ABSTRACT
Lisfranc injuries, often accompanied with tarsometatarsal joint (TMTJ) disruption, are not well documented in football despite becoming increasingly more prevalent within other athletic populations. Currently there is a paucity of evidence documenting prognosis, rehabilitation strategy and outcome. The presented case summarizes the conservative rehabilitation and return to play of a 26-year-old elite professional footballer who presented with a Lisfranc injury alongside a 3rd TMTJ coalition stress response. Injury was sustained when landing awkwardly from a jump causing the midfoot to be forced into a hyper-plantarflexed position. Palpation identified tenderness over the 2nd and 3rd MT, with a positive piano key test. Magnetic resonance imaging (MRI), computed tomography (CT), stork view x-ray and review from a leading foot and ankle specialist confirmed diagnosis, post-contradictory MRI results. Presented is a summary of the assessment process, conservative management of the injury and the resultant rehabilitation process followed, which led to the successful return to play of the athlete.
Introduction
Lisfranc injuries in the general population are uncommon, representing 0.2% of all fractures, with an incidence of 1 in 55,000 people (Eleftheriou et al., Citation2013). These injuries are becoming more recognized in the sporting population, although more research is required to identify rehabilitation strategies and time to return to training or game play (Deol et al., Citation2016; Michael, Citation2017).
Knowledge of the anatomy of the Lisfranc complex is essential to understanding the clinical, imaging and biomechanical features of an acute Lisfranc injury (LFI) (Mulcahy, Citation2018; Palastanga et al., Citation2006). The tarsometatarsal joint (TMTJ) capsules and the ligaments make up an interlaced framework surrounding the Lisfranc joint. Each set of ligaments consists of fibres which run longitudinal, oblique and transversely, which may give reason regarding inconsistency in the orthopaedic and radiological literature (Castro et al., Citation2010; Hatem, Citation2008). The dorsal and plantar ligament systems are reinforced by intertarsal and intermetatarsal ligaments and generally the plantar ligament system is stronger than the dorsal ligament system, hence why dorsal dislocations are more common (Mulcahy, Citation2018; De Orio et al., Citation2009; Palastanga et al., Citation2006). The interosseous Lisfranc ligament runs obliquely from the base of the second metatarsal to the medial cuneiform with its importance highlighted because no ligament connects the base of first and second metatarsals (Arastu & Buckley, Citation2012). The plantar surface has a certain degree of stability primarily due to its various ligaments however this is further reinforced, especially medially, by the insertion of muscles. Slips from tibialis posterior and anterior tendon reinforce the joints of the medial three metatarsals (Palastanga et al., Citation2006).
Biomechanically the recovery of alignment of the Lisfranc joint (midfoot) is very important to ensure the transference of load from the midfoot to the forefoot. Despite the small movement possible at the TMTJ, a small degree of flexibility is achieved, particularly inversion and eversion. The obliquity of the line of the TMTJ’s from medial, superior and anterior to lateral, inferior and posterior is further complexified by the two ends having opposing obliquity. Resultant change in height of the transverse metatarsal arch is possible during weight-bearing activity. The mobility of the first metatarsal (medial column) is necessary to allow inversion and eversion. In contrast the immobile and rigid second metatarsal (middle column), together with the slenderness of its shaft, is associated with increased fracture risk (Palastanga et al., Citation2006).
Case Description
The present case study represents a 26 yr old elite footballer, who previously displayed residual lower limb asymmetries associated with previous syndesmotic ankle sprain injury. These included a cavus (high arch) foot position and a reduced range of dorsiflexion, which have been associated with mid-foot injury (Burns & Crosbie, Citation2005; Mason-Mackay et al., Citation2017; Riddle et al., Citation2003). During game play the player experienced a sharp localized pain in the left midfoot region when landing, forcing the foot into a hyper-plantarflexed position, a mechanism consistent with LFI (Myerson et al., Citation1986; McGarvey & Coetzee, Citation2020; Rosenbaum et al., Citation2011; Wagner et al., Citation2020). Presentation highlighted tenderness over the proximal aspect of the 2nd and 3rd metatarsals (MT) with a positive piano key test, a key indicator of LFI (Seybold & Coetzee, Citation2015) ().
