Abstract
Workers, particularly outdoor workers, are among the populations most disproportionately affected by climate-related hazards. However, scientific research and control actions to comprehensively address these hazards are notably absent. To assess this absence, a seven-category framework was developed in 2009 to characterize the scientific literature published from 1988–2008. Using this framework, a second assessment examined the literature published through 2014, and the current one examines literature from 2014–2021. The objectives were to present literature that updates the framework and related topics and increases awareness of the role of climate change in occupational safety and health. In general, there is substantial literature on worker hazards related to ambient temperatures, biological hazards, and extreme weather but less on air pollution, ultraviolet radiation, industrial transitions, and the built environment. There is growing literature on mental health and health equity issues related to climate change, but much more research is needed. The socioeconomic impacts of climate change also require more research. This study illustrates that workers are experiencing increased morbidity and mortality related to climate change. In all areas of climate-related worker risk, including geoengineering, research is needed on the causality and prevalence of hazards, along with surveillance to identify, and interventions for hazard prevention and control.
Introduction
Climate and weather patterns are changing (Dahl et al. Citation2019b; Moda et al. Citation2019; IPCC Citation2021). As a result, the burden of climate change on workers is increasing (Kim and Lee Citation2020). However, the attention on this burden in the occupational safety and health (OSH) field, the media, and state and business action plans is limited (Constible et al. Citation2020; Toivanen and Uusitalo Citation2022). Identifying how all worker populations may be at increasing yet variable risk of adverse effects is essential to implementing preventive measures.
Workers are one of the first societal groups exposed to climate-related hazards. Their exposure may be longer and greater than for the rest of the population because often work environments are difficult to modify, work must continue, and tasks must be completed despite changes in climate and weather. Consequently, morbidity, mortality, and injury rates related to climate change hazards appear to be increasing, as is the economic burden (Gubernot et al. Citation2015; Dong et al. Citation2019; Kjellstrom et al. Citation2019; Pradhan et al. Citation2019; Dillender Citation2021).
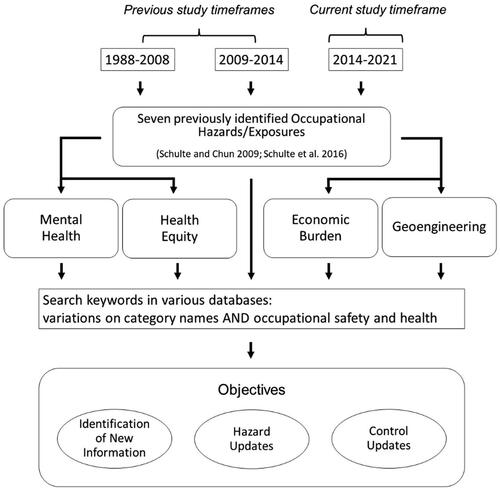
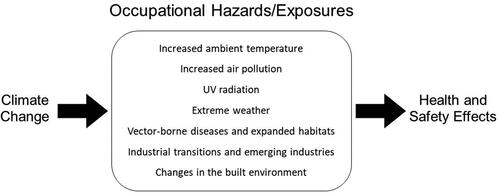
Historically, no systematic, comprehensive means of identifying OSH hazards from climate change existed. To address this deficit, Schulte and Chun (Citation2009) reviewed the scientific literature published from 1988–2008 to develop a framework that identified these seven categories of climate hazards: (1) increased ambient temperature; (2) air pollution; (3) ultraviolet exposure; (4) extreme weather; (5) vector-borne diseases and expanded habitats; (6) industrial transitions and emerging industries; and (7) changes in the built environment (). Workers will likely be exposed to more than one of these hazards, at the same time or at various times, and cumulative effects will probably occur (US EPA Citation2003). In 2016, the literature on the framework was updated for 2008–2014 (Schulte et al. Citation2016), and additional topics related to OSH were considered, including mental health effects, economic burden, and geoengineering. These additional topics are related to the framework and crosscut each of the hazard categories. Additionally, Schulte et al. (Citation2016) addressed key priorities for actions to better characterize and understand the relationship between climate change and worker health and safety issues. These priorities included research, surveillance, risk assessment, and management. A detailed review of research priority needs was also presented (Schulte et al. Citation2016). The current update presents further information from 2014–2021.
Figure 1. Summary schematic of the Schulte and Chun (Citation2009) conceptual framework of the relationship between climate change and occupational safety and health.
Methods
Building on the previous assessments during 1988–2008 and 2009–2014, this paper updates the literature further during 2014–2021 with new studies of climate change–related adverse effects that workers experience on the job (). The literature update involved searching databases (PubMed, Scopus, PsychInfo, Social Services Abstracts, Sociology Abstracts, ABI Inform, Agricultural & Environmental Science Collection, Safety Lit, and GreenFILE) for English-language articles. The keywords were variations of the seven category names for climate-related occupational hazards. The authors used ad hoc searches and snowball techniques to supplement searches of scientific and gray literature. They reviewed the titles and abstracts from the searches and included literature that added new information to the climate hazard categories or the knowledge base for hazard protection and control. The searches also addressed crosscutting issues that the authors considered critical: mental health implications, economic burden, equity issues, and the potential impact on workers of geoengineering. Because of the vast, wide-ranging relevant literature, this article scans the horizon rather than presenting a systematic review (Streit et al. Citation2021). For each of the categories in the framework, the authors characterized the literature in terms of hazards and controls. In addition, they addressed new information illustrating the importance of the critical crosscutting topics listed above.
Results: occupational health hazards and effects related to climate change—2014–2021
Increased ambient temperatures
Hazard update
One of the most commonly identified and discussed effects of climate change is increasing ambient temperatures and the resulting additional heat burden placed on populations. Heat stress has long been a major concern for many worker populations, both outdoors and indoors (Kjellstrom et al. Citation2009; Schulte and Chun Citation2009; Arbury et al. Citation2014; Applebaum et al. Citation2016; Constible et al. Citation2020; Park et al. Citation2021). In the United States, outdoor workers are expected to experience a three- to four-fold increase in the number of days with a heat index of above 100 °F (38 °C) by the mid-2000s (Dahl et al. Citation2019a; Dahl et al. Citation2019b). The heat index is an indicator of heat discomfort and is also known as apparent temperature, which considers temperature and humidity interactions and the associated perceived equivalent (apparent) temperature. It feels hotter than its reported temperature on a thermometer when ambient humidity is high because increasing levels of humidity decrease the water vapor partial pressure gradient between the skin and air, restricting the evaporative process of sweat. Higher humidities and ambient temperatures that exceed the temperature of the skin (approximately 95 °F (35 °C)) result in a net heat gain because sweat does not readily evaporate, interfering with the body’s ability for cooling via evaporation of sweat (Larrañaga and Wang Citation2012).
Outdoor workers such as those in construction, agriculture, and landscaping are at the highest risk of adverse effects from increased ambient temperatures. Many of those work activities are labor intensive, which can cause the body to generate excessive heat (NIOSH Citation2016). A substantial proportion of heat-related fatalities occur during the first day on the job, which emphasizes the importance of acclimatization (Arbury et al. Citation2014). From 1992–2016, 285 construction workers died from heat-related causes, accounting for more than one-third of all U.S. occupational deaths related to heat exposure (Dong et al. Citation2019). A study of construction workers in Washington State found a 0.5% increase in the chances of experiencing traumatic injuries per 1 °C increase in maximum daily humidex (a mean of how hot it feels that combines temperature and humidity) (Calkins et al. Citation2019). A review of existing epidemiological research on heat stress and construction workers in the United States and internationally found that heat-related health effects among construction workers were a significant but understudied topic (Acharya et al. Citation2018).
Populations disproportionately affected by heat stress include foreign-born workers, particularly because many work outdoors and in industries such as agriculture, construction, and services. In a review of Nepali migrant construction workers in Qatar, investigators estimated that 200 of the 571 deaths during 2009–2017 could have been prevented if effective heat-protective measures had been implemented as part of local OSH programs (Pradhan et al. Citation2019). It can be difficult to determine whether a worker’s death is heat-related (for example, causes of death are often poorly described, e.g., “cardiac arrest”) and whether the implementation of useful controls has been inadequate (Pradhan et al. Citation2019).
Agricultural workers are another group at high risk of experiencing adverse health effects caused by extreme heat. As the average ambient temperature increases, farmworkers have been shown to experience an increase in heat-related events leading to morbidity and mortality (Gubernot et al. Citation2015; Hesketh et al. Citation2020). Likewise, agriculture workers may be at increased risk for traumatic injury when working in elevated and extreme temperatures (Spector et al. Citation2016). However, more research is needed to understand the relationship between traumatic injury risks and higher temperatures.
Roughly 20% of heat-related deaths reported to the Occupational Safety and Health Administration (OSHA) are in the Agriculture, Fishing, and Forestry sector (Gubernot et al. Citation2015; Morris et al. Citation2019). A study of workers’ compensation claims in Washington State during 2006–2017 found that Hispanic workers, as well as agriculture and public administration workers, were disproportionately represented in heat-related illness (HRI) cases. Furthermore, many of these cases occurred below the state’s 89 °F (31.7 °C) heat rule (Hesketh et al. Citation2020). Langer et al. (Citation2021) concluded that even when farm workers reported compliance with California OSHA (Cal/OSHA) regulations, worker training and hydration replacement were not sufficient to prevent HRI, especially during work at a fast rate.
Extreme heat exposure is linked to chronic kidney disease (CKD). The literature shows an increase in the prevalence of kidney disease among agricultural and construction workers, especially in hot regions (Pradhan et al. Citation2019; Shih Citation2023). Sugarcane work is known to be associated with this disease (Pundee et al. Citation2021). However, although the cause(s) of the disease are unknown, at least one group has suggested heat stress nephropathy may be a driver of CKD of unknown etiology as climate change contributes to rising temperatures (Glaser et al. Citation2016).
Control update
In 2016, the National Institute for Occupational Safety and Health (NIOSH) published an updated guidance document, the NIOSH Criteria for a Recommended Standard: Occupational Exposure to Heat and Hot Environments (NIOSH Citation2016). This document, along with stakeholder efforts and the recognition that heat continues to cause heat-related deaths, illnesses, and injuries in working populations, has led to a major push in the United States for a federally mandated occupational heat standard.
Currently, there is no OSHA federal heat standard requiring employers to abide by defined rules for heat safety at their workplaces. A few state OSHA programs, such as Cal/OSHA, have implemented heat standards for employers (Cal/OSHA Citation2005). In 2021, additional state OSHA programs, recognizing the increasingly extreme temperatures being experienced by workers, created temporary or emergency heat standards (Oregon Citation2021; Washington State Department of Labor and Industries Citation2021). In addition, OSHA announced plans to launch a rulemaking process to develop a workplace heat standard (OSHA. Citation2021). Setting a federal standard for occupational heat stress is an important step toward protecting workers. As previously recognized, many workers are at additional risk of HRIs, not only from environmental exposures (temperature, humidity, direct sun) but also from the exertion of work activities and from wearing necessary personal protective equipment and clothing (NIOSH Citation2016).
The need for acclimatization programs has been previously recognized in the literature (Arbury et al. Citation2014; Schulte et al. Citation2016; Morrissey et al. Citation2021). However, acclimatization provides little protection for workers during heat waves or other extreme heat events, when temperatures rise too quickly for them to physiologically adjust to working in suddenly hotter environments. For this reason, steps should be taken by employers to implement a heat alert plan that will increase the precautions taken to protect workers during heat waves (NIOSH Citation2016).
There are several factors associated with heat stress on the body, including clothing, physical fitness level, and activity. Other factors are environmental: relative air velocity, mean radiant temperature, air temperature, and air relative humidity (Pal et al. Citation2021). Modifiable factors include providing proper shade, drinking water, and other cooling mechanisms, as well as increasing awareness and prevention training. Agriculture workers have been found to benefit from taking regular breaks and having shifts adjusted to the coolest part of the day. However, shift adjustments must be balanced with controls for sleep disruption and deprivation. Piece-rate payment in agriculture has been associated with an increased risk for HRI (Spector et al. Citation2015). The effects of increased heat exposure are also disproportionately borne by foreign-born, migrant, seasonal, and rural workers, who are employed in sectors that work predominantly outside (Moyce and Schenker Citation2017).
The National Weather Service has created a Weather-Ready Nation Strategic Plan that includes a national early warning system for extreme heat, heat metrics developed with the support of public health research, and a national outline for the systematic tracking of reliable data on extreme heat and HRI (NWS Citation2020). Furthermore, the plan explains the importance of developing measures to enhance resilience and targeted interventions to manage extreme heat in the United States.
Air pollution
Hazard update
Although numerous studies have captured the negative health impact on the general population of ambient air pollutants, primarily ozone and PM2.5 (particles with a diameter of 2.5 µm or less), few have captured the long-term impact of air pollution due to climate change on worker health (Karita et al. Citation2001; Muhammad et al. Citation2014). Available studies show that the increasing impact of climate change on levels of air pollutants will disproportionately impact outdoor workers with increased exposure to PM2.5 (Kinney Citation2018), ozone (Vinikoor-Imler et al. Citation2014; Adam-Poupart et al. Citation2015; Carvalho et al. Citation2018; Schifano et al. Citation2019; Tang et al. Citation2021), and allergens (Lee et al. Citation2021). The impact of these exposures is often heightened by the physical demands related to many outdoor occupations (US EPA Citation2020). Exposure to nitrogen dioxide (NO2), mainly in warm months, was associated with work-related injuries, and exposure to PM10 (particles with a diameter of 10 µm or less), sulfur dioxide (SO2), and NO2 was associated with hyperuricemia in traffic police officers (Tang et al. Citation2021).
Ambient ozone exposures are expected to continue to increase in the United States, particularly affecting outdoor workers (Fann et al. Citation2015). The health impacts of ambient ozone are both acute and chronic (Applebaum et al. Citation2016). The effects of acute and ambient ozone exposure can occur in healthy adults at concentrations lower than the U.S. occupational limit of 100 parts per billion (ppb) (Applebaum et al. Citation2016; Kinney Citation2018; OSHA Citation2022). In 2020, the EPA completed its review of the body of available scientific evidence and exposure/risk information and decided to retain the existing ozone National Ambient Air Quality Standard (NAAQS) of 70 ppb (EPA Citation2020). This applies to tropospheric ozone, which is the ground layer closest to the earth, as opposed to upper-level or stratospheric ozone.
