Abstract
Tris(1-chloro-2-propyl) phosphate (TCPP, also referenced as TCIPP), a flame retardant used in spray polyurethane foam insulation, increases cell toxicity and affects fetal development. Spray polyurethane foam workers have the potential to be exposed to TCPP during application. In this study, we determined exposure to TCPP and concentrations of the urinary biomarker bis(1-chloro-2-propyl) phosphate (BCPP) among 29 spray polyurethane foam workers over 2 work days. Work was conducted at residential or commercial facilities using both open-cell (low density) and closed-cell (high density) foam. Study participants provided two personal air samples (Day 1 and Day 2), two hand wipe samples (Pre-shift Day 2 and Post-shift Day 2), and two spot urine samples (Pre-shift Day 1 and Post-shift Day 2). Bulk samples of cured spray foam were also analyzed. Sprayers were found to have significantly higher TCPP geometric mean (GM) concentration in personal air samples (87.1 μg/m3), compared to helpers (30.2 μg/m3; p = 0.025). A statistically significant difference was observed between TCPP pre- and post-shift hand wipe GM concentrations (p = 0.004). Specifically, TCPP GM concentration in post-shift hand wipe samples of helpers (106,000 ng/sample) was significantly greater than pre-shift (27,300 ng/sample; p < 0.001). The GM concentration of the urinary biomarker BCPP (23.8 μg/g creatinine) was notably higher than the adult male general population (0.159 μg/g creatinine, p < 0.001). Urinary BCPP GM concentration increased significantly from Pre-shift Day 1 to Post-shift Day 2 for sprayers (p = 0.013) and helpers (p = 0.009). Among bulk samples, cured open-cell foam had a TCPP GM concentration of 9.23% by weight while closed-cell foam was 1.68%. Overall, post-shift BCPP urine concentrations were observed to be associated with TCPP air and hand wipe concentrations, as well as job position (sprayer vs. helper). Spray polyurethane foam workers should wear personal protective equipment including air-supplied respirators, coveralls, and gloves during application.
Introduction
This study is an analysis of one industry as part of a larger study measuring flame retardants across multiple industries. Specifically, this analysis focused on spray polyurethane foam (SPF) application and tris(1-chloro-2-propyl) phosphate (TCPP, also referred to as TCIPP), an additive flame retardant used primarily in rigid and soft polyurethane foams.[Citation1] At room temperature, TCPP (CAS number 13675-84-5) is a clear, colorless liquid with low vapor pressure and is considered semivolatile.[Citation2]
TCPP was first commercially used in the 1960s and has been used as a replacement for tris(2-chloroethyl) phosphate (TCEP), a chemical labeled as a carcinogen.[Citation3] TCPP has been used to retard flame formation in furniture foams[Citation4] and SPF insulation. TCPP is used in SPF because it is not a known carcinogen and, compared to TCEP, more stable in the presence of water and amine catalysts, an important factor for increasing shelf life of the spray.[Citation5] In spray foams used for insulation, TCPP concentration contributes up to 12% of the total by weight.[Citation6]
The SPF consists of two liquid parts, A and B. Side A is a polymeric methylene diphenyl diisocyanate, and side B is a combination of polyol, blowing agents, catalysts, and flame retardants, including TCPP. For application, Sides A and B are heated and combined in a 1:1 ratio at 1,000–1,500 pounds per square inch (psi) to form a solid polyurethane foam.[Citation7] There are two densities of SPF: open-cell and closed-cell. Open-cell uses water as a blowing agent and has a lower density, while closed-cell has a higher density.[Citation7] Open-cell spray foam generally has higher concentrations of TCPP compared to closed-cell foam.[Citation6]
Organophosphate flame retardants such as TCEP and tris(1,3-dichloro-2-propyl) phosphate (TDCPP), similar in structure to TCPP, are listed in California prop 65 as carcinogenic.[Citation8,Citation9] At high concentrations, TCPP may affect development in chicken embryos[Citation10] and has been shown to be toxic to human cells.[Citation11,Citation12] A study investigating the effects of some (TDCPP, triphenyl phosphate, and isopropyl phenol phosphate) organophosphate flame retardants on reproduction found low-level urinary biomarkers to be associated with adverse reproductive effects.[Citation13] TCPP is persistent in the environment and absorbed through the skin.[Citation6] In an in vitro dermal absorption study, 2.3–32.8% of the applied dose of TCPP was absorbed through the skin.[Citation9] In another study, 25% of an applied dose of TCPP to ex vivo skin was absorbed after 24-hr exposure.[Citation14] There is limited information available on the metabolism of TCPP in humans and the elimination half-life has not been reported.[Citation15,Citation16] TCPP is rapidly metabolized[Citation9] in fish and rats, though it can accumulate in the liver of rats.[Citation17] An in vitro study in herring gulls confirmed a rapid depletion rate.[Citation18]
Occupational and residential studies have been conducted to evaluate TCPP exposures. These studies collected indoor air samples in households, offices, and industries, reporting relatively low concentrations in air (≤0.26 μg/m3).[Citation19,Citation20] More specific to SPF application, several studies have taken area air samples and found TCPP concentrations ranging from 20 μg/m3 to 110 μg/m3.[Citation7,Citation21,Citation22] Bello et al. found personal TCPP air concentrations during SPF application were much higher (geometric mean, GM = 295 μg/m3) than previously reported.[Citation23]
