Abstract
Introduction
Caustic substance ingestion is frequently life-threatening, and its pathological mechanisms of tissue damage are well documented. However, few studies have assessed the combined effects of pH and the ingested dose on patient outcomes. Additionally, the miscellaneous chemical properties are not immediately available for providing predictive insights to physicians. This study aimed to provide a new perspective of the risk assessment of caustic substance ingestion based on the pH and dose.
Methods
The retrospective study analyzed adults treated for caustic substance ingestion at Chang Gung Memorial Hospital between January 1999 and December 2018. Uniformly strict inclusion/exclusion criteria and a double-checked process during chart review were adopted. All patients underwent urgent esophagogastroduodenoscopy (EGD) within 24 h. Caustic mucosal damage was graded using Zargar’s modified endoscopic classification. The pH and ingested dose of caustic substances were clearly recorded. Statistical analyses were conducted using IBM SPSS, version 22.
Results
Based on the 468 enrolled cases, the pH and dose were valuable predictors of the extent of gastrointestinal tract injury, commonly encountered complications, and long-term overall survival outcomes. Risks of mortality and perforation were dose-dependent for acids and pH-dependent for alkalis. The severe EGD findings (grade ≥ 2b) in this study were pH-dependent for both substances and additionally dose-dependent for acids.
Conclusion
Combining pH and dose, we proposed a new perspective for the risk assessment of caustic substance ingestion. Such findings may provide predictive insights for resolving clinical uncertainty before the availability of examination results. “Large doses of acids” and “high pH of alkalis” deserve special attention. This new perspective with a retrospective nature requires further validation.
Introduction
Caustic substance ingestion is an uncommon but difficult problem worldwide. Caustic injury of the gastrointestinal (GI) tract frequently is life-threatening, especially in adults, and causes a wide variety of complications for patients and places a heavy burden on healthcare organizations [Citation1–11].
Over the past century, experimental studies of animals and microscopic analyses of resected human tissues have constituted the current pathologic framework of caustic ingestion [Citation12–17]. Essential theories have been widely accepted, namely that strong acids cause coagulation necrosis/eschar formation and thus limit deepening, whereas strong alkalis are notorious for their penetrating nature associated with saponification/liquefaction effects [Citation1,Citation2,Citation7,Citation8,Citation11,Citation18,Citation19]. Both strong caustics and large ingested doses serve as risk factors for caustic injury patients. Nevertheless, scarce research has examined the combined effects of these variables on patient outcomes.
Conversely, the consensus is that caustic tissue damage simultaneously depends on the type of substance, commercial formulation, pH, dose, concentration, viscosity, duration of contact, and the concept of titratable acid/alkaline reserve [Citation1–3,Citation6–8,Citation11,Citation18–24]. However, exact information is difficult to obtain [Citation1,Citation8,Citation11]. In clinical situations, miscellaneous caustic properties cannot immediately or directly offer physicians predictive insights. Moreover, symptoms are not sufficiently specific for the severity of injuries [Citation2,Citation6,Citation18,Citation19]. This study aimed to provide clinical physicians with a new perspective to overcome clinical uncertainty prior to examination data. The extent of GI tract injury, commonly encountered complications, and long-term overall survival outcomes are three important aspects for patients with caustic injury. We examined whether pH and ingested dose could provide an accurate risk assessment.
Methods
Study population and data extraction
This study was reviewed and approved by the Chang Gung Memorial Hospital (CGMH) institutional review board (IRB number: 202000583B3). Adult and elderly patients were defined as those ≥18 and ≥65 years old, respectively. We searched our comprehensive electronic database to find all adults who sought medical assistance at CGMH emergency department (ED) for caustic substance ingestion between January 1999 and December 2018. The corresponding and first authors double-screened the cases by strictly following the exclusion criteria. We excluded any case that could not simultaneously fulfill all of the following conditions: (1) definite evidence to support the ingestion of caustic substances, (2) undergoing urgent EGD within 24 h, (3) substance pH values confirmed by either container labels or toxicology laboratory reports, and (4) cross-validated ingested dose from different information origins. After screening, data for enrolled cases were collected under electronic chart review by the authors, who are all licensed physicians and are familiar with the hospital database and our study project. A standardized extraction form was used in the full chart review process after a thorough discussion. Data for all variables were double-checked case by case by the first author in pursuit of accuracy.
The pH value of ingested caustic substances was confirmed by the label on containers or measured by the toxicology laboratories. Strong caustics were defined as substances with pH <2 or >12. The obtained ingested dose was strictly cross-validated during the full chart review. Information was originally obtained from patients, family, and caregivers; records from emergency medical technicians or referral physicians; and face-to-face diagnostic interview reports from psychiatrists. If available, the amounts of caustic substances left in the containers also were checked. All cases with vague information, equivocal narratives, or discrepant information were excluded. The intent of ingestion, psychiatric comorbidities, previous suicide attempts, treatment courses, intensive care unit (ICU) admittance, and GI/systemic complications also were reviewed for each patient.