One of the most studied groups with increased adverse health risks due to climate change and air pollution is wildland firefighters. The primary exposure of concern to this cohort is PM2.5 (US EPA Citation2019), however, there are many additional pollutants of concern, including ozone, polycyclic aromatic hydrocarbons, and aldehydes (Adetona et al. Citation2016; Wu et al. Citation2020). Although there are many measures of wildland firefighter exposure and acute effects, the long-term impact of exposure is not well studied or understood (Adetona et al. Citation2016). A consistent trend across the limited studies shows declines in lung function when post-season and pre-season values are compared (Betchley et al. Citation1997; Miranda et al. Citation2012), but the long-term impact is uncertain. Further evaluation of significant clinical health endpoints in this population is needed.
Control update
Conventional workplace measures to prevent worker exposure to air pollution, such as engineering controls, encapsulation, and ventilation, are not applicable in the outdoor environment, and employers and workers may not have control over sources of air pollution (WHO Citation2018). Still, some measures can be taken to protect outdoor workers from ambient air pollution, such as reducing time spent outdoors; rotating workers; restricting work during times of severe air pollution; using a respiratory protection program, medical surveillance, and case reporting; and supporting the development of air quality standards (WHO Citation2018).
Various organizations and investigators have published guidance to protect wildland firefighters and workers in offices and commercial buildings (Broyles Citation2013; National Wildfire Coordinating Group Citation2013; Occupational Health and Safety Citation2019; CDC Citation2020; Washington State Department of Labor and Industries Citation2020; US EPA Citation2021c). A 2019 workshop sponsored by the American Thoracic Society recommended a unified federal response to wildland fires (Rice et al. Citation2021). The dynamic environment of wildland fires makes hazard prevention and control difficult. The workshop recommended multidisciplinary research, policy development, and communication to address hazards for those managing and fighting wildland fires as well as the general public. Semmens et al. (Citation2021) identified specific wildland firefighter tasks related to direct suppression that could be targets for intervention aimed at wildland firefighters’ perception of smoke exposure and minimizing smoke exposure.
Ultraviolet radiation
Changes in various constituents of the atmosphere, such as a decrease in stratospheric ozone, affect the intensity of ultraviolet (UV) radiation at the earth’s surface and the exposure of workers (Bais et al. Citation2015). Stratospheric ozone works as a filter to absorb UV radiation before it comes into the lower atmosphere.
Hazard update
The health effects of UV radiation have been identified before the time period surveyed by this report and include cancer, eye effects, and disturbed immune function (Schulte and Chun Citation2009; Barnes et al. Citation2019; Parker Citation2021). The extent of outdoor workers’ exposure to UV radiation varies at different places on the Earth. Despite indications from measurements in a few studies, no statistically significant decreases in UVB radiation attributable to the beginning of stratospheric ozone recovery have yet been detected (Bais et al. Citation2015). Nonetheless, the Montreal Protocol (an international treaty to phase out ozone-depleting gases) has “prevented global depletion of stratospheric ozone and consequently large-scale increases in solar UV-B radiation” and played an important role in preventing many adverse effects of high UV exposure (Barnes et al. Citation2019).
Control update
There are specific measures employers and outdoor workers can take to mitigate exposures, including the use of sunscreens and sun-protective clothing. Certain recommendations for sun-protective clothing may be at odds with choosing appropriate clothing for working in the heat, such as long sleeves, dark versus light colors, and a tighter fabric weave. However, the extent of their use depends on employers’ and workers’ perceptions and motivation or direction to implement them (Hault et al. Citation2016; Peters et al. Citation2020; Cherrie et al. Citation2021).
Extreme weather
Hazard update
The increase in global temperature has been linked to an increase in the frequency, severity, and impact of extreme weather such as heat waves, floods, landslides, drought, and wildfires (Pinkerton et al. Citation2019). Establishing such links is challenging because of combinations of factors, including natural variability (Knutson et al. Citation2017). A new type of research called “attribution science” is being developed to determine “not if climate change causes an event but if climate change made some events more severe and more likely to occur, and if so by how much” (Cho Citation2021). In the United States from 1980–2021, 310 weather events caused at least $1 billion in total damages (NOAA NCEI Citation2022). Workers died and were injured in these events, but comprehensive counts are not available for the scope of this update. Previously, it was reported that from 1992–2006, 317 workers died or were injured in these events (Schulte and Chun Citation2009). One population of workers—aptly named “storm chasers,” consisting largely of migrant workers involved in restoring buildings, towns, regions, and waterways—has experienced a range of hazards and adverse health effects (Stillman Citation2021). In addition, because of a lack of occupational health and safety programs, these workers suffer from concomitant deprivation of food, shelter, labor protection, and health insurance. These factors interact with workplace hazards to negatively affect worker health and safety.
Extreme weather directly affects agriculture workers, from landowners to laborers, resulting in a variety of acute and chronic adverse health outcomes such as traumatic injuries, fatigue, and mental stress. These extreme weather events include prolonged drought, flooding, hurricanes, and extreme El Niño/La Niña weather patterns, as well as severe storms, heatwaves, freezes, and wildfires. In commercial fishing, weather is an important risk factor in vessel sinkings and crewmember survival (Lucas et al. Citation2018). As extreme weather events increase and weather patterns change over time, research is needed on the best way to relay accurate, tailored, useful forecasts to fishing workers (Finnis et al. Citation2019).
Sea levels are rising, contributing to increased storm surges that will cause flooding and high humidity (Beggs Citation2014; Levy and Patz Citation2015a; D'Amato et al. Citation2016; Sheehan et al. Citation2017; D'Amato M et al. Citation2018; Demain Citation2018; Katelaris and Beggs Citation2018; Thien et al. Citation2018; Poole et al. Citation2019; American Academy of Allergy Asthma and Immunology Citation2020; D'Amato et al. Citation2020; Eguiluz-Gracia et al. Citation2020; Katelaris Citation2021). Rising sea levels can lead to damp buildings and mold growth. More moisture and higher temperatures are leading to fungal growth, which impacts indoor air quality (Katelaris and Beggs Citation2018; Poole et al. Citation2019; Deng et al. Citation2020).
Higher temperatures are integral in creating conditions for lightning. In 2021, 24 million more lightning strikes (an increase of 14%) occurred in the United States, compared with 2020 (Vaisala Citation2022). A drastic rise in lightning strikes was also seen in the Arctic, with 7,278 lightning strikes north of 80°N, almost double the total number for the previous 9 years (Vaisala Citation2022). The increasing number of workers projected to work in the Arctic will result in a larger population at risk for lightning strikes.
Control update
The protection of workers at the macro level will depend on global governments and economic policies. At the micro level of workers and employers, the amount of risk will depend on the response to risk. The primary responsibility for controlling these hazards falls on employers. One major type of response is adaptation, such as hardening physical infrastructure, relocating people and assets, and ensuring backup capacity, which may have an impact on workers who have to perform tasks in extreme weather conditions (Woetzel et al. Citation2020). Beyond adaptation, employers and workers need training in preventative practices. They also should be included in the development and implementation of climate mitigation plans that affect worker safety (Pinkerton et al. Citation2019). A McKinsey Company report on 105 countries found that “while companies and communities have been adapting to reduce climate risk, the pace and scale of adaptation are likely to need to significantly increase to manage rising levels of physical climate risk” (Woetzel et al. Citation2020).
Vector-borne diseases and other biological hazards
Infectious diseases, including zoonotic diseases, are affected by changing environments. Climate change can alter the habitat and geographic distribution of disease vectors and other biological hazards. Outdoor workers are at the highest risk of exposure. provides additional details on selected at-risk worker populations for these hazards and associated diseases.
Table 1. Populations disproportionately affected by select biological hazards.
Hazard update
Vector-borne diseases
The potential impact of climate change on vector-borne diseases continues to be a well-researched topic, although the available literature on specific workers or occupations remains limited (Beard et al. Citation2016; Ogden Citation2017; Levi et al. Citation2018; Caminade et al. Citation2019; Fouque and Reeder Citation2019; Adam-Poupart et al. Citation2021). Climate factors such as temperature extremes and precipitation patterns affect the seasonality and distribution of vector-borne diseases (Ogden and Lindsay Citation2016; Caminade et al. Citation2019; Fouque and Reeder Citation2019). A review of studies showed a positive correlation between higher air temperature and the expansion of vector habitats (Levi et al. Citation2018). Temperature affects the biting, survival, and reproductive rates of vectors, as well as the survival and development rates of the pathogens they carry (Campbell-Lendrum et al. Citation2015; Levi et al. Citation2018). Precipitation is an important factor for vectors with aquatic developmental stages, such as mosquitoes, and affects humidity, which impacts many vectors (Campbell-Lendrum et al. Citation2015).
Mosquitoes are one of the world’s deadliest animals (CDC Citation2019). In the United States in 2020, West Nile virus was the most common cause of domestic arboviral neuroinvasive disease, with 559 cases reported, for an incidence of 0.17 cases per 100,000 population (Soto et al. Citation2022). More than 150,000 cases of mosquito-borne diseases were reported from 2004-2016 in the United States (Rosenberg et al. Citation2018). During this time, West Nile Virus was the most common mosquito-borne disease in the continental United States (nearly 32,000 reported cases), while epidemics of dengue, chikungunya, and Zika viruses were reported, mainly in U.S. territories (Rosenberg et al. Citation2018). Increased rainfall or extreme rainfall associated with climate change is an important factor for mosquito-borne diseases (Campbell-Lendrum et al. Citation2015). Worksites (such as construction sites) with poor water drainage collect water from increased precipitation and provide breeding sites for mosquitoes, resulting in an increased risk of bites by infected mosquitoes (Applebaum et al. Citation2016; Wilke et al. Citation2018).
Tick-borne diseases (with the majority being Lyme disease) more than doubled in the United States and U.S. territories during 2004–2016, with more than 490,000 cases, made up more than 75% of all reported vector-borne disease cases (Rosenberg et al. Citation2018). In 2019, more than 34,900 confirmed and probable cases of Lyme disease were reported to CDC (CDC Citation2021a). Although the use of insurance databases is critical for determining the actual number of cases treated each year, Lyme disease is under-reported due to reporting complexities. An analysis of insurance claims data during 2010–2018 estimated that Lyme disease was diagnosed and treated in about 476,000 patients annually (Kugeler et al. Citation2021).
Climate change has been associated with the geographic distribution, local abundance, seasonal tick activity, and expansion of ticks to higher altitudes and latitudes (Eisen et al. Citation2016; Semenza and Suk Citation2017; Ogden et al. Citation2021). Researchers projected that the average annual period of Lyme disease onset in endemic states will be 0.4–0.5 weeks earlier for 2025–2040 and 0.7–1.9 weeks earlier beyond 2065 (Monaghan et al. Citation2015), and the activity of nymphs in some areas is predicted to advance 8–11 days by the 2050s (Levi et al. Citation2018).
Poisonous plants
Changes in temperature and precipitation can affect the distribution and growth rates of a variety of vegetation, including poisonous plants. Giant hogweed, a plant that was purposely imported as a unique ornamental, has become more invasive because of climate change and is spreading in parts of the United States and Europe (Klimaszyk et al. Citation2014; Schindler et al. Citation2018). Giant hogweed sap contains furanocoumarins, causing skin hypersensitivity to UV light, and resulting in rashes and blistering (Klimaszyk et al. Citation2014; Downs et al. Citation2019). Outdoor workers have reported serious injuries from blistering skin after mowing or other work after contact with giant hogweed (Klimaszyk et al. Citation2014; Downs et al. Citation2019). More outdoor workers will be at risk of exposure as this species continues to expand its range.
Allergens and molds
With climate change-related high temperatures and precipitation, it is likely that the amounts of airborne fungal spores (aeroallergens and asthmagens) will increase (Grinn-Gofron et al. Citation2019). As climate change brings higher global temperatures and increased precipitation, flooding, storm damage, and indoor mold growth will likely become a more widespread problem, along with changing geographic distributions (Levy and Patz Citation2015a; D'Amato et al. Citation2016; Pugatch Citation2019; Buis Citation2020; Knutson et al. Citation2020; Du et al. Citation2021; Katelaris Citation2021). Both outdoor and indoor workers may experience higher fungal exposure and higher rates of fungal diseases.
Occupational exposure to mycotoxins (including aflatoxins) is a growing concern as climate change is expected to impact the ecology, adaptation, and proliferation of mycotoxins (Marroquin-Cardona et al. Citation2014; Viegas et al. Citation2016; Valencia-Quintana et al. Citation2020; Viegas et al. Citation2020). While mycotoxins are a public health concern when ingested, workers can be exposed to fungal toxins and carcinogens via respiratory, dermal, and mucosal routes (Marroquin-Cardona et al. Citation2014; Wangia et al. Citation2019).
As climate change causes drier and windier conditions in the southern and western United States, coccidioidomycosis (also known as Valley fever) continues to be a growing occupational health challenge (Wilken et al. Citation2015; Benedict et al. Citation2017; Freedman et al. Citation2018; de Perio et al. Citation2019; Pearson et al. Citation2019). By 2100, it is predicted that climate change will more than double the area where Coccidioides is present in the soil, and the number of cases will increase by 50% (Gorris et al. Citation2019). In California, construction employers in counties where coccidioidomycosis is highly endemic are required to provide annual training to all employees before beginning work that may cause substantial dust disturbance (California Legislature Citation2019).
