Abstract
To investigate the clinical effects and application value of self-made disseminating and descending breathing exercises on home rehabilitation of patients with stable chronic obstructive pulmonary disease (COPD). Seeking to generate concepts for creating novel, convenient, and efficient COPD prognosis rehabilitation exercises aimed at enhancing the well-being and rehabilitation confidence of both COPD patients and their families. A total of 70 COPD patients admitted to our outpatient department from July 2019 to September 2021 were randomly divided into the exercise group (n = 35) and the control group (n = 35). The control group received routine breathing training, while the exercise group was treated with self-made disseminating and descending breathing exercises. The respiratory function, including pulmonary function (FVC, FEV1, FEV1/FVC) and respiratory muscle strength (MIP, MEP), exercise tolerance (6-min walking distance, 6MWT), Modified Medical Research Council Dyspnea Scale (mMRC, Borg), COPD quality of life score (CAT, SGRQ), anxiety and depression scores (HAMA, HAMD) were compared between the two groups after 12-week exercise. After 12-week training, the FEV1, MIP, and MEP in the exercise group were significantly higher than those in the control group (p < 0.001), and the 6MWT was significantly increased in the exercise group compared to the control group (p < 0.001); while the mMRC, Borg score, the scores of CAT, SGRQ, HAMA, and HAMD were found significantly lower than those in the control group (p < 0.001). The self-made disseminating and descending breathing exercises can improve respiratory function and reduce symptoms of dyspnea in COPD patients, while enhancing exercise tolerance and relieving anxiety and depression, and are worthy of clinical application.
Introduction
Chronic obstructive pulmonary disease (COPD) is an inflammatory multisystemic disease caused by environmental exposures and/or genetic factors [Citation1–3]. According to the World Health Organization data, it is the third leading cause of mortality worldwide at present (https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. Accessed 9 Dec 2020.). According to another study, COPD will become the 7th leading cause of disability and still be the 4th leading cause of death by 2030 [Citation4]. Consequently, effective management of stable COPD is paramount, with a focus on interventions that can prevent disease progression, decelerate its advancement, and enhance the quality of life for patients. This area of research represents a critical focus for improving COPD outcomes [Citation5]. The 2022 GOLD guidelines re-emphasize the effectiveness and importance of respiratory rehabilitation in COPD, and respiratory rehabilitation has been shown to improve exercise capacity, muscle metabolism, and quality of life [Citation6–8]. Nevertheless, the existing exercise training programs for COPD patients primarily conducted in hospitals often encounter challenges such as low patient adherence and participation rates. Hence, there is a need for an internet-based respiratory rehabilitation management and follow-up system that can offer patients a more convenient, efficient, environmentally friendly, and user-friendly approach to enhance adherence and engagement in COPD rehabilitation training [Citation9, Citation10]. This study designed a set of disseminating and descending breathing exercises applicable to train at home for COPD patients to improve their respiratory function, exercise tolerance, and quality of life, thereby promoting the clinical practice of the exercise to benefit more patients. The self-made disseminating and descending breathing exercises consist of four parts: Refreshing and awakening; Neck and shoulder exercises; Open the chest and smooth the flow; Bend and strengthen the legs. The breathing training can reduce the work of respiratory muscles to a certain extent, lower oxygen consumption, improve the lung function of the patients, lessen the acute exacerbations, as well as enhancing the muscle strength of patients upper and lower limbs and improving their exercise capacity. This pioneering study introduces innovative self-designed divergent and descending breathing exercises for COPD rehabilitation training, offering promising insights for the future treatment of COPD patients. This approach stands out for its cost-effectiveness, environmental friendliness, user-friendliness, and positive therapeutic outcomes.
Materials and methods
General information
No statistical methods were used to predetermine sample sizes, but our sample sizes are similar to those reported in previous publications (please delete after reading). A total of 70 COPD patients admitted to the Department of Respiratory and Critical Care Medicine of the Three Gorges Hospital Affiliated to Chongqing University from July 2019 to September 2021 were enrolled in this Institutional Review Board (IRB) approved study. The patients were randomly classified into the exercise group (n = 35) and the control group (n = 35).