Caustic mucosal damage of the GI tract was graded using Zargar’s modified endoscopic classification (0, 1, 2a, 2b, 3a, and 3b) [Citation25]. An injury grade ≥ 2b was defined as severe damage. Approximately half of the urgent EGDs were performed by the same endoscopist (Cheng H-T), who also reviewed the endoscopic photos of all other enrolled patients and confirmed the Zargar’s grades for consistency and accuracy.
Early management and patient care
Baseline laboratory data, including hematologic and biochemical data, were collected upon arrival to the ED. Urgent EGD was performed within 24 h after substance ingestion in all patients if possible. Patients with toxic signs, suspected respiratory system involvement, or other indications underwent plain chest radiography (CXR) or computed tomography (CT).
EGD is available 24 h a day at CGMH. EGD was performed by experienced endoscopists within 24 h of substance ingestion using standard upper GI endoscopes (GIF XQ-230 [9.2 mm], GIF Q-240X [9.4 mm], GIF Q-260J [9.9 mm], and GIF Q-260 [9.2 mm]; Olympus, Tokyo, Japan). Oral xylocaine spray was used except in patients who required ventilation support under general anesthesia for respiratory difficulty or unclear consciousness. Insufflation and retrovision maneuvers were carefully performed or avoided in patients with severe injury.
Proton pump inhibitors or H2 antagonists were prescribed to treat caustic injury. Patients received parenteral nutrition without oral intake until their clinical status was regarded as stable. In cases of suspected infection, blood cultures were obtained before the administration of antibiotics (gentamicin and first-generation cephalosporins). Once destabilization or respiratory difficulty was encountered, a patient was transferred to the ICU for critical care. Follow-up EGD was performed if indicated. After discharge, patients were followed up in the outpatient clinic for at least 6 months. Although the exact treatment strategies might have been altered individually according to different clinical conditions, the major principles for similar cases did not change significantly during the past 20 years at our center.
Complications
Any observed GI or systemic complications were recorded during follow-up. Upper GI complications included perforation, bleeding, fistula, and stricture formation. Bleeding was defined as melena, hematemesis, or coffee ground vomitus. Perforation and/or fistula formation was diagnosed using CXR, CT, or endoscopy. Stricture was indicated by symptoms of dysphagia, regurgitation, or odynophagia with confirmation via endoscopy or upper GI radiography.
Systemic complications included aspiration injury, respiratory failure, hepatic injury, renal injury, sepsis, and disseminated intravascular coagulation (DIC). Hepatic injury was defined as serum alanine aminotransferase or aspartate aminotransferase elevation to 3× the upper limit of normal. Renal injury was defined as serum creatinine levels >1.4 mg/dL without other noted renal diseases.
Statistical analyses
The demographic data of continuous variables were expressed as the median and interquartile range (IQR = Q3 − Q1) or range, and those of categorical variables were presented as numbers with percentages. The calculation of percentages excluded patients with missing values from the chart review. All statistical tests were two-sided, and they were performed using Statistical Product and Service Solutions version 22 (IBM, Armonk, NY, USA). The categorical variables were assessed via Pearson’s χ2 tests or Fisher’s exact tests. Multivariate logistic regression analyses were conducted to explore the associations among dose, pH, endoscopic findings, and complications. The odds ratio (OR) and 95% confidence interval (CI) were reported. The Kaplan–Meier method was used for survival analyses in the univariate setting, and the differences between survival curves were assessed via log-rank tests. Cox proportional hazards models were used performed alternatively in the multivariate setting to obtain the hazard ratio (HR) and 95% CI. p < 0.05 was considered statistically significant.
Results
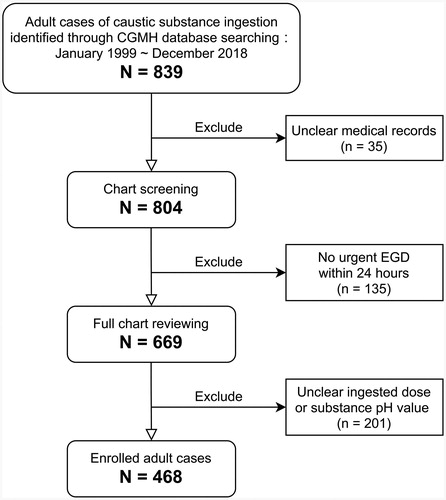
We retrospectively searched the medical records of patients treated for caustic substance ingestion between 1999 and 2018 at CGMH. Initially, 839 adults were identified. We excluded 35 patients due to unclear medical records and 135 because an urgent esophagogastroduodenoscopy (EGD) survey was not conducted within 24 h. A full chart review was conducted for the remaining 669 patients to obtain details about the etiology and clinical course of caustic injury. Another 201 patients were excluded because their records on the ingested dose or substance pH were vague or unclear. Thus, 468 adults were included in our study ().