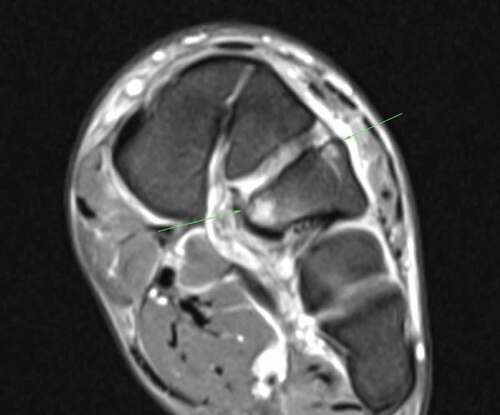
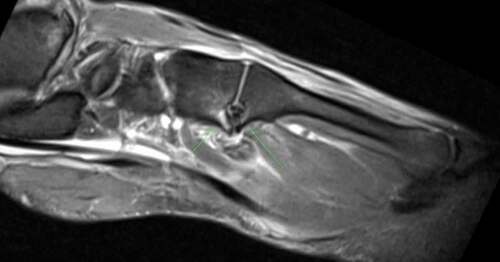
Radiographs are mandatory for a suspected LFI with initial evaluation of non-weight-bearing (NWB) anteroposterior, 30 degrees internal oblique, and lateral images of the injured foot (Lewis & Anderson, Citation2016; Mulcahy, Citation2018). Magnetic resonance imaging (MRI) and a subsequent computed tomography (CT) scan to identify subtle findings associated with LFI (Hatem, Citation2008; Preidler et al., Citation1999) were arranged and reviewed by two radiologists detailing different findings. Initial reporting identified avulsion fracture immediately medial to the base of the 2nd MT with associated oedema, thickening and poor definition of the Lisfranc ligament. The follow up described no LFI or acute fracture, an acute osseous stress response in the lateral cuneiform () and associated chronic fibrosis coalition across the plantar joint margin of the 3rd TMTJ (). Highlighting, the importance of patient presentation, clinical assessment and appropriate imaging (Eleftheriou et al., Citation2013; Keiserman et al., Citation2003; Sherief et al., Citation2007). Subtle LFI may not be identified via NWB radiographs due to osseous overlap at the TMTJ and possible spontaneous reduction after trauma therefore important to obtain weight-bearing films if possible (Llopis et al., Citation2016; Myerson et al., Citation1986; Raikin et al., Citation2009).
Figure 3. Magnetic resonance imaging highlighting 3rd TMTJ fibrous coalition and traumatic stress response
Further review by a foot and ankle specialist (MD) with associated weight-bearing (stork view) x-ray confirmed initial suspicion of LFI. No lateral subluxation at the 2nd TMTJ or widening between the medial and middle columns was reported. A conservative management approach was recommended (Lewis & Anderson, Citation2016). The athlete remained in an Aircast® AirSelect Elite Boot (DJO Aircast Walker, Vista, CA) non-weight bearing (NWB) via elbow crutches for a period of 6-weeks prior to a gradual increase in weight-bearing (WB) activities with a 3-4 month return to play prognosis discussed. This initiated the rehabilitation process completed and outlined within .
