Abstract
The assigned protection factor (APF) for quarter-facepiece respirators is currently 5, based on fit test data from the 1970s with models no longer commercially available. The goal of this project was to evaluate the respirator fit capability of a NIOSH-approved N95 quarter-facepiece elastomeric respirator with a gel-based facial seal design (Envo Mask by Sleepnet Corporation). Human subjects were recruited from healthcare and the general population to satisfy a 25-member NIOSH bivariate panel. Subjects were fit tested with a fast fit protocol using a TSI Portacount Model 8038 in the N95 mode. Second-by-second measures of fit were then collected while subjects performed a 30-min series of simulated healthcare activities. Subjects completed a short comfort questionnaire. The median (5th, 95th percentile) fit factor was 188 (48, 201). Simulated workplace protection factors (SWPFs) had a median (5th, 95th percentile) of 181 (94, 199) (data truncated at 200) and 570 (153, 1508) (non-truncated data). Subjects ranked inhalation and exhalation as “easy” with average scores of 5.0/6.0 and 5.2/6.0, respectively. The facepiece was ranked between slightly comfortable and comfortable (4.8/6.0) and the harness as comfortable (5.0/6.0). Most users agreed (5.2/6.0) that the mask was stable on their faces. The 5th percentile SWPF of 95 supports an APF of at least 10 for this quarter-facepiece elastomeric respirator, similar to the APF for half-facepiece respirators. This study supports increasing the APF for quarter-facepiece respirators, a class that has been largely ignored by manufacturers for the past 40 years. A lightweight, low profile, reusable quarter-facepiece respirator is an effective option for healthcare and other worker protection during a pandemic and similar situations.
Introduction
Quarter-facepiece respirators, which cover just the mouth and nose and do not extend below the chin, have an assigned protection factor (APF) of 5 and are expected to reduce the external concentration of hazardous contaminants for the wearer by five times (OSHA Citation2006). Quarter-facepiece elastomeric respirators were some of the earlier models worn by workers in dusty environments, such as mines, but have been largely supplanted by half-facepiece designs (disposable and reusable). The Envo Mask respirator by Sleepnet Corporation (model 73950) is currently the only quarter-facepiece elastomeric respirator approved by the National Institute for Occupational Safety and Health (NIOSH) (approval number 9228).
The preamble to the final rule adding APFs to the Occupational Safety and Health Administration (OSHA) Respiratory Protection Standard indicates that OSHA first proposed an APF of 10 for quarter-facepiece respirators (OSHA Citation2006). OSHA apparently relied on the 1992 ANSI Z88.2 standard, which proposed an APF of 10 for quarter- and half-facepiece respirators (disposable and reusable), although supporting data were only available for half-facepiece respirators (Nelson Citation1995). OSHA received comments on the quarter-facepiece APF; recommendations ranged from support for an APF of 10, lowering the value to 5, disallowing quarter-facepiece respirators altogether, and waiting for more studies.
Those in favor of lowering the APF to 5 noted that the only relevant studies were those of Hyatt (Citation1976) at Los Alamos Scientific Laboratories. Hyatt studied quarter-facepiece respirators with high efficiency filters and found that 100% of a 16 subject (males only) panel achieved a fit factor (FF) greater than 10 on four of five quarter-facepiece respirator models and 94% of subjects achieved a FF greater than 10 on the remaining model. The passing rates were much lower for the same respirators with less efficient dust filters, which would include penetration through the filter as well as around the facepiece. Hyatt relied on these latter data in proposing an APF of 5 for quarter-facepiece respirators.
Commenters in favor of an APF of 10 for quarter-facepiece respirators drew comparisons to the similarity in structural characteristics of quarter- and half-facepiece respirators. One commenter noted similarities in leakage routes for both designs, i.e., through the filter or around the facepiece, which would be captured in a similar manner by fit testing. Others noted, as described above, that Hyatt did not adequately control for filter leakage in tests with dust filters.
Those in favor of an APF of 5 noted that no workplace protection factor (WPF), simulated workplace protection factor (SWPF), or similar studies had been conducted on quarter-facepiece respirators. Hyatt’s research involved only laboratory-based fit testing and was not representative of respirator performance during real or simulated work. Some argued that a quarter-facepiece design would be more likely to move on the face due to head movement or perspiration than a half-facepiece respirator.
Ultimately, OSHA promulgated the final standard with an APF of 5 for quarter-facepiece respirators based on the Hyatt data with lower efficiency dust filters (OSHA Citation2006).