Inclusion criteria: (1) GOLD2020: FEV1/FVC < 70% after inhalation of bronchodilators; (2) aged from 40 to 80 years old, with stable chronic obstructive pulmonary disease; (3) mMRC score > 2 points and able to complete the 6-min walk test; (4) All the patients signed the informed consent.
Exclusion criteria: The study excluded patients with (1) pulmonary diseases other than COPD, such as asthma, bronchiectasis, and pulmonary tuberculosis; (2) unstable angina, recent myocardial infarction, acute pulmonary heart disease, poorly controlled arrhythmias, severe valvular stenosis, active myocarditis and other heart diseases; (3) poorly controlled hypertension; (4) acute systemic disease or persistent high fever; (5) recent pulmonary embolism and severe pulmonary hypertension; (6) abnormal metabolism (acute thyroiditis, etc.); (7) musculoskeletal diseases that affect walking or upper limb movement; (8) severe anemia; (9) severe osteoporosis; (10) poor adherence; (11) high cognitive impairment and mental disorders.
Methods
The control group was given routine nursing care, drug therapy, medication skill guidance, oxygen inhalation and diet guidance, self-management, and routine breathing training.
The exercise group was given self-made disseminating and descending breathing exercises which was on top of the routine basic treatment. Outpatient follow-up was performed every 4 weeks for 12 weeks, during which the specialist nurses made weekly telephone follow-up, which included medication, physical status, and exercise.
Routine breathing training mainly guides patients to take a comfortable position for pursed-lip abdominal breathing. The main contents include: (1) Breathing with pursed lips: inhale through the nose, hold the breath for 3 s, and then slowly exhale through the mouth in a “whistling” shape. (2) Abdominal breathing: place the right hand on the belly button and the left hand on the chest, then inhale to expand the abdomen, keep the chest still, and hold the breath for 1s; exhale to retract the abdomen and keep the chest still. The whole set of movements was repeated 3 times a day.
The self-made disseminating and descending breathing exercises consist of 4 parts: (1) Refreshing and awakening: finger movements, hair combing movement, and nose rubbing. (2) Neck and shoulder exercises: neck movement and shoulder shaking. (3) Open the chest and smooth the flow: flapping movement, chest expansion movement, and rotation movement. (4) Bend and strengthen the legs: side lying up training; self-weight squat training; the flexion and extension movements of the ankle joint. Choose "To Alice" by Beethoven as the background music to play during the exercise, 25 min per exercise, twice a day. The patients could take oxygen during the exercise or rest if they are intolerant. The rehabilitation specialist would lead the patients and their families to the rehabilitation hall to master the full set of exercises.
Exercise quality control: (1) a video was made and broadcast on the TV in the rehabilitation hall to ensure that the patients had mastered the full set of action essentials and the video was copied to the patients. The role and benefits of subduing breathing exercises highlighted the importance of home rehabilitation training. (2) The patients were followed up by telephone every 1 week after discharge to inquire about their conditions and exercise status and be given corresponding guidance and supervision. (3) A COPD patient meeting was held every 3 weeks, with the participation of medical staff, patients, and their families. The contents of the patient meeting were as follows: re-instruction and training of breathing exercises, correction of typical wrong movements, the importance of home rehabilitation for COPD, precautions in the process of respiratory rehabilitation, the necessity of respiratory muscle training, treatment of COPD during remission, correct use of inhalation drug device, and feelings and experiences during the recovery process shared by the patients, etc.
Observation indicators
Respiratory function
Respiratory function indexes of the patients, including pulmonary function (FEV1, FVC, FEV1/FVC) and respiratory muscle function (MIP, MEP), were measured before and after exercise using a pulmonary function instrument (JAEGER MasterScreen PFT) [Citation11].
Exercise tolerance
The 6-min walking distance test was carried out to measure the exercise tolerance of patients before and after exercise. The specific method was as follows: in the case of oxygen, each patient walked back and forth as quickly as possible through a 30-m-long corridor, and the 6-min walking distance was calculated. The test was repeated twice, with a 30-min interval between each, and then the mean distance was chosen to analyze the data. During the test, the clinical manifestations of the patients were closely observed, and the test should be stopped immediately once symptoms such as paleness, chest pain, and sweating occurred [Citation12].