Other fungal allergic reactions and diseases may be caused by contact with trees or animal droppings. Maple bark disease is a hypersensitivity pneumonitis illness caused by a fungus, Cryptostroma corticale, found on maple trees infested with sooty bark disease (Braun et al. Citation2021). This fungus thrives in hot summers and on trees impacted by drought, and thus it is expected to spread in some areas placing more outdoor workers at risk of exposure. Histoplasmosis is a fungal infection often associated with working in areas with bird or bat droppings, or areas where there are spores in the soil (Benedict et al. Citation2017). Demolition or construction where the spores in the soil are disturbed may place workers at risk for exposure. The fungus is being found in new regions, and climate change is believed to be partially responsible (Benedict et al. Citation2017; Gnat et al. Citation2021).
There is a growing body of literature concerning increasing levels of aeroallergens, asthma, allergic rhinitis, and occupational exposures. As carbon dioxide levels and temperatures have increased, this has led to longer plant growing seasons with earlier flowering and pollen production, increased length of pollen season, higher levels of pollen production, increased allergenicity of pollen, and later frosts (Beggs Citation2014; Levy and Patz Citation2015a; Sheehan et al. Citation2017; Demain Citation2018; Poole et al. Citation2019; American Academy of Allergy Asthma and Immunology Citation2020; D'Amato et al. Citation2020; Deng et al. Citation2020; Eguiluz-Gracia et al. Citation2020; Choi et al. Citation2021; Katelaris Citation2021; Pawankar and Wang Citation2021; Schramm et al. Citation2021; US EPA Citation2021b). Outdoor workers are at increased risk of pollen exposure, as many jobs involve intense physical activity and resultant increased inhalation rates (D'Ovidio et al. Citation2016). Similarly, to the previously mentioned poisonous plants, climate change is expected to influence the geographic distribution of a variety of plants and pollens.
Control update
Recommendations for protecting workers from the potential impact of climate change on biological hazards have included robust disease and vector surveillance, vector control, training for workers about biological hazards and best preventive practices, and personal protective clothing and equipment for workers where appropriate (Tong et al. Citation2016; NIOSH Citation2021). One Health is a transdisciplinary approach that recognizes the interrelationships of human health, animal health, and environmental health to achieve optimal health outcomes (CDC Citation2021b). Due to its comprehensive approach to hazards, the One Health approach may best protect workers and help OSH and public health communities prepare, plan, and respond to the potential impacts of climate change on biological hazards. The expansion of habitats of vectors and biological hazards may lead to increased use of pesticides and herbicides (Gatto et al. Citation2016). Agricultural workers, landscape workers, and other outdoor workers may be at risk of exposure to these substances.
Industrial transitions and emerging industries
The greatest driver of climate change is rising planetary temperatures resulting from the production of greenhouse gases (IPCC Citation2021). A major cause of greenhouse gases is the burning of fossil fuels. The social and economic pressures involved in reducing fossil fuel use and transitioning to renewable energy frame the view of the types of hazards workers will experience. Further, a growth in recycling (which may be one response to climate change and resource depletion) may increase workers’ risk of exposure to hazardous materials and conditions (Anderson et al. Citation2020).
Hazard update
Phasing out fossil fuels has a direct impact on workers in the industries dealing with these energy sources, as well as on the workers in surrounding communities who depend on those industries. Coal is the primary fossil fuel that has been flagged for phasing out globally (UN Environment Programme Citation2019). High costs of coal extraction have led to an undercutting of coal prices by natural gas since the early 2010s (Neal Citation2020). Coal workers continue to suffer from the adverse health effects (such as pneumoconiosis, silicosis, traumatic injury, and hearing loss) they have experienced since the 1800s (Cho and Lee Citation1978; Khanzode et al. Citation2011; NIOSH Citation2011). However, the impact of industrial transitions may be more in the psychosocial realm. Claudia Strambo of the Stockholm Environment Institute stated, “History shows that when a mining transition is not well managed, the impacts to the environment, economy, and social fabric of former mining regions can be catastrophic,” (Casey Citation2019).
To reduce global carbon emissions, significant changes in energy production are expected. The number of renewable energy sources, primarily solar, wind, and hydrogen-generated energy (US EIA Citation2021). Ultimately, solar and wind energy production are expected to partially replace fossil fuel energy generation. However, nuclear power will likely serve as a growing intermediary energy supply for many decades until solar and wind energy provide ample supply and deliver power continuously (IAEA Citation2021). Occupational hazards in the nuclear industry, in terms of injuries and fatalities, are predominantly from the mining and milling of raw materials (Roscoe et al. Citation1995). During operations, a potential for ionizing radiation exposure exists, although even at less concerning levels they are likely still important (Richardson et al. Citation2015). Unresolved issues associated with the disposal of nuclear waste are potentially a more significant occupational and environmental concern; these may be resolved through the commercial development of nuclear fusion. Nuclear fusion, which is a promising energy source, uses radioactive materials with half-lives substantially less than those for fission, and the risk of a major accident is substantially less (Markandya and Wilkinson Citation2007; Ball Citation2022).
Solar photovoltaic systems and wind turbines are likely to be a major replacement for fossil fuels in the future. Various methods of manufacturing photovoltaic materials involve a variety of different materials, most of which are potentially toxic or hazardous (National Research Council Citation2010). Although most of these chemicals have been involved in a fair amount of basic toxicological research (Bakhiyi et al. Citation2014), very little quantitative or qualitative risk assessment research has been done on the occupational health issues arising during the mining of component materials, manufacturing, and recycling processes (Bradbrook et al. Citation2013; Bakhiyi et al. Citation2014). Furthermore, several physical and electrical hazards are associated with the installation and maintenance of photovoltaic systems, including falls and manual-handling concerns, as well as heat stress. However, little data are available for quantifying the rates at which these risks directly affect installers (Duroha et al. Citation2020).
In the wind energy–generation industry, manufacturers of wind turbines have hazards similar to those in the automobile and aerospace industries. Primarily, these involve exposures to epoxy-based resins, glass-reinforced plastic, and noise. Installation and maintenance of wind turbines are associated with work in confined spaces, electrical risks, and falls from heights, potentially exacerbated by the unpredictability of wind gusts (Freiberg et al. Citation2018). Off-shore wind farm hazards include isolation, delay in emergency care for life-threatening injury, and the potential for longer work shifts (Mette et al. Citation2018). Similar to the lack of literature on risks in solar energy production, occupational health hazards in the wind energy industry have been addressed in only limited peer-reviewed scientific literature (Karanikas et al. Citation2021).
Hydrogen technologies may also provide renewable energy (Federal Ministry for Economic Affairs and Energy Citation2020), and the hazards will need to be assessed (Rivikin et al. Citation2015). Although hydrogen energy has the potential to replace fossil fuels, its impact on the atmosphere has yet to be fully assessed (Warwick et al. Citation2022).
Recycling is an important means of energy efficiency, but hazards have arisen in this industry (Anderson et al. Citation2020). More broadly, the transition to a circular economy may expose workers to new hazards, and OSH-relevant knowledge for dismantling old infrastructure may be lacking (Daheim et al. Citation2021).
Another area of transition is the Agriculture, Fishing, and Forestry sector. The agriculture industry is changing because of significant alterations in weather, including rainfall patterns, and more frequent weather extremes, such as high temperatures and longer droughts. The locations where crops have traditionally been grown are moving farther north. Land that has never supported crops is being purchased, anticipating a future opportunity to grow crops. This may result in a need for workers to be located potentially in further remote areas where infrastructure is lacking. In addition, traditional agriculture areas will need to transition to other crops or otherwise adapt.
Control update
In general, the prevention and control of adverse effects on workers from industrial transitions and emerging industries will involve anticipation of scenarios in a matrix of old and new hazards by traditional and future jobs (Schulte et al. Citation2020). For the most part, the hazards will be known ones but in new situations. A critical control measure will be the use of strategic foresight approaches to protect and promote worker safety, health, and well-being (Streit et al. Citation2021). Ultimately, the occupational safety and health field can be a resource to promote a “just transition” for workers who are displaced due to responses to climate change (UNFCCC Secretariat Citation2020).
Changes in the built environment
Hazard update
Much of the response to climate change may be changes in the built environment, which may present hazards to workers. Clearly, some of the new technologies, such as wind and solar, will involve building and construction with new or exacerbated hazards. Moreover, building and construction are responsible for 39% of carbon emissions globally (UN Environment Programme Citation2019). New construction scenarios or expanded construction demands may present hazards to workers beyond those in construction. Additionally, buildings designed to save energy (“tight buildings”) may allow for the buildup of toxic substances, radon gas, and infectious agents, which might affect worker occupants and maintenance staff (Schulte and Chun Citation2009). Other potential impacts on workers could arise from commonly used built environment strategies to combat climate change, such as tree planting, road diets (roadway reconfiguration), bike lane installation, and cool roofs, but these have not been specifically characterized in the literature.
Control update
As with industrial transitions, anticipating hazards from climate change for construction and maintenance workers will benefit from strategic foresight (Streit et al. Citation2021). This may also be useful for identifying hazards for users of built environments, such as workers who are building occupants.
Crosscutting topics
The topics of mental health, health equity, economic burden, and geoengineering crosscut the seven-category framework, and the literature on these is growing.
Mental health effects of climate-related occupational hazards
Although the attribution of adverse mental health outcomes to climate-related hazards is challenging, exposure to climate- or weather-related disasters can cause or exacerbate mental health effects ranging from stress, anxiety, depression, and substance abuse to post-traumatic stress disorders and suicide (Tiesman et al. Citation2015; Dodgen et al. Citation2016; Wang et al. Citation2016; Bromet et al. Citation2017; Casas et al. Citation2017; Tallon et al. Citation2017; Tempest et al. Citation2017; Hanigan et al. Citation2018; Orui et al. Citation2018; Groot et al. Citation2019; Bundo et al. Citation2020; Cruz et al. Citation2020; Fitzgerald et al. Citation2020; Hrabok et al. Citation2020; Clayton et al. Citation2021). Climate impacts and influencing factors include not only health threats from air quality, wildfires, sea level rise, storms, heat, floods, and droughts but also vulnerability at larger community or societal scales, such as natural and built environments, governance and management, and institutions (Dodgen et al. Citation2016). Specific occupations, including first responders, farmers, forestry and fishing workers, public safety workers, and healthcare workers, are at higher risk for adverse mental health outcomes (Dodgen et al. Citation2016; Wang et al. Citation2016; Daghagh et al. Citation2019; Howard et al. Citation2020; Metregiste et al. Citation2020). Overwork, disaster relief work that interferes with personal lives, loss of family members or homes, and economic instability could increase the risk for adverse mental health, including depression and suicidal ideation (Lowe et al. Citation2016; Wang et al. Citation2016; Orui et al. Citation2018).The link between climate change–related occupational hazards and mental health does not appear to be a major consideration of employers. General recommendations have been published but few for employers and workers (Clayton et al. Citation2021). Various authors in trade publications have issued a call for employers to take action as climate change increasingly impacts health, productivity, and well-being (Gifford Citation2018).
Emerging issues include the impacts on the mental health of mass evacuation, inter- and intra-country migration, and relocation related to extreme weather events and the cumulative or mixed effects of hotter temperature, poor air quality, vector-borne risks, and/or extreme events (Dodgen et al. Citation2016; Burke et al. Citation2018; Maitre et al. Citation2018; Li et al. Citation2020). Multiple strategies must be undertaken by employers, workers, and communities to enhance adjustment and coping post-disaster, including enhancing access to care, interagency cooperation, and adequate preparation (Marinucci et al. Citation2014; Dodgen et al. Citation2016; Hrabok et al. Citation2020).
Occupational health equity
Work conditions or work-related conditions
Overall, the literature demonstrates that the nature of work and social determinants of health overlap to affect exposure to climate risks (Hayes et al. Citation2018; Benevolenza and DeRigne Citation2019). In high-income countries like the United States, economically disadvantaged workers (Levy and Patz Citation2015b; US EPA Citation2021a) are disproportionately affected by the negative health effects caused or exacerbated by climate change. Some of these poor health outcomes include respiratory and allergy disorders, vector-borne diseases, and heat-related disorders (Levy and Patz Citation2015b). These populations are also at high risk for the psychosocial impact of climate change, which can include the adverse mental health effects discussed earlier, as well as financial impact (US DOL Citation2022). For example, as a result of Hurricane Katrina, permanently displaced residents (who were largely African American single mothers) and workers experienced significantly higher levels of distress and perceived stress than those who were not uprooted by the disaster (Palinkas Citation2020).
Immigrant workers and those of lower socio-economic status are frequently employed in high-risk occupations (such as agriculture, construction, transportation, and emergency work) that are often subject to extreme weather conditions exacerbated by climate change (Spector and Sheffield Citation2014; Kiefer et al. Citation2016; Schulte et al. Citation2016). Immigrant workers face a combination of risk factors for HRIs, including lack of OSH knowledge and quality training, poverty, language barriers, seasonality of jobs, lack of decision-making autonomy, differences with treatment on the job, and extreme work conditions (Flynn Citation2014; Flynn et al. Citation2014; O'Connor et al. Citation2014; Stoecklin-Marois et al. Citation2015; Fan and Qian Citation2017; Ellis and Stam Citation2018). Immigrants and minorities are also overrepresented in outdoor jobs such as construction, farm work, landscaping, and roofing. For example, Latino farmworkers in the United States are disproportionately exposed to extreme heat waves and other climate risks because of the nature of their work (Mera et al. Citation2015). Limited access to resources (such as food, discretionary funds, and health care) at home and work can also complicate these workers’ climate risk and ability to deal with work-related injuries or illnesses. Migrant farmworkers’ exposure to excess heat is also influenced by other factors such as lack of access to healthcare and living in employer-provided housing that often lacks air conditioning (Arcury et al. Citation2015).
Changes to the workforce
Climate change and human migration patterns are interrelated. It is anticipated that the increasing severity and frequency of catastrophic events (such as hurricanes), as well as the negative impact of shifting weather patterns (such as rainfall levels) on agricultural production, will continue to drive more individuals to migrate to the United States (Palinkas Citation2020). For example, analysis of state-level data showed a significant effect of climate-driven changes in crop yields on the rate of emigration from Mexico to the United States (Hunter et al. Citation2015). Increased migration to the United States will contribute to the increasing diversity within the U.S. workforce, which presents unique challenges to the future of OSH (Tamers et al. Citation2020). Due to unequal treatment and opportunity, as the foreign-born proportion of the workforce grows, work-related injuries and illnesses along with the economic burden on society are anticipated to increase (Flynn Citation2014; Hargreaves et al. Citation2019).