Studies of protection factors for particulate respirators are difficult to perform in real-world workplace settings, although these are preferred to laboratory-based studies of fit that utilize a small set of standardized face, head and body movements. Studies of fit using simulated job tasks are easier to perform than workplace-based studies and may be more representative of real-world settings than traditional fit testing. A simulated workplace protection factor study offers the best of both worlds, allowing more careful control of experimental variables while also providing insight into the impact of typical head, face, and body movements using representative job tasks (Sietsema and Brosseau Citation2018). OSHA (Citation2006) considered WPF and SWPF studies in its determination of APFs for other respirator classes.
The goal of this research is to determine the SWPF of a NIOSH-approved quarter-facepiece elastomeric respirator equipped with an N95 filter by measuring fit on a NIOSH bivariate panel of human subjects performing simulated healthcare tasks. We hypothesized that based on its innovative facepiece design the performance of this quarter-facepiece respirator would be similar to that of half-facepiece respirators, which have an APF of 10.
Methods
Overview of research design
A NIOSH bivariate panel of subjects was recruited to perform an experimental protocol consisting of two OSHA approved modified ambient aerosol condensation nuclei counter (CNC) protocols followed by a simulated workplace protection factor (SWPF) protocol. After the SWPF protocol subjects completed a comfort questionnaire.
Recruitment and selection of subjects
Subjects were first recruited from the healthcare worker population at Rush University Hospital via posted signs, emails, handouts, and in-person presentations at staff meetings. Recruitment was expanded in the last month of the study to include members of the general population. Inclusion criteria included being able to speak and understand English, in general good health, between the ages of 18 and 65, clean shaven, and able to avoid smoking and eating for 30 min prior to the scheduled appointment.
During initial recruitment efforts at Rush University, only subjects medically cleared to wear a respirator were included in the study. During secondary recruitment subjects were screened by phone with a short medical evaluation survey. The survey confirmed subjects were in overall good health, did not have any preexisting health conditions that would make wearing a respirator difficult, did not experience claustrophobia, and would be able to comfortably perform all the research activities. The study was approved by the University of Illinois at Chicago Institutional Review Board Protocol #2021-0626.
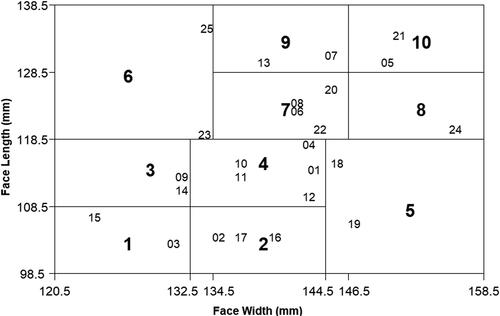
NIOSH bivariate panel
Subjects were recruited to fill a 25-member NIOSH bivariate panel as described in ASTM F3407-20 Standard Test Method for Respirator Fit Capability for Negative-Pressure Half-Facepiece Particulate Respirators (ASTM Citation2020). Face length (menton sellion) and width (bizygomatic breadth) were measured for each subject using sliding and spreading calipers, respectively (Seritex, East Rutherford, NJ, Models 104 and 106, respectively) to determine their corresponding NIOSH bivariate panel cell. If the cell was already filled, the subject was thanked for their time and excused from further testing.
Respirator description
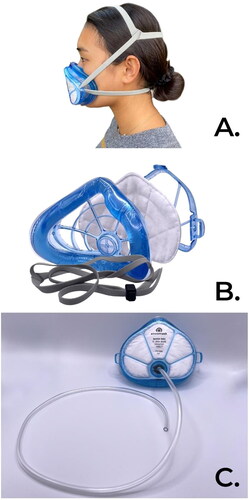
The Envo Mask quarter-facepiece respirator (NIOSH approval number 9228) consists of a plastic body attached to a gel-filled cushion that rests on the face over the nose and between the mouth and chin. A flat N95 filter is held in place with a plastic cover that snaps into place. The respirator is available with and without an exhalation valve. For the purposes of this study, respirators were provided by the manufacturer with a built-in sampling probe in place of the exhalation valve ().
Over 50% of Envo Mask customers are healthcare, public safety, and affiliate health-related businesses. Since March 2020 these businesses have purchased more than 500,000 units.