Dyspnea score
mMRC and Borg scales were used to score dyspnea before and after exercise. mMRC scale: The patient selected a level of dyspnea according to the description of each level in the table. There were four levels in total, the higher the score, the more severe the dyspnea [Citation13]. Borg scale: The improved scale was composed of grades, arranged from bottom to top. The top of the scale was used to describe the degree of breathing effort of the patient under extremely strenuous exercise, and the bottom of the scale was used to note the breathing effort degree of the patient at rest. The patients would choose the level that best described their breathing effort during exercise [Citation14].
COPD quality of life assessment test
CAT scale and SGRQ score were applied to evaluate the quality of life of patients before and after exercise. The CAT questionnaire was relatively short, with 8 questions covering symptoms, activities, and conditions. Each question corresponded to a 0 to 5 marks option and the full score was 40. The higher the score, the worse the health status [Citation15]. There were 50 items in the SGRQ score, which were divided into three subscales: symptoms, exercise, and effects. The total score for the three subscales ranged from 0 to 100, with higher scores indicating poorer health; 0 meant no injury, and 100 meant maximum damage. The SGRQ score could well reflect the changes in exercise tolerance and quality of life in COPD patients [Citation16].
Hospital anxiety and depression scale (HAD)
This scale is an assessment tool developed specifically to identify anxiety and depression in patients with medical illnesses. It can effectively assess the severity of anxiety and depression symptoms in patients with chronic illnesses. The HAD scale was divided into two subscales, anxiety (HAMA) and depression (HAMD), both containing 7 items, each scored on a scale of 0 to 3, with the highest score of 21 for both scales. A total score of less than 8 on both tables indicated normal, a score between 8 and 10 indicated possible mental illness, and a score greater than or equal to 11 indicated a higher degree of anxiety or depression [Citation17].
Statistical analysis
Statistical analysis of the data was performed using the statistical software SPSS 19.0. The data was verified through the Shapiro-wilk W test to conform the Normal distribution. Measurement data were expressed as mean ± standard deviation or median and compared between two groups using the t-test, which could test whether two sets of uncorrelated samples came from a population with the same mean. The non-parametric rank sum test (Mann-Whitney U) was employed for measurement data that was not normally distributed. Count data were analyzed using the Chi-square test and expressed as frequency or percentage. p < 0.05 was regarded as a statistically significant difference.
Results
Comparison of basic information between the two groups
The basic conditions of the patients were as follows: 18 males and 17 females in the exercise group; aged 40 to 75 years, mean (52.37 ± 12.21) years; 5 to 13 years of disease duration, mean (8.08 ± 3.36) years; 18 patients had a history of smoking; 20 males and 15 females in the control group; aged 45 to 70 years, mean (58 ± 12.56) years; 6 to 15 years of disease duration, mean (8.6 ± 3.32) years; 20 patients had a history of smoking. There were no significant differences in sex, age, course of the disease, and smoking history between the two groups (p > 0.05), which were comparable ().
Table 1. General information of patients.
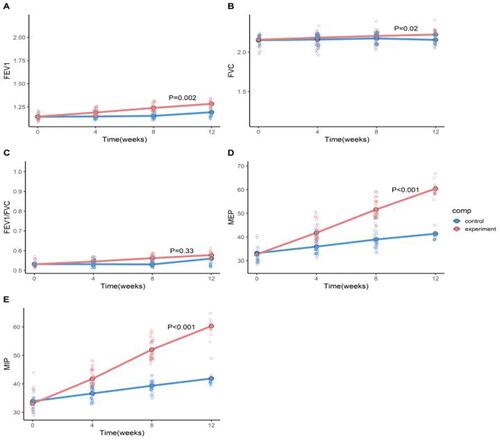
Comparison of respiratory function between the two groups of patients before and after exercise
There was no significant difference in lung function (FEV1, FVC, FEV1/FVC) and respiratory muscle function (MIP, MEP) between the two groups before exercise (p > 0.05). At week 12 after exercise, the respiratory function of the two groups was improved to varying degrees compared with that before exercise. The FEV1, MIP, and MEP of the exercise group at week 12 after exercise were all higher than those in the control group, and the difference was statistically significant (p < 0.05) (). Additionally, the FVC and FEV1/FVC in the exercise group were improved compared to those in the control group and the difference was statistically significant (p < 0.05) ().
