The definition of an acute exacerbation of Chronic Obstructive Pulmonary Disease (COPD) has been modified several times the last decade in Global Initiative for COPD (GOLD) recommendations. According to the updated GOLD 2024 recommendations, an exacerbation of COPD is defined as an event characterized by dyspnea and/or cough and sputum that worsen over <14 days [Citation1]. This definition and all the previous ones are descriptive, mainly due to the lack of certain biomarkers which could support a more accurate definition of AECOPD.
Accordingly, the classification of the severity of an exacerbation is based to the level of treatment needed for the management of the event. Currently, COPD exacerbations are classified as mild (treated only with short acting bronchodilators, SABDs), moderate (treated with SABDs and oral corticosteroids ± antibiotics) and severe (visit to the emergency room or hospitalization) [Citation1]. Thus, severe exacerbations according to this definition are linked to hospital visits and admissions. However, the criteria for emergency room visits and hospitalizations are affected by thevariability of healthcare systems worldwide.
GOLD has recently adopted the Rome definition of AECOPD, that considers as severe exacerbations only the events where patients present with hypercapnia and respiratory acidosis [Citation2]. However, this definition is based on laboratory tests and may often fail to stratify the severity of COPD exacerbations in the real-world setting, where many exacerbations are severe even without hypercapnia. Additionally, there are certain difficulties of classifying severe exacerbations according to Rome criteria in a real-world setting: a visual analogue scale (VAS) on dyspnea may not be available for all patients in all settings, arterial blood gases (ABG) may not be available in certain non-tertiary centers, manypatients receive treatment (e.g. with systemic corticosteroids and/or intravenous antibiotics)without proper evaluation of severity based on objective measurements (SaO2, respiratory and heart rate, serum C-reactive protein, or ABG). Nevertheless, the current classification of the GOLD 2024 recommendations is more appropriate for the grading of severity of AECOPD retrospectively (e.g. for the evaluation of future exacerbation risk), and also for clinical trials.
Since 2011, when the assessment and classification of the severity of COPD moved from a simple spirometric grading system to a more combined initial assessment, the history of exacerbations has been used to classify the patients. The original ABCD combined assessment toolhas been reasonablymodified in the 2023 GOLD document bymerginggroupsC and D into the new group “E,” which includes all the exacerbatingpatients, irrespective of their symptomatic status [Citation1]. The single group termed “E” to highlight the clinical relevance of exacerbations and includes COPD patients who have experienced in the previous year ≥ 2 moderate exacerbations or ≥1 ("severe") exacerbation leading to hospitalization. Based on the above, one severe exacerbation would suffice for a patient to be classified in the group “E”. But do all severe COPD exacerbations have the same impact to the course of the disease? Moreover, have all severe COPD exacerbations been correctly defined as severe based on the clinical condition and management of the patients?
In an attempt to address the above questions, we propose a four-level classification system for the severe COPD exacerbations which is presented in :
Figure 1. The proposed 4-levelclassification system of severe COPD exacerbations according to healthcare resource utilization.
SABDs: short acting bronchodilators; CS: Corticosteroids; AECOPD: Acute exacerbation of COPD; NIV: Noninvasive ventilation; MV: Mechanical ventilation
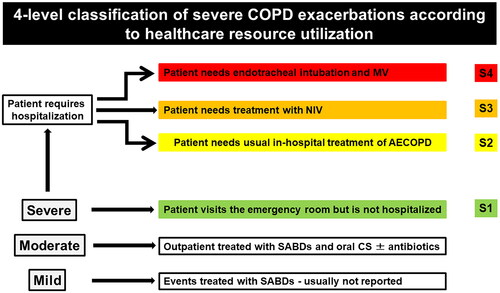
S1: The patient visits the emergency department*, but hospital admission is not needed. Patients who present to emergency room and are not hospitalized may have lower risk of subsequent exacerbations and/or mortality compared to patients with hospitalization for a severe COPD exacerbation [Citation3].
*Importantly, the term visiting emergency department reflects a clear and pragmatic need and not a visit based on social or/and limited access to primary care facilities.
S2: The patient requires hospitalization and is treated with SABDs, systemic corticosteroids (usually not more than 5-7 days), antibiotics when indicated and conventional oxygen therapy (COT) when needed.
S3: The patient needs ventilatory support with noninvasive ventilation (NIV), due to the presence of respiratory acidosis and/or persistent hypoxemia despite supplemental oxygen therapy and/or severe dyspnea with clinical signs suggestive of respiratory muscle fatigue. NIV patients have worse outcomes than those on conventional exacerbation management [Citation4].
S4: The patient needs endotracheal intubation and mechanical ventilation (MV). Possible reasons include inability to tolerate NIV or NIV failure, massive aspiration, inability to remove respiratory secretions, lower level of consciousness, severe hemodynamic instability, severe ventricular or sub-ventricular arrhythmias, status post-respiratory or cardiac arrest). It is important to note that not all patients with severe exacerbations end up in the ICU, despite the physiologic indication to be intubated. The usual reason is futility in patients with severe/very severe COPD in whom a Do-Not-Resuscitate (DNR)/Do-Not-Intubate (DNI) decision has been taken.
In conclusion, our schematic proposal provides a more detailed approach to the severity of hospitalized COPD exacerbations according to healthcare resource utilization. This approach may be useful for and needs to be supported by appropriately designed future trials, and potentially to be tested against current criteria, including the Rome criteria.
Declaration of interest
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- https://goldcopd.org/2024-gold-report/
- Celli BR, Fabbri LM, Aaron SD, et al. An updated definition and severity classification of chronic obstructive pulmonary disease exacerbations: the Rome proposal. Am J Respir Crit Care Med. 2021;204(11):1251–1258. doi:10.1164/rccm.202108-1819PP.
- Janson C, Nwaru BI, Wiklund F, et al. Management and risk of mortality in patients hospitalised due to a first severe COPD exacerbation. Int J Chron Obstruct Pulmon Dis. 2020;15:2673–2682. doi:10.2147/COPD.S276819.
- Stefan MS, Nathanson BH, Higgins TL, et al. Comparative effectiveness of noninvasive and invasive ventilation in critically ill patients with acute exacerbation of chronic obstructive pulmonary disease. Crit Care Med. 2015;43(7):1386–1394. doi:10.1097/CCM.0000000000000945.