Fit testing
Two fit tests were conducted following the OSHA ambient aerosol condensation nuclei counter quantitative fast fit test protocol using a Portacount Respirator Fit Tester (TSI, Inc., Shoreview, MN, Model 8038), which collects a 20-sec ambient sample followed by a 30-sec in-mask sample for each of four exercises (bending over, talking, moving head side to side, and moving head up and down) followed by a final 9-sec ambient sample.
The fast fit test protocols were developed by Richardson et al. (Citation2013, Citation2014a, Citation2014b) following the American National Standard for Respirator Fit Testing Methods, ANSI/AIHA Z88.10 – 2010, Annex A2 – Criteria for Evaluating New Fit Test Methods (ANSI Citation2010). OSHA approved their addition to Appendix A Fit Testing Procedures of its Respiratory Protection Standard (OSHA Citation2019).
The first fit test was conducted in N95 mode followed by a second fit test in N99 mode (the latter measures total inward penetration through the filter and around the facepiece). The respirator was not moved or altered between the two fit tests.
Simulated healthcare tasks
Without adjusting the respirator, subjects then completed a simulated workplace protection factor (SWPF) protocol (Sietsema and Brosseau Citation2018) involving 30 min of simulated healthcare work activities. A single set of activities involved taking vitals (120 sec), changing a hospital bed sheet (120 sec), and performing cardiopulmonary resuscitation (CPR) (90 sec); each of these is alternated with 60 sec of normal breathing. Each set was performed three times ().
Table 1. Simulated workplace activities and sampling time.
During the vitals activity, subjects were instructed to simulate a series of tasks on a manikin, which included measuring temperature, blood pressure, pulse, and oxygen level, hanging an IV bag, and inputting information into a portable computer. Bed sheet making involved rolling the manikin on its side, rolling the sheet lengthwise toward the middle of the bed, placing a clean sheet on the mattress and moving it toward the old sheet, rolling the patient over the mound in the middle onto the clean sheet, and rolling the original sheet off the bed and new sheet to complete the sheet changing. CPR was conducted by performing chest compressions on the manikin for approximately 30 sec followed by bending over the manikin and placing first one ear and then turning and placing the other ear over the manikin’s mouth to simulate listening for breathing.
The Portacount instrument was in N95 mode throughout the SWPF protocol. Specialty software (developed by TSI Inc., Shoreview, MN and not commercially available) was used to collect second-by-second concentrations from the instrument. Every 3 min the software switches to collect ambient particle concentrations for 15 sec during a normal breathing period. At least 20 min prior to the beginning of each subject’s experiment, an aerosol generator (TSI, Inc., Shoreview, MN, Model 8026) was started to increase ambient particle counts in the room.
Comfort assessment
Each subject was asked to complete a short questionnaire assessing respirator comfort. On a six-point scale with higher values indicating a more positive response, subjects were asked to rate how easy it was to breathe through the respirator, comfort of the respirator facepiece and harness, stability of the respirator on the face, and whether the respirator was stable on the face during wear.
Data analysis
Fit factors (FF) for the two fit tests in N95 and N99 mode were computed by the Portacount Software, FitPro+ (TSI Inc., Shoreview, MN), which calculates an individual FF for each of the four exercises and the harmonic mean for an overall FF. In N95 mode the software truncates all FF greater than 200 as 200+; for data analysis purposes, this was recorded as 201.
The proprietary software calculates a SWPF by dividing the most recent ambient concentration by the inside-mask aerosol concentration. The software truncates SWPFs greater than 200 as 201.
A second-by-second SWPF measurement was also calculated in Microsoft Excel by dividing the ambient concentration measured just prior to a simulated activity by the mask concentration measured each second during the activity.
Using both the truncated values and those calculated by spreadsheet, an activity SWPF was determined for each healthcare task activity by taking the arithmetic mean of the second-by-second SWPFs obtained throughout the duration of that activity. An overall SWPF was calculated by taking the harmonic mean of the nine healthcare activity SWPFs and the nine normal breathing period SWPFs ().
Fit factors measured in the N95 mode and SWPFs using truncated values were not normally or lognormally distributed. Non-truncated SWPFs were lognormally distributed. All data were summarized using the median, 5th, and 95th percentile. Overall, FFs measured in the N95 mode (which are truncated at 200) were compared to overall truncated SWPFs using Spearman’s sign rank correlation. Comfort assessment data were scored 0–6 for each question and summary statistics were calculated. Fit factors measured in the N99 mode will be described in a separate publication.