Catastrophic events
Low-wage workers, who are disproportionately racialized ethnic minorities and foreign-born individuals, often reside in neighborhoods and housing more susceptible to extreme weather events (Huang et al. Citation2011; Klinenberg Citation2015; Palinkas Citation2020). Additionally, these workers are more likely to be employed in clean-up and rebuilding efforts, which may expose them to unique and more hazardous or toxic conditions with less government oversight, supervision, and access to protective equipment (Donato et al. Citation2007; Delp et al. Citation2009). For example, during the Katrina disaster, people of color were the most impacted and also the most employed in the rebuilding of the city; residents of the Lower Ninth Ward in New Orleans, who were predominantly African American, and many Latino workers were involved in the rebuilding (Palinkas Citation2020). These OSH concerns will likely rise, given an expected increase in extreme weather events and a surge in foreign-born workers due to increased global climate-related migration to the United States (Palinkas Citation2020).
Future needs
Future OSH attention to climate change should consider the interrelationships among health equity, environmental justice, and climate change. Environmental justice is defined by the CDC as the fair treatment and meaningful involvement of all people, regardless of race, color, national origin, or income, to develop, implement, and enforce environmental laws, regulations, and policies (ATSDR Citation2022). Economic activity and how it is structured in society are fundamental drivers of both workplace conditions and environmental degradation (pollution and climate change). As a result, the relationships between work, social inequity, and environmental justice must be better understood (Kingsolver Citation2011). The practice of externalizing risk (placing the burden of risk on a third party) has negative impacts on workers (Weil Citation2017). For example, individuals from groups and communities who are socially disadvantaged are overrepresented in dangerous and low-paying jobs. As a result, these workers are not only at increased risk of workplace injuries but also at increased risk of living near environmental hazards (such as toxic waste sites) (Klinenberg Citation2015; Palinkas Citation2020).
Economic burden of climate-related OSH hazards
Climate change has affected weather patterns, resulting in extreme temperatures. Both high and low temperatures are detrimental to workers’ health, especially those working outdoors (Dillender Citation2021). These workers are mostly employed in the agriculture, construction, emergency response, commercial fishing, paramedic and firefighting, and transportation industries. Extreme temperatures impose costs on employers in the form of increased energy outlays and reduction in labor productivity or labor supply (Deschênes and Greenstone Citation2011; Auffhammer and Mansur Citation2014; Park et al. Citation2021). Few studies have focused on estimating the economic burden associated with occupational health and climate change. Limaye (Citation2020) estimated the public health costs of 10 climate-sensitive events in 2012 in the United States as $10 billion. According to the Natural Resources Defense Council, the annual health costs of air pollution and climate change are more than $800 billion and are expected to increase over the years (Limaye Citation2021). The International Labor Organization reported that heat stress is gradually becoming an obstacle to economic activities (Kjellstrom et al. Citation2019), reducing the productivity of workers in four sectors (agriculture, construction, industry, and services). Even if appropriate resources are utilized to limit global warming to 1.5 °C above pre-industrial levels by the end of the century, the accumulated financial loss due to heat stress is expected to reach $2.4 trillion by 2030 (Kjellstrom et al. Citation2019). According to estimates, the impact of heat stress on reducing worker productivity is expected to be 0.91% of total working hours (the equivalent of 800,000 full-time jobs) in 2030 (Kjellstrom et al. Citation2019). Licker et al. (Citation2022) estimated that with a modest greenhouse gas emissions reduction, outdoor workers will be exposed to extreme heat conditions in the mid-twenty-first century which is triple that of the late twentieth century, with earnings of approximately $39.3 billion at risk annually. Neidell et al. (Citation2021) assessed that workers’ annual wage loss due to a reduction in time spent working on days with temperatures above 90ºF across the United States will range from $36.7 to $80.0 billion in 2090 under intermediate and high emissions, respectively.
Studies incorporating economic models have shown that the climate change effects on workers are among the most important drivers of the total economic costs of climate change (Orlov et al. Citation2019; Dasgupta et al. Citation2021; Somanathan et al. Citation2021). Dillender (Citation2021) examined 6 months of medical costs for workers’ compensation claims associated with extreme temperatures in Texas in 2015. Higher temperatures were associated with worse health outcomes. He found that a majority of the claims resulting from low temperatures involved above-median medical costs, whereas the claims resulting from high temperatures were more evenly split above and below the median costs. He extrapolated his results, using the assumption that claims arising from temperature have an average work-related injury cost of $20,500 in 2014 dollars (Leigh Citation2011). Each day with a high temperature above 90 °F (32.2 °C) leads to costs from incidents of $0.08 per worker, and each day with a high temperature below 40 °F (4.4 °C) leads to costs from occupational health incidents of $0.15 per worker. Since roughly 10% of workers work outdoors at least one day per week and have an average hourly wage of $18 in 2014 dollars, the implied cost of the reduction in hours worked from each day with a high temperature below 40 °F is about $1.82 per worker in warmer climates, when averaged across all U.S. workers (Dillender Citation2021). Total annual costs in Texas were estimated to be $69.7 million for days above 90 °F and $97.6 million for days below 40 °F (Dillender Citation2021).
Orlov et al. (Citation2019) used an interdisciplinary approach, combining meteorological, epidemiological, and economic analyses, to assess the cost of heat-induced reductions in outdoor worker productivity in Europe caused by the heat waves in August 2003, July 2010, and July 2015 (Orlov et al. Citation2019). They estimated that for the top 10 most affected European countries, average direct economic losses (estimated as the productivity losses in specific sectors) in agriculture accounted for $59–$90 per worker. In construction, these losses were $41–$72 per worker in 2015 U.S. dollar values. According to these authors, the average social costs of these events (estimated as the loss in productivity of other sectors as a result of the heat-induced impacts in agriculture and construction) ranged from $1.6 to $2.7 per capita.
Geoengineering
Geoengineering, also known as “climate intervention” or “climate engineering,” is defined as the intentional, large-scale human manipulation or alteration of the environment (Effiong and Neitzel Citation2016; Jones et al. Citation2017; Abatayo et al. Citation2020). Potential geoengineering interventions to address the changing climate are diverse and could include such approaches as the following: the chemical capture of carbon from the atmosphere; the facilitation of the growth and use of carbon-eating plankton; and using large mirrors to reflect sunlight into space and/or creating and injecting a reflective haze (usually chemicals such as carbon black [soot], various sulfate compounds, fine aluminum particles, aluminum oxides, and nanoparticles like barium titanate) to reflect sunlight into space. To date, the use of geoengineering to mitigate climate change is based on predictive models and, as such, remains highly controversial because it carries a strong possibility of unintended consequences (Ocean Studies Board Citation2015a, Citation2015b).
The extent to which geoengineering would create risks and hazards or decrease climate-related risks and hazards for workers is unknown. Outdoor workers, especially those of low socio-economic status such as manual laborers, farmworkers, nursery workers, ranch workers, construction workers, and wildland firefighters, would be at greatest risk from the effects of climate change and the potential effects of geoengineering. Few studies have been done to determine the human health impacts of exposure to atmospheric aerosols (inorganic sulfates, carbon black, powdered aluminum, aluminum oxides, nanoparticle barium titanates, etc.) proposed for use in geoengineering and the environmental changes that may result from geoengineering. Developing scenarios for different types of geoengineering may help identify potential hazards for workers and would be the first step in identifying prevention and control measures.
Discussion
This review is an update of two earlier reports that established and increased awareness of workers’ risk of exposure to, and adverse effects from, climate change-related hazards (Schulte and Chun Citation2009; Schulte et al. Citation2016). This current horizon-scanning effort discussed new information in all seven categories of climate-related hazards presented in the original framework. These findings support the importance of the complementary, crosscutting topics of mental health, occupational health equity, economic burden, and geoengineering.
The framework initiated in the earlier reviews served as the basis for two reports (NIEHS Citation2015, Citation2022) that described a climate change vulnerability assessment to determine how the impacts of climate change affect workers and how to prepare for these impacts. The findings discussed here imply that workers are at increased risk of exposure to climate-related hazards and that investigators, authorities, employers, trade associations, unions, and workers must make a concerted effort to identify the extent of exposure to these hazards and ways to control them.
Conclusions
The literature on the relationship between climate change and OSH hazards has continued to grow since 1988. However, many gaps persist, particularly regarding mental and physical health effects on worker exposure to air pollution, UV radiation, risks in the built environment, and inequities. Scenarios must be developed for identifying hazards in geoengineering, and more interventions should be developed to prevent and control the hazards related to vector-borne diseases. Since employers are not accustomed to dealing with climate-related hazards, programs that address employer and worker behaviors will be critical.
Anticipating potential futures and regional variations is necessary for preventing and controlling climate-related occupational hazards. Foresight techniques that predict climate-related OSH hazards can help establish priorities and responsibilities for workers’ safety and health (Daheim et al. Citation2021; Streit et al. Citation2021).
Although there is a growing literature on health equity and climate change, the surveillance data are insufficient for addressing equity issues related to worker exposures and adverse outcomes with regard to race/ethnicity, nativity, immigration status, and language. Researchers must continue assessing the economic costs of climate-related hazards on workers and employers, assess the impact of such hazards on indoor workers, and find new hazard control and risk management interventions employers can use to protect workers. A bolder front must be opened up for surveillance and research to address the needs of workers exposed to climate-related hazards.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
At the time the study was initiated, P.A.S. was employed by the U.S. National Institute for Occupational Safety and Health and then subsequently as a contractor with ATL International, Inc.
Acknowledgments
The authors thank Marc Bovenschulte, Miranda Dally, and Cecilia Sorensen for comments on earlier drafts, Cheryl Hamilton and Seleen Collins for editing, and Rick Colbert and Joanna Taliano for assisting with the literature searches.
References
- American Academy of Allergy Asthma and Immunology [AAAAI] 2020. Does climate change impact allergic disease? [accessed 2021 Jul 28]. https://www.aaaai.org/Tools-for-the-Public/Conditions-Library/Allergies/Does-Climate-Change-Impact-Allergic-Disease.
- Abatayo AL, Bosetti V, Casari M, Ghidoni R, Tavoni M. 2020. Solar geoengineering may lead to excessive cooling and high strategic uncertainty. Proc Natl Acad Sci U S A. 117(24):13393–13398. doi:10.1073/pnas.1916637117
- Acharya P, Boggess B, Zhang K. 2018. Assessing heat stress and health among construction workers in a changing climate: a review. IJERPH. 15(2):247. doi:10.3390/ijerph15020247
- Adam-Poupart A, Drapeau L-M, Bekal S, Germain G, Irace-Cima A, Sassine M-P, Simon A, Soto J, Thivierge K, Tissot F. 2021. Foodborne and animal contact disease outbreaks: occupations at risk of contracting zoonoses of public health significance in Québec. Can Commun Dis Rep. 47(1):47–58. doi:10.14745/ccdr.v47i01a08
- Adam-Poupart A, Labrèche F, Busque MA, Brand A, Duguay P, Fournier M, Zayed J, Smargiassi A. 2015. Association between outdoor ozone and compensated acute respiratory diseases among workers in Quebec (Canada). Ind Health. 53(2):171–175. doi:10.2486/indhealth.2014-0136
- Adetona O, Reinhardt TE, Domitrovich J, Broyles G, Adetona AM, Kleinman MT, Ottmar RD, Naeher LP. 2016. Review of the health effects of wildland fire smoke on wildland firefighters and the public. Inhal Toxicol. 28(3):95–139. doi:10.3109/08958378.2016.1145771
- Anderson VP, Schulte PA, Novakovich J, Pfirman D, Bhattacharya A. 2020. Wholesale and retail trade sector occupational fatal and nonfatal injuries and illnesses from 2006 to 2016: implications for intervention. Am J Ind Med. 63(2):121–134. doi:10.1002/ajim.23063
- Applebaum KM, Graham J, Gray GM, LaPuma P, McCormick SA, Northcross A, Perry MJ. 2016. An overview of occupational risks from climate change. Curr Environ Health Rep. 3(1):13–22. doi:10.1007/s40572-016-0081-4
- Arbury S, Jacklitsch B, Farquah O, Hodgson M, Lamson G, Martin H, Profitt A. 2014. Heat illness and death among workers—United States, 2012–2013. MMWR Morb Mortal Wkly Rep. 63(31):661–665.
- Arcury TA, Summers P, Talton JW, Chen H, Sandberg JC, Johnson CRS, Quandt SA. 2015. Heat illness among North Carolina Latino farmworkers. J Occup Environ Med. 57(12):1299–1304. doi:10.1097/JOM.0000000000000552
- ATSDR. 2022. Environmental justice index. [accessed 2022 Oct 14]. https://www.atsdr.cdc.gov/placeandhealth/eji/index.html.
- Auffhammer M, Mansur ET. 2014. Measuring climatic impacts on energy consumption: a review of the empirical literature. Energy Econ. 46:522–530. doi:10.1016/j.eneco.2014.04.017
- Bais A, McKenzie R, Bernhard G, Aucamp P, Ilyas M, Madronich S, Tourpali K. 2015. Ozone depletion and climate change: impacts on UV radiation. Photochem Photobiol Sci. 14(1):19–52. doi:10.1039/c4pp90032d
- Bakhiyi B, Labreche F, Zayed J. 2014. The photovoltaic industry on the path to a sustainable future–environmental and occupational health issues. Environ Int. 73:224–234. doi:10.1016/j.envint.2014.07.023
- Ball P. 2022. U.S. project readies major milestone toward practical fusion. Scientific American. [accessed 2022 Oct 14]. https://www.scientificamerican.com/article/u-s-project-reaches-major-milestone-toward-practical-fusion-power/
- Barnes PW, Williamson CE, Lucas RM, Robinson SA, Madronich S, Paul ND, Bornman JF, Bais AF, Sulzberger B, Wilson SR, et al. 2019. Ozone depletion, ultraviolet radiation, climate change and prospects for a sustainable future. Nat Sustain. 2(7):569–579. doi:10.1038/s41893-019-0314-2
- Beard CB, Eisen RJ, Barker CM, Garofalo JF, Hahn M, Hayden M, Monaghan AJ, Ogden NH, Schramm PJ. 2016. Ch. 5: vectorborne diseases. The impacts of climate change on human health in the United States: a scientific assessment. Washington (DC): U.S. Global Change Research Program; p. 129–156.
