 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Gasdermin-D (GSDMD) belongs to the Gasdermin family (GSDM), which are pore-forming effector proteins that facilitate inflammatory cell death, also known as pyroptosis. This type of programmed cell death is dependent on inflammatory caspase activation, which cleaves gasdermin-D (GSDMD) to form membrane pores and initiates the release of pro-inflammatory cytokines. Pyroptosis plays an important role in achieving immune regulation and homeostasis within various organ systems. The role of GSDMD in pyroptosis has been extensively studied in recent years. In this review, we summarize the role of GSDMD in cellular and organ injury mediated by pyroptosis. We will also provide an outlook on GSDMD therapeutic targets in various organ systems.
Overview of pyroptosis and gasdermin-D
Pyroptosis is an inflammatory form of programmed cell death mediated by inflammatory caspases upon exposure to a pathogenic infection, pathogen-associated molecular patterns (PAMPs), or host-derived damage-associated molecular patterns (DAMPs) through canonical and noncanonical pathways.Citation1–5 The canonical pathway depends on the inflammasomes, such as NLRP1b, NLRP3, NLRC4, AIM2, or Pyrin, to form a complex and induce inflammation and systemic immune response by activating caspase-1. The noncanonical pathway is inflammasome-independent and occurs when gram-negative bacterial lipopolysaccharide (LPS) can recognize caspase-11 in mice and caspase-4/5 in humans. Gasdermin-D is a substrate of both caspase-1 and caspase-11, where they both cleave the N-terminal of Gasdermin-D (GSDMD-NT) to release pro-inflammatory cytokines interleukin-1β (IL1β) and interleukin-18 (IL18) which induce pyroptosis.Citation1–5
Gasdermin (GSDM) is a family of proteins comprised six members: GSDMA, GSDMB, GSDMC, GSDMD, GSDME/DNFA5, and PVJK/GSDMF.Citation6 They are mostly composed of C-terminal, N-terminal and linker domains.Citation7 The first GSDM protein was discovered in 1998 as a mutation in age-related hearing loss as DNFA5.Citation6, Citation7 In 2000, Saeki et al.Citation8 identified GSDM gene expressed in GI tract and skin on mouse chromosome 11.Citation7–9 GSDMD was determined to be required for pyroptosis in 2015.Citation10–12 Shi et al.Citation10 showed that cleavage of GSDMD by caspase-1 and other inflammatory caspases can drive pyroptosis.
However, Kayagaki et al.Citation11 refuted Shi et al.Citation10 hypothesis and demonstrated that caspase-11 requires GSDMD to promote pyroptosis, caspase-1 activation and non-canonical inflammasome signaling due to LPS.Citation10 Upon proteolytic cleavage of GSDMD, the N-terminal fragment interacts with the membrane lipids to form GSDMD pores and promotes the secretion of IL-1βin pyroptosis, thus GSDMD is best known as a pyroptosis executioner.Citation12
The role of gasdermin-D in liver injury
Gasdermin-D-mediated pyroptosis is hepatoprotective in various NAFLD stages
Liver injury is the primary cause of abdominal trauma involving cell death and inflammation.Citation13,Citation14 GSDMD plays a major role in hepatocyte pyroptosis, with extensive studies done on its role in alcoholic fatty liver disease and various forms of liver injuries.Citation14–19 Xu et. al, demonstrated that cleaved GSDMD N-terminal fragments are increased in both nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis patients (NASH), resulting in lobular inflammation, which is one of the key features of NASH.Citation15, Citation16, Citation18 As a result, several studies show that inhibiting hepatocyte GSDMD-mediated pryoptosis can alleviate different severities on liver injuries.Citation17–21 Yin et al.Citation17 demonstrate that Jiangzhi Ligan Decoction (JZLGD), a Chinese herbal formula, decreased hepatic steatosis and liver inflammation by inhibiting GSDMD levels and its N-terminal fragments, by preventing the expression of ASC, NLRP3, Caspase-1 and Caspase-11 located upstream of GSDMD in both canonical and non-canonical pathways. JZLGD regulates the activation of GSDMD, pore formation, and the release of proinflammatory cytokines IL1β and IL-18.Citation17
GSDMD has also been shown to target different levels of NAFLD such as fibrosis by activating stellate cells.Citation19 This indicates that regulation of hepatocyte pryoptosis can lead to hepatoprotective effects in different NAFLD stages. Other studies investigated the effect of inhibiting hepatocyte pyroptosis in severe forms of liver injury. Wang et al.Citation20 show that phenethyl isothiocyanate (PEITC), a natural product found in cruciferous vegetables, can significantly reduce both chemical and inflammatory liver injury. Similar to JZLGD, PEITC targets NLRP3 and Caspase-1. Additionally, PEITC directly inhibits GSDMD cleavage and membrane pore formation by binding to cysteine 191 on GSDMD.Citation20
Gasdermin-D-mediated pyroptosis plays a role in hepatoxicity and liver failure
As acute liver injury (ALI) may progress to acute liver failure (ALF), a recent study demonstrated Necrosulfonamide, a GSDMD inhibitor, to alleviate ALF induced by Lipopolysaccharide/D-galactosamine .Citation21, Citation33
Table 1. Summary of therapeutic compounds in organ injury targeting pathways leading to GSDMD-mediated pyroptosis.
GSDMD inhibition has been shown to be hepatoprotective in NAFLD, ALI and ALF. However, additional studies show GSDMD deficiency can be hepatotoxic in noninfectious liver injury such as Acetaminophen (APAP)-induced liver failure and hypoxic liver induced by hemorrhagic shock.Citation35 Yang et al.Citation35 demonstrated that inhibiting GSDMD in mice increases liver damage after APAP overdose and hemorrhagic shock due to increase in hepatocyte death. When GSDMD is inhibited, caspase-8 cleavage is increased, resulting in increased apoptosis and necroptosis and ultimately hepatocyte death.Citation35 Activation of GSDMD is hepatoprotective in noninfectious liver injury by downregulating caspase-8 cleavage, resulting in reduction of apoptosis and necroptosis signaling pathways.Citation35 They further showed that inhibition of GSDMD leads to absence of pyroptosis resulting in the activation of other cell death signaling pathways such as apoptosis and necroptosis.Citation35 In line with their study, Yang et al.Citation35, also shed light on hepatocyte morphology when undergoing GSDMD-mediated pyroptosis. Pyroptosis in hepatocytes exhibit low levels of GSDMD cleavage compared to macrophages. Hepatocytes are also shown to be resistant to pyroptosis by experiencing slight cell shrinkage and no cell rupture.Citation36
GSDMD-mediated pyroptosis plays a role in 70% partial hepatectomy (PH), where its inhibition alleviates liver injury and accelerates liver regeneration through upregulation of mitogen signaling pathways, including epidermal growth factor receptor (EGFR) and hepatocyte growth factor receptor (HGFR) pathways.Citation37
Gasdermin-D is essential in Kupffer cells and liver sinusoidal endothelial cells
There are few studies investigating the role of GSDMD in hepatic stellate cells, liver sinusoidal endothelial cells and Kupffer cells. Yamagishi et al.Citation38 demonstrated that GSDMD-NT cell membrane pore formation mediates the release of IL-33 from senescent hepatic stellate cells, which promotes obesity-associated hepatocellular carcinoma. Interestingly, one study showed that GSDMD specific deficiency in myeloid cells is protective hepatic-ischemia reperfusion injury (IRI), with no protective effects in GSDMD specific deficiency in hepatocytes cells.Citation39 Lastly, GSDMD plays a crucial role in disseminated intravascular coagulation (DIC) in sepsis; GSDMD deficiency ameliorates thrombin generation, fibrin deposition, and platelet aggregation in the liver microvasculature.Citation40
GSDMD is a double-edged sword, since it is involved in different cell death signaling pathways, its effect on liver injury depends on the severity of the damage.Citation36 We can conclude that GSDMD inhibition is hepatoprotective due to the rigorous research on severe liver injury and various liver cells. GSDMD deficiency in hepatoprotective in various liver injuries includes, but is not limited to, NAFLD, ALI, ALF, and 70% PH. In addition, GSDMD deficiency further inhibits DIC in sepsis in the liver microvasculature and protects against obesity-induced HCCCitation38,Citation40. However, further studies are needed to determine how GSDMD-mediated pyroptosis leads to liver injury and disease and investigate its effect in different liver cell types, including stellate and parenchymal cells.
