ABSTRACT
Labial minora fusion persisting to the reproductive age is a rare type of labial fusion. Only 17 sporadic case-reports have been published to describe this disease. We report a retrospective cohort study of nine patients undergone surgical dissections in our hospital with labial minora fusion of reproductive age. General information, a medical history, gynecological examinations, preoperative ultrasonography and observations during surgery were reviewed. Four patients found vulva deformity at age 1.25 ± 1.09 years, and the remaining 5 patients discovered the disease when they reached child-bearing age (25.20 ± 4.31). The average age of operation was 22.89 ± 6.21 years. The characteristic symptoms of the disease were menstrual blood and urine excretion from the urethral orifice. No endometriosis was detected in all 9 patients. One patient was found to have congenital defects, with a double cervical and complete uterine septum. All patients recovered well without re-adhesion. Seven patients (7/9, 77.80%) were interviewed by telephone. Three patients had normal sexual life and all patients were able to control urination normally. This labial fusion was found in 44.44% patients shortly after birth and might combined with other defects, suggesting a congenital nature of the disease, and further indicates the developmental feature of the vulva.
Introduction
Labial fusion refers to partial or complete fusion of the labial minora (from the clitoris to the posterior commissure). This condition is most frequently referred to labial adhesion, which is related to a low estrogen state. Most labial adhesion patients are infants or postmenopausal women, and local use of estrogen can relieve most symptoms. Labial minora fusion either persisted into the reproductive age or discovered at reproductive age is an extremely rare type of labial fusion. Since the first report in 1972, only 17 sporadic case reports have been documented (),Citation1–15 most of which were discovered at reproductive age. The main complaints of these patients were dyspareunia or difficult coitus. Physical examinations showed an otherwise normal woman with partial or complete fusion of the labial minora. In patients with complete labial fusion, a pinhole structure could be found, where urine and menstrual blood drained. Ultrasound or magnetic resonance imaging revealed normal urinary and genital systems. Surgical treatment could completely restore the normal appearance of the vulva, and all patients had a good prognosis in terms of both sexual and urinary function.
Table 1. Summary of reported cases of labial minora fusion in the reproductive age
Nine cases of labial fusion in women of child-bearing age were included here and retrospectively reviewed based on medical records, as well as follow-up telephone interviews with patients. With the largest reported cohort of this rare type of labial fusion, we summarize the clinical presentation, surgical findings, and outcomes after surgery and further discuss the developmental feather of the disease.
Results
By applying the ICD-10 code (labial fusion, Q52.500) in the screening database of our Hospital, 17 patients were selected. Four patients with cloacal anomalies and undergone anoplasty before 3 years of age were excluded because this procedure is a potential risk factor for labial adhesion involving genital cutting.Citation16 Two patients were excluded for maternal usage of androgen during pregnancy. Two patients were excluded for diagnosis of congenital adrenal hyperplasia (CAH). A total of 9 medical histories of labial fusion in women of reproductive age were reviewed. All medical records were complete, with general information, medical histories, physical examination data, laboratory test data, and ultrasound data for urinary and genital systems ().
Table 2. Course of disease and clinical symptoms of 9 patients treated in our hospital
Of the 9 patients, 4 were found to have vulva/perineum deformity at the age of 0–3 (1.25 ± 1.09) years and persisted into the reproductive age, and the remaining 5 patients discovered the disease when they reached child-bearing age (25.20 ± 4.31). Regarding the patients of child-bearing age, the first symptoms were discovered during a physical examination (3/5), due to difficult coitus (1/5) or due to difficulties in voiding (1/5). A total of 5 patients (55.56%) mentioned “blood and urination from the urethral orifice” in their medical history. This symptom referred to a blood or blot clots drained from the same orifice as urine during the menstrual period. Two patients mentioned mild dysmenorrhea. Of all 9 patients, none reported having symptom of dysmenorrhea, and a blood CA125 level or ultrasound test found no support for endometriosis. One patient was found to have congenital defects. She was diagnosed with a double cervical and complete uterine septum by magnetic resonance imaging (MRI).