Table 2. Comparison of respiratory function before and after 12 weeks of exercise in two groups.
Comparison of exercise tolerance and dyspnea scores between the two groups before and after exercise
There were no significant differences in the 6-min walking distance, m MRC score and Borg score between the two groups before exercise (p > 0.05). In the 12th week after exercise, the above three indicators in the two groups were improved to varying degrees compared with those before exercise (). The 6-min walking distance in the exercise group at 12 weeks after exercise was significantly longer than that in the control group, and the m MRC score and Borg score were dramatically lower than those in the control group (p < 0.05) ().
Figure 2. Comparison of exercise tolerance and dyspnea scores before and after exercise in two groups.
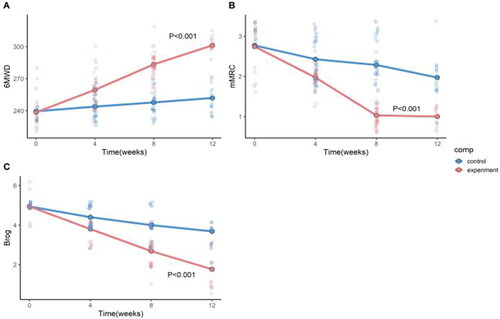
Table 3. Comparison of exercise tolerance and dyspnea scores before and after 12 weeks of exercise in two groups.
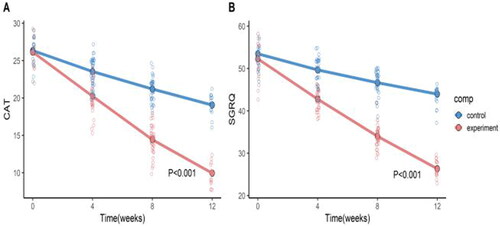
Comparison of the quality of life between the two groups before and after exercise
There were no significant differences in the CAT score and SGRQ score between the two groups before exercise (p > 0.05) (). The CAT score and SGRQ score of the exercise group in the 12th week after exercise were prominently lower than those of the control group (p < 0.001), as shown in .
Table 4. Comparison of the quality of life before and after 12 weeks of exercise in two groups.
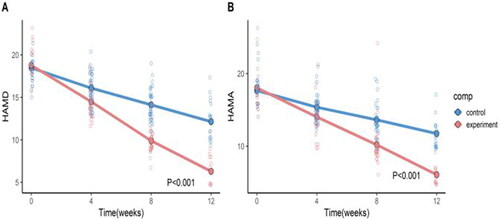
Assessment of anxiety and depression before and after exercise in the two groups
There were no significant differences in the scores of HAMA and HAMD between the two groups before exercise (p > 0.05) (). The HAMA and HAMD scores of the exercise group were markedly lower than those of the control group in the 12th week after exercise (p < 0.001), as shown in .
Table 5. Comparison of anxiety and depression before and after 12 weeks of exercise in two groups.
Discussion
Compared with before exercise, both groups of patients showed varying degrees of improvement in respiratory function. The FEV1, MIP, and MEP of the exercise group were higher than those of the control group at the 12th week after exercise. The 6-min walking distance, mMRC score, and Borg score of both groups of patients showed varying degrees of improvement compared to before exercise, but there was no significant difference between the groups. The CAT score and SGRQ score of the exercise group were significantly lower than those of the control group at the 12th week after exercise. At the 12th week after exercise, the HAMA and HAMD scores of the exercise group were significantly lower than those of the control group. The breathing training is an exercise method that combines abdominal breathing, pursed lip breathing, chest expansion, bending over, and lower limbs. It can increase pulmonary ventilation, enhance respiratory muscle function, lessen residual air volume in alveoli after forced exhalation, reduce alveolar expansion, improve breathing type, improve breathing efficiency, increase muscle strength of the patients’ limbs, and improve chronic breathing and disease-induced skeletal muscle dysfunction. In addition, this exercise can reduce patients fear and anxiety about physical activity, increase their confidence in exercise, help further improve their quality of life, and facilitate patients’ early reintegration into society [Citation5, Citation18–20]. Although the breathing training is helpful for home rehabilitation of COPD, in general, the effect and adherence of respiratory rehabilitation exercises for COPD patients in China are not ideal.
