Abstract
Recently, health technology systems offering monitoring of the peripheral oxygen saturation level and automated oxygen administration (AOA) have emerged. AOA has been shown to reduce duration of hypoxemia and the length of hospital stay, but the patients’ perspective on AOA has not been investigated. This qualitative study, based on the interpretive description methodology, aimed to explore how patients hospitalized with exacerbation of chronic obstructive pulmonary disease (COPD) experience being treated with AOA. Eighteen patients treated with AOA were included in the study. Data was collected during admission or in the patients’ homes using semi-structured interviews focusing on patients’ experiences of AOA using the word “robot” as used by patients. The findings revealed two themes “adaptation of behavior to the robot” and “robots can make patients feel safe but not cared for” and six subthemes. Our findings illustrate how patients were willing to compromise their own therapy and thereby safety by avoiding behavior triggering AOA alarms and disturbing their fellow patients and the health care professionals. Adherence, defined as patients’ consistency in taking their medications as prescribed, becomes an important point of attention for health professionals when applying individualized robotic therapies such as AOA to patients with COPD. To support patients in the process of managing adherence to therapeutic technology, we propose a person-centered care approach that, through education and communication with the patients, generates an understanding of how they can self-manage AOA and its alarms without activating avoiding behavior that threatens their treatment and recovery.
Introduction
Dyspnea is the cardinal symptom of COPD and worsening of dyspnea is the main reason that patients with COPD are hospitalized (Citation1). Hypoxemia is common among patients hospitalized with exacerbation of COPD and the patients are, therefore, treated with supplemental oxygen (Citation1).
In hospital settings, oxygen flow is titrated by health professionals according to predefined algorithms depending on vital parameters and clinical observations (Citation2–4). Audits of oxygen supplementation in pre-hospital and hospital settings have documented wide guideline discordancy, with hypo- or hyper-oxygenation threatening patient safety and recovery (Citation4–10).
To prevent hypo- and hyper-oxygenation as a consequence of suboptimal oxygen treatment, automated oxygen administration (AOA) has been developed as a closed-loop system that titrates oxygen according to the patient’s peripheral oxygen saturation (SpO2) level (Citation10–13). Previous studies have documented that personalized therapy that automatically adjusts the oxygen flow according to the patient’s SpO2 level, increases time within the target saturation range and reduces severe hypoxemia, hyperoxemia and length of hospital stay compared to conventional oxygen therapy (Citation10, Citation12–16). In a clinical setting, AOA has been rated as equally appropriate to conventional therapy by nurses and physicians (Citation12). However, to improve the course of treatment and the subsequent benefits of AOA, management and tolerance of the technical device and thereby adherence to medication, defined as patients consistency in taking their prescribed medications, are essential (Citation17). A Danish study that investigated patients’ experience of long-term oxygen therapy in domestic settings identified six themes of importance to patients’ adherence to therapy: perceived lower work of breathing, reduced symptoms, improved quality of sleep, increased activities of daily living, feeling safe, and technology use (Citation18). However, our knowledge about hospitalized patients’ perspectives on conventional oxygen therapy is limited, and we have not identified any studies describing patients’ perspectives on AOA. This study, thus, aimed to explore how patients with COPD experienced being treated with AOA as part of the therapeutic management during their admission for exacerbation.
Methods
This study had a qualitative research design and was inspired by the methodology of interpretive description (ID) (Citation19, Citation20). The study was nested in the randomized controlled trial (RCT) entitled “Automated oxygen control with O2matic during admission with exacerbation in COPD” (ClinicalTrials.Gov: NCT 03661086). The in- and exclusion criteria of the RCT are given in below.
Table 1. Inclusion and exclusion criteria.
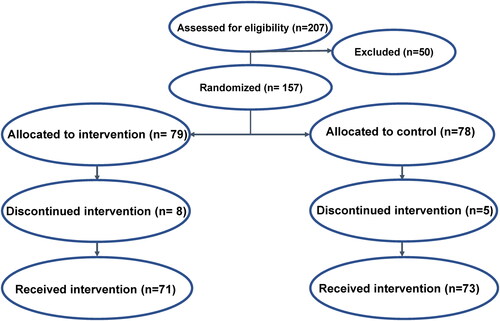
A total of 157 patients were randomized 1:1 to either AOA or conventual oxygen therapy. The trial was completed by 144 patients of whom 71 received the AOA intervention (flowchart below).