Table 1. Conservative management Lisfranc injury rehabilitation guide
Discussion
The present case study highlights the importance of following a routine systematic approach when examining the athlete. Clinical findings in LFI can be varied and high clinical suspicion is critical to diagnose especially when considering the mechanism of injury (MOI). Diagnosis of the injury aligned clinical examination findings (inability to WB, pain TMTJ, positive Piano Key Test) (Keiserman et al., Citation2003; Seybold & Coetzee, Citation2015; Sherief et al., Citation2007) with appropriate MRI, CT and X-ray imaging (Hatem, Citation2008; Lewis & Anderson, Citation2016; Mulcahy, Citation2018; Preidler et al., Citation1999). Literature highlights differences between surgical and conservative management in relation to return to training/play (RTP), with complications reported with surgical approaches (Desmond & Chou, Citation2006; Stavlas et al., Citation2010; Wedmore et al., Citation2015). The approach taken is dependent on the integrity of the Lisfranc complex and stability of the midfoot (Brin et al., Citation2010; Kuo et al., Citation2000; Pelt et al., Citation2011). Implementation of a conservative accelerated rehabilitation programme returned the current case study to full training at 87 days, playing competitively at 93 days. Completion of a 6-month post RTP review highlights that the player is asymptomatic with no associated joint laxity or injury risk.
The accelerated rehabilitation protocol consists of an initial 6-week progressive strengthening programme abiding by the non and partial weight-bearing instruction on the ipsilateral lower limb. An example of this strength programme can be seen in . In week two localized work around the LFI was initiated. Ankle range of motion (ROM) exercises was initiated in a NWB position utilizing active and passive plantarflexion and dorsiflexion physiological movements alongside talocrural and subtalar accessory movements. The muscular capacity of the intrinsic foot muscles (IFM) was developed from week two. Acting as the main local stabilizers of the foot and as part of the active and neural subsystems that constitute the foot core (McKeon et al., Citation2015). The abductor hallucis, flexor digitorum brevis and quadratus plantae are key muscles that eccentrically lengthen during the early stance phase of running producing negative work, prior to a concentric contraction aiding in propulsion by positive work during the late stance phase as the arch recoils (Tourillon et al., Citation2019). High neural stimulus and muscular adaptations resulting in strength increases of the contralateral limb after performing high load unilateral exercises are well documented in the literature (Cirer-Sastre et al., Citation2017; Fisher, Citation2018). This concept of “cross education” was utilized during weeks one to six of the rehabilitation to increase strength and prevent atrophy, particularly within the calf musculature during the period of immobilization (Farthing & Zeir, Citation2014; Hendy et al., Citation2012; Lepley & Palmieri-Smith, Citation2014).
Table 2. Example of a 2 day microcycle alternating a themed quadriceps and hamstrings and gluteal, adductor and posterior lower leg strengthening programme
Close consideration had to be taken to ensure loading the plantar flexors did not have a detrimental effect on the injury site, the Lisfranc region. Progressive plantarflexion strengthening correlated with the WB status and associated loading through the midfoot. Optimal loading to maximize healing is well established with manipulation of load having a significant effect on the morphology and mechanical properties of the musculoskeletal system (Glasgow et al., Citation2015). Whilst it was important to load the LFI and the atrophied ankle plantar flexors compartment, identification and progression of optimal load within a progressive strengthening plan were crucial to maximize physiological adaptation (Korpelainen et al., Citation2001; Pegrum et al., Citation2012). Strength gains were superimposed by alternating blood flow restriction (BFR) and neuromuscular electrical stimulation (NMES) throughout the whole rehabilitation process in accordance with current research (Hughes et al., Citation2017; Maffiuletti, Citation2010; Rosenblatt, Citation2012). Weight-bearing plantarflexion strengthening exercises correlated with the athlete mobilizing and moving a proportion of body weight on the Alter G anti-gravity treadmill (Thomson et al., Citation2017). Contralateral strengthening using the IKD was prescribed throughout the entirety of the rehabilitation alongside ipsilateral strengthening away from the injury site. Ipsilateral ankle plantarflexion strengthening started at week eight initially at 30-50% of contralateral peak torque. Week ten addressed the bilateral equalization of total work and peak torque of ankle plantarflexion concentrically and eccentrically (90 + 10 degrees/second), which correlated with the start of outdoor rehabilitation (Hébert-Losier et al., Citation2009). An evidence-informed graduated progression and return to loading were followed in accordance with Thomson et al. (Citation2017), to estimate peak plantar forces. All outdoor sessions were monitored utilizing Catapult Sports Vector Units and guided by the “control/chaos” approach (Taberner et al., Citation2019). Force absorption and production alongside reactive strength and plyometric-based activity were developed from week six and continued as daily preparation for on-field rehabilitation.