The role of gasdermin-D in brain injury
Gasdermin-D plays a role in Ischemia/reperfusion brain injury
Central nervous system injuries are common causes of morbidity and mortality at different ages, lacking sufficient treatments.Citation41 GSDMD-mediated pyroptosis is associated with traumatic brain and spinal cord injuries, where recent studies and reviews highlight the role of NLRP3 in the central nervous system.Citation42–45 However, in the past five years, GSDMD has been extensively studied in ischemic stroke and cerebral ischemia, making it a potential therapeutic target in ischemia and reperfusion brain injury.Citation22, Citation41, Citation46 Zhang et al.Citation46 showed that middle cerebral artery occlusion/reperfusion has elevated levels of GSDMD and N-terminal fragments (GSDMD-NT) that induce pyroptosis. In addition, another group demonstrated that pyroptosis occurs in neurons.Citation22 They showed significantly high GSDMD expression on day one post-acute stroke.Citation22 They further assessed the neuronal effects of VX765 treatment, a caspase-1 inhibitor, post-ischemia, which showed a significant reduction of GSDMD on day one and suppression of the canonical inflammasome pathway leading to neuroprotection following ischemic stroke.Citation22 GSDMD-mediated pyroptosis was also shown in microglia after ischemia/reperfusion brain injury. Therefore, knocking down GSDMD improves recovery after ischemic brain injury by preventing pro-inflammatory cytokine release of IL-1β and IL18.Citation41
Inflammasome inhibition regulates GSDMD-mediated pyroptosis in brain injury
Interestingly, growing evidence documents the effect of AIM2 inflammasome on GSDMD-mediated pyroptosis in early brain injury (EBI) after aneurysmal subarachnoid hemorrhage (SAH).Citation47 EBI after SAH involve the secretion of pro-inflammatory cytokines IL-1β and IL-18. Patients with SAH exhibit high levels of AIM2 inflammasome in their cerebrospinal fluid (CSF).Citation47 Since AIM2 is upstream to GSDMD in the canonical pathway, they revealed that GSDMD-mediated pyroptosis by AIM2 inflammasome is essential in EBI after SAH.Citation47 These findings suggest potential therapeutic targets for different brain injuries by regulating GSDMD-mediated pyroptosis.
Inflammasome inhibition regulates GSDMD-mediated pyroptosis in spinal cord injury
GSDMD-mediated pyroptosis can further regulate spinal cord injuries (SCI). Inflammasomes play a critical role in SCI, resulting in inflammatory cell death.Citation48, Citation49 Recent evidence demonstrated the therapeutic effects of inhibiting GSDMD and suppressing pyroptosis in SCI to reduce the inflammatory response.Citation47, Citation34,Citation50–52 Dai et al.Citation50 demonstrated that ASC, caspase-1, and GSDMD in the canonical inflammasome pathway associated with pyroptosis, were significantly elevated in spinal cord injury rat models compared to the sham groups. They inhibited SCI pyroptosis and neuroinflammatory response by using Celastrol, a therapeutic agent for cerebral ischemia, significant neuroinflammation reduction seven days after spinal cord injury in rat models and recovery of motor dysfunction.Citation50
Another group further investigated the effect of CD73, an immune homeostasis regulator, in GSDMD-mediated pyroptosis.Citation44, Citation51 S. Xu and colleaguesCitation51 first showed that CD73 and GSDMD levels are positively correlated with the severity of SCI patients.They further elucidated the CD73 mechanism in microglia pyroptosis, where CD73 overexpression increased Foxo1 activation in PI3K/AKT/Foxo1 in BV2 microglial cells.Citation51, Citation52 Interestingly, they revealed that Foxo1 is a transcriptional activator in the promoter region of the GSDMD gene, indicating that CD73 regulates the expression of GSDMD through Foxo1.Citation51, Citation52 CD73 targeting GSDMD through PI3K/AKT/Foxo1 mechanism is a promising approach for identifying an effective therapeutic target for SCI. In addition, AIM2 inflammasome has also been shown to play a role in SCI.Citation53 Using Carbon monoxide release molecule-3 (CORM3) has been shown to inhibit inflammasome activation, which is a potential therapeutic target for SCI.Citation53 Nevertheless, further studies need to investigate the potential role of GSDMD-mediated pyroptosis by AIM2 inflammasome in SCI ().
Table 2. Summary of therapeutic compounds in organ injury targeting GSDMD cleavage, IL1β and IL18 release.
The role of gasdermin-D in cardiovascular Injury
Emerging evidence suggests the role of GSDMD in cardiomyocytes pyroptosis. Lei and colleagues revealed the role of pyroptosis and oxidative stress in myocardial infarction (MI), where they examined GSDMD and its transcription factor NFB.Citation62 Using the myocardial infarction rat model, they revealed that GSDMD-mediated pyroptosis by NLRP3 inflammasome results in cardiomyocyte loss following MI. They further showed that inhibiting oxidative stress can reduce NLRP3-mediated pyroptosis and therefore regulate the activity of the NFκB-GSDMD signaling axis, making it a promising approach for targeted MI therapies.Citation62 GSDMD plays a role in different stages of MI. MI can result in ischemic myocardial tissue, and myocardial ischemia/reperfusion (I/R) injury upon reperfusion. Shi and colleaguesCitation63 investigated the role of GSDMD-mediated cardiomyocyte pyroptosis in MI I/R injury, where they proved that GSDMD deficiency reduced myocardial I/R in mice. In addition, they demonstrated that GSDMD was cleaved in cardiomyocytes when stimulated with H2O2 to induce oxidative stress.Citation63 GSDMD deficiency has also been shown to attenuate LPS-induced septic myocardial dysfunction by reducing cardiac inflammation, NFκB signaling pathways, ROS production and NLRP3 activation.Citation64
NFkB/NLRP3/GSDMD pathway is a therapeutic target in myocardial infarction (MI)
In line with the previous study, several studies revealed GSDMD to be a potential therapeutic target in MI and myocardial I/R injury through NFκB/NLRP3/GSDMD pathway. Ye and colleaguesCitation23 showed that mRNA levels of GSDMD and its N-terminus (GSDMD-NT) were upregulated in cardiomyocytes after hypoxia/reoxia (H/R). They investigated the effects of an anti-inflammatory compound, Emodin, which protected cardiomyocytes from GSDMD-mediated pyroptosis when exposed to H/R.Citation23 Emodin showed a protective mechanism by reducing infarct size after myocardial I/R injury and pyroptosis in vivo. They further elucidated the Emodin mechanism, which targets the TLR4/MyD88/NFκB/NLRP3 pathway, all leading to GSDMD cleavage and pyroptosis.Citation23 TLR4 recruits MyD88, which triggers NFκB activation, a GSDMD transcription factor.Citation23, Citation63, Citation64 NF B activates NLRP3, resulting in the cleavage of caspase-1 and ultimately GSDMD cleavage.Citation23, Citation65 Conversely, Emodin blocks the TLR4 pathway, inhibiting NFκB and NLRP3 activation, caspase-1 and GSDMD cleavage, and IL1βrelease.