TCPP hand wipe samples have been collected in previous studies, but both sampling methods and concentrations have varied widely. Hand wipe samples taken during a study examining flame retardants in various industries found TCPP concentrations ranged from 0.1–1.3 ng/cm2.[Citation24] Hand wipe samples taken at gymnastic facilities resulted in TCPP concentrations ranging from below the limit of detection (LOD) to 97.4 ng per sample.[Citation25] An additional study analyzed hand wipe samples from children and found TCPP concentrations ranged from below LOD to 530 ng per sample.[Citation26] Bello et al. used a glove dosimeter and reported TCPP GM concentration of 18,800,000 ng/pair of gloves.[Citation23]
Concentrations of bis(1-chloro-2-propyl) phosphate (BCPP), a TCPP metabolite, appear to be higher for SPF workers compared to other populations, as Bello et al.[Citation23] reported a BCPP GM urinary concentration of 2.9 μg/g creatinine (cr). By comparison, the GM urinary concentration of BCPP was 0.200 μg/g cr for the U.S. population and 0.159 μg/g cr for the U.S. adult male population.[Citation27] An occupational study evaluating aircraft technicians found their BCPP concentrations to be between 0.2 and 0.3 μg/g cr.[Citation28]
Compared to the other industries, potential exposure to TCPP is likely much higher for SPF workers due to the high-pressure application method that aerosolizes spray foam components. There is a need for evaluation of hand wipe and personal air exposures during SPF application and to assess the effectiveness of personal protective equipment (PPE). We sought to determine exposure levels to select organophosphate flame retardants among SPF workers by monitoring air, hand wipes, and urine while also evaluating exposure-modifying factors.
Methods
Six SPF companies were recruited within the construction industry. The goal was to recruit 30 workers from three companies, but most companies did not employ 10 workers who installed SPF; therefore, more companies were recruited. A database of spray foam companies was compiled by conducting a Google search with the terms “Spray foam insulation” and “specific city or state.” Overall, 54 companies were selected where half were located within 300 miles of Cincinnati, Ohio. Those companies whose employees participated in the study were selected based on convenience. Candidate companies were contacted about participation in the survey, and a site visit was scheduled.
All workers at each company were asked to participate and given a brochure explaining the study. Workers signed an informed consent, and the study was approved by the National Institute for Occupational Safety and Health (NIOSH) Institutional Review Board. We asked participants demographic and career-related questions to better understand their exposures (). We conducted sampling to evaluate 2 consecutive days of exposure for each participant. The six companies performed residential or industrial insulation work, using seven types of open-cell and eight types of closed-cell foam. Workers were categorized by job assignment as either a helper or sprayer. demonstrates the type of work completed and PPE usage for each classification. If the worker operated the spray foam gun at any point, they were considered a sprayer. Otherwise, helpers did tasks such as cutting foam, moving tarps, and preparing surfaces for SPF application. Sprayers were generally more senior, drove the trucks, and completed paperwork.
Figure 1. Photos of helper (left) and sprayer (right). The helpers cut and bundled freshly sprayed foam, sometimes without coveralls or gloves. The sprayer usually wore partial coverall, gloves, and an air-supplied respirator for protection from overspray.

Table 1. Characteristics of participating spray polyurethane foam workers.
Air and bulk samples were collected and analyzed for TCPP and TDCPP from workers at all companies. Hand wipe samples were collected and analyzed for TCPP from workers at all companies and TDCPP at four of six companies. Urinary biomarkers from workers at all companies were measured for a panel of nine flame retardant metabolites ().
Table 2. Flame retardant metabolites quantified in urine samples.
Bulk samples
Bulk samples of the liquid side B spray foam component and cured foam were collected at each site. Side A was collected initially, but found to be non-detectable for flame retardants tested (N = 2, LOD = 0.10 μg/sample). Side B was collected in glass jars with a PTFE lined lid (SKC 225-8377). Cured foam samples were cut from the area sprayed, and stored in plastic bags. The specific product was documented and safety data sheets (SDS) were collected. The SDS were available for all SPF brands used in this study, and TCPP percentages were listed for over half the brands. Some SDS did not specifically list TCPP percentage, instead classifying the information as “proprietary,” or provided a percentage for “flame retardants.” TDCPP bulk results were evaluated, but results were near or below the LOD (0.10–100 μg/g), so no further analysis was conducted.
Air samples
Workers wore AirChek 5000 (SKC Inc., Eighty Four, PA) personal air samplers on 2 sequential days, operated at sample flow rates of 1 L/min, using an OSHA Versatile Sampler (OVS) with XAD-2 sorbent and glass wool separator. This sampling was conducted for their entire work shift while at the job sites, not including time in transit. Samplers were worn on the collar outside of respirators.
Sampling capture media were compared to determine whether SPF is in an aerosol or vapor state when being sprayed. PocketPumps (SKC Inc., Eighty Four, PA) were worn during the first four site visits by sprayers with a 25-mm GFF (glass fiber filter) cassette followed by an XAD-2 sorbent tube, with pumps operating at a flow rate of 0.2 L/min. The GFF and XAD-2 sampling media were analyzed separately to compare to the performance of the OVS sampling media when analyzing the filter and sorbent components separately. All pumps were calibrated, before and after data collection, to within 10% of the target flow rate using a low or medium flow DryCal Defender (MesaLabs, Lakewood, CO).