Appropriate weekly planning of sessions was significant to ensure optimal load progressions with graduated running volumes and musculoskeletal impact forces. In the initial stages of rehabilitation highly controlled straight-line work was commenced with gradual progressions in terms of volume (total distance and high-speed running (HSR)) and intensity (metres per minute and HSR) (Buchheit & Laursen, Citation2013). Technical and positional specific tasks were minimized during this stage to reduce movement variability and build confidence in the athlete. During weeks 11 and 12 the athlete was exposed to a progressive mechanical stimulus with the integration of change of direction and acceleration/deceleration movements alongside position-specific drills. Fundamental movement patterns relating to the MOI that players are exposed to during game play (Bloomfield et al., Citation2007; Harper et al., Citation2019). This approach addressed specific conditioning to increase fatigue resistance and reduce injury risk (Gabbett & Ullah, Citation2012; Harper et al., Citation2019; Verheul et al., Citation2019). All work completed in this return to training stage was guided by previous competitive accelerometry data considering total distance (m), high-speed running (>5.5m/s), sprint distance (>7 m/s), number and intensity (0-1, 1-2, 2-3, 3+ ms−2) of accelerations and decelerations () and the internal load using heart rate analysis to determine adaptation to training (Gabbett & Ullah, Citation2012; Harper et al., Citation2019). Failure to recognize possible LFI early can be catastrophic for the biomechanical function of the athlete’s foot. The present case presents issues surrounding conflicting diagnosis surrounding interpretation of the initial MRI. Thorough clinical assessment guided further investigation and early identification of the LFI was essential for a successful management plan to be implemented. In this case a conservative approach resulted in successful return to play of this athlete, with no re-injury issues to date.
Table 3. GPS and accelerometry data outlining absolute/relative external loads in the final 4 days of rehabilitation prior to return to training
References
- Arastu, M. H., & Buckley, R. E. (2012). Tarsometatarsal joint complex and midtarsal injuries. Acta chirurgiae Orthopaedicae Et Traumatologiae Cechoslovaca, 79(1), 21–30.
- Bloomfield, J., Polman, R., & O’Donoghue, P. (2007). Deceleration movements performed during FA premier league soccer matches. Journal of Sports Science and Medicine, 6(10), 6.
- Brin, Y. S., Nyska, M., & Kish, B. (2010). Lisfranc injury repair with the TightRope™ device: a short-term case series. Foot & Ankle International, 31(7), 624–627. doi:https://doi.org/10.3113/FAI.2010.0624
- Buchheit, M., & Laursen, P. B. (2013). High-intensity interval training, solutions to the programming puzzle. Sports Medicine, 43(10), 927–954. doi:https://doi.org/10.1007/s40279-013-0066-5
- Burns, J., & Crosbie, J. (2005). Weight bearing ankle dorsiflexion range of motion in idiopathic pes cavus compared to normal and pes planus feet. The Foot, 15(2), 91–94. doi:https://doi.org/10.1016/j.foot.2005.03.003
- Castro, M., Melao, L., Canella, C., Weber, M., Negrao, P., Trudell, D., & Resnick, D. (2010). Lisfranc joint ligamentous complex: MRI with anatomic correlation in cadavers. American Journal of Roentgenology, 195(6), W447–W455. doi:https://doi.org/10.2214/AJR.10.4674
- Cirer-Sastre, R., Beltrán-Garrido, J. V., & Corbi, F. (2017). Contralateral effects after unilateral strength training: A meta-analysis comparing training loads. Journal of Sports Science & Medicine, 16(2), 180.