- Beggs PJ. 2014. Impacts of climate change on allergens and allergic diseases: knowledge and highlights from two decades of research. In Butler CD, editor. Climate change and global health. Croydon, UK: CABI. p. 105–113.
- Benedict K, Mody RK. 2016. Epidemiology of histoplasmosis outbreaks, United States, 1938–2013. Emerg Infect Dis. 22(3):370–378. doi:10.3201/eid2203.151117
- Benedict K, Richardson M, Vallabhaneni S, Jackson BR, Chiller T. 2017. Emerging issues, challenges, and changing epidemiology of fungal disease outbreaks. Lancet Infect Dis. 17(12):e403–e411. doi:10.1016/S1473-3099(17)30443-7
- Benevolenza MA, DeRigne L. 2019. The impact of climate change and natural disasters on vulnerable populations: a systematic review of literature. J Hum Behav Soc Environ. 29(2):266–281. doi:10.1080/10911359.2018.1527739
- Betchley C, Koenig JQ, van Belle G, Checkoway H, Reinhardt T. 1997. Pulmonary function and respiratory symptoms in forest firefighters. Am J Ind Med. 31(5):503–509. doi:10.1002/(SICI)1097-0274(199705)31:5<503::AID-AJIM3>3.0.CO;2-U
- Bradbrook S, Duckworth M, Ellwood P, Miedzinski M, Ravetz J, Reynolds J. 2013. Green jobs and occupational safety and health: foresight on new and emerging risks associated with new technologies by 2020. Bilbao (Spain): European Agency for Safety and Health at Work.
- Braun M, Klingelhöfer D, Groneberg DA. 2021. Sooty bark disease of maples: the risk for hypersensitivity pneumonitis by fungal spores not only for woodman. J Occup Med Toxicol. 16(1):2. doi:10.1186/s12995-021-00292-5
- Bromet EJ, Clouston S, Gonzalez A, Kotov R, Guerrera KM, Luft BJ. 2017. Hurricane Sandy exposure and the mental health of World Trade Center responders. J Trauma Stress. 30(2):107–114. doi:10.1002/jts.22178
- Broyles GA. 2013. Wildland firefighter smoke exposure study. Logan, UT: Department of Natural Resources, Utah State University. doi:10.26076/e0a0-f5fa
- Buis A. 2020. How climate change may be impacting storms over Earth’s tropical oceans. NASA Climate; [accessed 2021 Aug 11]. https://climate.nasa.gov/blog/2956/how-climate-change-may-be-impacting-storms-over-earths-tropical-oceans/.
- Bundo M, de Schrijver E, Federspiel A, Luterbacher J, Franco O, Müller T, Vicedo-Cabrera A. 2020. Impact of ambient temperature on mental health in Bern, Switzerland: a time-series study. Eur J Public Health. 30(Suppl_5):ckaa165. 373.
- Burke M, González F, Baylis P, Heft-Neal S, Baysan C, Basu S, Hsiang S. 2018. Higher temperatures increase suicide rates in the United States and Mexico. Nat Clim Change. 8(8):723–729. doi:10.1038/s41558-018-0222-x
- Cal/OSHA. 2005. Title 8, Section 3395. Heat illness prevention in outdoor places of employment.
- California Legislature. 2019. Assembly Bill No. 203 Chapter 712. AB-203 Occupational safety and health: Valley Fever.
- Calkins MM, Bonauto D, Hajat A, Lieblich M, Seixas N, Sheppard L, Spector JT. 2019. A case-crossover study of heat exposure and injury risk among outdoor construction workers in Washington State. Scand J Work Environ Health. 45(6):588–599. doi:10.5271/sjweh.3814
- Caminade C, McIntyre KM, Jones AE. 2019. Impact of recent and future climate change on vector-borne diseases. Ann N Y Acad Sci. 1436(1):157–173. doi:10.1111/nyas.13950
- Campbell-Lendrum D, Manga L, Bagayoko M, Sommerfeld J. 2015. Climate change and vector-borne diseases: what are the implications for public health research and policy? Phil Trans R Soc B. 370(1665):20130552. doi:10.1098/rstb.2013.0552
- Carvalho RB, Carneiro MFH, Barbosa F, Batista BL, Simonetti J, Amantéa SL, Rhoden CR. 2018. The impact of occupational exposure to traffic-related air pollution among professional motorcyclists from Porto Alegre, Brazil, and its association with genetic and oxidative damage. Environ Sci Pollut Res Int. 25(19):18620–18631. doi:10.1007/s11356-018-2007-1
- Casas L, Cox B, Bauwelinck M, Nemery B, Deboosere P, Nawrot TS. 2017. Does air pollution trigger suicide? A case-crossover analysis of suicide deaths over the life span. Eur J Epidemiol. 32(11):973–981. doi:10.1007/s10654-017-0273-8
- Casey J. 2019. Social transition and why it matters in coal mine closure. Mining Technol. https://www.mining-technology.com/features/social-transition-and-why-it-matters-in-coal-mine-closure/.
- CDC. 2019. Fighting the world’s deadliest animal. [accessed 2022 Oct 23]. https://www.cdc.gov/globalhealth/stories/2019/world-deadliest-animal.html.
- CDC. 2020. Evidence on the use of indoor air filtration as an intervention for wildfire smoke pollutant exposure: a summary for health departments. BRACE Technical Report Series.
- CDC. 2021a. Lyme disease recent surveillance data. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; [accessed 2021 Jul 28]. https://www.cdc.gov/lyme/datasurveillance/recent-surveillance-data.html.
- CDC. 2021b. One Health. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; [accessed 2021 Jul 28]. https://www.cdc.gov/onehealth/index.html.
- Cherrie JW, Nioi A, Wendelboe-Nelson C, Cowan S, Cherrie M, Rashid S, Cowie H, Ritchie P, Lansdown TC. 2021. Exposure to solar UV during outdoor construction work in Britain. Ann Work Expo Health. 65(2):176–182. doi:10.1093/annweh/wxaa028
- Cho K, Lee S. 1978. Occupational health hazards of mine workers. Bull World Health Organ. 56(2):205–218.
- Cho R. 2021. Attribution science: linking climate change to extreme weather. Columbia Climate School State of the Planet. https://news.climate.columbia.edu/2021/10/04/attribution-science-linking-climate-change-to-extreme-weather/.
- Choi YJ, Lee KS, Oh JW. 2021. The impact of climate change on pollen season and allergic sensitization to pollens. Immunol Allergy Clin North Am. 41(1):97–109. doi:10.1016/j.iac.2020.09.004
- Claudio L, Rivera GA, Ramirez OF. 2016. Association between markers of classroom environmental conditions and teachers’ respiratory health. J Sch Health. 86(6):444–451. doi:10.1111/josh.12398
- Clayton S, Manning CM, Speiser M, Hill AN. 2021. Mental health and our changing climate: impacts, inequities, responses. Washington (DC): American Psychological Association, and ecoAmerica.
- Constible J, Chang B, Morganelli C, Blandon N. 2020. On the frontlines: climate change threatens the health of America’s workers. New York (NY): Natural Resources Defense Council (NRDC).
- Cruz J, White PCL, Bell A, Coventry PA. 2020. Effect of extreme weather events on mental health: a narrative synthesis and meta-analysis for the UK. Int J Environ Res Public Health. 17(22):8581. doi:10.3390/ijerph17228581
- D'Amato G, Chong-Neto HJ, Monge Ortega OP, Vitale C, Ansotegui I, Rosario N, Haahtela T, Galan C, Pawankar R, Murrieta-Aguttes M, et al. 2020. The effects of climate change on respiratory allergy and asthma induced by pollen and mold allergens. Allergy. 75(9):2219–2228. doi:10.1111/all.14476
- D'Amato G, Pawankar R, Vitale C, Lanza M, Molino A, Stanziola A, Sanduzzi A, Vatrella A, D'Amato M. 2016. Climate change and air pollution: effects on respiratory allergy. Allergy Asthma Immunol Res. 8(5):391–395. doi:10.4168/aair.2016.8.5.391
- D'Amato M, Cecchi L, Annesi-Maesano I, D Amato G. 2018. News on climate change, air pollution, and allergic triggers of asthma. J Investig Allergol Clin Immunol. 28(2):91–97. doi:10.18176/jiaci.0228
- D'Ovidio MC, Annesi-Maesano I, D'Amato G, Cecchi L. 2016. Climate change and occupational allergies: an overview on biological pollution, exposure and prevention. Ann Ist Super Sanita. 52(3):406–414.
- Daghagh Yazd S, Wheeler SA, Zuo A. 2019. Key risk factors affecting farmers’ mental health: a systematic review. Int J Environ Res Public Health. 16(23):4849. doi:10.3390/ijerph16234849
- Daheim C, Prendergast J, Rampacher J, Désaunay C. 2021. Foresight study on the circular economy and its effects on occupational safety and health. Phase 1: macro-scenarios. Bilbao (Spain): European Agency for Safety and Health at Work.
- Dahl K, Licker R, Abatzoglou JT, Declet-Barreto J. 2019a. Increased frequency of and population exposure to extreme heat index days in the United States during the 21st century. Environ Res Commun. 1(7):075002. doi:10.1088/2515-7620/ab27cf
- Dahl K, Spanger-Siegfried E, Licker R, Caldas A, Abatzoglou J, Mailloux N, Cleetus R, Udvardy S, Declet-Barreto J, Worth P. 2019b. Killer heat in the United States: climate choices and the future of dangerously hot days. Cambridge (MA): Union of Concerned Scientists.
- Dasgupta S, van Maanen N, Gosling SN, Piontek F, Otto C, Schleussner C-F. 2021. Effects of climate change on combined labour productivity and supply: an empirical, multi-model study. Lancet Planet Health. 5(7):e455–e465. doi:10.1016/S2542-5196(21)00170-4
- de Perio MA, Materna BL, Sondermeyer Cooksey GL, Vugia DJ, Su CP, Luckhaupt SE, McNary J, Wilken JA. 2019. Occupational coccidioidomycosis surveillance and recent outbreaks in California. Med Mycol. 57(Supplement_1):S41–S45. doi:10.1093/mmy/myy031
- Delp L, Podolsky L, Aguilar T. 2009. Risk amid recovery: occupational health and safety of Latino day laborers in the aftermath of the Gulf Coast hurricanes. Organ Environ. 22(4):479–490. doi:10.1177/1086026609347193
- Demain JG. 2018. Climate change and the impact on respiratory and allergic disease: 2018. Curr Allergy Asthma Rep. 18(4):22. doi:10.1007/s11882-018-0777-7
- Deng SZ, Jalaludin BB, Anto JM, Hess JJ, Huang CR. 2020. Climate change, air pollution, and allergic respiratory diseases: a call to action for health professionals. Chin Med J (Engl). 133(13):1552–1560. doi:10.1097/CM9.0000000000000861
- Deschênes O, Greenstone M. 2011. Climate change, mortality, and adaptation: evidence from annual fluctuations in weather in the US. Am Econ J Appl Econ. 3(4):152–185. doi:10.1257/app.3.4.152
- Dillender M. 2021. Climate change and occupational health are there limits to our ability to adapt? J Hum Res. 56(1):184–224. doi:10.3368/jhr.56.1.0718-9594R3
- Dodgen D, Donato D, Kelly N, La Greca A, Morganstein J, Reser J, Ruzek J, Schweitzer S, Shimamoto M, Tart KT, et al. 2016. Ch. 8: Mental health and well-being. Washington (DC): US Global Change Research Program.
- Donato KM, Trujillo-Pagan N, Bankston CL, III, Singer A. 2007. Reconstructing New Orleans after Katrina: the emergence of an immigrant labor market. In: Brunsma DOD, Picou S editor. The sociology of Katrina: perspectives on a modern catastrophe. Landham (MD): Rowman & Littlefield Publishers; p. 217–234.
- Dong XS, West GH, Holloway‐Beth A, Wang X, Sokas RK. 2019. Heat‐related deaths among construction workers in the United States. Am J Ind Med. 62(12):1047–1057. doi:10.1002/ajim.23024
- Downs JW, Cumpston KL, Feldman MJ. 2019. Giant hogweed phytophotodermatitis. Clin Toxicol (Phila). 57(9):822–823. doi:10.1080/15563650.2018.1559327
- Du C, Li B, Yu W. 2021. Indoor mould exposure: characteristics, influences and corresponding associations with built environment—a review. J Build Eng. 35:101983. doi:10.1016/j.jobe.2020.101983
- Duroha JC, Brownson JRS, Macht GA. 2020. Occupational risks associated with solar installations: a review. In: Proceedings of the American Solar Energy Society National Solar Conference 2020 Proceedings. p. 49–55.
- Effiong U, Neitzel RL. 2016. Assessing the direct occupational and public health impacts of solar radiation management with stratospheric aerosols. Environ Health. 15:7. doi:10.1186/s12940-016-0089-0
- Eguiluz-Gracia I, Mathioudakis AG, Bartel S, Vijverberg SJH, Fuertes E, Comberiati P, Cai YS, Tomazic PV, Diamant Z, Vestbo J, et al. 2020. The need for clean air: the way air pollution and climate change affect allergic rhinitis and asthma. Allergy. 75(9):2170–2184. doi:10.1111/all.14177
- Eisen RJ, Eisen L, Ogden NH, Beard CB. 2016. Linkages of weather and climate with ixodes scapularis and Ixodes pacificus (Acari: Ixodidae), enzootic transmission of Borrelia burgdorferi, and Lyme disease in North America. J Med Entomol. 53(2):250–261. doi:10.1093/jme/tjv199
- Ellis BD, Stam HJ. 2018. Cycles of deportability: threats, fears, and the agency of ‘irregular’ migrants in Canada. Migr Stud. 6(3):321–344. doi:10.1093/migration/mnx049
- EPA. 2020. Review of the ozone national ambient air quality standards. 85 FR 87256. 87256–87351.