Hand wipe samples
On the second day of sampling, pre‐shift and post-shift hand wipe samples were collected from worker’s hands. This method is similar to previous studies examining dermal exposure to flame retardants.[Citation25,Citation29] This hand wipe method was chosen because gloves were worn intermittently during the workday; therefore, any sampling method that measured under gloves would not have been well received. Hands were chosen as the sampling site due to the high potential for exposure during application, specifically to cured foam. Two 3” x 3” sterile gauze pads (Dynarex, Orangeburg, NY) were placed in 120 mL amber glass jars (Fisher Scientific, Pittsburgh, PA). Each jar included 6 mL of 99% HPLC grade isopropanol (Fisher Scientific) using an automatic pipette. The jars were tightly sealed and stored at approximately 5 °C for up to 7 days, until they were used for collection. Samples were collected either at company headquarters or in a construction trailer. During sample collection, participants were instructed to remove gloves, grab one of the gauze pads, and wipe both bare hands (the area from the bend of the wrist to the fingertips) for 30 sec. Then, they were instructed to grab the other wipe and repeat the process. Both gauze pads were placed back into a jar, sealed, and stored at refrigerated temperatures until analyzed. At the post-shift hand wipe collection, workers were asked how many times they washed their hands since pre-shift.
Urine samples
We collected spot urine samples from workers pre-shift on the first day and post-shift on the second day of sampling. For each collection, study participants were given a sterile urine collection cup. Prior to providing a sample, participants were instructed to wash their hands with only water. A minimum 60 mL of urine was requested for each sample. Following collection, samples were kept in coolers with ice for up to 4 hr, aliquoted into 10 mL polypropylene vials, and stored at −20 °C or lower until analyzed. Specific gravity was measured in the field with a Master Refractometer (Master-SUR/Nα, Atago, Tokyo, Japan). The timing of urine collection was chosen to best determine the difference over 2 days to compare to 2 days of air sampling. It was presumed that nonwork exposures during these hours were extremely low. The metabolite of TCPP to be analyzed matched the NHANES study, namely BCPP. Another metabolite, as measured by Bello et al.[Citation23] 1-hydroxy-2-propyl bis(1-chloro-2-propyl) phosphate (BCIPHIPP), was not analyzed in this study.
Exposure-modifying factors
One or more industrial hygienist was at each job site evaluating the workers during both work shifts, except for eight workers who were observed the first day before switching to a different SPF crew on the second day. The industrial hygienist recorded PPE usage and duration of spraying activities. Glove use was categorized as yes, no, or intermittent, as some workers took their gloves on and off for different tasks. Respirator use was categorized as none, half-face air-purifying, full-face air-purifying, or air-supplied. Air-purifying respirators were equipped with either dual organic vapor and P100 filter cartridges or just organic vapor cartridges. Investigators recorded the number of minutes the personal air sampling pumps were running per day, equivalent to the total time that the workers spent on the job site. The time that spraying was observed was recorded. Those workers not observed on the second workday were asked about their glove and respirator use at the end of the work day and spraying time was estimated.
Sample analysis
Air, hand wipe, and bulk samples were analyzed for TCPP and TDCPP at Virginia Institute of Marine Sciences, College of William and Mary. The analysis was completed by ultra-performance liquid chromatography–atmospheric pressure photoionization tandem mass spectrometry, adapted from the method of La Guardia and Hale.[Citation30] Additional analytical information on these analyses can be found in the online supplemental materials.
Organophosphate flame retardant biomarkers and creatinine were quantified in urine samples at the Centers for Disease Control and Prevention as described by Jayatilaka et al.[Citation31] Biomarker urinary concentrations reported here are adjusted for creatinine.[Citation32] See supplemental materials for results adjusted for specific gravity.
Quality control
At least two field blanks for every 10 samples of each type (air or hand wipe) were collected at each company. A surrogate standard deuterated TDCPP (dTDCPP) was used to estimate extraction recoveries, and those recovery values were used to correct TCPP and TDCPP levels. Briefly, dTDCPP was added to all samples at 6,000 ng/sample when analytes of interest were evaluated. dTDCPP levels were also evaluated, and the result was a percentage of the “spiked” amount. All samples were adjusted by the recovery percentage. The average dTDCPP recovery for air sampling media was 85.8%, hand wipe media was 100%, and bulk materials were 109%. Sample concentrations were adjusted for the dTDCPP recovery, media blanks and field blanks.
After pre- and post-shift urine samples were collected from participants, urine blanks (using deionized water) and blind duplicates were prepared (10% of each type). No BCPP blanks were above the LOD, and no BCPP blind duplicates had differences greater than 10%.
Data analysis
Concentrations for air, hand wipe, and urine samples were log transformed. For each worker, air sampling concentrations from the two consecutive sampling days were averaged together using the time-weighted average (TWA) method. Six participants had only one air concentration due to laboratory or sampling error, for example, sampling pumps were sometimes broken while workers performed routine tasks. All TCPP concentrations were above the LOD. LOD divided by square root of two[Citation33] was assigned for one nondetected TDCPP hand wipe sample concentrations for presenting descriptive statistics. Descriptive statistics were presented as frequency (%), mean ± standard deviation (SD) for characteristics of participating workers. In addition, median, GM, geometric standard deviation (GSD), and 25th and 75th percentiles were provided for TCPP hand wipe samples, and BCPP and BDCPP urine samples, broken out by sample collection and job position. A paired t-test was conducted to examine differences between pre- and post-collection, and when comparing similar air sampling capture media concentrations. One-way analysis of variance (ANOVA) and Student’s t-test was utilized to compare concentrations for covariates, glove use, and handwashing, respectively.