Results
Subjects
Ninety subjects expressed interest in participating in the study, 32 completed the study, 21 were excused because their face size was not needed, the remainder were lost to follow-up. Of the 32 subjects who completed the study, data from four subjects were not used in the data analysis: one did not don the respirator correctly and failed the fit tests, a respirator defect was identified for two subjects, and the instrument exhibited measurement errors for the fourth subject. Three of the 32 participants had facial dimensions outside of the NIOSH bivariate panel and were not included in the final data analysis. Data from 25 subjects (11 female; 14 male) are reported here.
Requirements for the NIOSH bivariate panel were largely satisfied, with the exceptions of one subject (rather than two) in cell 8 and three (rather than two) subjects in cell 2 (). None of the 25 subjects were regular Envo Mask respirator users. Eight subjects reported wearing a respirator for more than 10 years, three subjects had 6 to 10 years of respirator experience, eight had been a respirator user for 1 to 5 years, and six had been a respirator user for less than 1 year. Thirteen subjects identified as White, three as Black or African American, two as White/Asian, one Hispanic, four Hispanic/White and two Asian.
Fit factors and simulated workplace protection factors
The median ambient concentration across all subjects was 130 when measured in N95 mode. Fit factors measured in the N95 mode ranged from 48 to 201 with a median of 188. The 5th percentile was 48 and the 95th percentile was 201. Truncated SWPFs ranged from 94 to 199 with a median of 181. The 5th percentile was 94 and the 95th percentile was 199. Non-truncated SWPFs ranged from 126 to 4330 with a median of 570. The 5th percentile was 153 and the 95th percentile was 1,508 (; ). The Spearman’s correlation coefficient between N95 FFs (truncated) and truncated SWPFs was 0.55 ().
Figure 3. Comparison of fit factors (FF95) and overall truncated simulated workplace protection factors (SWPF). Dotted line indicates a 1 to 1 correlation.
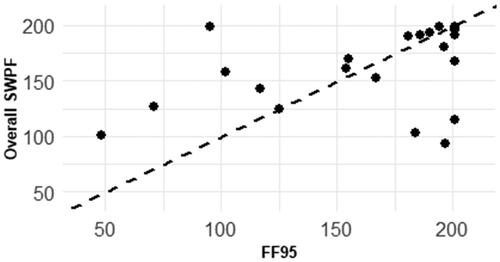
Table 2. Summary statistics – it actor (FF) in N95 mode, simulated sorkplace protection factor (SWPF) with truncated and non-truncated data.
The three subjects with face sizes near but just outside cell numbers 1, 5, and 8 had N95 FFs of 107, 201, and 65 and SWPFs (truncated) of 78, 183, and 38, respectively. Including these subjects would have resulted in a 5th percentile FF and SWPF of 48 and 38, respectively.
Comfort assessment
On average, subjects ranked inhalation as “easy” with an average score of 5.0/6.0. The average exhalation score was slightly higher: 5.2/6.0. Users ranked the facepiece comfort between slightly comfortable and comfortable (4.8/6.0) and harness comfort as comfortable (5.0/6.0). Most users agreed (5.2/6.0) that “The mask was stable on my face and did not slip during wear.”
Discussion
An assigned protection factor of 10 indicates that at least 95% of respirator wearers would achieve a protection factor of at least 10 performing their work tasks. This study demonstrated, in a simulated work environment, that 95% of Envo Mask wearers achieved an SWPF > 94 (truncated data) or > 153 (non-truncated data). Median SWPF values were consistent throughout the experimental protocol, indicating that over time the respirator remained on the face. Most subjects thought the respirator was easy to breathe through, moderately comfortable, and stable on the face.
Considering the data from Hyatt (Citation1976), it is not clear whether OSHA appreciated that the fit test results for quarter-facepiece respirators equipped with high efficiency filters were more appropriate to the derivation of an APF for this respirator class. If OSHA had used these data, it is likely the agency would have promulgated an APF of 10 for quarter-facepiece respirators. We found no further studies of laboratory, simulated or workplace fit for quarter-facepiece respirators.
There are no standardized methods for measuring an SWPF. Approaches have included performance of tasks designed to mimic workplace activities, as in this study (Cohen et al. Citation2001; Dietrich et al. Citation2015; Sietsema et al. Citation2015); multiple respirator donnings (Coffey et al. Citation1999, Citation2004; Lawrence et al. Citation2006); and tasks conducted in a simulated workplace environment (Hauge et al. Citation2012).