The flowchart illustrates the number of patients (n) assessed for eligibility, randomization, allocation and who received the full intervention
Functionalities of the assistive technological device for automated oxygen administration
AOA is a closed-loop system that monitors a patient’s SpO2 level and automatically titrates the oxygen flow accordingly and makes audio alarms when the saturation level is outside the defined range. The device is placed behind the headboard of the patient’s bed (see ), and the patient is connected to the device by a nasal cannula and a wired finger clip pulse oximeter.
The illustration is shared with permission from O2matic ApS
Participants
The study participants were recruited from three different hospitals and respiratory wards in the capital region of Denmark. Patients were invited to participate in interviews if they were included in the RCT and allocated to the intervention arm with AOA. The interviews were conducted when the patients had completed the intervention, including follow-up. The sampling strategy was convenience sampling, although the greatest possible variation in terms of sex, age, disease severity and which hospital they were admitted to was sought. The characteristics of the participants are shown in .
Table 2. Characteristics of the participants (n = 18).
Participants: Identification number; sex: F = female/M = male; age: age by 5-year intervals; FEV1%:pred forced expiratory volume by 1 s in percentage of expected value; sat/O2: percentage of peripheral oxygen saturation measured by the finger clip and oxygen flow and given in liters/min.
Data collection
Data were collected through individual semi-structured interviews. The interviews were conducted between November 2019 and November 2021. Fifteen interviews were conducted during the admission immediately after the end of the intervention, and three interviews in the patients’ homes up to seven days after the end of the intervention. After conducting 18 interviews, we were convinced that further data collection would be superfluous as our data were repeated in a recognizable and stable pattern (Citation21).
First, we conducted a pilot interview with an experienced patient with COPD. The patient had a history of several hospitalizations with exacerbation requiring supplemental oxygen therapy and had experience with the new therapeutic modality AOA. This pilot interview, in combination with the existing literature and our clinical experience, formed the basis for our interview topic guide. The topic guide consisted of open-ended questions, allowing the patients to bring up any thoughts they had about AOA. The AOA device was referred to as a “robot” as the staff at the respiratory ward usually used this term when communicating with patients about AOA. The topic guide allowed the interviewer to respond to and validate the participants’ answers by asking them to explain these as thoroughly as possible. The guide was reviewed and adjusted by all the authors according to substance and clinical relevance after 6 and 12 interviews (). The interviews were conducted by the first and second author of the present paper, recorded digitally, and subsequently transcribed verbatim by the first author. The interviews had a mean duration of 21 min (range: 5–52 min). The length of the interview transcript was 89 pages (font size 12, single-spaced).
Table 3. Interview topic guide.
Data analysis
The data analysis was thematic and inductive, searching for patients’ understanding of the clinical phenomenon of AOA. The analysis searched for understanding by illuminating characteristics, patterns, and structures through a concurrent and responsive process between data collection and data analysis. This constant comparative method was achieved by incorporating the authors’ knowledge into the project (Citation19, Citation20). In the first phase of the analysis, the obtained data were initially read, and pre-coded, preliminary categories were identified from them, adjustments were made to the interview guide, and the process was repeated after 6 and 12 interviews. In the second phase, the codes were reviewed to ensure that they captured the essence of the data; in the third phase, the final themes were defined and named; and in the last phase, the findings were reported.
Ethics
Informed written consent was obtained from all the participants before their inclusion in the study. The RCT study was approved by the Regional Committee on Health Research Ethics (H-17040114). No further approval was needed due to the study’s qualitative nature (http://www.nvk.dk). The participants’ anonymity and the confidentiality of the data to be obtained from them were ensured, and the study was approved by the Danish Data Protection Agency (number: p-2019-682).
Results
Our findings were captured in two themes and six subthemes (). The patients referred to the first few days of their hospitalization as unclear and “blurry,” and did not remember that they had received oxygen treatment through a robot. Despite this, the patients had a clear impression that the health professionals perceived the robot as a device that optimized therapy, without the patients being able to account for how it optimized.
Table 4. Themes and subthemes.