Gasdermin-D-mediated pyroptosis is activated in acute myocardial infarction (AMI)
In more recent studies, GSDMD is also shown to be activated in acute myocardial infarction (AMI), indicating that pyroptosis plays an essential role in the progression of AMI.Citation54, Citation66 Zhang et al.Citation66 revealed that pro-inflammatory adipokine, retinol-binding protein 4 (RBP4), contributes to AMI by activating the canonical inflammasome NLRP3/Caspase-1/GSDMD-NT resulting in pyroptosis. Furthermore, they showed that knockdown of RBP4 can attenuate NLRP3-mediated pyroptosis and protect against cardiac dysfunction after AMI injury. Thus, targeting RBP4 can be beneficial for AMI treatment.Citation66 These studies highlighted the importance of NFκB/NLRP3/GSDMD pathway in regulating cardiac dysfunction and myocardial injury. K. Jiang and colleaguesCitation54 further demonstrated that GSDMD activation in AMI injury results in infiltration of neutrophils/monocyte and cardiac inflammation. In groundbreaking results, Jiang et al.Citation54 revealed that GSDMD pharmacological inhibition using Necrosulfonamide can reduce infarct size after AMI injury ().
Gasdermin-D-mediated pyroptosis plays a major role in endothelial dysfunction
Pulmonary Arterial Hypertension (PAH) is caused due to endothelial dysfunction, which enhances vascular inflammation due to activation of caspase-1 and caspase-11 in pyroptosis.Citation67 Caspase-11 in mice, homologous to caspase-4 in humans, was activated in PAH rat models and injury simulated human pulmonary artery endothelial cells (HPAECs) by TNF .Citation67 They inhibited caspase-11/4 activity using wedelolactone, which hindered the progression of PAH rat models.Citation67 Wu and colleaguesCitation67 further examined downstream effects of caspase-11 in TNF
-induced HPAECs, which activated GSDMD to induce endothelial cell pyroptosis. GSDMD is activated through different inflammasome pathways; therefore, GSDMD inhibition in PAH needs to be further studied and validated.
NLRP3/GSDMD has been further studied in coronary endothelial cell dysfunction in Kawasaki disease (KD).Citation68 KD is the most common cause of pediatric cardiac disease in developed countries.Citation68 In addition to coronary endothelial cell dysfunction, KD is also caused by the production of pro-inflammatory cytokine IL1β; thus, the role of pyroptosis was investigated in endothelial cells in KD.Citation68 Jia and colleaguesCitation68 revealed that proteins in the canonical inflammasome pathway associated with pyroptosis (ASC, cleaved caspase-1, GSDMD, matureIL1β, and IL18) are significantly elevated in KD patients compared to healthy personnel. Moreover, NLRP3 inflammasome was expressed in KD-treated endothelial cells, resulting in activation of downstream NLRP3-mediated pyroptosis, including cleaved caspase-1 GSDMD-NT, mature IL1β, and IL8.Citation68 These results suggest the role of endothelial cell pyroptosis in KD and how targeting NLRP3-mediated pyroptosis, including GSDMD-NT, could be a potential targeted therapy for KD and other related conditions with systemic inflammation.
GSDMD-mediated pyroptosis effects vascular inflammation
As myocardial hypertrophy is associated with chronic inflammation and increase in inflammatory cytokines, GSDMD-mediated inflammation also plays a role in myocardial hypertrophy and cardiac dysfunction.Citation55, Citation69, Citation70 Han and colleaguesCitation55 investigated the effects of using DL-3-n-butylphthalide (NBP), a neuroprotective agent widely used in various Asian countries to treat ischemic stroke, in GSDMD-mediated inflammation. They used a transverse aortic constriction (TAC) mouse model to induce cardiac injury, which showed that NBP administration prevents myocardial hypertrophy and cardiac dysfunction by targeting GSDMD-NT and reducing inflammation.Citation55 GSDMD has been studied in various cardiac dysfunction and vascular inflammation severities. Cardiovascular endothelial cell injury induced by Decabromodiphenyl ethane (DBDPE) enhances NLRP3 and caspase-1 activity, yet no studies have covered the therapeutic implications of GSDMD in cardiovascular injury induced by air pollutants.Citation71 Lastly, GSDMD plays a role in vascular smooth muscle cells and cardiovascular injury. GSDMD specific deficiency in vascular smooth muscle cells alleviates abdominal aortic aneurysm (AAA) by reducing putrescine compound levels in the aorta.Citation24 Inhibiting the synthesis of putrescine with difluoromethylornithine (DMFO), a compound in a clinical trial for Neuroblastoma, results in the prevention of AAA development. Thus, DMFO could be a potential drug for AAA treatment with few side effects ().Citation24 GSDMD is activated in macrophages and vascular smooth muscle cells in human plaques, which exacerbates atherogenesis; thus, inhibition of GSDMD and pyroptosis in atherosclerosis can be a potential therapeutic target.Citation72
The role of gasdermin-D in lung injury
GSDMD plays a pivotal role in circulating vesicles in endothelial cell lung injury including sepsis-mediated pulmonary vascular endothelial cell injury and ventilation-induced lung injury.Citation73, Citation74 During a pathological condition of the vascular endothelium, microparticles encapsulating caspase-1 are being released, where they circulate and accumulate in areas of disordered blood flow.Citation73, Citation75, Citation76 Mitra et al.Citation73 revealed that GSDMD induced by LPS simulation is encapsulated with the active caspase-1 microparticles to induce endothelial cell death. The group further showed that GSDMD knockout cells exhibit no circulation of active caspase-1 microparticles.Citation73 Interestingly, a more recent group examined the effect of pyroptosis on circulating extracellular vesicles (EVs) in ventilation-induced lung injury (VILI).Citation76 VILI has been shown to activate caspase-1/GSDMD in the lung, where only caspase-1 is transported to the brain in circulating EVs, leading to neuroinflammation and cell death by activating GSDMD and more caspase-1 in the brain.Citation74 These studies highlight the importance of understanding circulating vesicles regulation in endothelial lung injuries inducing inflammation through GSDMD activation.
Gasdermin-D inhibition is a therapeutic target in lung inflammation
Many studies in the past few years investigated the role of LPS-induced lung vascular endothelial pyroptosis leading to acute lung injury and ultimately traumatic brain injury and multiorgan failure dysfunction.Citation77–80 These studies primed the way to explore different therapeutic targets of acute lung injury and lung inflammation (). Wang and colleaguesCitation56 examined the effect of Dihydromyricetin (DHM), an anti-inflammatory flavonoid, in the cecal-ligation puncture model of sepsis to induce acute lung injury, which showed significant downregulation of lung inflammation by targeting the NLRP3/caspase-1/IL1β/IL18/GSDMD-NT pyroptosis pathway. DHM has been also previously shown to inhibit vascular endothelial cell pyroptosis in vitro through the Nfr2 signaling pathway.Citation81 Downregulation NLRP3 inflammasome-mediated pyroptosis revealed many therapeutics approaches in the treatment of sepsis-induced acute lung injury using hemin,Citation25 corticosteroids,Citation26 and cyclic helix B peptide.Citation27 In addition, Geranylgeranyl pyrophosphate synthase large subunit (GGPPS1) has also been shown to be effective against sepsis-induced acute lung injury by suppressing NLRP3 inflammasome activity in the TLR4-NFκB pathway.Citation82, Citation83 Consistent with the previous finding, Ghrelin, a hormone protective against neuronal injury and stroke, has been shown to alleviate brain injury induced by acute lung injury by blocking the TLR4-NFκB signaling pathway.Citation28 Therapeutic targets in LPS-induced acute lung injury through pyroptosis have been heavily studied, showing promising results in inhibiting lung injury and pulmonary inflammation ().