- Fan W, Qian Y. 2017. Native-immigrant occupational segregation and worker health in the United States, 2004–2014. Soc Sci Med. 183:130–141. doi:10.1016/j.socscimed.2017.04.029
- Fann N, Nolte CG, Dolwick P, Spero TL, Brown AC, Phillips S, Anenberg S. 2015. The geographic distribution and economic value of climate change-related ozone health impacts in the United States in 2030. J Air Waste Manag Assoc. 65(5):570–580. doi:10.1080/10962247.2014.996270
- Federal Ministry for Economic Affairs and Energy. 2020. The national hydrogen economy. Berlin (Germany): The National Hydrogen Economy.
- Finnis J, Shewmake JW, Neis B, Telford D. 2019. Marine forecasting and fishing safety: improving the fit between forecasts and harvester needs. J Agromedicine. 24(4):324–332. doi:10.1080/1059924X.2019.1639576
- Fitzgerald KC, Pit SW, Rolfe M, McKenzie J, Matthews V, Longman J, Bailie R. 2020. Cross sectional analysis of depression amongst Australian rural business owners following cyclone-related flooding. J Occ Med Toxicol. 15:12.
- Flynn MA. 2014. Safety & the diverse workforce: lessons from NIOSH’s work with Latino immigrants. Prof Saf. 59(6):52–57.
- Flynn MA, Carreón T, Eggerth DE, Johnson AI. 2014. Immigration, work, and health: a literature review of immigration between Mexico and the United States. Revista Trab Soc. 6:129–149.
- Fouque F, Reeder JC. 2019. Impact of past and on-going changes on climate and weather on vector-borne diseases transmission: a look at the evidence. Infect Dis Poverty. 8(1):51. doi:10.1186/s40249-019-0565-1
- Freedman M, Jackson BR, McCotter O, Benedict K. 2018. Coccidioidomycosis outbreaks, United States and worldwide, 1940-2015. Emerg Infect Dis. 24(3):417–423. doi:10.3201/eid2403.170623
- Freiberg A, Schefter C, Girbig M, Murta VC, Seidler A. 2018. Health effects of wind turbines in working environments – a scoping review. Scand J Work Environ Health. 44(4):351–369. doi:10.5271/sjweh.3711
- Freire FDCO, da Rocha MEB. 2016. Impact of Mycotoxins on Human Health. In: Mérillon J-M, Ramawat KG, editors. Fungal metabolites. Cham (Switzerland): Springer International Publishing; p. p. 1–23.
- Gatto MP, Cabella R, Gherardi M. 2016. Climate change: the potential impact on occupational exposure to pesticides. Ann Ist Super Sanita. 52(3):374–385.
- Gifford B. 2018. Views: How climate change is impacting mental health—and what employers can do. Employee Benefit News; [accessed]. https://www.benefitnews.com/opinion/how-climate-change-is-impacting-mental-health-and-what-employers-can-do.
- Glaser J, Lemery J, Rajagopalan B, Diaz HF, García-Trabanino R, Taduri G, Madero M, Amarasinghe M, Abraham G, Anutrakulchai S, et al. 2016. Climate change and the emergent epidemic of CKD from heat stress in rural communities: the case for heat stress nephropathy. Clin J Am Soc Nephrol. 11(8):1472–1483. doi:10.2215/CJN.13841215
- Gnat S, Łagowski D, Nowakiewicz A, Dyląg M. 2021. A global view on fungal infections in humans and animals: infections caused by dimorphic fungi and dermatophytoses. J Appl Microbiol. 131(6):2688–2704. doi:10.1111/jam.15084
- Gorris ME, Treseder KK, Zender CS, Randerson JT. 2019. Expansion of Coccidioidomycosis endemic regions in the United States in response to climate change. Geohealth. 3(10):308–327. doi:10.1029/2019GH000209
- Grinn-Gofroń A, Nowosad J, Bosiacka B, Camacho I, Pashley C, Belmonte J, De Linares C, Ianovici N, Manzano JMM, Sadyś M, et al. 2019. Airborne Alternaria and Cladosporium fungal spores in Europe: forecasting possibilities and relationships with meteorological parameters. Sci Total Environ. 653:938–946. doi:10.1016/j.scitotenv.2018.10.419
- Groot E, Caturay A, Khan Y, Copes R. 2019. A systematic review of the health impacts of occupational exposure to wildland fires. Int J Occ Med Environ Health. 32(2):121–140.
- Gubernot DM, Anderson GB, Hunting KL. 2015. Characterizing occupational heat‐related mortality in the United States, 2000–2010: an analysis using the Census of Fatal Occupational Injuries database. Am J Ind Med. 58(2):203–211. doi:10.1002/ajim.22381
- Gutarowska B, Skóra J, Stępień L, Twarużek M, Błajet-Kosicka A, Otlewska A, Grajewski J. 2014. Estimation of fungal contamination and mycotoxin production at workplaces in composting plants, tanneries, archives and libraries. World Mycotoxin J. 7(3):345–355. doi:10.3920/WMJ2013.1640
- Habschied K, Kanizai Saric G, Krstanovic V, Mastanjevic K. 2021. Mycotoxins-biomonitoring and human exposure. Toxins (Basel). 13(2):113. doi:10.3390/toxins13020113
- Hanigan IC, Schirmer J, Niyonsenga T. 2018. Drought and distress in southeastern Australia. Ecohealth. 15(3):642–655. doi:10.1007/s10393-018-1339-0
- Hargreaves S, Rustage K, Nellums LB, McAlpine A, Pocock N, Devakumar D, Aldridge RW, Abubakar I, Kristensen KL, Himmels JW, et al. 2019. Occupational health outcomes among international migrant workers: a systematic review and meta-analysis. Lancet Glob Health. 7(7):e872–e882. doi:10.1016/S2214-109X(19)30204-9
- Hault K, Rönsch H, Beissert S, Knuschke P, Bauer A. 2016. Knowledge of outdoor workers on the effects of natural UV radiation and methods of protection against exposure. J Eur Acad Dermatol Venereol. 30(S3):34–37. doi:10.1111/jdv.13631
- Hayes K, Blashki G, Wiseman J, Burke S, Reifels L. 2018. Climate change and mental health: risks, impacts and priority actions. Int J Ment Health Sys. 12(1):1–12.
- Hesketh M, Wuellner S, Robinson A, Adams D, Smith C, Bonauto D. 2020. Heat related illness among workers in Washington State: a descriptive study using workers’ compensation claims, 2006‐2017. Am J Ind Med. 63(4):300–311. doi:10.1002/ajim.23092
- Howard M, Ahmed S, Lachapelle P, Schure MB. 2020. Farmer and rancher perceptions of climate change and their relationships with mental health. J Rural Ment Health. 44(2):87–95. doi:10.1037/rmh0000131
- Hrabok M, Delorme A, Agyapong VI. 2020. Threats to mental health and well-being associated with climate change. J Anxiety Disord. 76:102295. doi:10.1016/j.janxdis.2020.102295
- Huang G, Zhou W, Cadenasso M. 2011. Is everyone hot in the city? Spatial pattern of land surface temperatures, land cover and neighborhood socioeconomic characteristics in Baltimore, MD. J Environ Manage. 92(7):1753–1759. doi:10.1016/j.jenvman.2011.02.006
- Hunter LM, Luna JK, Norton RM. 2015. Environmental dimensions of migration. Annu Rev Sociol. 41:377–397. doi:10.1146/annurev-soc-073014-112223
- [IAEA] International Atomic Energy Agency. 2021. Energy, electricity and nuclear power estimates for the period up to 2050. Reference Data Series No. 1. Vienna, Austria.
- IPCC. 2021. Summary for policymakers. Cambridge University Press, Cambridge (United Kingdom) and New York (NY): (Climate Change 2021: The Physical Science Basis Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change).
- Johanning E, Auger P, Morey PR, Yang CS, Olmsted E. 2014. Review of health hazards and prevention measures for response and recovery workers and volunteers after natural disasters, flooding, and water damage: mold and dampness. Environ Health Prev Med. 19(2):93–99. doi:10.1007/s12199-013-0368-0
- Jones AC, Haywood JM, Dunstone N, Emanuel K, Hawcroft MK, Hodges KI, Jones A. 2017. Impacts of hemispheric solar geoengineering on tropical cyclone frequency. Nat Commun. 8(1):1382. doi:10.1038/s41467-017-01606-0
- Karanikas N, Steele S, Bruschi K, Robertson C, Kass J, Popovich A, MacFadyen C. 2021. Occupational health hazards and risks in the wind industry. Energy Rep. 7:3750–3759. doi:10.1016/j.egyr.2021.06.066
- Karita K, Yano E, Jinsart W, Boudoung D, Tamura K. 2001. Respiratory symptoms and pulmonary function among traffic police in Bangkok, Thailand. Arch Environ Health. 56(5):467–470. doi:10.1080/00039890109604484
- Katelaris CH. 2021. Climate change and extreme weather events in Australia: impact on allergic diseases. Immunol Allergy Clin North Am. 41(1):53–62. doi:10.1016/j.iac.2020.09.003
- Katelaris CH, Beggs PJ. 2018. Climate change: allergens and allergic diseases. Intern Med J. 48(2):129–134. doi:10.1111/imj.13699
- Khanzode VV, Maiti J, Ray P. 2011. A methodology for evaluation and monitoring of recurring hazards in underground coal mining. Saf Sci. 49(8-9):1172–1179. doi:10.1016/j.ssci.2011.03.009
- Kiefer M, Rodríguez-Guzmán J, Watson J, van Wendel de Joode B, Mergler D, da Silva AS. 2016. Worker health and safety and climate change in the Americas: issues and research needs. Rev Panam Salud Pública. 40(3):192–197.
- Kim D, Lee J. 2020. Spatial changes in work capacity for occupations vulnerable to heat stress: potential regional impacts from global climate change. Saf Health Work. 11(1):1–9. doi:10.1016/j.shaw.2019.10.004
- Kingsolver A. 2011. Worker well‐being: uniting economic, environmental, and social justice concerns in the anthropology of work. Anthropol Work Rev. 32(1):2–3. doi:10.1111/j.1548-1417.2011.01051.x
- Kinney PL. 2018. Interactions of climate change, air pollution, and human health. Curr Environ Health Rep. 5(1):179–186. doi:10.1007/s40572-018-0188-x
- Kjellstrom T, Holmer I, Lemke B. 2009. Workplace heat stress, health and productivity–an increasing challenge for low and middle-income countries during climate change. Glob Health Action. 2(1):2047. doi:10.3402/gha.v2i0.2047
- Kjellstrom T, Maître N, Saget C, Otto M, Karimova T. 2019. Working on a warmer planet: the impact of heat stress on labour productivity and decent work. Geneva (Switzerland): International Labor Organization.
- Klimaszyk P, Klimaszyk D, Piotrowiak M, Popiolek A. 2014. Unusual complications after occupational exposure to giant hogweed (Heracleum mantegazzianum): a case report. Int J Occup Med Environ Health. 27(1):141–144.
- Klinenberg E. 2015. Heat wave: a social autopsy of disaster in Chicago. Chicago (IL): University of Chicago Press.
- Knutson T, Camargo SJ, Chan JCL, Emanuel K, Ho C-H, Kossin J, Mohapatra M, Satoh M, Sugi M, Walsh K, et al. 2020. Tropical cyclones and climate change assessment: part II: projected response to anthropogenic warming. Bull Am Meteor Soc. 101(3):E303–E322. doi:10.1175/BAMS-D-18-0194.1
- Knutson T, Kossin J, Mears C, Perlwitz J, Wehner M. 2017. Ch. 3: Detection and attribution of climate change. Washington (DC): U.S. Global Change Research Program.
- Kugeler KJ, Schwartz AM, Delorey MJ, Mead PS, Hinckley AF. 2021. Estimating the frequency of Lyme disease diagnoses, United States, 2010–2018. Emerg Infect Dis. 27(2):616–619. doi:10.3201/eid2702.202731
- Langer CE, Mitchell DC, Armitage TL, Moyce SC, Tancredi DJ, Castro J, Vega-Arroyo AJ, Bennett DH, Schenker MB. 2021. Are Cal/OSHA regulations protecting farmworkers in California from heat-related illness? J Occup Environ Med. 63(6):532–539. doi:10.1097/JOM.0000000000002189
- Larrañaga MD, Wang Q. 2012. Heat stress. In: Bingham E and Cohrssen B, editors. Patty’s Toxicology. 6th ed. New York (NY): John Wiley and Sons; p. 37–78.
- Lee KS, Kim K, Choi YJ, Yang S, Kim CR, Moon JH, Kim KR, Lee YS, Oh JW. 2021. Increased sensitization rates to tree pollens in allergic children and adolescents and a change in the pollen season in the metropolitan area of Seoul, Korea. Pediatr Allergy Immunol. 32(5):872–879. doi:10.1111/pai.13472
- Leigh JP. 2011. Economic burden of occupational injury and illness in the United States. Milbank Q. 89(4):728–772. doi:10.1111/j.1468-0009.2011.00648.x
- Levi M, Kjellstrom T, Baldasseroni A. 2018. Impact of climate change on occupational health and productivity: a systematic literature review focusing on workplace heat. Med Lav. 109(3):163–179.
- Levy B, Patz J. 2015a. Climate change and public health. Oxford (UK): Oxford University Press.
- Levy B, Patz J. 2015b. Climate change, human rights, and social justice. Ann Glob Health. 81(3):310–322. doi:10.1016/j.aogh.2015.08.008
- Li M, Ferreira S, Smith TA. 2020. Temperature and self-reported mental health in the United States. PLoS One. 15(3):e0230316. doi:10.1371/journal.pone.0230316
- Licker R, Dahl K, Abatzoglou JT. 2022. Quantifying the impact of future extreme heat on the outdoor work sector in the United States. Elem Sci Anth. 10(1):00048.