Adaptation of behavior to the robot
Due to the patients’ dependency on supplemental oxygen, they adapted their behaviors to the robot. The robot nudged specific forms of behaviors or actions; if these did not occur, it would respond with alarms of high intensity. This was problematic if the wardrooms were shared with one or up to three other patients. Triggering the robotic alarm was described as unpleasant and as something that should be avoided at all costs, sometimes even at the cost of one’s own therapy and thereby potentially safety.
It’s not a problem being treated by the robot. The problem is when you go to the loo. If you’re getting diuretics, then you need to go quite often. It just hangs there, screaming and yelling at the wall! You get stressed and confused because you don’t want to wake up the other people in the room in the middle of the night. You want to show some empathy, right? That really pisses me off! (Participant 18)
The patients also described how AOA liberated them from their dependency on the nurses, while at the same time restricting them through the limiting wires.
Rather compromise own therapy than being a nuisance
The patients expressed a sincere wish not to disturb the “sweet and busy nurses” or their fellow patients through unnecessary and avoidable robotic alarms. When the patients disconnected themselves from the robot (by taking off the finger clip) to eat, go to the toilet, or get dressed, an alarm would start after five minutes. The alarm would also go off if SpO2 dropped below a given range, like after a toilet visit, and then its intensity would increase with time until SpO2 was back within range. To avoid this scenario, the patients adjusted their activities of daily living by e.g. rushing through their normal routines in the toilet.
Whenever I was in the toilet, it was in my subconscious that I needed to return to the bed before the alarms went off. (Participant 14)
The patients reported that sometimes when the robot’s alarms went off, the nurses did not come to help or did not know how to stop the alarms. As a response to this lack of assistance, the patients silenced the robot by switching it to manual mode. However, this reduced the robot’s functionality to a standard flow device and therefore increased the risk of suboptimal oxygen therapy. This was often known to the patients, but they found themselves willing to make the tradeoff to stay on good terms with their fellow patients. In desperation, it was described how patients even switched off the robot.
… So then, it started acting all silly. Suddenly, it started blipping randomly. I said to my neighbor, ‘I can’t stop it!’ But, in the end, I had to get up and stop it! I had to stop it as we couldn’t sleep…. I didn’t want to disturb the other patients in my room or to be on bad terms with them. (Participant 4)
Although the auditive environment in the wards was described as problematic due to the pool of sounds emanating from many different technologies and “patient calls,” the patients still described it as severely problematic to indirectly be a source of noise, especially during the night.
Liberated from dependency on the nurses
Manual administered supplemental oxygen require the frequent presence of nurses to monitor the patient’s SpO2 level and, if necessary, subsequently adjust the oxygen flow. The patients mentioned how sweet and hardworking the nurses were and how they (the patients) did not want to be a burden to them. The robot was perceived by the patients as a device that removed a task from the nurses’ hands.
It was described how patients mistrusted nurse-administered oxygen therapy as they felt that they had to beg for what they considered a sufficient oxygen flow. On the other hand, however, patients said that the robot could not replace the nurses when it came to caring.
I believe the robot must be a big relief for the nurses. With the robot, the nurses don’t need to run in and out of my room to give me the right amount of oxygen. (Laughs) I mean, it must be difficult to give me the exact amount of oxygen I need. They run in and out of my room, turn it up and down, and then repeat the whole process shortly after. That’s why I’m saying it must feel like a relief to them to have the robot around. (Participant 17)
The patients described how the robot liberated them from their dependency on the nurses and empowered them as individuals. They no longer needed to be insecure if the nurses gave them the right oxygen flow, as the robot automatically provided them with it.
The robot gave me what I needed (oxygen), and I didn’t need to depend on anyone. (Participant 14)
However, it was still the nurses who operated the robot. It happened that patients turned off the “robot function” and switched to manual mode to get rid of the alarms, but it was also stated that patients had sparse knowledge of the robot’s functionalities and thus did not dare operate it, especially if they had had a negative experience with it when they did. Fortunately, no adverse events were reported in relation to manual adjustments/shutdowns made by the patients.