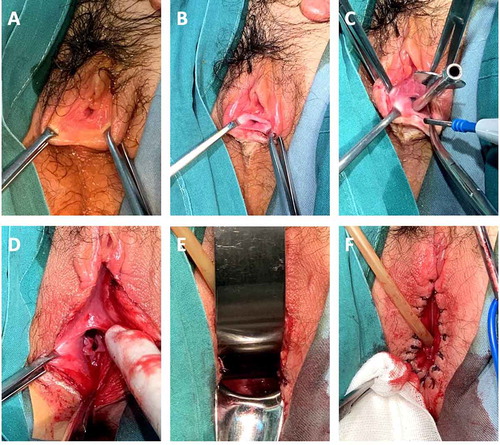
All patients underwent labial minora dissection in our hospital under general anesthesia. The mean age of surgical treatment was 22.89 ± 6.21 years. The mean time from discovering the condition to surgical treatment was 8.67 ± 9.89 years (ranging from 0–28 years). Careful physical examination was important to clarify the relationship between the urethral meatus and vagina. A metal urinary catheter was inserted as a guide to avoid injuries. After separation of the fused labia with a cold knife, the urethral orifice and vaginal orifice were fully exposed. The vaginal width was ensured to accommodate 2 fingers. Absorbable sutures were used to suture the labia intermittently to stop bleeding (). The average operation time was 30 minutes, and blood loss was less than 10 ml. The patient could be discharged on the first day after the operation, with an average hospitalization time of 2 days. After discharge, seed oil was applied to the wound to improve wound healing and prevent re-adhesion.
Figure 1. Procedure for labial fusion dissection. (a, b) Overview of the fused labial minora. Only the urethra meatus was visible. (c) A metal urethral catheter was inserted as a guide to avoid urethral injuries. (d) The fused labial minora were separated, and the vagina was revealed to have a normal width. (e) A normal cervix was evident. (f) The edges of the incision were sutured with 1/0 coated VICRYL separately
Seven patients (7/9, 77.80%) were interviewed by telephone, and the others could not be contacted. Regular follow-up checks 4–6 weeks after surgery showed that all patients exhibited good recovery from the operation. The annual follow-up checks revealed the normal appearance of the vulva and no further adhesion. The average time of follow-up is 6 months. Between March and May 2018, patients were interviewed by telephone for urinary symptoms, sexual function and pregnancy status. Three patients had a normal sexual life, while the remaining patients had no sexual partners. None of the patients had urinary symptoms, including urinary infection and urinary incontinence. None of the patients were pregnant.
Discussion
Criteria were proposed to differentiate this condition from labial adhesion, a more common disease with similar clinical presentation. After summarizing the clinical presentation, surgical findings and long-term outcomes after surgery, we clarify the nature of this condition and intend to share some perspectives in managing these patients. To our knowledge, this is the first article to report a combination of labial minora fusion and uterine defect in reproductive age women.
We found that the septum between the urethra and vagina was significantly thin in all patients, which was related to congenital malformation. At the fifth week of embryonic development, the mesodermal tissue, located between the cloaca and the posterior intestine, grows downward to form a cloacal septum. The cloaca is divided into two parts: the urogenital sinus and the rectum. As the embryo develops, the connection between the two parts of the cloaca becomes narrow and forms a cloacal tube, which is closed at 7th week. If embryonic development stops before the seventh week, different degrees of cloacal malformation can form, which may present as a current thin septum between the urethra and vagina.Citation17–19 Exposure to androgen can retard the descent of the sinus ridge of the female mouse and is sufficient to cause vaginal attachment to the urethra and prevent vaginal opening in the vulva. In addition, the masculinization of the vulva is related to androgen actions.Citation19 The relative position of the urogenital sinus ridge and the Müllerian ducts shifts along the urethra until reaching the vulva. When female mouse embryo was treated with methyltestosterone, the vagina was more closely related to the urethra. Besides androgen intake, CAH can lead to similar clinical symptoms. CAH is a hereditary disease that can cause excessive androgen production in the fetal adrenal gland during the embryonic period, leading to vulvar masculinization in patients with chromosome 46, XX. Therefore, excessive androgen or abnormal activation of androgen receptors by unknown factors may be the etiology of congenital labia minor fusion, and further genetic testing is needed.