Gasdermin-D inhibition impedes multiorgan failure development in sepsis
Furthermore, pancreatitis can induce lung injury, known as severe acute pancreatitis (SAP)-associated lung injury.Citation57 Wu and colleaguesCitation57 revealed activation of GSDMD and release of IL1β and IL18 in SAP mice models. They further showed that Disulfiram, an approved drug for alcohol use disorder, prevented GSDMD activation and IL1β and IL18 release, ameliorating SAP-induced lung injury.Citation57 GSDMD downregulation is also effective against SAP in intestinal injuries by reducing systemic inflammatory response.Citation58 Intravenous injection of siRNA to deplete GSDMD in SAP mice models, reduced IL1β and IL18 levels and improved intestinal musical changes and intestinal villus breakage.Citation58 These studies suggest that GSDMD inhibition can reduce systemic inflammation in multiple organ dysfunction syndromes studied by C. Silva and colleagues.Citation59 Similar to Wu et al.'s findings,Citation57 they showed effective treatment with Disfulram, which inhibited sepsis development to multiple organ dysfunction syndromes ().Citation59
Gasdermin-D inhibition alleviates vaso-occlusion in sickle cell disease
Lastly, GSDMD plays a vital role in inflammatory lung injury in sickle-cell disease (SCD), which promotes caspase-4/11 dependent activation of neutrophil-GSDMD and shedding of neutrophil extracellular traps (NETs) in the liver in P-selectin dependent manner.Citation29 The NETs translocate to the lung and lead to neutrophil-platelet aggregation.Citation29 Vats et al.Citation29 further showed that inhibition of GSDMD using GSDMD-NT inhibitors Necrosulfamide and LDC7559, pan-caspase inhibitor Z-VAD-FMKCitation38 alleviated lung vaso-occlusion in SCD.
The role of gasdermin-D in gastrointestinal tract injury
Gasdermin-D is expressed in intestinal epithelial cells
GSDMD-associated pyroptosis contributes to inflammatory bowel disorders such as ulcerative colitis (UC) and Crohn’s disease and is increased in intestinal epithelial cells during colitis and inflammatory bowel disease (IBD).Citation84, Citation85 GSDMD can be derived from dysregulated gut microbiota, specifically E.coli, increasing IL18 release, while mediating the release of nonlytic IL1β-containing small extracellular vesicles from the intestinal epithelial cells to promote DSS-induced colitis.Citation84, Citation85 GSDMD also plays a role in metabolic diseases, systemic endotoxemia, and gut dysbiosis.Citation86 Mice fed with high fat diet (HFD) have activated GSDMD-NT in mouse liver, kidney, and adipose tissue, and prevents systemic endotoxemia by killing endogenous bacteria (Proteobacteria) produced from LPS in HFD-mice.Citation86 Interestingly, GSDMD is the only GSDM protein that can protect against Salmonella typhimurium gut infection.Citation86
In addition to its activation in intestinal epithelial cells, GSDMD is also activated in colonic macrophages independent of the gut microbiota, making it protective in DSS-induced colitis.Citation31 GSDMD−/− mice treated with DSS exhibit more colitis phenotype, including shorter colon length and more body weight loss on day 9 compared to WT mice by exacerbating cGAS inflammation.Citation31 The use of cGAS inhibitor RU.521 in the DSS-treated mice attenuates colitis phenotypes in WT mice but completely abolishes them in GSDMD−/− mice, making it a potential target for protection from IBD.Citation31
Gasdermin-D mediated macrophage pyroptosis plays a role in inflammatory bowel disorders
Another study targeted GSDMD-mediated pyroptosis in macrophages through TLR4/NFκB signaling pathway in ulcerative colitis using Honokiol, a compound isolated from genus Magnolia.Citation32, Citation87 Wang et al.Citation32 demonstrated that Honokiol targets the TLR4/NFκB suppressing gasdermin-D mediated pyroptosis through anti-inflammatory effects on DSS-induced colitis mice and LPS-induced RAW264.7 macrophages, making Honokiol a promising drug for UC.Citation32 Lastly, GSDMD deficiency plays a role in gastric cancer (GC), where Wang et al.Citation88 showed GSDMD downregulation in mouse GC tissue and human cell lines. GSDMD protects against gastric cancer development by inhibiting the S/G2 cell cycle and abnormal activation of the oncogenic signaling pathway.Citation88
Gasdermin-B regulates inflammatory bowel disorders
Both Gasdermin-B (GSDMB) and Gasdermin-C (GSDMC) play a role in gastrointestinal health. Nitish et al.Citation89 demonstrated that GSDMB is highly expressed and localizes in intestinal epithelial cells (IECs) of Crohn’s Disease (CD) and ulcerative colitis (UC) patients compared to healthy personnel.Citation89–91 They showed that GSDMB full length (FL) promotes cell migration and adhesion, including IEC repair and wound closure by regulating focal adhesion kinase (FAK) phosphorylation through platelet-derived growth factor subunit (PDGFA).Citation89 Whereas, GSDMB deficiency results in dysregulated epithelial wound repair.Citation89–91 In addition, GSDMC, GSDMC2, GSDMC3 and GSDMC4 were upregulated in IECs of mice infected with N.brasiliensis, indicating GSDMCs play a role in worm-induced type 2 immunity.Citation92
The role of gasdermin-D in kidney injury
Studies have further shown the effect of GSDMD-mediated pyroptosis in different acute kidney injuries. GSDMD-NT was activated in acute kidney injury (AKI) and renal tubular cell injury induced by the chemotherapeutic agent cisplatin, leading to pyroptosis and renal inflammatory response.
Interestingly, the deletion of GSDMD in AKI mice models alleviated renal inflammation.Citation93 Following this study, another group revealed that paricalcitol, a vitamin D receptor agonist, alleviates cisplatin-induced AKI by reducing pyroptosis through downregulation of NFκB NLRP3/cleaved caspase-1/GSDMD pathway.Citation60 Moreoever, GSDMD is associated with AKI induced by radial contrast media such as iopromide.Citation61
F. Chen and colleaguesCitation61 investigated the protective effects of acetylbritannilactone, medicinal herb, in iopromide-induced AKI, which targets NLRP3/ASC/GSDMD and release of IL1β and IL18. To further investigate the activation of GSDMD in kidney injury, N. Maio and colleaguesCitation94 determined GSDMD activation in tubular epithelial cell pyroptosis, which plays an essential role in acute and chronic kidney injuries. They showed that GSDMD is activated by caspase-11 through cisplatin and ischemia/reperfusion inducing tubular damage and neutrophil infiltration.Citation94 In addition, GSDMD-NT activation also results in membrane pore formation secreting urinary IL18.Citation94 With that, another group further elucidated the mechanism of tubular epithelial cell pyroptosis in I/R induced acute kidney injury.Citation30 They revealed Tisp40 involved in phosphorylation NFκB p65 leads to overexpression of tubular epithelial cell pyroptosis by targeting NLRP3/cleaved caspase-1/GSDMD-NT in I/R-induced kidney injury.Citation30 These findings show that inhibition of NFκB using parthenolide, and Tisp40 deficiency reduces renal damage. Therefore, they conclude that Tisp40 regulates GSDMD-mediated tubular endothelial cell pyroptosis through NFκB p65 phosphorylation.Citation30
Gasdermin-D in Autoimmune Disease
Emerging insight highlights the role of GSDMD-mediated pyroptosis in autoimmune diseases. GSDMD activation and inhibition have different effects on autoimmune diseases. For example, GSDMD deficiency in Lupus enhances systemic autoimmunity. Thus, GSDMD is essential in regulating Lupus’s immunological dysfunction.Citation95 In contrast, GSDMD deficiency attenuates the pathogenesis of osteoarthritis but does not inhibit the formation of autoantibody-immune complexes.Citation96
GSDMD has recently found to play a protective role in autoimmune hepatitis (AIH), with GSDMD depletion exacerbated liver injury, intestinal barrier damage after concanavalin (ConA) injection to induce AIH.Citation97 These studies conclude that GSDMD regulation is essential in maintaining immunological homeostasis. Furthermore, aberrant inflammasome activation causes different autoinflammatory responses. More studies are needed to investigate the role of GSDMD in autoimmunity.