It’s not illegal to think for yourself. If I see that it provides me with 14 L of oxygen, then I know something’s wrong. You couldn’t imagine how quickly I got rid of it when that happened! It was like oxygen stormed into my nose, and it was painful, like hell! I took it off immediately. I was sitting alone behind a closed door and thought to myself, ‘This is stupid!’ Then I started coughing so I tried opening the door to get some help…. I didn’t know how to stop it. I didn’t dare touch it. (Participant 18)
The placement of the robot, behind the headboard of the bed, made it hard for patients to see the robot and engage in it. However, patients who were mobile often looked at the robot’s display as it made them feel safe to know that all the vital values were as they should be.
Tied by wires mentally and physically
The patients described how they felt restricted by the nasal cannula and especially by the finger clip pulse oximeter, as it had to be placed correctly on their fingers to provide reliable measurements. The equipment’s sensitivity made the robot therapy less flexible to patients’ normal activities, inducing them to adapt their sleep, meals, toilet visits, and resting positions to the “options” dictated by the robot.
… That thing over there (the robot), it’s been most unpleasant…. It’s been so tight on my fingers. I’ve tried to attach it to other fingers, but my fingers are so crooked, so it’s been difficult…. I tried to take it off, but then it started to talk behind me…. I put it back on again because it felt safer. (Participant 10)
To prevent the finger clip from dropping off, some patients asked the nurses to tape it onto their fingers. Another patient’s strategy was to lie completely still in bed, with the hand placed in a fixed position on top of the duvet. The finger clip was often kept in the optimal position for many hours, putting a slight and continuous pressure t on the finger to which it was attached, and by that potentially painful. In addition, the patients described how the length of the robot’s oxygen tube and wires constituted both a physical and a mental barrier for their activities as it made them dependent on nursing assistance to transfer to a chair, to go to the toilet, or to walk.
I must admit, the first day I got rid of it (the robot), I missed it in a somewhat awkward way. I missed looking up to see the state of things, such as if my saturation level was 90% or 85%. That way, I really missed it. It didn’t bother me too much, though, maybe only as little as if I squished my fingers, which could be painful. (Participant 1)
Despite the wire/tubing that tied the patients to the robot, the patients stated that the robot did not bother them and even expressed a feeling of emptiness if the finger clip was not in place. The patients perceived it as essential for their recovery to wear the finger clip, and it was described it as a form of mental dependency on the robot to frequently check it to ensure that the therapy was adequate.
Robots made the patients feel safe but not cared for
The patients who participated in this study spontaneously stated how the robot made them feel safe. Close monitoring and minimal use of oxygen were important to the patients but were not an alternative to the care given by the nurses.
It provided me with a feeling of safety but no care, and it didn’t greet me in the morning, as the nurses did. (Participant 9)
The patients described how they believed that the robot had reduced the intensity of their dyspnea, anxiety, and need for rescue inhalation as well as the risk of adverse events, by keeping the oxygen flow as low as possible as they believed it reduced their risk of generating a high level of carbon dioxide.
Pendulating between feelings of safety and lack of safety
The feeling of safety was to some extent generated through reassurance and control as the patients were able to self-monitor vital values and oxygen flows in combination with a bodily sensation of fluctuating flow changes in their nostrils.
The robot did help me. It didn’t take so much effort for me to breathe with it on; it was like the air was there automatically. Once in a while, I’d take a deep breath through my nose, but I’d rather not do that because it would make my nose feel icy, and then it could start bleeding. The alarm also didn’t bother me at all. I got used to it, and whenever it went off, I immediately felt it in my nose. I’d get a cold nose, and it would make me happy. (Laughs) (Participant 15)
Although the robot provided a feeling of safety, it also introduced fear and a feeling of lack of safety when the therapeutic alterations were taking some time to reach the defined SpO2 range. If the robot detected hypoxemia after the patient visited the toilet, for instance, it would increase the oxygen flow, and its alarms would go off and intensify in time. Its response would continue until an acceptable oxygen saturation level was achieved. If the patient is alone, without a nurse at his/her bedside to translate and support the robot’s response, the patient may perceive the amplified airflow and intensified alarms as indicating that he/she is in a precarious health condition and can be terrified by this. One patient expressed mistrust of the device in the quote below.