A mixed model with company as a random effect was used to account for the statistical correlation among workers from the same company. Specifically, univariate and multivariate analyses were carried out using BCPP urine post-shift concentrations as the dependent variable. Covariates treated as fixed effects, including BCPP urine pre-shift concentrations, TCPP air and hand wipe concentrations, job position, respirator use, hours since last shift, glove use, handwashing, age, body mass index (BMI), and length of working time, were evaluated for these analyses. A multivariate regression model was conducted using covariates that had p-values ≤ 0.1. A stepwise model selection approach was utilized for fitting a model, in which the covariates were entered one at a time into the model until all remaining variables had the smallest Akaike information criterion. All statistical tests were two-sided at the 0.05 significance level. Analyses were performed in SAS (version 9.4, SAS Institute, Cary, NC).
Results
Demographics
Thirty-three SPF workers were consented to participate in this study, but four participants were excluded due to missing urine or hand wipe samples. Data from 29 workers were included in the analysis (). The majority of participants wore gloves during work. Fewer helpers wore a respirator than sprayers, and sprayers wore air-supplied respirators more frequently than other types. Workers were sampled on the job site for an average of 386 min (range 177–640 min) per day and SPF spraying occurred an average of 189 min (range 56–302 min) per day.
Bulk results
Fifteen different SPF products were used by six companies (Supplemental Table S1). TCPP was detected in all bulk samples. TCPP levels were significantly lower (p < 0.001) in closed-cell than open-cell foam. The GM of TCPP in cured foam was 1.68% for closed-cell and 9.23% for open-cell. TDCPP was found at low concentrations (0.01–0.09%) in three of the fifteen bulk samples (Supplemental Table S2).
Air results
When comparing capture media, the XAD sorbent (GM = 1.60 μg/m3) was statistically lower than OVS sorbent (GM = 52.3 μg/m3; p < 0.001). The GFF was found to have significantly higher GM (141 μg/m3), relative to OVS filter (GM = 65.9 μg/m3; p = 0.01). The differences between combined measurements (OVS sorbent and filter compared to XAD sorbent and GFF) were not statistically significant (p = 0.567).
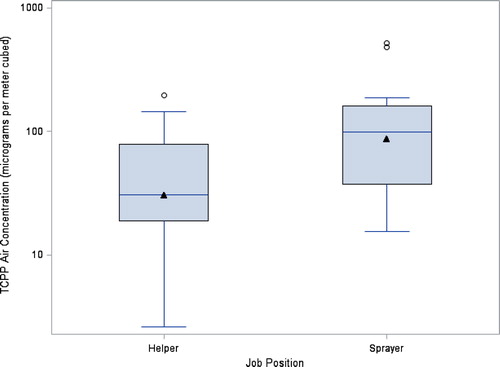
Personal TWA air samples were collected from 29 SPF workers, with at least one full-shift sample per participant (Supplemental Table S3). TCPP GM concentration of personal air samples was 48.5 μg/m3 (range 2.62–519 μg/m3). Sprayer TCPP GM air concentration (87.1 μg/m3) was significantly higher than helper concentration (30.2 μg/m3; p = 0.025) (). Note that personal TCPP air concentration was significantly associated with both the covariates, job position, and pump minutes. TDCPP air concentrations were often (74%) below the LOD (15.6, 2, or 1 ng/sample, improving with each set) and corresponding concentrations ranged from nondetectable to 0.317 μg/m3.
Figure 2. TCPP air concentrations by job position (N = 29). The box represents the interquartile range, the line in each box represents the median, and the triangle represents the GM. The upper whisker represents the far upper fence 1.5 IQR above the 75th percentile, the lower whisker represents the lower fence 1.5 IQR below the 25th percentile, and the circles represent outliers.
Hand wipe results
Fifty-eight hand wipe samples were analyzed (). Workers were found to have significantly higher post-shift TCPP hand wipe concentration (p = 0.004). Specifically, helpers were more likely to have greater post-shift hand wipe concentrations compared to pre-shift (p < 0.001), whereas no significant association between pre- and post-shift hand wipe concentrations for sprayer was observed (p = 0.512). In addition, there was not a statistically significant difference in post-shift hand wipe TCPP concentration for glove use or hand washing. We note that covariates, including job position, minutes sprayed, pump minutes, and glove usage, were tested for the multivariate analysis using post-shift TCPP hand wipe concentration as the dependent variable, but none were significantly related. Results of TDCPP hand wipe concentrations for job position, glove use, and hand washing are shown in Supplemental Table S4.
Table 3. TCPP hand wipe concentrations* (ng/sample) and comparisons.
