization decreased from 22 L/min during conventional periods to 10 L/min during the hybrid weeks, which corresponds with a significant reduction in oxygen consumption by 54% (p = 0.013).
Correction for confounding factors
Manual registration of the three confounding factors showed that the average number of patients per day during the different weeks was nearly constant, whereas the average oxygen flow rate prescribed and administered per patient was significantly lower during the hybrid weeks (p = 0.01) (). A total 1876 sessions of aerosolization were registered.
Table 2. Averaged oxygen consumption (L/min) of the ward measured by the datalogger and manually registered oxygen flow during each 6 consecutive periods.
For every period of the study, the average oxygen delivery as recorded by the DataTaker data was corrected for the utilization of oxygen for aerosolization. No correction was performed for the first hybrid period, as the investigators were unaware of the fact that oxygen was used for aerosolization instead of pressurized air at the start of the study and aerosolization data were lacking for that period (, first row).
After correction for these confounding factors, net reduction in oxygen utilization was 39% ( and ).
Figure 3. Mean oxygen delivery in L/min during the conventional (dark gray), the hybrid (light gray) flow meter periods and after normalization for occupancy, O2 prescription and administration, and aerosolization. The oxygen sparing effect by 54% based on the mass flow meter logged data is reduced to 39% after normalization.
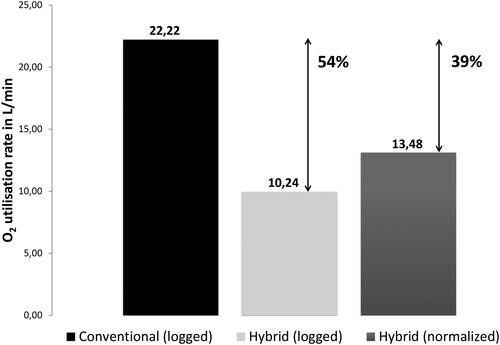
Table 3. Total and adjusted oxygen consumption (L/min) of the ward averaged over the 6 weeks period measured by the datalogger during the conventional and the hybrid weeks. Corrections for the hybrid weeks were made for bed occupancy, oxygen administration, and oxygen utilization in aerosol therapy.
Comfort study
A total of 30 patients took part to the study at the Ghent University Hospital and 27 patients at the Máxima Medical Center of Veldhoven. represents the averages of the relative humidity of patient receiving 1 to 4 L/min. A significant downward trend is seen in the relative humidity when increasing the continuous flow of oxygen (). Since humidity stabilized after the third measurement only, a large spread is seen in the boxplots (). The measured SpO2 in the comfort study also showed lowering of the SpO2 level by 1 to 2% ( and ).
Figure 4. Comparison between the relative humidity using continuous flow rates from 1 to 4 liters per minute and their equivalent on-demand flow settings 1 to 4. O = outlier 3rd quartile + 1.5 * interquartile range or 1st quartile -1.5 * interquartile range.
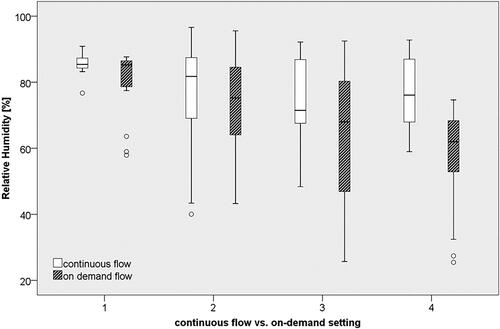
Figure 5. Comparison between the saturation levels using continuous flow rates from 1 to 4 liters per minute and their equivalent on-demand flow settings 1 to 4. O = outlier 3rd quartile +/- 1.5 * interquartile range or 1st quartile -1.5 * interquartile range; * = outlier 3rd quartile + 3 * interquartile range or 1st quartile - 3 * interquartile range.
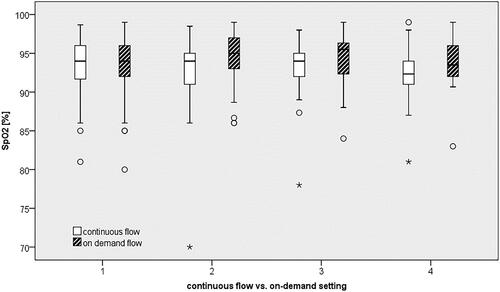
Table 4. Summary of average relative humidity (RH) between on-demand mode and continuous flow.
Table 5. Average saturation level between on-demand mode and continuous flow for different flow rates.
shows that the average score of the modified Wong-Baker pain scale, was statiscally significantly higher for continuous flow (p = 0.015 for the median over all oxygen flow rates). Whether this numerical difference reached clinical significance, is unclear, as the minimal clinically significant difference for dehydration has not been established so far. However, 30 patients indicated they preferred the on-demand therapy, 14 patients preferred a continuous flow, and 13 patients expressed no preference for either therapy. Patients who preferred the on-demand mode experienced less feelings of cold, burning, or dry air, less nasal irritation referring thereby to the back of the nose, and less dehydration. Some of them mentioned less crust formation or stated that they could breathe more freely. Those who preferred the continuous mode were disturbed by the puffing sound of the on-demand mode or thought that they might have more difficulties to get asleep with the on-demand mode.