Labial adhesion is associated with low estrogen level, having higher incident in prepubertal and postmenopausal, and can be relieved by local use of estrogen. But there are evidences indicating that there is no significant different estrogen level between patients and healthy controls.Citation20 There is an interesting case that a woman was diagnosed as labial fusion six weeks of pregnancy.Citation10 Postpartum labial adhesions have also been reported.Citation21 Therefore, there may be some disturbances in estrogen signaling and need further researches.
We’ve noticed that Asian population may have higher incidence of the current disease, as six cases have been reported in Japan.Citation12 As labial fusion causes no serious complaints in these patients, incident may be underestimated. More attention should be paid in daily clinical work of gynecologists.
Patients and methods
The records of patients with a diagnosis of labial fusion were selected based on the ICD-10 code (labial fusion, Q52.500) from the database of our Hospital for retrospective study, from 1984 to 2018.
To differentiate the persistent labial minora fusion in women from labial adhesion, the following criteria were proposed:
Inclusion of labial minora fusion patients discovered either in infant or pubertal age and persisted into the reproductive age or at reproductive age with a history of menstruation and normal sex hormone.
Exclusion of congenital adrenal cortical hyperplasia, false hermaphroditism, true hermaphroditism and other acquired conditions.Citation16
General information, a detailed medical history (with particular interest in urinary symptoms and sexual function), physical examinations, gynecological examinations, laboratory tests, preoperative ultrasonography data of both the pelvis and urinary system, and observations during surgery were reviewed. All patients underwent surgical treatment to separate the labial minora. The operating time, estimated blood loss, and length of the hospital stay were also recorded. All patients were given ulceration oil to improve wound recovery and underwent regular follow-up checks 4–6 weeks after surgery and annually thereafter. Between March and May 2018, patients were interviewed by telephone for urinary symptoms, sexual activity and pregnancy status.
Follow-up data and photographs of all patients were used with patient consent. The study was approved by the local Institutional Ethics Committee.
Author contributions
Dr. Ze LIANG: Project development, Data Collection, Manuscript writing. Dr. Juan CHEN: Data collection. Dr. Xin YU: Manuscript writing. Dr. Lan ZHU: Project development, Comments and critical reading of the manuscript.
Disclosure statement
The authors declare that they have no conflicts of interest and nothing to disclose.
References
- Goldstein AI, Rajcher WJ. Conglutination of the labia minora in the presence of normal endogenous estrogen levels: an exception to the rule. Am J Obstet Gynecol. 1972;113(6):845–46. doi:10.1016/0002-9378(72)90572-8.
- Topcuoglu MA, Koc O, Duran B, Donmez M. Labial fusion causing acute urinary retention in a young adult: a case report. Aust N Z J Obstet Gynaecol. 2009;49(1):115–17. doi:10.1111/j.1479-828X.2008.00946.x.
- Watanabe T, Matsubara S, Ikeda T, Kawai S, Nakamura S, Nakai H. Labial adhesion causing voiding but not sexual problems in a married woman. J Obstet Gynaecol Res. 2013;39(1):415–19. doi:10.1111/j.1447-0756.2012.01934.x.
- Kuo DM, Chuang CK, Hsieh CC, Liou JD, Chen KC, Hsieh TT. Labial fusion in a thirty-year-old woman. Acta Obstet Gynecol Scand. 1998; 77(6): 697–98. http://europepmc.org/abstract/MED/9688253
- Kutlu O, Koksal IT. Labial adhesion in a reproductive aged girl. Saudi Med J. 2010;31:202–03.