Summary and perspective
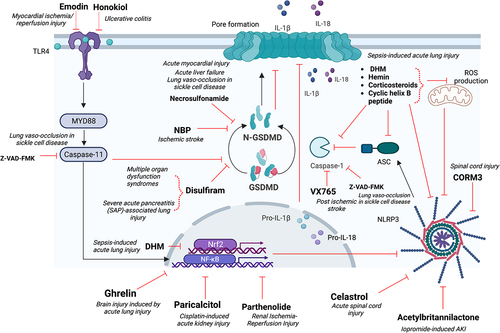
GSDMD-mediated pyroptosis plays a pivotal role in inflammatory diseases resulting in organ injury, including but not limited to the liver, brain, heart, lungs, gastrointestinal tract, and kidneys. Therefore, many studies reveal GSDMD as a potential therapeutic target. They targeted GSDMD through specific inhibition or inhibition of its upstream pathways, specifically NLRP3 inflammasome or cleaved caspase-1/11/4-5 (). GSDMD is part of the Gasdermin (GSDM) family, composed of six members, GSDMA, GSDMB, GSDMC, GSDMD, GSDME/DNFA5, and PVJK/GSDMF.Citation5
Figure 1. GSDMD contributes to organ injury regulation through different pathways: caspase-1, ASC and NLRP3; TLR4-NFκB pathway; Gasdermin-D cleavage, IL1β and IL18 release.
All other members are equally important and play significant roles in cell death pathways. For example, GSDME is a vital regulator in necrosis, where it plays a critical role in tumor suppression.Citation98–100 GSDME and GSDMF were previously identified as DNFA5 and PVJK/DFNB59, respectively, where a mutation in those genes cause age-related hearing loss.Citation6, Citation7 GSDMB is highly expressed in lung epithelium in asthma patients and gut epithelium in inflammatory bowel disease patients;Citation89, Citation91, Citation101 thus, it plays a pivotal role in lung and intestinal injuries. In addition, GSDMA also contributes to inflammatory bowel disease.Citation102 GSDMC is identified as a prognostic factor in lung adenocarcinoma.Citation89 In addition, J. Zhang and colleagues identified caspase-8 mediated cleavage of GSDMC in pyroptosis as a potential therapeutic target for tumor progression.Citation103
GSDMD has been the most extensively studied protein of the GSDM family due to its involvement in inflammatory regulation and homeostasis. Yet, there are limited number of GSDMD inhibitors going into clinical trials. Disulfiram is the only FDA-approved drug and potent GSDMD-NT inhibitor; however, it is only approved for alcoholism.Citation104 Future studies need to investigate the role of disulfiram and adapt it to inflammatory diseases and organ injury.
Acknowledgments
We would like to thank Drs. Alex-Soto Gutierrez and Rodrigo Machado Florentino at the University of Pittsburgh, Department of Pathology for the opportunity to publish
Disclosure statement
No potential conflict of interest was reported by the authors.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Guo H, Callaway J, Ting JY . Inflammasomes: mechanism of action, role in disease, and therapeutics. Nat Med. 2015;21:677–14. https://doi.org/10.1038/nm.3893.
- Zheng D, Liwinski T, Elinav E. Inflammasome activation and regulation: toward a better understanding of complex mechanisms. Cell Discov. 2020;6:36. https://doi.org/10.1038/s41421-020-0167-x.
- Sun Q, Fan J, Billiar TR, et al. Inflammasome and autophagy regulation - a two-way street. Mol Med. 2017;23:188–95. https://doi.org/10.2119/molmed.2017.00077.
- Krakauer T. Inflammasomes, autophagy, and cell death: the Trinity of innate host defense against intracellular bacteria. Mediators Inflamm. 2019;2471215:1–10. https://doi.org/10.1155/2019/2471215.
- Swanson KV, Deng M, Ting JP-Y. The NLRP3 inflammasome: molecular activation and regulation to therapeutics. Nat. Rev. Immunol. 2019;8:477–89. https://doi.org/10.1038/s41577-019-0165-0.
- Laer L, Huizing E, Verstreken M, et al. Nonsyndromic hearing impairment is associated with a mutation in DFNA5. Nat Genet. 1998;20:194–97. https://doi.org/10.1038/2503.
- Zou J, Zheng Y, Huang Y, et al. The versatile gasdermin family: their function and roles in diseases. Front. Immunol. 2021;12:751533. https://doi.org/10.3389/fimmu.2021.751533.
- Saeki N, Kuwahara Y, Sasaki H, et al. Gasdermin (Gsdm) localizing to mouse Chromosome 11 is predominantly expressed in upper gastrointestinal tract but significantly suppressed in human gastric cancer cells. Mammalian Genome. 2000;11:718–24. https://doi.org/10.1007/s003350010138.
- Tamura M, Tanaka S, Fujii T, et al. Members of a novel gene family, Gsdm, are expressed exclusively in the epithelium of the skin and gastrointestinal tract in a highly tissue-specific manner. Genomics. 2007;89:618–29. https://doi.org/10.1016/j.ygeno.2007.01.003.
- Shi J, Zhao Y, Wang K, et al. Cleavage of GSDMD by inflammatory caspases determines pyroptotic cell death. Nat. 2015;526:660–665. https://doi.org/10.1038/nature15514.
- Kayagaki N, Stowe I, Lee B, et al. Caspase-11 cleaves gasdermin D for non-canonical inflammasome signalling. Nat. 2015;526:666–71. https://doi.org/10.1038/nature15541.
- He W, Wan H, Hu L, et al. Gasdermin D is an executor of pyroptosis and required for interleukin-1β secretion. Cell Res. 2015;25:1285–98. https://doi.org/10.1038/cr.2015.139.
- Taghavi S, Askari R. Liver trauma.Treasure island (FL). StatPearls Publishing; 2022.
- Badger SA, Barclay R, Campbell P, et al. Management of liver trauma. World J Surg. 2009;33:2522–37. https://doi.org/10.1007/s00268-009-0215-z.
- Rodríguez-Antonio I, López-Sánchez GN, Uribe M, et al. Role of the inflammasome, gasdermin D, and pyroptosis in non-alcoholic fatty liver disease. J Gastroenterol Hepatol. 2021;36:2720–27. https://doi.org/10.1111/jgh.15561.
- Xu B, Jiang M, Chu Y, et al. Gasdermin D plays a key role as a pyroptosis executor of non-alcoholic steatohepatitis in humans and mice. J Hepatol. 2018;68:773–82. https://doi.org/10.1016/j.jhep.2017.11.040.
- Yin K, Zhou X, Jiang W, et al. Jiangzhi ligan decoction inhibits GSDMD-Mediated canonical/noncanonical pyroptosis pathways and alleviates high-fat diet-induced nonalcoholic fatty liver disease. Disease Markers. 2021;9963534:1–11. https://doi.org/10.1155/2021/9963534.
- Beier JI, Banales JM. Pyroptosis: an inflammatory link between NAFLD and NASH with potential therapeutic implications. J. Hepatol. 2021;68:643–45. https://doi.org/10.1016/j.jhep.2018.01.017.