Robots are dumb. If you give them the wrong information, they will keep repeating it indefinitely. They don’t reflect as nurses do. (Participant 2)
When everything was going according to the plan, the robot strengthened the patients’ feeling of being in control and ability to manage the situation, but in the case of unforeseen events, nursing assistance was required. The experience of a gain or a loss often depended on the patients’ physical or cognitive abilities and personal beliefs. If the patients believed in the usefulness of technology and were physically and cognitively able to understand the robot’s features, they were more likely to experience a gain from therapy rather than a loss.
Humanized robot
The robot became part of the surrounding environment, and due to its alarms, it required much attention. Consequently, the patients often found themselves engaged in dialogue with it. Several patients talked about the robot as if it was a person, jokingly referring to it as “he” or “she.” The patients described how they and the nurses interacted and communicated with the robot by replying to it whenever “it talked” or by asking it to keep its “mouth” shut.
I kept telling it to shut up. I was doing things as fast as I could, and I told it that it would have its way again in a second! When I went to the toilet, it started making trouble. It kept calling me, and I answered by saying, ‘I’m coming! I’m coming!’…. I found it funny how I talked with it, and so did the nurses…. They’d ask it to shut up. (Laughs) (Participant 6)
The presence of the robot in the room made it comparable to a third person who filled an empty space and interacted loudly with its surroundings, attracting much attention, with the risk of diverting attention away from the patient.
Competition for attention
The patients expressed different perspectives on the robot’s impact on their relationships with the nurses. It was stated that the robot, as a new technical treatment modality, received substantial attention from the nurses, who seemed focused on achieving new skills rather than on communicating with them.
The patients described how their bedside talk with the nurses became centered on the information displayed on the robot, with the nurses no longer asking them how they felt.
No, there was not much talk about how I felt, and that’s not meant as criticism. I mean, you can just read everything right there. In that way, it’s smart. You can get all the information you need from the display. The robot was something we shared with the nurses…. It was as if we had it together. It gave us the exact same information. (Participant 1)
On the other hand, other patients recounted how the information displayed on the robot provided an objective description of their actual physical state, creating an option for nurses and patients to engage in a more equal dialog regarding therapy.
Discussion
We wanted to explore how patients with acute exacerbation of COPD experienced being treated with AOA during their hospitalizations. Our main findings were captured in two themes: “adaptation of behavior to the robot” and “robots make patients feel safe but not cared for.”
Our findings showed that patients were willing to compromise their own safety by switching off the AOA so it would not be a “noisy burden.” To some extent, this coincides with the results of the study by Servaty et al. who identified loss of control, dependency, unfamiliarity with technology, decreased human contact, and fear of negative effects on health as the main barriers to the integration of robotics into nursing care (Citation22). To our knowledge, no previous studies have described the role of audio alarms in “human–robot relations.” Despite the fact, that the robotic alarms were intended to optimize patient safety, they may have adverse effects and by generating an avoiding behavior in patients that threaten their safety and recovery. The clinical “management of adherence,” defined as the process of monitoring and supporting patients’ adherence to medications by health care systems, providers, patients, and their social networks (Citation23) must be prioritized and supported by ward staff. It is thus important for health professionals initiating and surveilling robot therapy to understand the patient–robot interaction. We recommend that health professionals engage in a dialogue with patients, providing patients with sufficient information on how to self-manage AOA and its alarms, and health professionals with patients’ perspectives. This dialogue may need to be repeated several times during patients’ hospitalization as the balance in care between therapeutic modifications and patients’ personal perspectives often varies according to the patients’ day-to-day status. Ultimately, if patients are not adherent to therapy, it becomes a nursing task to respond to all the robotic alarms and thereby ensure effective AOA treatment during patients’ hospitalization.
Our study described how the patients felt safe with AOA as they could see how they were being continuously surveilled and provided with sufficient supplemental oxygen. The bodily sensation of airflow as a reassurance of “therapeutic effect” was a mediator for comfort found not only in our study but also in an Australian study by Eastwood et al. who examined a mixed etiology of 17 cardiothoracic and 20 medical surgical patients’ and nurses’ perspectives on oxygen therapy during hospitalization (Citation24). In that qualitative study, Eastwood et al. also found “level of comfort” from device-related soreness and poor fit and “restricted ability to maintain activities of daily living” due to the device as themes mirroring our findings.