Coffey et al. (Citation2004) and Lawrence et al. (Citation2006) measured SWPFs by averaging the results of eight-exercise fit tests on the same respirator re-donned six times; in each study a respirator was tested on 25 subjects with varying face sizes but not selected to fulfill any panel criteria. Coffey et al. (Citation2004) found a mean 5th percentile SWPF of 74.5 for 13 filtering facepiece respirator (FFR) models that passed an initial quantitative fit test; no subjects passed the quantitative fit test on five additional FFR models. For those subjects passing a quantitative fit test, Lawrence et al. (Citation2006) measured an average 5th percentile SWPF of 20.5 and 13 for 15 half-facepiece elastomeric respirator models and eleven FFR models, respectively. No subjects passed the quantitative fit test for four additional FFR models.
Hauge et al. (Citation2012) measured second-by-second fit on a single FFR model worn by eight registered nurses performing realistic healthcare tasks in a simulated patient room; the 5th percentile SWPF was 208. Sietsema and Brosseau (Citation2018) measured second-by-second fit on a single FFR model worn by 15 subjects with face sizes in 7 of 10 cells of the NIOSH bivariate panel. Subjects performed three simulated healthcare tasks (similar to those used in this study). The 5th percentile SWPF was 108.
The performance of the Envo Mask quarter-facepiece respirator is similar to that of reusable half-facepiece elastomeric respirators and some high-performing N95 FFRs and much better than most N95 FFRs.
The work of Coffey et al. (Citation2004), Lawrence et al. (Citation2006), and others illustrates the importance of fit testing to ensure well-fitting respirators; as well, quantitative methods are more rigorous than qualitative ones in assuring a well-fitting respirator. Few studies have examined the association between quantitative FFs and SWPFs or WPFs. Sietsema and Brosseau (Citation2018) found a strong association (r = 0.88) in a similar study of 15 subjects wearing an N95 FFR; FFs were measured using the eight-exercise OSHA protocol. This study found a less strong correlation (r = 0.55) indicating the variable nature between fit factors obtained during a fit test and those achieved while a subject is performing their job tasks, even with a single donning as performed in this study.
The exclusion of three subjects whose face sizes did not fall within the NIOSH bivariate panel dimensions suggests that some fraction of the current worker population may not be adequately represented. One of the excluded subjects had a relatively wide face size and was not able to achieve a passing fit factor; their SWPF (truncated) was also well below that of subjects whose faces fit within the panel dimensions.
Hines et al. (Citation2019) surveyed healthcare workers with respirator experience for their impressions of the comfort and protection offered by different types of respirators. Those wearing N95 FFRs gave higher comfort ratings than half-facepiece elastomeric respirator users. Conversely, elastomeric respirator users rated the protection offered by their respirator more highly than N95 FFR users. Respondents were more likely to select an elastomeric or powered air purifying respirator over an N95 FFR for higher risk scenarios. These data suggest that a relatively lightweight quarter-facepiece elastomeric respirator providing a similar level of protection as a reusable half-facepiece respirator could have a role to play in healthcare and other workplace settings.
A limitation of this study is that the final set of subjects deviated slightly from the NIOSH bivariate panel requirements; however, at least one subject was located in each of the ten cells. We used a modified fit testing protocol instead of the full eight exercises as described in ASTM F3407-20; however, the modified protocol is a validated and OSHA-approved fit test (OSHA Citation2019). It should be noted that SWPF values calculated manually in Microsoft Excel will have larger errors for the recorded measurements when compared to the truncated values.
The data that support the findings of this study are available from the corresponding author, MS, upon reasonable request.
Conclusions
These data confirm the 1976 findings of Hyatt and suggest the APF of quarter-facepiece respirators should be greater than 5. This class of respirators has been largely ignored by manufacturers for the past 40 years, with the advent of filtering facepiece respirators (FFRs). Our results suggest that a quarter-facepiece respirator is capable of achieving a degree of fit similar to that of half-facepiece respirators.
Reusable elastomeric respirators offer several important advantages over FFRs. In healthcare settings the general practice is to wear an FFR once and then throw it away, while an elastomeric respirator can be cleaned and re-used many times, a considerable cost savings during a pandemic. Elastomeric half-facepiece respirators can be bulky and uncomfortable; a relatively lightweight quarter-facepiece elastomeric respirator may be more likely to be worn. When FFRs are in short supply, a well-fitting, comfortable, low-profile, reusable quarter-facepiece respirator offers an acceptable option for ensuring healthcare and other worker protection.