Urine results
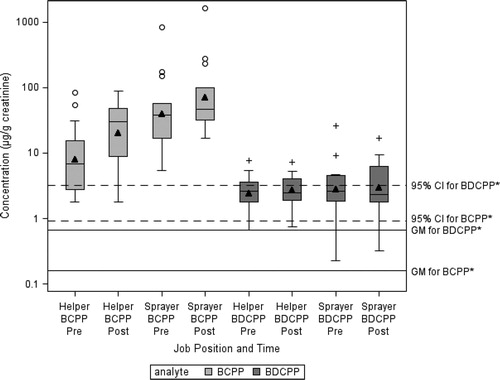
BCPP and Bis(1,3-dichloro-2-propyl) Phosphate (BDCPP) were detected in all samples (). BCPP post-shift urine concentration was significantly higher than pre-shift concentration for sprayers (p = 0.013) and helpers (p = 0.009). Sprayers had higher BCPP post-shift urine concentrations compared to helpers (p < 0.001). Although BDCPP post-shift urine concentration for sprayers and helpers were higher than pre-shift urine concentration for sprayers and helpers, the differences were not statistically significant.
Table 4. Urine sampling concentrations* using paired t-test (μg/g cr).
Univariate analysis results with post-shift BCPP urine concentration as the dependent variable are shown in . Sprayers were more likely to have greater BCPP post-shift urine concentrations than helpers. Workers wearing supplied air respirator had significantly higher urinary post-shift BCPP concentrations relative to those not wearing a respirator. Furthermore, increased post-shift BCPP urine concentration were significantly associated with increased pre-shift BCPP urine, TCPP TWA air, and pre-shift TCPP hand wipe concentrations, respectively, and decreased hours since last shift. On multivariate analysis, TCPP TWA air concentration, pre-shift hand wipe concentration, post-shift hand wipe concentration and job position were found to have notable impacts on the dependent variable, post-shift BCPP urine concentration (). We also found that covariates significantly related to pre-shift urine BCPP concentration were job position and last shift worked (both p < 0.001).
Table 5. Univariate analysis results using a mixed model with company as a random effect.
Table 6. Multivariate analysis results using a mixed model with company as a random effect.
Urinary concentrations from nine flame retardant from SPF workers were compared to the U.S. general population for men 18 and older (Supplemental Table S5). Of the nine biomarkers, only BCPP and BDCPP concentrations in spray foam workers were significantly higher (p < 0.001) than the concentrations from the U.S. general population for men 18 and older (). Supplemental Tables S6 and S7 show urine concentrations that were adjusted for specific gravity.
Figure 3. BCPP and BDCPP creatinine-adjusted urine concentrations by position and time compared to the adult male general population (N = 29). The box represents the interquartile range, the line in each box represents the median, and the black triangle represents the GM. The upper whisker represents the far upper fence 1.5 IQR above 75th percentile, the lower whisker represents the lower fence 1.5 IQR below the 25th percentile, and the circles represent outliers. *The GM and 95th% CI for BCPP and BDCPP were general population averages calculated using the National Health and Nutrition Examination Survey 2013–2014 (men above age 18).
Discussion
To our knowledge, studies evaluating the bulk composition of SPF primarily focused on isocyanates from side A or foam found in furniture.[Citation34] This study measured the amount of TCPP in many common spray foam products on the market. TCPP bulk analysis percentages were within or below percentages listed in SDS. As expected, open-cell foam we measured had significantly higher percentages of TCPP by weight compared to closed-cell foam.
Comparison of the air concentrations from the filter and sorbent air sampling media indicated TCPP was collected in the aerosol phase. When sampling using the filter (GFF) and sorbent (XAD) in series, it became clear that TCPP was primarily collected on the GFF, whereas when sampling with the OVS filter and sorbent, it is likely that TCPP migrated from the filter to the sorbent during storage. The SPF was sprayed from a nozzle at 1250 to 1900 psi producing aerosol droplets in the immediate area. Although other chemicals could be in the gas phase at the time of spraying, these data show that TCPP was in an aerosol phase. In an internal NIOSH study, spiked glass fiber filter punches with 161 μg TCPP were placed against the filter in an OVS tube and stored for 32 days. Analysis of the samples found the mean level of TCPP migration to the front and back sorbent sections was 85.4% (relative standard deviation (RSD) 1.1%).[Citation35]
The air concentrations in the current study (GM = 48.5 μg/m3, range = 2.62–519 μg/m3) were considerably less than reported in Bello et al.[Citation23] (GM = 295 μg/m3, range = 9.5–1,850 μg/m3). This difference is likely due to the fact that Bello et al.[Citation23] only measured air for the duration of certain tasks, 15–176 min per sample, likely the highest air concentrations of the day. For the current study, we measured air during the workers’ shift (mean = 340 min, range 177–640 min), likely capturing the workers’ entire daily exposure, including other tasks like set-up and clean-up. Overall, TCPP air concentrations for SPF workers are orders of magnitude higher than for other occupations.[Citation19,Citation20] Additionally, job position is a strong predictor of TCPP exposure through inhalation, as sprayers had significantly higher TCPP air concentrations compared to helpers. This finding was expected because sprayers were closer to the application of SPF than helpers.