Our findings illuminate how the participating patients’ perceived both the pros and cons of AOA. Duality in patients’ perceptions of health technologies was previously described by reviews of robotic technology in nursing care and highlights how robotic interventions can generate different attitudes depending on patients’ individual abilities and perspectives (Citation17, Citation25). The scoping review by Maalouf et al. pointed out how patients’ perceptions of robotic interventions were affected by their understanding of such interventions’ actual intentions (Citation17). A discrepancy between the perceived and actual intentions of the robot can have a negative impact on the patient–robot relationship. In our study, the patients pointed out how the robot made them feel safe but not cared for, even if the only pronounced purpose of the robot was to deliver AOA. The emphasis on “lack of care” in relation to AOA highlights the difference between patients’ expectations and the robot’s intentions. Robotic therapy was shown to be perceived by patients as having the advantage of fostering patient independence from human caregivers and the disadvantage of leading to a loss of freedom and a strong dependence on the robot. Interestingly, this paradox has been confirmed by several studies (Citation17, Citation22, Citation25).
The aforementioned duality of the pros and cons of robotic therapy may exemplify contradictory perspectives of individualized therapies in the form of assistive technologies such as AOA and person-centered care. According to McCormack (Citation26), the impact of emotions on patients’ conscious and unconscious decisions calls for a culture of care, where patients’ views are considered valid by health professionals, and a legitimate basis for decision making. The split between patients’ conscious and unconscious behavioral alterations exemplified by their switching off OA highlights how supporting patient management of adherence to therapeutic technologies should incorporate person-centered care to achieve “adherence to medication.” The transactive relationships between patients, nurses, and the robot have several dimensions and require reciprocity, described by Tetsuya et al. and Schoenhofer et al. as an iterative dynamic “dance” between patients, caregivers, and the robot (Citation27–29). Thus, a dynamic and iterative application process based on person-centered care may prevent patients from altering their behaviors in a way that will threaten their recovery and health.
To our knowledge, no previous studies have examined COPD patients’ experience of AOA during hospitalization. Individualized treatment through the use of different kinds of technologies is expected to evolve rapidly in the years to come, and nurses are predicted to be the primary users of new health technologies (Citation25, Citation30). This calls for nurses to explore and reflect on the interactions between patients, nurses, and technologies. Our findings illustrate how important a person-centered approach is in informing nursing practice on how to optimize the care of COPD patients treated with AOA during their hospitalization. As this study is the first to explore how patients with COPD experienced being treated with AOA during their hospitalization, further research on this topic is recommended.
Strengths and limitations
We believe that the pragmatic yet rigorous and iterative process of the ID methodology helped enhance the credibility of our findings (Citation20, Citation31). To apply our findings to clinical practice in the respiratory wards, we made ongoing considerations of the moral defensibility, disciplinary relevance, pragmatic obligation, contextual awareness, and probable truth of our design (Citation20, Citation31). Based on these considerations, we believe it is a strength of our study that it represents the perspectives of seriously ill COPD patients, a population often excluded from studies. However, due to the patients’ severe illness, breathlessness, and fatigue, some of the interviews in this study were quite short. Nevertheless, these interviews contributed important data because those who were interviewed largely represented the population of interest. The rate of female participants matches the gender distribution in the Danish COPD population (Citation32).
One possible weakness of this study was that the first author both enrolled patients in the RCT and conducted the interviews. In addition, most of the interviews were conducted in hospital with the interviewer wearing a uniform and thereby representing the nursing staff. The combination of the two above mentioned factors may have introduced social-desirability bias, and our findings should be interpreted with this precaution. Another limitation to our study is that it is device-specific, and findings may be specifically related to the interface or alarm limits on the O2matic device used in our study, limiting its generalizability to other AOA-devices. However, we believe that our findings may serve as useful inspiration for health professionals applicating any kind of technical device, by illuminating the variety of patient-specific experiences illustrating facilitators and barriers in the implementation of technical devices.
Conclusion
Our findings illustrate how the AOA alarms making the patients willing to compromise their normal activities, therapy and thereby potentially safety to avoid disturbing their fellow patients and the health professionals in the hospital. This knowledge is essential for health care professionals to be able to support patients’ management of adherence to AOA. We suggest that health professionals, through a person-centered care approach, educate and communicate with patients on how to self-manage AOA and its alarms without activating avoiding behavior that threaten their treatment and recovery.