- Limaye V. 2020. The public health cost of climate change is already in the billions. New York (NY): Natural Resources Defense Council (NRDC).
- Limaye V. 2021. The costs of inaction: the economic burden of fossil fuels and climate change on health in the United States. New York (NY): Natural Resources Defense Council (NRDC).
- Lowe SR, Kwok RK, Payne J, Engel LS, Galea S, Sandler DP. 2016. Why does disaster recovery work influence mental health?: Pathways through physical health and household income. Am J Community Psychol. 58(3-4):354–364. doi:10.1002/ajcp.12091
- Lucas DL, Case SL, Lincoln JM, Watson JR. 2018. Factors associated with crewmember survival of cold water immersion due to commercial fishing vessel sinkings in Alaska. Saf Sci. 101:190–196. doi:10.1016/j.ssci.2017.09.009
- Maitre N, Monh G, Saget C. 2018. The employment impact of climate change adaptation. Geneva (Switzerland): International Labour Office.
- Marinucci GD, Luber G, Uejio CK, Saha S, Hess JJ. 2014. Building resilience against climate effects—a novel framework to facilitate climate readiness in public health agencies. Int J Environ Res Public Health. 11(6):6433–6458. doi:10.3390/ijerph110606433
- Markandya A, Wilkinson P. 2007. Electricity generation and health. Lancet. 370(9591):979–990. doi:10.1016/s0140-6736(07)61253-7
- Marroquin-Cardona AG, Johnson NM, Phillips TD, Hayes AW. 2014. Mycotoxins in a changing global environment–a review. Food Chem Toxicol. 69:220–230. doi:10.1016/j.fct.2014.04.025
- Mera R, Massey N, Rupp DE, Mote P, Allen M, Frumhoff PC. 2015. Climate change, climate justice and the application of probabilistic event attribution to summer heat extremes in the California Central Valley. Clim Change. 133(3):427–438. doi:10.1007/s10584-015-1474-3
- Metregiste D, Boucaud-Maitre D, Aubert L, Noubou L, Jehel L. 2020. Explanatory factors of post-traumatic distress and burnout among hospital staff 6 months after Hurricane Irma in Saint-Martin and Saint-Barthelemy. PLoS One. 15(3):e0229246. doi:10.1371/journal.pone.0229246
- Mette J, Velasco Garrido M, Harth V, Preisser AM, Mache S. 2018. Healthy offshore workforce? A qualitative study on offshore wind employees’ occupational strain, health, and coping. BMC Public Health. 18(1):172. doi:10.1186/s12889-018-5079-4
- Miranda AI, Martins V, Cascão P, Amorim JH, Valente J, Borrego C, Ferreira AJ, Cordeiro CR, Viegas DX, Ottmar R. 2012. Wildland smoke exposure values and exhaled breath indicators in firefighters. J Toxicol Environ Health A. 75(13-15):831–843. doi:10.1080/15287394.2012.690686
- Moda HM, Filho WL, Minhas A. 2019. Impacts of climate change on outdoor workers and their safety: some research priorities. Int J Environ Res Public Health. 16(18):3458. doi:10.3390/ijerph16183458
- Monaghan AJ, Moore SM, Sampson KM, Beard CB, Eisen RJ. 2015. Climate change influences on the annual onset of Lyme disease in the United States. Ticks Tick Borne Dis. 6(5):615–622. doi:10.1016/j.ttbdis.2015.05.005
- Morris CE, Gonzales RG, Hodgson MJ, Tustin AW. 2019. Actual and simulated weather data to evaluate wet bulb globe temperature and heat index as alerts for occupational heat-related illness. J Occup Environ Hyg. 16(1):54–65. doi:10.1080/15459624.2018.1532574
- Morrissey MC, Casa DJ, Brewer GJ, Adams WM, Hosokawa Y, Benjamin CL, Grundstein AJ, Hostler D, McDermott BP, McQuerry ML, et al. 2021. Heat safety in the workplace: modified Delphi consensus to establish strategies and resources to protect the US workers. Geohealth. 5(8):e2021GH000443. doi:10.1029/2021GH000443
- Moyce SC, Schenker M. 2017. Occupational exposures and health outcomes among immigrants in the USA. Curr Environ Health Rep. 4(3):349–354. doi:10.1007/s40572-017-0152-1
- Muhammad NS, Jalaludin J, Sundrasegaran S 2014. Exposure to respirable dust (PM10) and respiratory health among traffic policemen in Selangor. Adv Environ Biol. 8(15):199–206.
- [NIEHS] National Institute of Environmental Health Sciences. 2015. Climate change vulnerability assessment: a report assessing how climate change will impact worker helath and how to prepare for these impacts. Wahington, D.C.: National Clearinghouse for Worker Safety and Health Training.
- [NIEHS] National Institute of Environmental Health Sciences. 2022. Climate change vulnerability assessment: a report on assessing how climate change impacts worker health and how to prepare for these impacts. Washington, D.C.: National Clearinghouse for Worker Safety and Health Training.
- National Research Council. 2010. Hidden costs of energy: unpriced consequences of energy production and use. Washington (DC): National Academies Press.
- National Wildfire Coordinating Group. 2013. 6 Minutes for Safety; [accessed 2021 Sep 9]. https://www.nwcg.gov/committees/6-Minutes-for-safety.
- Neal A. 2020. Issue brief: how coal country can adapt to the energy transition. Washington, D.C.: Environmental and Energy Study Institute.
- Neidell M, Graff Zivin J, Sheahan M, Willwerth J, Fant C, Sarofim M, Martinich J. 2021. Temperature and work: time allocated to work under varying climate and labor market conditions. PLoS One. 16(8):e0254224. doi:10.1371/journal.pone.0254224
- NIOSH. 2004. Histoplasmosis, Protecting Workers at Risk. By Lenhart SW, Schafer MP, Singal M, Hajjeh RA. Cincinnati, OH: U.S. Department of Health And Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, National Center for Infectious Diseases, In: DHHS (NIOSH) Publication No. 2005–109.
- NIOSH. 2011. Coal mine dust exposures and associated health outcomes. A review of information published since 1995. Cincinnati (OH): U.S. Department of Health And Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health,: Centers for Disease Control, DHHS (NIOSH) Publication No. 2011–172.
- NIOSH 2016. Criteria for a recommended standard: occupational exposure to heat and hot environments. Rev. 2016. By: Jacklitsch B, Williams J, Musolin K, Coca A, Kim J-H, Turner N. Cincinnati (OH): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication 2016–106.
- NIOSH. 2021. Hazards to outdoor workers. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; [accessed 2021 Aug 28]. https://www.cdc.gov/niosh/topics/outdoor/default.html.
- NOAA NCEI. 2022. Billion-dollar weather and climate disasters. National Oceanic and Atmospheric Administration, National Centers for Environmental Information; [accessed 2022 Feb 7]. https://www.ncdc.noaa.gov/billions/overview.
- NWS. 2020. Weather-Ready Nation Strategic Plan (2019–2022); [accessed 2021 Sept9]. https://www.weather.gov/news/192203-strategic-plan.
- O'Connor T, Flynn M, Weinstock D, Zanoni J. 2014. Occupational safety and health education and training for underserved populations. New Solut. 24(1):83–106. doi:10.2190/NS.24.1.d
- Occupational Health and Safety. 2019. OSHA reminds employers to protect employees from CA wildfire Wmoke; [accessed 2021 Sep 10]. https://ohsonline.com/articles/2019/11/01/osha-reminds-employers-to-protect-employees-from-ca-wildfire-smoke.aspx.
- Ocean Studies Board. 2015a. intervention: carbon dioxide removal and reliable sequestration. Washington (DC): National Academies Press.
- Ocean Studies Board. 2015b. Climate intervention: reflecting sunlight to cool the Earth. Washington (DC): National Academies Press.
- Ogden N. 2017. Climate change and vector-borne diseases of public health significance. FEMS Microbiol Lett. 364(19):1–8. doi:10.1093/femsle/fnx186
- Ogden N, Lindsay L. 2016. Effects of climate and climate change on vectors and vector-borne diseases: ticks are different. Trends Parasitol. 32(8):646–656. doi:10.1016/j.pt.2016.04.015
- Ogden NH, Ben Beard C, Ginsberg HS, Tsao JI. 2021. Possible effects of climate change on ixodid ticks and the pathogens they transmit: Predictions and observations. J Med Entomol. 58(4):1536–1545. doi:10.1093/jme/tjaa220
- Oregon OSHA. 2021. Heat illness prevention rule 437-002-0155 and 437-004-1130. Salem, OR: Oregon Occupational Safety and Health.
- Orlov A, Sillmann J, Aaheim A, Aunan K, de Bruin K. 2019. Economic losses of heat-induced reductions in outdoor worker productivity: a case study of Europe. EconDisCliCha. 3(3):191–211. doi:10.1007/s41885-019-00044-0
- Orui M, Suzuki Y, Goto A, Yasumura S. 2018. Factors associated with maintaining the mental health of employees after the Fukushima Nuclear Disaster: findings from companies located in the evacuation area. Int J Environ Res Public Health. 15(1):53. doi:10.3390/ijerph15010053
- OSHA. 2021. Heat injury and illness prevention in outdoor and indoor work settings. Docket No. OSHA-2021-0009. Fed Reg. p. 59309–59326.
- OSHA 2022. OSHA permissible exposure limit (PEL) for general industry. Limits for air contaminants. 29 CFR 1910.1000 Table Z-1. Washington (DC): U.S. Department of Labor, Occupational Safety and Health Administration.
- Pal G, Patel T, Banik T. 2021. Effect of climate change associated hazards on agricultural workers and approaches for assessing heat stress and its mitigation strategies–review of some research significances. Int J Curr Microbiol Appl Sci. 10(2):2947–2975. doi:10.20546/ijcmas.2021.1002.325
- Palinkas LA. 2020. Global climate change, population displacement, and public health: the next wave of migration. Cham (Switzerland): Springer Nature.
- Park J, Pankratz N, Behrer A. 2021. Temperature, workplace safety, and labor market inequality. IZA DP No. 14560. Bonn, Germany: Institute of Labor Economics. doi:10.2139/ssrn.3892588
- Parker ER. 2021. The influence of climate change on skin cancer incidence–a review of the evidence. Int J Womens Dermatol. 7(1):17–27. doi:10.1016/j.ijwd.2020.07.003
- Pawankar R, Wang JY. 2021. Climate change, air pollution, and biodiversity in Asia Pacific and impact on respiratory allergies. Immunol Allergy Clin North Am. 41(1):63–71. doi:10.1016/j.iac.2020.09.008
- Pearson D, Ebisu K, Wu X, Basu R. 2019. A review of coccidioidomycosis in California: exploring the intersection of land use, population movement, and climate change. Epidemiol Rev. 41(1):145–157. doi:10.1093/epirev/mxz004
- Peters CE, Tenkate T, Heer E, O'Reilly R, Kalia S, Koehoorn MW. 2020. Strategic task and break timing to reduce ultraviolet radiation exposure in outdoor workers. Front Public Health. 8:354. doi:10.3389/fpubh.2020.00354
- Pinkerton KE, Felt E, Riden HE. 2019. Extreme weather resulting from global warming is an emerging threat to farmworker health and safety. J Agric Saf Health. 25(4):189–190. doi:10.13031/jash.13555
- Poole JA, Barnes CS, Demain JG, Bernstein JA, Padukudru MA, Sheehan WJ, Fogelbach GG, Wedner J, Codina R, Levetin E, et al. 2019. Impact of weather and climate change with indoor and outdoor air quality in asthma: a work group report of the AAAAI Environmental Exposure and Respiratory Health Committee. J Allergy Clin Immunol. 143(5):1702–1710. doi:10.1016/j.jaci.2019.02.018
- Pradhan B, Kjellstrom T, Atar D, Sharma P, Kayastha B, Bhandari G, Pradhan PK. 2019. Heat stress impacts on cardiac mortality in Nepali migrant workers in Qatar. Cardiology. 143(1-2):37–48. doi:10.1159/000500853
- Pugatch T. 2019. Tropical storms and mortality under climate change. World Dev. 117:172–182. doi:10.1016/j.worlddev.2019.01.009
- Pundee R, Kongtip P, Nankongnab N, Anutrakulchai S, Robson MG, Woskie S. 2021. Cross-shift change of acute kidney injury biomarkers in sugarcane farmers and cutters. Hum Ecol Risk Assess. 27(5):1170–1187. doi:10.1080/10807039.2020.1812049
- Rice MB, Henderson SB, Lambert AA, Cromar KR, Hall JA, Cascio WE, Smith PG, Marsh BJ, Coefield S, Balmes JR, et al. 2021. Respiratory impacts of wildland fire smoke: future challenges and policy opportunities. An official American Thoracic Society Workshop report. Ann Am Thorac Soc. 18(6):921–930. doi:10.1513/AnnalsATS.202102-148ST
- Richardson DB, Cardis E, Daniels RD, Gillies M, O'Hagan JA, Hamra GB, Haylock R, Laurier D, Leuraud K, Moissonnier M, et al. 2015. Risk of cancer from occupational exposure to ionising radiation: retrospective cohort study of workers in France, the United Kingdom, and the United States (INWORKS). BMJ. 351:h5359. doi:10.1136/bmj.h5359
- Rivikin C, Burgess R, Buttner W. 2015. Hydrogen technologies safety guide. Technical report, NREL/TP5400-6094. Golden (CO): National Renewable Energy Laboratory.