Results suggest the most protective respirators were selected by the company supervisors or workers for situations with the highest potential for inhalation exposure. Because samplers were worn outside respirators, air concentrations are not reflective of the amount of TCPP workers actually inhaled. Helpers were more likely to wear no respirator or a less protective respirator, while sprayers were more likely to wear more protective respirators. Workers wearing no respirator or a half-face air-purifying respirator generally had lower TCPP air concentrations compared to workers with a full-face air-purifying respirator and air-supplied. Urinary post-shift BCPP concentrations were statistically lower (p = 0.003) among those wearing no respirator (GM = 13.0 µg/g cr) compared to air-supplied (GM = 61.1 µg/g cr). Post BCPP concentrations for those wearing half-face air-purifying (GM = 48.2 µg/g cr) and full-face air-purifying respirators (GM = 38.8 µg/g cr) were also lower than those wearing air-supplied, though the difference was not statistically significant.
Helpers were more likely to be dermally exposed to TCPP than sprayers. When considering TCPP in hand wipes, pre-shift samples were significantly lower than post-shift samples for all workers in this study. When comparing by job position, helper TCPP hand wipe pre-shift samples were significantly lower than post-shift samples. Helpers were less likely to wear gloves and came in direct contact with cured foam more often. Direct contact with cured foam is believed to be a major source of exposure.
The TCPP hand wipe concentrations we observed are higher compared to other studies. Using a similar method to that used in this study, Stapleton et al. sampled children’s TCPP concentrations on hands[Citation26] and observed a GM of 31.3 ng/hand wipe. Liu et al sampled students and office workers in China, and found a GM of 3,100 ng/m2 with a range of < LOD – 62,900 ng/m2 [Citation35] Our sampling technique consisted of the workers wiping over bare hands several times, rather than twice as in Stapleton et al.[Citation34] and Liu et al.,[Citation36] possibly accounting for the differences. Bello et al. assessed dermal exposure through the use of a glove dosimeter and found concentrations several orders of magnitude higher than ours, with a GM of 18.8 million ng/pair.[Citation23] The differences in sampling technique likely played a role in observed concentrations.
We observed relatively high concentrations for preshift hand wipe samples (). Although samples were taken at the company headquarters before and after driving to and from the job site, company headquarters could have had surface contamination of TCPP from previous insulation jobs. Additionally, workers may have taken home residual contamination on their clothes and automobile or reworn the same clothes from previous work days, raising their pre-shift hand wipe concentration.
GM concentrations of urinary BCPP and BDCPP in SPF workers were significantly higher than the U.S. adult male general population.[Citation27] Both sprayers and helpers had a significant increase in BCPP concentrations from Pre-shift Day 1 to Post-shift Day 2, which was not true for BDCPP. Our urinary concentrations for BDCPP (2.69 μg/g cr) were similar to those found in Bello et al. (2.5 μg/g cr), but our urinary concentrations for BCPP (23.8 μg/g cr) were nearly ten times higher[Citation23] (GM = 2.9 μg/g cr); these differences could be related to increased respirator usage or decreased time spraying in the Bello et al. study.[Citation23]
TCPP air concentration, TCPP pre-shift and post-shift hand wipe concentration, and job position were significant predictors of BCPP post-shift urinary concentration (). TCPP hand wipes were a slightly better predictor than air for post-shift urine BCPP concentrations, but both were strongly and significantly associated. Similar to our findings, Bello et al.[Citation23] found glove dosimeters to be the better predictor for BCPP concentrations than air concentrations. When considering job position, sprayers had significantly higher post-shift urine BCPP concentrations compared to helpers.
These results demonstrate spray foam workers are occupationally exposed to TCPP during SPF application. Overall, BCPP urinary concentrations were higher than previously reported in other studies.[Citation23,Citation27,Citation37] SPF workers’ pre-shift BCPP urinary concentrations were greater than the 95th percentile level of the general population, demonstrating that BCPP is present in the worker’s urine every day before starting their shift. Although no half-life has been established for metabolites of TCPP, it has been previously assumed concentrations of organophosphates in urine samples were likely from exposures occurring during the past 24 hr.[Citation23,Citation38] Pre-shift BCPP concentrations were significantly related to job position and hours since last shift; therefore, participants who worked most recently and who worked as sprayers had higher baseline concentrations of BCPP.
The air exposure pathway is of greater concern for sprayers, as seen by their higher urinary BCPP concentrations (both pre- and post-shift). The dermal exposure pathway, on the other hand, was relevant for both sprayers and helpers. Both jobs had an opportunity for dermal exposure and could benefit from improved use of gloves and increased hand washing.
This study had a few limitations. Urine samples were collected over 2 days instead of at the beginning and end of each day, making comparisons to other studies difficult. In addition, collecting more urine samples for each worker would have allowed us to gain more knowledge on metabolism and optimal sampling time for BCPP. However, this study design still allowed us to report pre- and post-shift urinary changes to identify occupational exposure to TCPP. Also, we assessed urinary concentrations of BCPP but not the second metabolite of TCPP, BCIPHIPP, recently reported in Bello et al.[Citation23] The second metabolite is detected in higher frequencies in most studies and could have given us more information about excretion characteristics. However, BCPP was detected in all samples because of its use in this occupation and was therefore useful for comparisons. Other limitations include the lack of toxicokinetic information available for TCPP, specifically on the dermal uptake mechanism and clearance through the body. Future studies should explore the toxicokinetics of TCPP, further examining the uptake of TCPP through dermal and inhalation exposures. The identification of a half-life for the metabolites of TCPP would be useful for better understanding of these exposures.