Contributions
The first and second authors interviewed all the patients. All the authors participated in the data analysis, but the first and last authors took the lead in it and were the ones who worked closest to the original data. The first draft of the paper was made by the first author, but all the authors contributed to the writing of the paper.
Acknowledgements
We thank the patients who participated in this study by sharing their thoughts and experiences about AOA with us, thereby providing us with valuable insights. We also thank the Niels Christian Nielsen Foundation, Danish Lung Association and Copenhagen University Hospital – Hvidovre for financing and supporting this study.
Declaration of interest
First author has no competing interests. O2matic Ltd has not been involved in the study. EFH is the main inventor of O2matic Ltd and a shareholder but has not been involved in data collection or analysis.
Funding
This study was funded by the Niels Christian Nielsens Foundation, the Danish Lung Association and Copenhagen University Hospital Hvidovre.
References
- Global Initiative for Chronic Obstructive Lung Disease. Global strategy for prevention, diagnosis and management of COPD GOLD REPORT 2021. 2021.
- Brill SE, Wedzicha JA. Oxygen therapy in acute exacerbations of chronic obstructive pulmonary disease. Int J COPD. 2014;9:1241–1252.
- Austin MA, Wills KE, Blizzard L, et al. Effect of high flow oxygen on mortality in chronic obstructive randomised controlled trial. BMJ Res. 2010;34:1–8.
- Cameron L, Pilcher J, Weatherall M, et al. The risk of serious adverse outcomes associated with hypoxaemia and hyperoxaemia in acute exacerbations of COPD. Postgrad Med J. 2012;88(1046):684–689. DOI:10.1136/postgradmedj-2012-130809
- Harper J, Kearns N, Bird G, et al. Audit of oxygen administration to achieve a target oxygen saturation range in acutely unwell medical patients. Postgr Med J. 2021;98:461–465.
- Deshpande S, Datey N, Liacos A, et al. Acute oxygen use in hospitalised patients with chronic obstructive pulmonary disease is guideline discordant. Intern Med J. 2021;51(5):780–783. DOI:10.1111/imj.15318
- Wijesinghe M, Perrin K, Healy B, et al. Pre-hospital oxygen therapy in acute exacerbations of chronic obstructive pulmonary disease. Intern Med J. 2009;39(December):1–18.
- De C, Wa B, Holbourn A, et al. Oxygen prescribing practice at Waikato hospital does not meet guideline recommendations. Intern Med J. 2014;44(12a):1231–1234. DOI:10.1111/imj.12602
- Devoe NC, Kyriazis P, Eltanbedawi A, et al. An audit of oxygen supplementation in a large tertiary hospital – we should treat oxygen as any other drug. Hosp Pract. 2020;(Nov):1–4. DOI:10.1080/21548331.2020.1845018
- Hansen FE, Ove JD, Bech CS, et al. Automated oxygen control with O2matic ® during admission with exacerbation of COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:3997–4003. DOI:10.2147/COPD.S183762
- Hansen EF, Bech CS, Vestbo J, et al. Automatic oxygen titration with O2matic ® to patients admitted with COVID-19 and hypoxemic respiratory failure. Eur Clin Respir J. 2020;7(1):1833695–1833698. 10.1080/20018525.2020.1833695.
- Lellouche F, Bouchard P-A, Roberge M, et al. Automated oxygen titration and weaning with FreeO2 in patients with acute exacerbation of COPD: a pilot randomized trial. Int J Chron Obstruct Pulmon Dis. 2016;11(1):1983–1990. DOI:10.2147/COPD.S112820
- L'Her E, Dias P, Gouillou M, et al. Automatic versus manual oxygen administration in the emergency department. Eur Respir J. 2017;50(1):1602552–1602559. DOI:http://dx.doi.org/10.1183/13993003.02552-2016
- Kofod LM, Westerdahl E, Kristensen MT, et al. Effect of automated oxygen titration during walking on dyspnea and endurance in chronic hypoxemic patients with copd: a randomized crossover trial. J Clin Med. 2021;10(21):1–11.