- De Orio, M., Erickson, M., Usuelli, F. G., & Easley, M. (2009). Lisfranc injuries in sport. Foot and Ankle Clinics, 14(2), 169–186. doi:https://doi.org/10.1016/j.fcl.2009.03.008
- Deol, R. S., Roche, A., & Calder, J. D. F. (2016). Return to training and playing after acute lisfranc injuries in elite professional soccer and rugby players. American Journal of Sports Medicine, 44(1), 166–170. doi:https://doi.org/10.1177/0363546515616814
- Desmond, E. A., & Chou, L. B. (2006). Current concepts review: Lisfranc injuries. Foot & Ankle International, 27(8), 653–660. doi:https://doi.org/10.1177/107110070602700819
- Eleftheriou, K. I., Rosenfeld, P. F., & Calder, J. D. (2013). Lisfranc injuries: An update. Knee Surgery, Sports Trauma and Arthroscopy, 21(6), 1434–1446. doi:https://doi.org/10.1007/s00167-013-2491-2
- Farthing, J. P., & Zeir, E. P. (2014). Restoring symmetry: Clinical applications of cross-education. Exercise and Sport Sciences Reviews, 42(2), 70–75. doi:https://doi.org/10.1249/JES.0000000000000009
- Fisher, J. P. (2018). Contralateral effects after unilateral strength training: A meta-analysis comparing training loads. Journal of Sports Science & Medicine, 17(1), 163.
- Gabbett, T. J., & Ullah, S. (2012). Relationship between running loads and soft-tissue injury in elite team sport athletes. The Journal of Strength and Conditioning Research, 26(4), 953–960. doi:https://doi.org/10.1519/JSC.0b013e3182302023
- Glasgow, P., Phillips, N., & Bleakley, C. (2015). Optimal loading: Key variables and mechanisms. British journal of Sports Medicine (online). doi:https://doi.org/10.1136/bjsports-2014-094443
- Harper, D. J., Carling, C., & Kiely, J. (2019). High-intensity acceleration and deceleration demands in elite team sports competitive match play: A systematic review and meta-analysis of observational studies. Sports Medicine, 49(12), 1923–1947. doi:https://doi.org/10.1007/s40279-019-01170-1
- Hatem, S. F. (2008). Imaging of Lisfranc injury and midfoot sprain. Radiologic Clinics of North America, 46(6), 1045–1060. doi:https://doi.org/10.1016/j.rcl.2008.09.003
- Hébert-Losier, K., Newsham-West, R. J., Schneiders, A. G., & Sullivan, S. J. (2009). Raising the standards of the calf-raise test: A systematic review. Journal of Science and Medicine in Sport, 12(6), 594–602. doi:https://doi.org/10.1016/j.jsams.2008.12.628
- Hendy, A. M., Spittle, M., & Kidgell, D. J. (2012). Cross education and immobilisation: Mechanisms and implications for injury rehabilitation. Journal of Science and Medicine in Sport, 15(2), 94–101. doi:https://doi.org/10.1016/j.jsams.2011.07.007
- Hughes, L., Paton, B., Rosenblatt, B., Gissane, C., & Patterson, S. D. (2017). Blood flow restriction training in clinical musculoskeletal rehabilitation: A systematic review and meta-analysis. British Journal of Sports Medicine, 51(13), 1003–1011. doi:https://doi.org/10.1136/bjsports-2016-097071