Acknowledgments
Drs. Sietsema and Hamza conducted this project with support from a contract between Sleepnet Corporation and the University of Illinois Chicago. Dr. Brosseau received support from a separate contract with Sleepnet to provide technical input and review and to assist in the preparation of this manuscript. We thank Dr. Steven Edwards from Rush University Medical Center, who assisted with subject recruitment and access to a simulated patient room with manakin and task trainers.
Data availability
The data that support the findings of this study are available from the corresponding author, MS, upon reasonable request.
Additional information
Funding
References
- ANSI. 2010. Z88.10-2010. Respirator fit testing methods. Fairfax (VA): American Industrial Hygiene Association.
- ASTM. 2020. F3407-20 Standard test method for respirator fit capability for negative-pressure half-facepiece particulate respirators. doi:10.1520/F3407-20.
- Coffey CC, Campbell DL, Zhuang Z. 1999. Simulated workplace performance of N95 respirators. Am Ind Hyg Assoc J. 60(5):618–624. doi:10.1080/00028899908984481.
- Coffey CC, Lawrence RB, Campbell DL, Zhuang Z, Calvert CA, Jensen PA. 2004. Fitting characteristics of eighteen N95 filtering-facepiece respirators. J Occup Environ Hyg. 1(4):262–271. doi:10.1080/15459620490433799.
- Cohen HJ, Hecker LH, Mattheis DK, Johnson JS, Biermann AH, Foote KL. 2001. Simulated workplace protection factor study of powered air-purifying and supplied air respirators. AIHA J. 62(5):595–604. doi:10.1080/15298660108984658.
- Dietrich J, Yermakov M, Reponen T, Kulkarni P, Qi C, Grinshpun SA. 2015. Protection of firefighters against combustion aerosol particles: simulated workplace protection factor of a half-mask respirator (pilot study). J Occup Environ Hyg. 12(6):415–420. doi:10.1080/15459624.2015.1006637.
- Hauge J, Roe M, Brosseau LM, Colton C. 2012. Real-time fit of a respirator during simulated health care tasks. J Occup Environ Hyg. 9(10):563–571. doi:10.1080/15459624.2012.711699.
- Hines SE, Brown C, Oliver M, Gucer P, Frisch M, Hogan R, Roth T, Chang J, McDiarmid M. 2019. User acceptance of reusable respirators in health care. Am J Infect Control. 47(6):648–655. doi:10.1016/j.ajic.2018.11.021.
- Hyatt EC. 1976. Respirator protection factors. Los Alamos (NM): Los Alamos Scientific Laboratory, Report Number LA-6084-MS. https://www.osti.gov/servlets/purl/4073433.
- Lawrence RB, Duling MG, Calvert CA, Coffey CC. 2006. Comparison of performance of three different types of respiratory protection devices. J Occup Environ Hyg. 3(9):465–474. doi:10.1080/15459620600829211.
- Nelson TJ. 1995. The assigned protection factor of 10 for half-mask respirators. Am Ind Hyg Assoc J. 56(7):717–724. doi:10.1080/15428119591016755.
- OSHA. 2006. Assigned protection factors: final rule. Federal Register. 71:50121–50192.
- OSHA. 2019. Additional ambient aerosol CNC quantitative fit testing protocols: respiratory protection standard. Final rule. Federal Register. 83:50739–50755.
- Richardson AW, Hofacre KC, Weed J, Holm R, Remiarz R. 2013. Evaluation of a faster fit testing method for full-facepiece respirators based on the TSI Portacount®. J Int Soc Respir Protect. 30(2):116–128.
- Richardson AW, Hofacre KC, Weed J, Holm J, Remiarz R. 2014a. Evaluation of a faster fit testing method for elastomeric half-mask respirators based on the TSI Portacount®. J Int Soc Respir Protect. 31:9–22.
- Richardson AW, Hofacre KC, Weed JC, Holm R, Remiarz R. 2014b. Evaluation of a faster fit testing method for filtering facepiece respirators based on the TSI Portacount®. J Int Soc Respir Protect. 31:43–56.
- Sietsema M, Bodurtha P, Dickson E, Brosseau L. 2015. Evaluating simulated workplace protection factors for a first responder low-level protective ensemble. J Int Soc Respir Protect. 32:1–13.
- Sietsema M, Brosseau LM. 2018. Are quantitative fit factors predictive of respirator fit during simulated healthcare activities? J Occup Environ Hyg. 15(12):803–809. doi:10.1080/15459624.2018.1515490.