- Vivodtzev I, L’Her E, Vottero G, et al. Automated O2 titration improves exercise capacity in patients with hypercapnic chronic obstructive pulmonary disease: a randomised controlled cross-over trial. Thorax. 2019;74(3):298–301. DOI:10.1136/thoraxjnl-2018-211967
- Ouanes I, Bouhaouala F, Maatouk S, et al. Automatic oxygen administration and weaning in patients following mechanical ventilation. J Crit Care. 2021;61(2021):45–51. 10.1016/j.jcrc.2020.10.005.
- Maalouf N, Sidaoui A, Elhajj IH, et al. Robotics in nursing: a scoping review. J Nurs Sch. 2018;50(6):590–600. DOI:10.1111/jnu.12424
- Storgaard LH, Weinreich UM, Laursen BS. COPD patients ‘ experience of Long-Term domestic Oxygen-Enriched nasal high flow treatment: a qualitative study COPD patients ‘ experience of Long-Term domestic oxyge. COPD J Chronic Obstr Pulm Dis. 2020;17(2):175–183. https://www.tandfonline.com/action/authorSubmission?show = instructions&journalCode = icop20.
- Hunt MR. Strengths and challenges in the use of interpretive description: reflections arising from a study of the moral experience of health professionals in humanitarian work. Qual Health Res. 2009;19(9):1284–1292. DOI:10.1177/1049732309344612
- Thorne S, et al. Interpretive description -qualitative research for applied practice. In: Russe Bernardl H, Kathy C, Clandini jean D, Corbin J, De la Cueste C, Engel J, editors. Interpretive description – Qualitative research for applied practice. 2nd ed. New York and London: Routledge–Taylor & Francis Group; 2016. p. 10–287.
- Thorne S. The great saturation debate: what the “S word” means and doesn’ t mean in qualitative research reporting. Can J Nurs Res. 2020;52(1):3–5. DOI:10.1177/0844562119898554
- Servaty R, Kersten A, Brukamp K, et al. Implementation of robotic devices in nursing care. Barriers and facilitators: an integrative review. BMJ Open. 2020;10(9):e038650-11. DOI:10.1136/bmjopen-2020-038650
- Vrijens B, Geest SD, Hughes DA, ABC Project Team, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012;73(5):691–705. DOI:10.1111/j.1365-2125.2012.04167.x
- Eastwood GM, Connell BO, Gardner A, et al. Patients’ and nurses’ perspectives on oxygen therapy: a qualitative study. J Adv Nurs. 2009;65(3):634–641. DOI:10.1111/j.1365-2648.2008.04933.x
- Gibelli F, Ricci G, Sirignano A, et al. The increasing centrality of robotic technology in the context of nursing care: bioethical implications analyzed through a scoping review approach. J Healthc Eng. 2021;2021:1478025–1478028. DOI:10.1155/2021/1478025
- McCormack B. A conceptual framework for person-centered practice with older people. Int J Nurs Pract. 2003;9(3):202–209. DOI:10.1046/j.1440-172x.2003.00423.x
- Locsin RC, Ito H. Can humanoid nurse robots replace human nurses? J Nurs. 2018;5(1):1–6. DOI:10.7243/2056-9157-5-1
- Tanioka T, Yasuhara Y, Dino MJS, et al. Distruptive engagements with technologies, robotics and caring: advancing the transactive relationship of nursing. Nurs Adm Q. 2019;43(4):313–321. DOI:10.1097/NAQ.0000000000000365
- Schoenhofer SO, Wynsberghe A, van Boykin A, et al. Engaging robots as nursing partners in caring meets care-centered value-sensitive design. Int J Hum Caring. 2019;23(2):157–167. DOI:10.20467/1091-5710.23.2.157
- Watson D, Womack J, Papadakos S. Is artificial intelligence a friend or foe to nursing practice? Crit Care Nurs Q. 2020;43(3):303–311. DOI:10.1097/CNQ.0000000000000315
- Thorne S, Kirkham SR, Macdonald-Emes J. Focus on qualitative methods interpretive description : a noncategorical qualitative alternative for developing nursing knowledge. Res Nurs Health. 1997;20(2):169–177. DOI:10.1002/(SICI)1098-240X(199704)20:2<169::AID-NUR9>3.0.CO;2-I
- Prescott E, Bjerg AM, Andersen PK, et al. Gender difference in smoking effects on lung function and risk of hospitalization for COPD : results from a danish longitudinal population study. Eur Respir J. 1997;10(4):822–827.