- Keiserman, L. S., Cassandra, J., & Amis, J. A. (2003). The piano key test: A clinical sign for the identification of subtle tarsometatarsal pathology. Foot & Ankle International, 24(5), 437–438. doi:https://doi.org/10.1177/107110070302400511
- Korpelainen, R., Orava, S., Karpakka, J., Siira, P., & Hulkko, A. (2001). Risk factors for recurrent stress fractures in athletes. American Journal of Sports Medicine, 29(3), 304–310. doi:https://doi.org/10.1177/03635465010290030901
- Kuo, R. S., Tejwani, N. C., Digiovanni, C. W., Holt, S. K., Benirschke, S. K., Hansen, J. S. T., & Sangeorzan, B. J. (2000). Outcome after open reduction and internal fixation of Lisfranc joint injuries. JBJS, 82(11), 1609. doi:https://doi.org/10.2106/00004623-200011000-00015
- Lepley, L. K., & Palmieri-Smith, R. M. (2014). Cross-education strength and activation after eccentric exercise. Journal of Athletic Training, 49(5), 582–589. doi:https://doi.org/10.4085/1062-6050-49.3.24
- Lewis, J. J. S., & Anderson, R. B. (2016). Lisfranc injuries in the athlete. Foot & Ankle International, 37(12), 1374–1380. doi:https://doi.org/10.1177/1071100716675293
- Llopis, E., Carrascoso, J., Iriarte, I., De Prado Serrano, M., & Cerezal, L. (2016). Lisfranc injury imaging and surgical management. In Seminars in musculoskeletal radiology. Thieme Medical Publishers, 20(2), 139–153. doi:https://doi.org/10.1055/s-0036-1581119
- Maffiuletti, N. A. (2010). Physiological and methodological considerations for the use of neuromuscular electrical stimulation. the European Journal of Applied Physiology, 110(2), 223–234. doi:https://doi.org/10.1007/s00421-010-1502-y
- Mason-Mackay, A. R., Whatman, C., & Reid, D. (2017). The effect of reduced ankle dorsiflexion on lower extremity mechanics during landing: A systematic review. Journal of Science and Medicine in Sport, 20(5), 451–458. doi:https://doi.org/10.1016/j.jsams.2015.06.006
- McGarvey, W. C., & Coetzee, J. C. (2020). Midfoot Fractures and Dislocations. Baxter’s The Foot and Ankle in Sport.
- McKeon, P. O., Hertel, J., Bramble, D., & Davis, I. (2015). The foot core system: A new paradigm for understanding intrinsic foot muscle function. British Journal of Sports Medicine, 49(5), 290. doi:https://doi.org/10.1136/bjsports-2013-092690
- Michael, C. P. (2017). Lisfranc Injuries. Foot and Ankle Sports Medicine, 10(1), 81–85. doi:https://doi.org/10.1007/s12178-017-9387-6
- Mulcahy, H. (2018). Lisfranc injury: Current concepts. Radiologic Clinics, 56(6), 859–876. doi:https://doi.org/10.1016/j.rcl.2018.06.003
- Myerson, M. S., Fisher, R. T., Burgess, A. R., & Kenzora, J. E. (1986). Fracture dislocations of the tarsometatarsal joints: end results correlated with pathology and treatment. Foot & Ankle, 6(5), 225–242. doi:https://doi.org/10.1177/107110078600600504
- Palastanga, N., Field, D., & Soames, R. (2006). Anatomy and human movement: Structure and function. Elsevier Health Sciences.