- Gaul S, Leszczynska A, Alegre F, et al. Hepatocyte pyroptosis and release of inflammasome particles induce stellate cell activation and liver fibrosis. J Hepatol. 2021;74:156–67.
- Wang J, Shi K, An N, et al. Direct inhibition of GSDMD by PEITC reduces hepatocyte pyroptosis and alleviates acute liver injury in mice. Front. Immunol. 2022;13:825428. https://doi.org/10.3389/fimmu.2022.825428.
- Wu Y-L, Ou W, Lin S, et al. GSDMD inhibitor NECROSULFONAMIDE protects mice from galactosamine/lipopolysaccharide-induced acute liver failure via pyrotosis pathway. J Clin Transl Hepatol. 2020:73. https://doi.org/10.1016/s0168-8278(20.
- Li J, Hao JH, Yao D, et al. Caspase-1 inhibition prevents neuronal death by targeting the canonical inflammasome pathway of pyroptosis in a murine model of cerebral ischemia. CNS Neurosci Ther. 2020;26:925–39.
- Ye B, Chen X, Dai S, et al. Emodin alleviates myocardial ischemia/reperfusion injury by inhibiting gasdermin D-mediated pyroptosis in cardiomyocytes. Drug Des Devel Ther. 2019;13:975–90. https://doi.org/10.2147/DDDT.S195412.
- Gao J, Chen Y, Wang H, et al. Gasdermin D deficiency in vascular smooth muscle cells ameliorates abdominal aortic aneurysm through reducing putrescine synthesis. Adv Sci. 2022:e2204038. https://doi.org/10.1002/advs.202204038.
- Luo YP, Jiang L, Kang K, et al. Hemin inhibits NLRP3 inflammasome activation in sepsis-induced acute lung injury, involving heme oxygenase-1. Int Immunopharmacol. 2014;20:24–32. https://doi.org/10.1016/j.intimp.2014.02.017.
- Yang JW, Mao B, Tao RJ, et al. Corticosteroids alleviate lipopolysaccharide-induced inflammation and lung injury via inhibiting NLRP3-inflammasome activation. J Cell Mol Med. 2020;24:12716–25. https://doi.org/10.1111/jcmm.15849.
- Zhang XP, Zhang WT, Qiu Y, et al. Cyclic helix B peptide alleviates sepsis-induced acute lung injury by downregulating NLRP3 inflammasome activation in alveolar macrophages. Int Immunopharmacol. 2020;88:106849. https://doi.org/10.1016/j.intimp.2020.106849.
- Shao XF, Li B, Shen J, et al. Ghrelin alleviates traumatic brain injury-induced acute lung injury through pyroptosis/NF-κB pathway. Int Immunopharmacol. 2020;79:106175. https://doi.org/10.1016/j.intimp.2019.106175.
- Vats R, Kaminski TW, Brzoska T, et al. Liver-to-lung microembolic NETs promote gasdermin D-dependent inflammatory lung injury in sickle cell disease. Blood. 2022;140:1020–37. https://doi.org/10.1182/blood.2021014552.
- Xiao C, Zhao H, Zhu H, et al. Tisp40 induces tubular epithelial cell GSDMD-mediated pyroptosis in renal ischemia-reperfusion injury via NF-κB signaling. Front. Physiol. 2020;11:906. https://doi.org/10.3389/fphys.2020.00906.
- Ma C, Yang D, Wang B, et al. Gasdermin D in macrophages restrains colitis by controlling cGAS-mediated inflammation. Sci Adv. 2020;6:eaaz6717. https://doi.org/10.1126/sciadv.aaz6717.
- Wang N, Kong R, Han W, et al. Honokiol alleviates ulcerative colitis by targeting PPAR-γ-TLR4-NF-κB signaling and suppressing gasdermin-D-mediated pyroptosis in vivo and in vitro. Int Immunopharmacol. 2022;111:109058. https://doi.org/10.1016/j.intimp.2022.109058.
- Rathkey JK, Zhao J, Liu Z, et al. Chemical disruption of the pyroptotic pore-forming protein gasdermin D inhibits inflammatory cell death and sepsis. Sci Immunol. 2018;3:eaat2738. https://doi.org/10.1126/sciimmunol.aat2738.
- de Rivero Vaccari JP. Carbon monoxide releasing molecule-3 inhibits inflammasome activation: a potential therapy for spinal cord injury. EBioMedicine. 2019;40:17–18. https://doi.org/10.1016/j.ebiom.2019.01.020.
- Yang C, Sun P, Deng M, et al. Gasdermin D protects against noninfectious liver injury by regulating apoptosis and necroptosis. Cell Death Dis. 2019;10:481. https://doi.org/10.1038/s41419-019-1719-6.
- Sun P, Zhong J, Liao H, et al. Hepatocytes are resistant to cell death from canonical and non-canonical inflammasome-activated pyroptosis. Cmgh. 2020;13:739–57. https://doi.org/10.1016/j.jcmgh.2021.11.009.
- Xingyu L, Jiang C, Jiayan H, et al. Gasdermin D–mediated pyroptosis suppresses liver regeneration after 70% partial hepatectomy. Hepatol Commun. 2022;6:2340–53. https://doi.org/10.1002/hep4.1973.
- Yamagishi R, Kamachi F, Nakamura M, et al. Gasdermin D-mediated release of IL-33 from senescent hepatic stellate cells promotes obesity-associated hepatocellular carcinoma. Sci Immunol. 2022;7:eabl7209. https://doi.org/10.1126/sciimmunol.abl7209.
- Li J, Zhao J, Xu M, et al. Blocking GSDMD processing in innate immune cells but not in hepatocytes protects hepatic ischemia–reperfusion injury. Cell Death Dis. 2020;11:244. https://doi.org/10.1038/s41419-020-2437-9.
- Yang X, Cheng X, Tang Y, et al. Bacterial endotoxin activates the coagulation cascade through gasdermin d-dependent phosphatidylserine exposure. Immunity. 2019;51:983–996.e6.
- Wang K, Sun Z, Ru J, et al. Ablation of GSDMD improves outcome of ischemic stroke through blocking canonical and non-canonical inflammasomes dependent pyroptosis in microglia. Front. Neurol. 2020;11:577927. https://doi.org/10.3389/fneur.2020.577927.
- Zhou K, Shi L, Wang Y, et al. Recent advances of the NLRP3 inflammasome in central nervous system disorders. J. Immunol. Res. 2016;9238290:1–9. https://doi.org/10.1155/2016/9238290.
- Shao BZ, Cao Q, Liu C. Targeting NLRP3 inflammasome in the treatment of CNS diseases. Front. Mol. Neurosci. 2018;11:320. https://doi.org/10.3389/fnmol.2018.00320.
- Walsh J, Muruve D, Power C. Inflammasomes in the CNS. Nat Rev Neurosci. 2014;15:84–97. https://doi.org/10.1038/nrn3638.
- Song L, Pei L, Yao S, et al. NLRP3 inflammasome in neurological diseases, from functions to therapies. Front. Cell. Neurosci. 2017;11:63. https://doi.org/10.3389/fncel.2017.00063.
- Zhang D, Qian J, Zhang P, et al. Gasdermin D serves as a key executioner of pyroptosis in experimental cerebral ischemia and reperfusion model both in vivo and in vitro. Journal of Neuroscience Research. 2019;97:645–60. https://doi.org/10.1002/jnr.24385.
- Yuan B, Zhou XM, You ZQ, et al. Inhibition of AIM2 inflammasome activation alleviates GSDMD-induced pyroptosis in early brain injury after subarachnoid haemorrhage. Cell Death Dois. 2021;11:76. https://doi.org/10.1038/s41419-020-2248-z.