To improve the adherence of home-based rehabilitation breathing training for COPD patients and increase their interest in exercise, our department designed a set of breathing rehabilitation exercises by reviewing the literature, referring to guidelines [Citation21], combining clinical practice, integrating the concepts of traditional Chinese medicine, and adding original light music [Citation8–10]. The breathing exercises take into account head-to-toe movements, and the acts are simple, the use of energy-saving breathing gives patients better tolerance. Through clinical trials, it was found that the pulmonary function (FEV1), respiratory muscle strength (MIP, MEP), exercise tolerance, dyspnea index, quality of life, anxiety, and depression of the exercise group were significantly better than those of the control group at 12 weeks after exercise (p < 0. 05), suggesting that this set of breathing training can reduce the work of respiratory muscles to a certain extent, lower oxygen consumption, improve the lung function of the patients, lessen the acute exacerbations, as well as enhancing the muscle strength of patients and improving their exercise capacity. This set of breathing exercises incorporates the principles of awakening the mind in traditional Chinese medicine concepts and helps to further improve the patient’s immunity. Furthermore, studies reported that the soothing musical atmosphere promotes the release of dopamine in the human body, making people feel happy, which in turn improves the function of the body systems and organs [Citation14]. Music therapy can be effective in reducing dyspnea, anxiety and depression in COPD patients, and can also improve sleep quality and physiological function in patients with COPD [Citation22,Citation23]. Therefore, we specially designed a piece of light music as the background music so that patients could complete the exercises in a more artistic atmosphere. In home-based rehabilitation exercises, the patient’s adherence is a direct factor affecting the rehabilitation effectiveness of COPD, so the quality control of the exercises by the rehabilitation team members is very important. This study used telephone follow-ups every 1 week and patient meetings every 3 weeks to improve the quality of exercise. Through patient association, mutual communication between patients was promoted, which helped increase their enthusiasm for rehabilitation exercises and gave them encouragement and supervision.
To sum up, disseminating and descending breathing exercises can improve the respiratory function and dyspnea index, increase exercise tolerance, improve the anxiety and depression state and the quality of life of COPD patients. Compared to routine respiratory function training, our self-made disseminating and descending breathing exercises are more effective and more innovative, and patients’ adherence is also higher, which is worthy of clinical application.
Research limitations
This study still had certain limitations. Firstly, the sample size selected for this study was relatively limited, and the representativeness of different types of patients might be insufficient. Secondly, this experiment was a single center, small sample study, which still need multi center, large sample and clinical Cohort study to further explore the role of the self-made disseminating and descending breathing exercises in improving the status of COPD patients. Finally, this study’s evaluation of adherence solely through telephone follow-up is not sufficiently comprehensive.
Authors’ contributions
(I) Conception and design: Y Jiao; (II) Administrative support: Y Jiao, LX Chen, FJ-Long; (III) Provision of study materials or patients: Y Jiao, SL Peng, HJ Xiang; (IV) Collection and assembly of data: Jiao Y, He Q, XW Luo; (V) Data analysis and interpretation: LX Chen, LP Mao, Q He (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study is approved by the Ethics Committee of Chongqing University Three Gorges Hospital. All the patients signed the informed consent. Various preventive measures had been taken to protect the privacy of research subjects and avoid the appearance of identifiable text, data, or images that could be traced back to patient information.
Declaration of interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Data availability statement
The simulation experiment data used to support the findings of this study are available from the corresponding author upon request.
Additional information
Funding
References
- Yusen RD. Evolution of the GOLD documents for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Controversies and questions. Am J Respir Crit Care Med. 2013;188(1):4–5. doi: 10.1164/rccm.201305-0846ED.
- Stolz D, Mkorombindo T, Schumann DM, et al. Toward the elimination of chronic obstructive pulmonary disease: a Lancet Commission. Lancet (London England). 2022;400(10356):921–972. doi: 10.1016/S0140-6736(22)01273-9.
- Montes de Oca M, Pérez-Padilla R. Global Initiative for Chronic Obstructive Lung Disease (GOLD)-2017: the alat perspective. Arch Bronconeumol. 2017;53(3):87–88. doi: 10.1016/j.arbres.2017.01.002.
- Wang C, Xu J, Yang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet. 2018;391(10131):1706–1717. doi: 10.1016/S0140-6736(18)30841-9.