- Pegrum, J., Crisp, T., & Padhiar, N. (2012). Diagnosis and management of bone stress injuries of the lower limb in athletes. The BMJ, 24, 344, e2511. doi:https://doi.org/10.1136/bmj.e2511
- Pelt, C. E., Bachus, K. N., Vance, R. E., & Beals, T. C. (2011). A biomechanical analysis of a tensioned suture device in the fixation of the ligamentous Lisfranc injury. Foot & Ankle International, 32(4), 422–431. doi:https://doi.org/10.3113/FAI.2011.0422
- Preidler, K. W., Peicha, G., Lajtai, G., Seibert, F. J., Fock, C., Szolar, D. M., & Raith, H. (1999). Conventional radiography, CT, and MR imaging in patients with hyperflexion injuries of the foot: Diagnostic accuracy in the detection of bony and ligamentous changes. AJR. American Journal of Roentgenology, 173(6), 1673–1677. doi:https://doi.org/10.2214/ajr.173.6.10584818
- Raikin, S. M., Elias, I., Dheer, S., Besser, M. P., Morrison, W. B., & Zoga, A. C. (2009). Prediction of midfoot instability in the subtle lisfranc injury: Comparison of magnetic resonance imaging with intraoperative findings. Journal of Bone & Joint Surgery, 91(4), 892–899. doi:https://doi.org/10.2106/JBJS.H.01075
- Riddle, D. L., Pulisic, M., Pidcoe, P., & Johnson, R. E. (2003). Risk factors for plantar fasciitis: A matched case-control study. JBJS, 85(5), 872–877. doi:https://doi.org/10.2106/00004623-200305000-00015
- Rosenbaum, A., Dellenbaugh, S., DiPreta, J., & Uh, R. (2011). Subtle injuries to the Lisfranc joint. Ortho, 34(11), 882–887. doi:https://doi.org/10.3928/01477447-20110922-23
- Rosenblatt, B. (2012). The effect of low blood flow restricted resistance training in rehabilitation of elite athletes. Int Cong of Strength Train.
- Seybold, J. D., & Coetzee, J. C. (2015). Lisfranc injuries: When to observe, fix or fuse. Clinics in Sports Medicine, 34(4), 705–723. doi:https://doi.org/10.1016/j.csm.2015.06.006
- Sherief, T. I., Mucci, B., & Greiss, M. (2007). Lisfranc injury: How frequently does it get missed? And how can we improve?. Injury, 38(7), 856–860. doi:https://doi.org/10.1016/j.injury.2006.10.002
- Stavlas, P., Roberts, C. S., Xypnitos, F. N., & Giannoudis, P. V. (2010). The role of reduction and internal fixation of Lisfranc fracture–dislocations: a systematic review of the literature. International Orthopaedics, 34(8), 1083–1091. doi:https://doi.org/10.1007/s00264-010-1101-x
- Taberner, M., Allen, T., & Cohen, D. D. (2019). Progressing rehabilitation after injury: Consider the ‘control-chaos continuum’. British Journal of Sports Medicine, 53(18), 1132–1136. doi:https://doi.org/10.1136/bjsports-2018-100157
- Thomson, A., Einarsson, E., Witvrouw, E., & Whiteley, R. (2017). Running speed increases plantar load more than per cent body weight on an AlterG® treadmill. Journal of Sports Science, 35(3), 277–282. doi:https://doi.org/10.1080/02640414.2016.1163401
- Tourillon, R., Gojanovic, B., & Fourchet, F. (2019). How to evaluate and improve foot strength in athletes: An update. Frontiers in Sports and Active Living, 1:46. doi:https://doi.org/10.3389/fspor.2019.00046
- Verheul, J., Nedergaard, N. J., Pogson, M., Lisboa, P., Gregson, W., Vanrenterghem, J., & Robinson, M. A. (2019). Biomechanical loading during running: can a two mass-spring-damper model be used to evaluate ground reaction forces for high-intensity tasks? Sports Biographies, 29, 1–12. doi:https://doi.org/10.1080/14763141.2019.1584238
- Wagner, E., Wagner, P., Baumfeld, T., Prado, M. P., Baumfeld, D., & Nery, C. (2020). Biomechanical evaluation with a novel cadaveric model using supination and pronation testing of a lisfranc ligament injury. Foot & Ankle Orthopedic, 5(1), 1–6. doi:https://doi.org/10.1177/2473011419898265
- Wedmore, I., Young, S., & Franklin, J. (2015). Emergency department evaluation and management of foot and ankle pain. Emergency Medicine Clinics of North America, 33(2), 363–396. doi:https://doi.org/10.1016/j.emc.2014.12.008