Table 6. Summary of average scores of the modified Wong-Baker pain scale for the on-demand mode and continuous flow. A low average score indicates more comfortable therapy. For further details: see text.
Financial analysis
We also conducted an estimation of the financial savings of this reduction in oxygen utilization. Based on the yearly cost for medical oxygen on the respiratory ward which (taking the current price of oxygen into account) averaged ± €7.100 before the study, a yearly benefit of ± €2.800 may be expected. At our ward, such savings would require an investment in 25 hybrid flow meters (with an investment difference of 5.000 €, or a yearly additional cost of 500 €, compared to 25 conventional flow meters). As this yearly cost must be substracted from the yearly benefit, the net benefit is 2.300 €/year, which corresponds with a return on investment of less than 2 years.
Discussion
This study is the first to demonstrate that a new hybrid flow meter with a complete range of continuous flows and on-demand functionalities can be used to decrease oxygen utilization in hospital wards, while still reaching the prescribed degree of oxygenation. It convincingly indicates that a systematic use of hybrid flow meters reduces the overall administration of oxygen by as much as 39%. If the financial savings, the cost, and the depreciation of these flow meters are considered, a return on investment could be expected after less than 2 years.
In the present study, raw data were normalized to correct for occupancy rate of the ward, number of aerosol administrations and oxygen flow prescribed and administered to the patients. Indeed, a correct comparison could only be made between continuous and hybrid weeks after normalization. The missing aerosolization data for the first hybrid period could, however, have had a relevant impact on the average utilization rate during the first hybrid weeks, since during in the other two hybrid periods the registered oxygen volume used for aerosolization averaged 11%. Consequently, the reported total savings of 39% represent an underestimation of the real savings that might have been expected.
It was beyond the scope of this study to elucidate the mechanisms responsible for the observed decrease in oxygen consumption. There are reasons to believe that, in addition to the discontinuous oxygen flow directly administered to the patient, the observed reduction in oxygen consumption may be attributed to other mechanisms. Although the present study did not investigate this issue, oxygen is also wasted by the phenomenon of “open valves at a ward”, which occurs when patients leave their room for a walk or technical investigations, and the oxygen valves are not closed by the nurses. Automatic closure of oxygen valves with an on-demand system prevents such inappropriate losses of oxygen.
An issue that deserves attention is whether the use of the new hybrid flow meter may negatively affect oxygenation of more critical patients with more pronounced hypoxemia. This may increase the need to monitor oxygenation of patients more frequently, augmenting thereby the workload of the nursing personnel. This was not the case at our ward but might be the case when more critical patients are hospitalized.
During the oxygen delivery study, the on-demand mode of this device was well accepted by patients suffering from an acute respiratory illness with a use of 55%. No significant correlation could be identified between acceptance rate and patient profile. It was noted by the nursing personnel that some COPD patients using DODS for ambulatory oxygen administration did not tolerate the on-demand mode during exacerbations due to perception of oxygen deficiency. Important here is the educational task of the nursing personnel in reassuring the patient on the equivalence of the therapy with the enhanced comfort when using the on-demand mode.
The improved nasal hydration, reported with discontinuous oxygen flow, was translated into an increased patient preference for the on-demand mode, with 50% of the population preferring the on-demand mode. 24% of the patients preferred the continuous mode, mainly due to the sound being produced during the comfort mode, usually during the night. In this regard, the choice of nasal cannula is of key importance, as sound production between nasal cannula brands may vary to a great extent.
Until recently, on-demand oxygen valves have been mainly used in stable and ambulatory patients on long term oxygen therapy [Citation10] to increase patients’ autonomy of portable oxygen sources [Citation9,Citation11–15]. The current study extrapolates the large empiric knowledge about DODS and the previous positive evaluations in ambulatory settings [Citation9,Citation16–17] to the hospital setting where the presently investigated hybrid device could easily be used with a standard nasal cannula.
One of the limitations of the present study is that the study was performed in the respiratory ward of a tertiary hospital. Savings might be even greater in regional hospitals where the on-demand mode of the device may be used in more than 55% of patients treated with oxygen in our study, since respiratory patients with a lower degree of disease severity may reside there. Furthermore, our comfort study is limited by the relatively short-term use of the on-demand mode since the nasal dehydration and saturation equivalency of patients may be different when patients are treated for longer periods of time. The high scatter of the data after 30 min suggests that the assessment of the relative humidity and SpO2 over a longer time interval could further validate the trends observed in the present study. It remains that significant differences can be seen between the continuous and on-demand mode.