Efforts should be made to ensure all workers on-site during application of SPF wear respiratory protection, as several helpers and one sprayer wore no respiratory protection during application. Others wore half-face air-purifying respirators, substandard protection for exposures of this magnitude. All SPF workers, including helpers, should more consistently wear coveralls and gloves to reduce the potential for dermal exposure. Although the effects of TCPP in humans are not well established, several harmful substances including isocyanates, di-isocyanates, amine catalysts, and blowing agents are released during application, so efforts should be made to reduce overall exposure during SPF application.
Conclusions
Findings from this study demonstrate SPF workers are occupationally exposed to TCPP during application. SPF workers have high air and hand wipe TCPP concentrations that are correlated with high urinary BCPP concentrations. Urinary BCPP concentrations were two orders of magnitude above the U.S. adult male population and remain elevated even over weekends. Some SPF companies did not choose the most protective respirators for their workers, and some workers wore no respirators during application. Other workers did not wear gloves or coveralls during application. These exposures show that SPF companies need to improve their use of air-supplied respirators, coveralls, and gloves, especially considering the concurrent isocyanates exposures.
Supplemental Material
Download PDF (179.4 KB)Acknowledgments
We would like to thank Chrissy Toennis, Deborah Sammons, Shirley Robertson, and Barb McKenzie for assistance in collecting, processing, and submitting urine samples for analysis. We thank Kenneth Fent, Kelsey Babik, Melissa Seaton, and Ken Sparks for assistance in collecting, processing, and submitting air and hand wipe samples for analysis. We thank Jen Roberts, Fariba Nourian, and Jim Arnold for their assistance with understanding of environmental sample results. We thank Paula Restrepo and Zack Davis for assistance in analyzing the urine samples. We thank Steve Bertke for statistical advice. Most of all, we thank the workers for participating in the study. This study was approved by the Institutional Review Board at NIOSH. This paper is contribution No. 3826 of the Virginia Institute of Marine Science, college of William & Mary.
Additional information
Funding
References
- Environmental Protection Agency (EPA): U.S., Flame Retardants Used in Flexible Polyurethane Foam: An Alternatives Assessment Update. Environmental Protection Agency, 2015.
- National Center for Biotechnology Information: PubChem Compound Database, 2005.
- World Health Organization (WHO): Flame Retardants: Tris(Chloropropyl) Phosphate and Tris(2-Chloroethyl) Phosphate, WHO (ed.). Geneva: World Health Organization, 1998.
- Van Der Veen, I., and J. de Boer: Phosphorus flame retardants: Properties, production, environmental occurrence, toxicity and analysis. Chemosphere. 88(10):1119–1153 (2012).
- Weil, E., and S. Levchik: Commercial flame retardancy of polyurethanes. J. Fire Sci. 22(3):183–210 (2004).
- Poppendieck, D., M. Gong, and L. Lawson: "Lessons Learned from Spray Polyurethane Foam Emission Testing Using Micro-chambers." The 59th Annual Polyurethanes Technical Conference, American Chemistry Council, Baltimore, MD., 2016.
- Wood, R: Center for the Polyurethanes Industry summary of unpublished industrial hygiene studies related to the evaluation of emissions of spray polyruetahne foam insulation. J. Occup. Environ. Hyg. 14(9):681–693 (2017).
- State of California: Chemicals Known to the State to Cause Cancer or Reproductive Toxicity. Environmental Protection Agency (Proposition 65 List of Chemicals), December 2017.
- EU Risk Assessment: European Union Risk Assessment Report Tris(2-Chloro-1-Methylethyl) Phosphate (TCPP). Ireland (lead) and United Kingdom, 2008.
- Farhat, A., D. Crump, S. Chiu, et al.: In ovo effects of two organophosphate flame retardants - TCPP and TDCPP - on pipping success, development, mRNA expression, and thyroid hormone levels in chicken embryos. Toxicol. Sci. 134(1):92–102 (2013).
- An, J., J. Hu, Y. Shang, Y. Zhong, X. Zhang, and Z. Yu: The cytotoxicity of organophosphate flame retardants on HepG2, A549 and Caco-2 cells. J. Environ. Sci. Health. 51(11):980–988 (2016).
- Li, F., L. Wang, C. Ji, H. Wu, J. Zhao, and J. Tang: Toxicological effects of tris(2-chloropropyl) phosphate in human hepatic cells. Chemosphere. 187:88–96 (2017).
- Carignan, C., L. Minquez-Alarcon, C. Butt, et al.: Urinary concentrations of organophosphate flame retardant metabolites and pregnancy outcomes among women undergoing in vitro fertilization. Environ. Health Perspect. 125(8): 087018-1-087018-8 (2017).
- Mohamed, A.E., G. Pawar, and K.H. Harada: Human dermal absorption of chlorinated organophosphate flame retardants: Implications for human exposure. Toxicol. Appl. Pharmacol. 291:28–37 (2016).
- Schindler, B.K., T. Weiss, A. Schutze, et al.: Occupational exposure of air crews to tricresyl phosphate isomers and organophosphate flame retardants after fume events. Arch. Toxicol. 87(4):645–648 (2013).
- Van den Eede, N., G. Tomy, F. Tao, et al.: Kinetics of tris (1-chloro-2-propyl) phosphate (TCIPP) metabolism in human liver microsomes and serum. Chemosphere. 144:1299–1305 (2016).