- Matte DL, Pizzichini MM, Hoepers AT, et al. Prevalence of depression in COPD: a systematic review and meta-analysis of controlled studies. Respir Med. 2016;117:154–161. doi: 10.1016/j.rmed.2016.06.006.
- Zhu B, Wang Y, Ming J, et al. Disease burden of COPD in China: a systematic review. Int J Chron Obstruct Pulmon Dis. 2018;13:1353–1364. doi: 10.2147/COPD.S161555.
- Mirza S, Clay RD, Koslow MA, et al. COPD Guidelines: a review of the 2018 GOLD Report. Mayo Clin Proc. 2018;93(10):1488–1502. doi: 10.1016/j.mayocp.2018.05.026.
- Mantoani LC, Dell’Era S, MacNee W, et al. Physical activity in patients with COPD: the impact of comorbidities. Expert Rev Respir Med. 2017;11(9):685–698. doi: 10.1080/17476348.2017.1354699.
- Lahham A, McDonald CF, Mahal A, et al. Home-based pulmonary rehabilitation for people with COPD: a qualitative study reporting the patient perspective. Chron Respir Dis. 2018;15(2):123–130. doi: 10.1177/1479972317729050.
- Coultas DB, Jackson BE, Russo R, et al. Home-based physical activity coaching, physical activity, and health care utilization in chronic obstructive pulmonary disease. Chronic obstructive pulmonary disease self-management activation research trial secondary outcomes. Ann Am Thorac Soc. 2018;15(4):470–478. doi: 10.1513/AnnalsATS.201704-308OC.
- Singh D, Agusti A, Anzueto A, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease: the GOLD science committee report 2019. Eur Respir J. 2019;53(5):1900164. doi: 10.1183/13993003.00164-2019.
- Holland AE, Spruit MA, Troosters T, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014;44(6):1428–1446. doi: 10.1183/09031936.00150314.
- Bestall JC, Paul EA, Garrod R, et al. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586. doi: 10.1136/thx.54.7.581.
- Higashimoto Y, Ando M, Sano A, et al. Effect of pulmonary rehabilitation programs including lower limb endurance training on dyspnea in stable COPD: a systematic review and meta-analysis. Respir Investig. 2020;58(5):355–366. doi: 10.1016/j.resinv.2020.05.010.
- Jones PW, Harding G, Berry P, et al. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34(3):648–654. doi: 10.1183/09031936.00102509.
- Wacker ME, Jörres RA, Karch A, et al. Assessing health-related quality of life in COPD: comparing generic and disease-specific instruments with focus on comorbidities. BMC Pulm Med. 2016;16(1):70. doi: 10.1186/s12890-016-0238-9.
- Zimmerman M, Martinez JH, Young D, et al. Severity classification on the Hamilton Depression Rating Scale. J Affect Disord. 2013;150(2):384–388. doi: 10.1016/j.jad.2013.04.028.
- Spielmanns M, Boeselt T, Gloeckl R, et al. Low-volume whole-body vibration training improves exercise capacity in subjects with mild to severe COPD. Respir Care. 2017;62(3):315–323. doi: 10.4187/respcare.05154.
- Probst VS, Kovelis D, Hernandes NA, et al. Effects of 2 exercise training programs on physical activity in daily life in patients with COPD. Respir Care. 2011;56(11):1799–1807. doi: 10.4187/respcare.01110.
- Grunau PD, Arneja S, Leith JM. A randomized clinical trial to assess the clinical effectiveness of a measured objective tensioning device in hamstring anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(6):1482–1486. doi: 10.1177/0363546516634021.
- Effing TW, Vercoulen JH, Bourbeau J, et al. Definition of a COPD self-management intervention: international Expert Group consensus. Eur Respir J. 2016;48(1):46–54. doi: 10.1183/13993003.00025-2016.
- Huang J, Yuan X, Zhang N, et al. Music therapy in adults with COPD. Respir Care. 2021;66(3):501–509. doi: 10.4187/respcare.07489.
- Gordon CS, Waller JW, Cook RM, et al. Effect of pulmonary rehabilitation on symptoms of anxiety and depression in COPD: a systematic review and meta-analysis. Chest. 2019;156(1):80–91. doi: 10.1016/j.chest.2019.04.009.