In conclusion, the present study demonstrates that implementation of oxygen conserving devices in a tertiary hospital setting is feasible, tended to increase patient comfort and may lead to financial savings while maintaining optimal patient oxygenation.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
| Abbreviation List: | ||
| DODS | = | demand oxygen delivery systems |
| SpO2 | = | peripheral capillary oxygen saturation |
| ICU | = | intensive care unit |
| L/min | = | liters per minute |
Acknowledgments
The authors thank the nurses and physiotherapists of the respiratory ward of the Department of Respiratory Medicine of Ghent University Hospital and Máxima Medical Center for their participation in this project. The authors also thank the company Oxypoint NV, Antwerp, Belgium for providing the oxygen flowmeters during the study.
Declaration of interest
The authors report no conflicts of interest in this work.
References
- Campbell EJ, Baker MD, Crites-Silver P. Subjective effects of humidification of oxygen for delivery by nasal cannula. A prospective study. Chest. 1988;93(2):289–293.
- Andres D, Thurston N, Brant R, et al. Randomized double-blind trial of the effects of humidified compared with nonhumidified low flow oxygen therapy on the symptoms of patients. Can Respir J. 1997;4(2):76–78. DOI:10.1155/1997/296763
- O’Driscoll BR, Howard LS, Davison AG. BTS guideline for emergency oxygen use in adult patients. Thorax. 2008;63(Supplement 6):vi1–68. DOI:10.1136/thx.2008.102947
- Jadhav S, Sahasrabudhe T, Kalley V, et al. The microbial colonization profile of respiratory devices and the significance of the role of disinfection: a blinded study. J Clin Diagn Res. 2013;7(6):1021–1026.
- Wada S, Tanaka M, et al. Effective timing of oxygen inhalation for alveolar gas exchange:a simulation using a respiratory model. Am Soc Mech Eng Bioeng Div. 2001;40:401–402.
- Barker AF, Burgher LW, Plummer AL. Oxygen conserving methods for adults. Chest. 1994;105(1):248–252. DOI:10.1378/chest.105.1.248
- Floreani A, Kerby GR, Pingleton SK, et al. Evaluation of a demand-flow O2 delivery device. Chest. 1986;89:485S.
- Tiep B, Carter R. Oxygen conserving devices and methodologies. Chron Respir Dis. 2008;5(2):109–114. DOI:10.1177/1479972308090691
- Kerby GR, O’Donohue WJ, Romberger DJ, et al. Clinical efficacy and cost benefit of pulse flow oxygen in hospitalized patients. Chest. 1990;97(2):369–372. DOI:10.1378/chest.97.2.369
- Gloeckl R, Osadnik C, Bies L, et al. Comparison of continuous flow versus demand oxygen delivery systems in patients with COPD: a systematic review and meta-analysis. Respirology. 2019;24(4):329–337. DOI:10.1111/resp.13457
- Langenhof S, Fichter J. Comparison of two demand oxygen delivery devices for administration of oxygen in COPD. Chest. 2005;128(4):2082–2087. DOI:10.1378/chest.128.4.2082
- Garrod R, Bestall JC, Paul E, et al. Evaluation of pulsed dose oxygen delivery during exercise in patients with severe chronic obstructive pulmonary disease. Thorax. 1999;54(3):242–244. DOI:10.1136/thx.54.3.242
- Cuvelier A, Muir JF, Czernichow P, et al. Nocturnal efficiency and tolerance of a demand oxygen delivery system in COPD patients with nocturnal hypoxemia. Chest. 1999;116(1):22–29. DOI:10.1378/chest.116.1.22
- Chatburn RL, Lewarski JS, McCoy RW. Nocturnal oxygenation using a pulsed-dose oxygen-conserving device compared to continuous flow. Respir Care. 2006;51(3):252–256.
- Bower JS, Brook CJ, Zimmer K, et al. Performance of a demand oxygen saver system during rest, exercise, and sleep in hypoxemic patients. Chest. 1988;94(1):77–80. DOI:10.1378/chest.94.1.77
- Peter T, Bliss L L, Robert W, et al. Characteristics of demand oxygen delivery systems: maximum output and setting recommendations. Respir Care. 2004;49(2):160–165.
- Peter T, L Bliss L, Robert W, et al. A bench study comparison of demand oxygen delivery systems and continuous flow oxygen. Respir Care. 1999;44:925–931.
&
Appendix A
Formula and calculation of the Normalized Saving Rate when Tau,c > Tau,h
Tau, c: Total average utilization in conventional flowmeter weeksTap, c: Total average prescribed oxygen flow in conventional flowmeter weeksTau, h: Total average utilization in hybrid flowmeter weeksTap, h: Total prescribed oxygen flow in hybrid flowmeter weeks