- Minegishi, K.I., H. Kurebayashi, S. Nambaru, et al.: Comparative studies on absorption, distribution, and excretion of flame retardants halogenated alkyl phosphate in rats. Eisei Kagaku 34(2):102–114 (1988).
- Greaves, A., G. Su, and R. Letcher: Environmentally relevant organophosphate triesters in herring gulls. Toxicol. Appl. Pharmacol. 308:59–65 (2016).
- Carlsson, H.: Organophosphate ester flame retardants and plasticizers in the indoor environment: Analytical methodology and occurrence. Environ. Sci. Technol. 31:2931–2936 (1997).
- Hartmann, P., D. Burgi, and W. Giger: Organophosphate flame retardants and plasticizers in indoor air. Chemosphere. 57(8):781–787 (2004).
- U.S. Department of Health and Human Services: Spray Polyurethane Foam Chemical Exposures during Spray Application, All About Kids, Crestwood, KY by Marlow, D., J. DeCapite, and A. Garcia (EPHB Report No. 005-163). National Institute for Occupational Safety and Health, December 2014.
- U.S. Department of Health and Human Services: Spray Polyurethane Foam Chemical Exposures during Spray Application by Marlow, D., J. DeCapite (EPHB Report No. 005-166) National Institute for Occupational Safety and Health, April 2017.
- Bello, A., C. Carignan, Y. Xue, H. Stapleton, and D. Bello: Exposure to organophosphate flame retardants in spray polyurethane foam applicators: Role of dermal exposure. Environ. Int. 113:55–65 (2018).
- Makinen, M.S., M. Makinen, J. Koistinen, et al.: Respiratory and dermal exposure to organophosphorus flame retardants and tetrabromobisphenol A at five work environments. Environ. Sci. Technol. 43(3):941–947 (2009).
- Carignan, C.C., W. Heiger-Bernays, M. McClean, et al.: Flame retardant exposure among collegiate United States gymnasts. Environ. Sci. Technol. 47(23):13848–13856 (2013).
- Stapleton, H.M., J. Misenheimer, K. Hoffman, and T. Webster: Flame retardant associations between children's handwipes and house dust. Chemosphere. 116:54–60 (2014).
- Ospina, M., N. Jayatilaka, L. Wong, P. Restrepo, and A. Calafat: Exposure to organophosphate flame retardant chemicals in the U.S. general population: Data from the 2013-2014 National Health and Nutrition Examination Survey. Environ. Int. 110:32–41 (2018).
- Schindler, B.K., S. Koslitz, T. Weiss, et al.: Exposure of aircraft maintenance technicians to organophosphates from hydraulic fluids and turbine oils: A pilot study. Int. J. Hyg. Environ. Health. 217(1):34–37 (2014).
- Ceballos, D., K. Broadwater, E. Page, G. Croteau, and M. LaGuardia: Occupational exposure to polybrominated diphenyl ethers (PBDEs) and other flame retardant foam additives at gymnastics studios: Before, during and after the replacement of pit foam with PBDE-free foams. Environ. Int. 116:1–9 (2018).
- La Guardia, M.J., and R. Hale: Halogenated flame-retardant concentrations in settled dust, respirable and inhalable particulates and polyurethane foam at gymnastic training facilities and residences. Environ. Int. 79:106–114 (2015).
- Jayatilaka, N.K., P. Restrepo, L. Williams, et al: Quantification of three chlorinated dialkyl phosphates, diphenyl phosphate, 2,3,4,5-tetrabromobenzoic acid, and four other organophosphates in human urine by solid phase extraction-high performance liquid chromatography-tandem mass spectrometry. Anal. Bioanal. Chem. 409(5):1323–1332 (2017).
- Boeniger, M.F., L. Lowry, and J. Rosenberg: Interpretation of urine results used to assess chemical exposure with emphasis on creatinine adjustments: A review. Am. Ind. Hyg. Assoc. J. 54(10):615–627 (1993).
- Hornung, R., and L. D. Reed: Estimation of average concentration in the presence of nondetectable values. Appl. Occup. Environ. Hyg. 5(1):46–51 (1990).
- Stapleton, H.M., S. Klosterhaus, S. Eagle, et al.: Detection of organophosphate flame retardants in furniture foam and U.S. house dust. Environ. Sci. Technol. 43(19):7490–7495 (2009).
- Streicher, R., J. Arnlod, and F. Nourian: Unpublished data - TCPP Storage and Migration Study. National Institute for Occupational Safety and Health, 2016.
- Liu, X., G. Yu, Z. Cao, et al.: Occurrence of organophosphorus flame retardants on skin wipes: Insight into human exposure from dermal absorption. Environ. Int. 98:113–119 (2017).
- Butt, C.M., J. Congleton, K. Hoffman, M. Fang, and H. Stapleton: Metabolites of organophosphate flame retardants and 2-ethylhexyl tetrabromobenzoate in urine from paired mothers and toddlers. Environ. Sci. Technol. 48(17):10432–10438. (2014).
- Van den Eede, N., A. Heffernan, L. Aylward, et al.: Age as a determinant of phosphate flame retardant exposure of the Australian population and identification of novel urinary PFR metabolites. Environ. Int. 74:1–8 (2015).