- Chen L, Deng H, Cui H, et al. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget. 2017;9:7204–18. https://doi.org/10.18632/oncotarget.23208.
- Okada S. The pathophysiological role of acute inflammation after spinal cord injury. Inflamm and regener. 2016;36:20. https://doi.org/10.1186/s41232-016-0026-1.
- Dai W, Wang X, Teng H, et al. Celastrol inhibits microglial pyroptosis and attenuates inflammatory reaction in acute spinal cord injury rats. Int Immunopharmacol. 2019;66:215–23. https://doi.org/10.1016/j.intimp.2018.11.029.
- Xu S, Wang J, Zhong J, et al. CD73 alleviates GSDMD-mediated microglia pyroptosis in spinal cord injury through PI3K/AKT/Foxo1 signaling. Clin Transl Med. 2021;11:e269. https://doi.org/10.1002/ctm2.269.
- Al Mamun A, Wu Y, Monalisa I, et al. Role of pyroptosis in spinal cord injury and its therapeutic implications. J Advanced Res. 2020;28:97–109. https://doi.org/10.1016/j.jare.2020.08.004.
- Wang SN, Guo XY, Tang J, et al. Expression and localization of absent in melanoma 2 in the injured spinal cord. Neural Regen Res. 2019;14:542–52. https://doi.org/10.4103/1673-5374.245481.
- Jiang K, Tu Z, Chen K, et al. Gasdermin D inhibition confers antineutrophil-mediated cardioprotection in acute myocardial infarction. J Clin Invest. 2022;132:e151268. https://doi.org/10.1172/JCI151268.
- Han B, Xu J, Shi X. et al. DL-3-n-Butylphthalide attenuates myocardial hypertrophy by targeting gasdermin D and inhibiting gasdermin D mediated inflammation. Front Pharmacol. 2021;12:688140. https://doi.org/10.3389/fphar.2021.688140.
- Wang Y, Liu Q, Zheng Q, et al. Dihydromyricetin Alleviates sepsis-induced acute lung injury through inhibiting NLRP3 inflammasome-dependent pyroptosis in mice model. Inflamm. 2019;42:1301–10. https://doi.org/10.1007/s10753-019-00990-7.
- Wu J, Zhang J, Zhao J, et al. Treatment of severe acute pancreatitis and related lung injury by targeting gasdermin D-mediated pyroptosis. Front.Cell Dev. Biol. 2021;9:780142. https://doi.org/10.3389/fcell.2021.780142.
- Lin T, Song J, Pan X, et al. Downregulating Gasdermin D reduces severe acute pancreatitis associated with pyroptosis. Med Sci Monit. 2021;27:e927968. https://doi.org/10.12659/MSM.927968.
- Silva C, Wanderley C, Veras FP, et al. Gasdermin D inhibition prevents multiple organ dysfunction during sepsis by blocking NET formation. Blood. 2021;138:2702–13. https://doi.org/10.1182/blood.2021011525.
- Jiang S, Zhang H, Li X, et al. Vitamin D/VDR attenuate cisplatin-induced AKI by down-regulating NLRP3/Caspase-1/GSDMD pyroptosis pathway. J Steroid Biochem Mol Biol. 2021;206:105789. https://doi.org/10.1016/j.jsbmb.2020.105789.
- Chen F, Lu J, Yang X, et al. Acetylbritannilactone attenuates contrast-induced acute kidney injury through its anti-pyroptosis effects. Biosci Rep. 2020;40:BSR20193253. https://doi.org/10.1042/BSR20193253.
- Lei Q, Yi T, Chen C. NF-κB-Gasdermin D (GSDMD) axis couples oxidative stress and NACHT, LRR and PYD domains-containing protein 3 (NLRP3) inflammasome-mediated cardiomyocyte pyroptosis following myocardial infarction. Med Sci Monit. 2018;24:6044–52. https://doi.org/10.12659/MSM.908529.
- Shi H, Gao Y, Dong Z, et al. GSDMD-mediated cardiomyocyte pyroptosis promotes myocardial I/R injury. Circ Res. 2021;129:383–96. https://doi.org/10.1161/CIRCRESAHA.120.318629.
- Dai S, Ye B, Zhong L, et al. GSDMD mediates LPS-induced septic myocardial dysfunction by regulating ROS-dependent NLRP3 inflammasome Activation. Front Cell and Dev Biol. 2021;9:779432. https://doi.org/10.3389/fcell.2021.779432.
- Ciesielska A, Matyjek M, Kwiatkowska K. TLR4 and CD14 trafficking and its influence on LPS-induced pro-inflammatory signaling. Cell. Mol. Life Sci. 2021;78:1233–61. https://doi.org/10.1007/s00018-020-03656-y.
- Zhang KZ, Shen XY, Wang M, et al. Retinol-Binding Protein WM. 4 promotes cardiac injury after myocardial infarction via inducing cardiomyocyte pyroptosis through an interaction with NLRP3. Journal of the American Heart Association. 2021;10:e022011. https://doi.org/10.1161/JAHA.121.022011.
- Wu Y, Pan B, Zhang Z, et al. Caspase-4/11-mediated pulmonary artery endothelial cell pyroptosis contributes to pulmonary arterial hypertension. Hypertension. 2021;79:536–48. https://doi.org/10.1161/HYPERTENSIONAHA.121.17868.
- Jia C, Zhang J, Chen H, et al. Endothelial cell pyroptosis plays an important role in Kawasaki disease via HMGB1/RAGE/cathespin B signaling pathway and NLRP3 inflammasome activation. Cell Death Dis. 2019;10:778. https://doi.org/10.1038/s41419-019-2021-3.
- Wang Q, Wu J, Zeng Y, et al. Pyroptosis: A pro-inflammatory type of cell death in cardiovascular disease. Clinic Chimic Acta. 2020;510:62–72. https://doi.org/10.1016/j.cca.2020.06.044.
- Yang F, Qin Y, Lv J, et al. Silencing long non-coding RNA Kcnq1ot1 alleviates pyroptosis and fibrosis in diabetic cardiomyopathy. Cell Death Dis. 2018;9:1000. https://doi.org/10.1038/s41419-018-1029-4.
- Zheng D, Shi Z, Yang M, et al. NLRP3 inflammasome-mediated endothelial cells pyroptosis is involved in decabromodiphenyl ethane-induced vascular endothelial injury. Chemosphere. 2021;267:128867. https://doi.org/10.1016/j.chemosphere.2020.128867.
- Puylaert P, Van Praet M, Vaes F, et al. Gasdermin D deficiency limits the transition of atherosclerotic plaques to an inflammatory phenotype in ApoE knock-out mice. Biomedicines. 2022;10:1171. https://doi.org/10.3390/biomedicines10051171.
- Mitra S, Exline M, Habyarimana F, et al. Microparticulate caspase HF. 1 Regulates gasdermin D and pulmonary vascular endothelial cell injury. Am Journal Respir Cell Mol Biol. 2018;59:56–64. https://doi.org/10.1165/rcmb.2017-0393OC.
- Chavez L, Meguro J, Chen S, et al. Circulating extracellular vesicles activate the pyroptosis pathway in the brain following ventilation-induced lung injury. J Neuroinflammation. 2021;18:310. https://doi.org/10.1186/s12974-021-02364-z.
- Martínez MC, Tesse A, Zobairi F, et al. Shed membrane microparticles from circulating and vascular cells in regulating vascular function. Am J Physiol Heart Circ Physiol. 2005;28:H1004–H1009. https://doi.org/10.1152/ajpheart.00842.2004.