- Ozekinci M, Yucel S, Sanhal C, Akar ME. Labial fusion causing coital and voiding difficulty in a young woman. Adv Sex Med. 2013;03(1):11–13. doi:10.4236/asm.2013.31002.
- Guldberg R, Thybo S, Andersen B. Synechia vulvae – an unusual cause of urinary symptoms in a 15-year-old girl. Acta Obstet Gynecol Scand. 2007;86(2):251–52. doi:10.1080/00016340600608287.
- Evruke C, Ozgunen FT, Kadayifci O, Atay Y, Demir C, Aridogan N. Labial fusion in a pubertal girl: a case report. J Pediatr Adolesc Gynecol. 1997;9(2):81–82. doi:10.1016/S1083-3188(96)70016-5.
- Erdoğdu E, Demirel C, Tahaoğlu AE, Özdemir A. Labial fusion: a rare cause of urinary retention in reproductive age woman and review of literature. Turk Urol Derg. 2017;43(1):98–101. doi:10.5152/tud.2017.58897.
- Kucuk M, Halil S, Ocer F, Oral E. Labial fusion first diagnosed during pregnancy with voiding difficulty and its management: a case report. Clin Exp Obstet Gynecol. 2011;38(1):94-5.
- Singh V, Sinha S, Singh A. Labial agglutination in a pubertal girl. J Clin Diagn Res. 2018;12(1):QD01–QD02. doi:10.7860/JCDR/2018/31835.11087.
- Tsujita Y Asakuma J, Kanbara T, Yoshii T, Azuma R, Sumitomo M, Asano. A case of labial adhesion in a reproductive woman. Acta Urol Jpn. 2010;56(8):463-5.
- Kumar RK, Sonika A, Charu C, Sunesh K, Neena M. Labial adhesions in pubertal girls. Arch Gynecol Obstet. 2006;273(4):243–45. doi:10.1007/s00404-005-0060-8.
- Halder A, Pati S, De Pati A, Halder S. Complete vulvar fusion in an adult woman mimicking vaginal agenesis. J Obstet Gynaecol (Lahore). 2009;29(4):361–62. doi:10.1080/01443610902842607.
- Özalp B, Bilgin Karabulut A. Labial fusion in an adult woman represented as a congenital disorder: case report. Turkiye Klin Jinekoloji Obstet. 2010;20(1):57-59.
- Nour NM. Urinary calculus associated with female genital cutting. Obstet Gynecol. 2006;107(2 Pt 2):521–23. doi:10.1097/00006250-200602001-00034.
- Roly ZY, Backhouse B, Cutting A, Tan TY, Sinclair AH, Ayers KL, Major AT, Smith CA. The cell biology and molecular genetics of Müllerian duct development. Wiley Interdiscip Rev Dev Biol. 2018;7(3):1–13. doi:10.1002/wdev.310.
- Mullen RD, Behringer RR. Molecular genetics of Müllerian duct formation, regression and differentiation. Sex Dev. 2014;8(5):281–96. doi:10.1159/000364935.
- Larkins CE, Enriquez AB, Cohn MJ. Spatiotemporal dynamics of androgen signaling underlie sexual differentiation and congenital malformations of the urethra and vagina. Proc Natl Acad Sci. 2016;113(47):E7510–E7517. doi:10.1073/pnas.1610471113.
- Çaǧlar MK. Serum estradiol levels in infants with and without labial adhesions: the role of estrogen in the etiology and treatment. Pediatr Dermatol. 2007;24(4):373–75. doi:10.1111/j.1525-1470.2007.00493.x.
- Seehusen DA, Earwood JS. Postpartum labial adhesions. J Am Board Fam Med. 2007;20(4):408–10. doi:10.3122/jabfm.2007.04.060214.