- Roscoe RJ, Deddens JA, Salvan A, Schnorr TM. 1995. Mortality among Navajo uranium miners. Am J Public Health. 85(4):535–540. doi:10.2105/ajph.85.4.535
- Rosenberg R, Lindsey NP, Fischer M, Gregory CJ, Hinckley AF, Mead PS, Paz-Bailey G, Waterman SH, Drexler NA, Kersh GJ, et al. 2018. Vital signs: trends in reported vectorborne disease cases - United States and territories, 2004-2016. MMWR Morb Mortal Wkly Rep. 67(17):496–501. doi:10.15585/mmwr.mm6717e1
- Schifano P, Asta F, Marinaccio A, Bonafede M, Davoli M, Michelozzi P. 2019. Do exposure to outdoor temperatures, NO2 and PM10 affect the work-related injuries risk? A case-crossover study in three Italian cities, 2001–2010. BMJ Open. 9(8):e023119. doi:10.1136/bmjopen-2018-023119
- Schindler S, Rabitsch W, Essl F, Wallner P, Lemmerer K, Follak S, Hutter HP. 2018. Alien species and human health: Austrian stakeholder perspective on challenges and solutions. Int J Environ Res Public Health. 15(11):2527. doi:10.3390/ijerph15112527
- Schramm P, Brown C, Saha S, Conlon K, Manangan A, Bell J, Hess J. 2021. A systematic review of the effects of temperature and precipitation on pollen concentrations and season timing, and implications for human health. Int J Biometeorol. 65(10):1615–1628. doi:10.1007/s00484-021-02128-7
- Schulte PA, Bhattacharya A, Butler C, Chun H, Jacklitsch B, Jacobs T, Kiefer M, Lincoln J, Pendergrass S, Shire J, et al. 2016. Advancing the framework for considering the effects of climate change on worker safety and health. J Occup Environ Hyg. 13(11):847–865. doi:10.1080/15459624.2016.1179388
- Schulte PA, Chun H. 2009. Climate change and occupational safety and health: establishing a preliminary framework. J Occup Environ Hyg. 6(9):542–554. doi:10.1080/15459620903066008
- Schulte PA, Streit JM, Sheriff F, Delclos G, Felknor SA, Tamers SL, Fendinger S, Grosch J, Sala R. 2020. Potential scenarios and hazards in the work of the future: a systematic review of the peer-reviewed and gray literatures. Ann Work Expo Health. 64(8):786–816. doi:10.1093/annweh/wxaa051
- Semenza JC, Suk JE. 2017. Vector-borne diseases and climate change: a European perspective. FEMS Microbiol Lett. 365(2):fnx244.
- Semmens EO, Leary CS, West MR, Noonan CW, Navarro KM, Domitrovich JW. 2021. Carbon monoxide exposures in wildland firefighters in the United States and targets for exposure reduction. J Expo Sci Environ Epidemiol. 31(5):923–929. doi:10.1038/s41370-021-00371-z
- Sheehan WJ, Gaffin JM, Peden DB, Bush RK, Phipatanakul W. 2017. Advances in environmental and occupational disorders in 2016. J Allergy Clin Immunol. 140(6):1683–1692. doi:10.1016/j.jaci.2017.09.032
- Shih G. 2023. The world’s torrid future is etched in the crippled kidneys of Nepali workers. Washington Post. https://www.washingtonpost.com/world/2023/01/06/climate-change-heat-kidney-disease/.
- Shusterman D. 2014. Occupational irritant and allergic rhinitis. Curr Allergy Asthma Rep. 14(4):425. doi:10.1007/s11882-014-0425-9
- Skóra J, Sulyok M, Nowak A, Otlewska A, Gutarowska B. 2017. Toxinogenicity and cytotoxicity of Alternaria, Aspergillus and Penicillium moulds isolated from working environments. Int J Environ Sci Technol. 14(3):595–608. doi:10.1007/s13762-016-1172-3
- Somanathan E, Somanathan R, Sudarshan A, Tewari M. 2021. The impact of temperature on productivity and labor supply: evidence from Indian manufacturing. J Polit Econ. 129(6):1797–1827. doi:10.1086/713733
- Soto RA, Hughes ML, Staples JE, Lindsey NP. 2022. West nile virus and other domestic nationally notifiable arboviral diseases—United States, 2020. MMWR Morb Mortal Wkly Rep. 71(18):628–632. doi:10.15585/mmwr.mm7118a3
- Spector JT, Bonauto DK, Sheppard L, Busch-Isaksen T, Calkins M, Adams D, Lieblich M, Fenske RA. 2016. A case-crossover study of heat exposure and injury risk in outdoor agricultural workers. PLoS One. 11(10):e0164498. doi:10.1371/journal.pone.0164498
- Spector JT, Krenz J, Blank KN. 2015. Risk factors for heat-related illness in Washington crop workers. J Agromedicine. 20(3):349–359. doi:10.1080/1059924X.2015.1047107
- Spector JT, Sheffield PE. 2014. Re-evaluating occupational heat stress in a changing climate. Ann Occ Hyg. 58(8):936–942.
- Stillman S. 2021. The migrant workers who follow climate disasters. New Yorker. https://www.newyorker.com/magazine/2021/11/08/the-migrant-workers-who-follow-climate-disasters.
- Stoecklin-Marois MT, Bigham CW, Bennett D, Tancredi DJ, Schenker MB. 2015. Occupational exposures and migration factors associated with respiratory health in California Latino farm workers: the MICASA study. J Occup Environ Med. 57(2):152–158. doi:10.1097/JOM.0000000000000325
- Streit JM, Felknor SA, Edwards NT, Howard J. 2021. Leveraging strategic foresight to advance worker safety, health, and well-being. Int J Environ Res Public Health. 18(16):8477. doi:10.3390/ijerph18168477
- Tallon LA, Manjourides J, Pun VC, Mittleman MA, Kioumourtzoglou M-A, Coull B, Suh H. 2017. Erectile dysfunction and exposure to ambient air pollution in a nationally representative cohort of older men. Environ Health. 16(1):1–9. doi:10.1186/s12940-017-0216-6
- Tamers SL, Streit J, Pana-Cryan R, Ray T, Syron L, Flynn MA, Castillo D, Roth G, Geraci C, Guerin R, et al. 2020. Envisioning the future of work to safeguard the safety, health, and well‐being of the workforce: a perspective from the CDC's National Institute for Occupational Safety and Health. Am J Ind Med. 63(12):1065–1084. doi:10.1002/ajim.23183
- Tang Y-X, Bloom MS, Qian ZM, Liu E, Jansson DR, Vaughn MG, Lin H-L, Xiao L-W, Duan C-W, Yang L, et al. 2021. Association between ambient air pollution and hyperuricemia in traffic police officers in China: a cohort study. Int J Environ Health Res. 31(1):54–62. doi:10.1080/09603123.2019.1628926
- Tempest EL, Carter B, Beck CR, Rubin GJ, English National Study on Flooding Health Study Group 2017. Secondary stressors are associated with probable psychological morbidity after flooding: a cross-sectional analysis. Eur J Public Health. 27(6):1042–1047. doi:10.1093/eurpub/ckx182
- Thien F, Beggs PJ, Csutoros D, Darvall J, Hew M, Davies JM, Bardin PG, Bannister T, Barnes S, Bellomo R, et al. 2018. The Melbourne epidemic thunderstorm asthma event 2016: an investigation of environmental triggers, effect on health services, and patient risk factors. Lancet Planet Health. 2(6):e255–e263. doi:10.1016/S2542-5196(18)30120-7
- Tiesman HM, Konda S, Hartley D, Menéndez CC, Ridenour M, Hendricks S. 2015. Suicide in US workplaces, 2003–2010: a comparison with non-workplace suicides. Am J Prev Med. 48(6):674–682. doi:10.1016/j.amepre.2014.12.011
- Toivanen M, Uusitalo H. 2022. Impacts of climate change are discussed in every other workplace – viewpoint of occupational safety is included rarely. Finnish Institute of Occupational Health. https://www.ttl.fi/en/topical/press-release/impacts-climate-change-are-discussed-every-other-workplace-viewpoint-occupational-safety-included.
- Tong MX, Hansen A, Hanson-Easey S, Xiang J, Cameron S, Liu Q, Liu X, Sun Y, Weinstein P, Han GS, et al. 2016. Perceptions of capacity for infectious disease control and prevention to meet the challenges of dengue fever in the face of climate change: a survey among CDC staff in Guangdong Province, China. Environ Res. 148:295–302. doi:10.1016/j.envres.2016.03.043
- UN Environment Programme. 2019. 2019 Global status report for buildings and construction sector towards a zero-emissions, efficient and resilient buildings and construction sector. International Energy Agency (IEA) for the Global Alliance for Buildings and Construction (GlobalABC).
- UNFCCC Secretariat. 2020. Just transition of the workforce, and the creation of decent work and quality jobs. Bonn, Germany: United Nations Framework Convention on Climate Change; April 2020.
- US DOL. 2022. Request for information on possible agency actions to protect life savings and pensions from threats of climate-related financial risk. Washington, DC: U.S. Department of Labor, Z-RIN 1210-ZA30. https://www.dol.gov/newsroom/releases/ebsa/ebsa20220211.
- US Energy Information Administration [US EIA]. 2021. Annual energy outlook.
- US EPA. 2003. Framework for cumulative risk assessment. U.S. Environmental Protection Agency, EPA/600/P-02/001F, 2003.
- US EPA. 2014. Fact sheet: mold in schools. Washington (DC): U.S. Environmental Protection Agency Indoor Environments Division (6609J).
- US EPA. 2019. Integrated science assessment (ISA) for particulate matter for ozone and related photochemical oxidants (final report). Washington (DC): U.S. Environmental Protection Agency, EPA/600/R-19/188.
- US EPA. 2020. Integrated science assessment (ISA) for ozone and related photochemical oxidants. Washington (DC).: U.S. Environmental Protection Agency, EPA/600/R-20/012.
- US EPA. 2021a. Climate change and social vulnerability in the United States: a focus on six impacts. Washington (DC): U.S. Environmental Protection Agency, EPA 430-R-21-003.
- US EPA. 2021b. Climate change indicators: length of growing season. U.S. Environmental Protection Agency; [accessed 2021 Jul 8]. https://www.epa.gov/climate-indicators/climate-change-indicators-length-growing-season.
- US EPA. 2021c. Wildfire smoke resources to protect your health. U.S. Environmental Protection Agency; [accessed 2021 Sep 21]. https://www.epa.gov/smoke-ready-toolbox-wildfires/wildfire-smoke-resources-protect-your-health.
- Vaisala. 2022. Total lightning statistics: 2021 annual lightning report. Vantaa (Finland): Vaisala.
- Valencia-Quintana R, Milic M, Jaksic D, Segvic Klaric M, Tenorio-Arvide MG, Perez-Flores GA, Bonassi S, Sanchez-Alarcon J. 2020. Environment Changes, Aflatoxins, and Health Issues, a Review. Int J Environ Res Public Health. 17(21):7850. doi:10.3390/ijerph17217850
- Viegas C, Meneses M, Viegas S, et. al. 2016. Climate changes influence in occupational exposure to fungi and mycotoxins. In: Arezes, editor. Occupational safety health and hygiene IV. London: Taylor and Francis; p. 11–15.
- Viegas S, Assunção R, Twarużek M, Kosicki R, Grajewski J, Viegas C. 2020. Mycotoxins feed contamination in a dairy farm - potential implications for milk contamination and workers’ exposure in a One Health approach. J Sci Food Agric. 100(3):1118–1123. doi:10.1002/jsfa.10120
- Vinikoor-Imler LC, Owens EO, Nichols JL, Ross M, Brown JS, Sacks JD. 2014. Evaluating potential response-modifying factors for associations between ozone and health outcomes: a weight-of-evidence approach. Environ Health Perspect. 122(11):1166–1176. doi:10.1289/ehp.1307541
- Wang XL, Yip PS, Chan CL. 2016. Suicide prevention for local public and volunteer relief workers in disaster-affected areas. J Public Health Manag Pract. 22(3):E39–E46. doi:10.1097/PHH.0b013e31829a303c
- Wangia RN, Tang L, Wang JS. 2019. Occupational exposure to aflatoxins and health outcomes: a review. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 37(4):215–234. doi:10.1080/10590501.2019.1664836
- Warwick N, Griffiths P, Keeble J, Archibald A, Pyle J, Shine K. 2022. Atmospheric implications of increased hydrogen use. https://assets publishing service gov uk/government/uploads/system/uploads/attachment_data/file/1067144/atmospheric-implications-of-increased-hydrogen-use pdf.75.
- Washington State Department of Labor and Industries. 2020. Protecting workers from wildfire smoke exposure: best practices. Tumwater (Washington): Washington State Department of Labor and Industries. F101-190-000 (09-2020).
- Washington State Department of Labor and Industries 2021. Outdoor heat exposure (emergency rule). Tumwater (Washington): Washington State Department of Labor and Industries.
- Weil D. 2017. The fissured workplace: why work became so bad for so many and what can be done to improve it. Cambridge (MA): Harvard University Press.
- WHO. 2018. Breathe clean air: everywhere, for everyone: protecting workers from air pollution outdoors and indoors (Concept Note). First WHO global conference on air pollution and health: improving air quality, combatting climate change – saving lives; 29 October 2018; Geneva (Switzerland): World Health Organization.
- Wilke ABB, Vasquez C, Petrie W, Caban-Martinez AJ, Beier JC. 2018. Construction sites in Miami-Dade County, Florida are highly favorable environments for vector mosquitoes. PLoS One. 13(12):e0209625. doi:10.1371/journal.pone.0209625
- Wilken JA, Sondermeyer G, Shusterman D, McNary J, Vugia DJ, McDowell A, Borenstein P, Gilliss D, Ancock B, Prudhomme J, et al. 2015. Coccidioidomycosis among workers constructing solar power farms, California, USA, 2011–2014. Emerg Infect Dis. 21(11):1997–2005. doi:10.3201/eid2111.150129
- Woetzel J, Pinner D, Samandari H, Engel H, Krishnan M, Boland B, Powis C. 2020. Climate risk and response: physical hazards and socioeconomic impacts. McKinsey Global Institute. https://www.mckinsey.com/capabilities/sustainability/our-insights/climate-risk-and-response-physical-hazards-and-socioeconomic-impacts
- Wu CM, Adetona A, Song C, Naeher L, Adetona O. 2020. Measuring acute pulmonary responses to occupational wildland fire smoke exposure using exhaled breath condensate. Arch Environ Occup Health. 75(2):65–69. doi:10.1080/19338244.2018.1562413