- Martin S, Tesse A, Hugel B, et al. Shed membrane particles from T lymphocytes impair endothelial function and regulate endothelial protein expression. Circulation. 2004;109:1653–59. https://doi.org/10.1161/01.CIR.0000124065.31211.6E.
- Wu DD, Pan PH, Liu B, et al. Inhibition of alveolar macrophage pyroptosis reduces lipopolysaccharide-induced acute lung injury in mice. Chin Med J (Eng). 2015;128:2638–45. https://doi.org/10.4103/0366-6999.166039.
- He X, Qian Y, Li Z, et al. TLR4-Upregulated IL-1β and IL-1RI promote alveolar macrophage pyroptosis and lung inflammation through an autocrine mechanism. Sci Rep. 2016;6:31663. https://doi.org/10.1038/srep31663.
- Wu D, Pan P, Su X, et al. Interferon regulatory factor-1 mediates alveolar macrophage pyroptosis during LPS-induced acute lung injury in mice. Shock. 2016;46:329–38. https://doi.org/10.1097/SHK.0000000000000595.
- Yang J, Zhao Y, Zhang P, et al. Hemorrhagic shock primes for lung vascular endothelial cell pyroptosis: role in pulmonary inflammation following LPS. Cell Death Dis. 2016;7:e2363. https://doi.org/10.1038/cddis.2016.274.
- Hu Q, Zhang T, Yi L, et al. Dihydromyricetin inhibits NLRP3 inflammasome-dependent pyroptosis by activating the Nrf2 signaling pathway in vascular endothelial cells. BioFactors. 2018;44:123–36. https://doi.org/10.1002/biof.1395.
- Li D, Li C, Wang T, et al. Geranylgeranyl diphosphate synthase 1 knockdown suppresses NLRP3 inflammasome activity via promoting autophagy in sepsis-induced acute lung injury. Int Immunopharmacol. 2021;100:108106. https://doi.org/10.1016/j.intimp.2021.108106.
- Xu WJ, Wang XX, Jin JJ, et al. Inhibition of GGPPS1 attenuated LPS-induced acute lung injury and was associated with NLRP3 inflammasome suppression. Am J Physiol Lung Cell Mol Physiol. 2019;316:L567–L577. https://doi.org/10.1152/ajplung.00190.2018.
- Gao H, Cao M, Yao Y. Dysregulated microbiota-driven GASDERMIN D activation promotes colitis development by mediating IL-18 release. Front Immunol. 2022;12:750841. https://doi.org/10.3389/fimmu.2021.750841.
- Bulek K, Zhao J, Liao Y. Epithelial-derived Gasdermin d mediates nonlytic il-1β release during experimental colitis. J Clin Invest. 2020;130:4218–34. https://doi.org/10.1172/jci138103.
- Fattinger SA, Maurer L, Geiser P, et al. Gasdermin D is the only Gasdermin that provides non-redundant protection against acute salmonella gut infection. bioRxiv. 2022. https://doi.org/10.1101/2022.11.24.517575.
- Abdel-Wahab B, Alkahtani S, Alqahtani A, et al. Umbelliferone ameliorates ulcerative colitis induced by acetic acid via modulation of TLR4/NF-κB-p65/iNOS and SIRT1/PPARγ signaling pathways in rats. Environ Sci Pollut Res. 2022;29:37644–59. https://doi.org/10.1007/s11356-021-18252-1.
- Wang WJ, Chen D, Jiang MZ, et al. Downregulation of gasdermin D promotes gastric cancer proliferation by regulating cell cycle-related proteins. J Dig Dis. 2018;19:74–83. https://doi.org/10.1111/1751-2980.12576.
- Rana N, Privitera G, Kondolf HC, et al. GSDMB is increased in IBD and regulates epithelial restitution/repair independent of pyroptosis. Cell. 2022;185:283–98. https://doi.org/10.1016/j.cell.2021.12.024.
- Privitera G, Pizarro TT. Live or let die: translational insights and clinical perspectives of gasdermin B-dependent intestinal epithelial cell fate. Clinical and Translational Medicine. 2022;12:e787. [Accessed 24 April 2022]. https://doi.org/10.1002/ctm2.787.
- Ivanov AI, Rana N, Privitera G, et al. The enigmatic roles of epithelial gasdermin B: recent discoveries and controversies. Trends Cell Biol. 2023;33:48–59. https://doi.org/10.1016/j.tcb.2022.06.006.
- Xi R, Montague J, Lin X, et al. Up-regulation of gasdermin C in mouse small intestine is associated with lytic cell death in enterocytes in worm-induced type 2 immunity. Proc Natl Acad of Sci U S A. 2021;118:e2026307118. [Accessed 29 April 2022]. https://doi.org/10.1073/pnas.2026307118.
- Li Y, Xia W, Wu M, et al. Activation of GSDMD contributes to acute kidney injury induced by cisplatin. Am J Physiol. Renal Physiol. 2020;318:F96–F106. https://doi.org/10.1152/ajprenal.00351.2019.
- Miao N, Yin F, Xie H, et al. The cleavage of gasdermin D by caspase-11 promotes tubular epithelial cell pyroptosis and urinary IL-18 excretion in acute kidney injury. Kidney Int. 2019;96:1105–20. https://doi.org/10.1016/j.kint.2019.04.035.
- Wang X, Blanco LP, Carmona-Rivera C, et al. Effects of gasdermin D in modulating murine lupus and its associated organ damage. Arthritis Rheumatol. 2020;72:2118–29. https://doi.org/10.1002/art.41444.
- Yang T, Sun K, Wang C, et al. Gasdermin D deficiency attenuates arthritis induced by traumatic injury but not autoantibody-assembled immune complexes. Arthritis Res Ther. 2021;23:286. https://doi.org/10.1186/s13075-021-02668-8.
- Wang K, Wu W, Jiang X, et al. Multi-Omics Analysis JX. Reveals the protection of gasdermin D in concanavalin A-induced autoimmune hepatitis. Microbiol Spectr. 2022;10:e0171722. https://doi.org/10.1128/spectrum.01717-22.
- Zhang Z, Zhang Y, Xia S, et al. Gasdermin e suppresses tumour growth by activating anti-tumour immunity. Nat. 2020;579:415–20. https://doi.org/10.1038/s41586-020-2071-9.
- Zhou B, Abbott DW. Gasdermin e permits interleukin-1 beta release in distinct sublytic and pyroptotic phases. Cell Rep. 2021;35:108998. https://doi.org/10.1016/j.celrep.2021.108998.
- Wang Y, Peng J, Xie X, et al. Gasdermin e-mediated programmed cell death: an unpaved path to tumor suppression. J Cancer. 2021;12:5241–48. https://doi.org/10.7150/jca.48989.
- Das S, Miller M, Beppu AK, et al. GSDMB induces an asthma phenotype characterized by increased airway responsiveness and remodeling without lung inflammation. Proc Natl Acad Sci U S A. 2016;113:13132–37. https://doi.org/10.1073/pnas.1610433113.
- Söderman J, Berglind L, Almer S. Gene expression-Genotype AS Analysis implicates GSDMA, GSDMB, and LRRC3C as contributors to inflammatory bowel disease susceptibility. BioMed Res Int. 2015:834805. https://doi.org/10.1155/2015/834805.
- J-yuan Z, Zhou B, R-yue S, et al. The metabolite α-kg induces GSDMC-dependent pyroptosis through death receptor 6-activated caspase-8. Cell Res. 2021;31:980–97. https://doi.org/10.1038/s41422-021-00506-9.
- Hu JJ, Liu X, Xia S, et al. FDA-approved disulfiram inhibits pyroptosis by blocking gasdermin D pore formation. Nat Immunol. 2020;21:736–45. https://doi.org/10.1038/s41590-020-0669-6.