Figure 1. Diagram of the study population enrollment. CGMH, Chang Gung Memorial Hospital; EGD, esophagogastroduodenoscopy.
Patient characteristics
The 468 patients included 215 males (45.9%) and 253 females (54.1%), and the median patient age at the time of substance ingestion was 41 years (IQR = 26, range = 18–107). Approximately three-quarters of patients reported intentional ingestion, and 37 patients (7.9%) recalled previous suicide/self-harm attempts. The median ingested dose was 100 mL (IQR = 150, range = 5–1000). Strong caustic substances accounted for 65.6% of ingested substances. The most commonly ingested substances were household toilet cleaners (n = 171, 36.5%; strong acids), followed by caustic soda (n = 55, 11.8%; strong alkalis) and bleach (n = 43, 9.2%; chlorine-based beach, 35; and peroxide-based bleach, 8). The median follow-up was 10.6 months (IQR = 92.2; range = 1 day to 234 months). The overall survival rates at 6 months and 1, 3, 5, and 10 years were 92.4, 89.4, 85.8, 82.6, and 71.8%, respectively.
Cases of caustic injury of the GI tract were categorized as mild (EGD grade 0, 1, or 2a) or severe (EGD grade 2b, 3a, or 3b). The grades for 12 patients (2.6%) with stomach injury and 51 (10.9%) with duodenal injury were excluded from analyses for three reasons: (1) patient intolerance to further examination, (2) incomplete study because of a high perforation risk, and (3) invisibility of the mucosa because of the absence of standard bowel preparation in urgency. As presented in , severe injury was associated with advanced age (p = 0.001), female gender (p = 0.020), intentional ingestion (p = 0.026), large doses (p = 0.0496), and strong caustics (p < 0.001). Such etiologies led to significantly higher rates of GI/systemic complications and greater medical resources distribution ().
Table 1. Demographic characteristics of the enrolled patients with caustic substance ingestion.
Table 2. Outcomes and clinical courses of the enrolled patients with caustic substance ingestion.
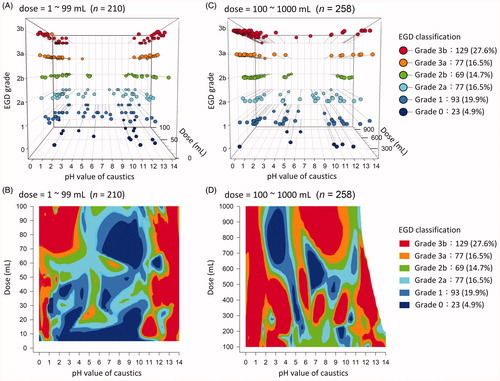
illustrates the findings for caustic injuries (n = 468) of various severity caused by substances with different doses and pH values. The “U-shaped” distribution in and contour plot in reveals that strong caustics (pH <2 or >12) predicted high-grade damage in the case of small doses. As the ingested dose increased, neither pH nor the dose alone could explain the severity of injuries ().
Behavior-related etiology
The ingested doses are distributed by pH in . The doses of strong caustic substances (pH <2 or >12), especially strong alkalis, had a smaller median and IQR. This suggests the “strong acids/alkalis” themselves, to some extent, limited the ingested dose during ingestion.
Impacts on EGD grading
Multivariate logistic regression analyses were performed to explore the associations among dose, pH, and severity of damage in the esophagus, stomach, and duodenum (). Regarding acidic substances, caustic injury was simultaneously pH- and dose-dependent. The factor of “pH < 2” significantly increased the risks of severe injury (EGD ≥ 2b) in the esophagus, stomach, and duodenum by 4.4- (OR = 4.40), 10.9- (OR = 10.92), and 23.5-fold (OR = 23.50), respectively. The increasingly pH-dependent trend could be visually observed in , illustrating that severe injuries converged toward strong acid areas from the esophagus to duodenum in low-dose scenarios. In addition, the ingestion of each additional 100 mL of caustic substances increased the risk of injury in the esophagus, stomach, and duodenum by 1.4- (OR = 1.39), 1.3- (OR = 1.29), and 1.7-fold (OR = 1.73) higher, respectively. The dose-dependent trend could explain the severe injuries caused by large-dose weak acids, as observed in .
Figure 4. Severity of caustic injury in the esophagus, stomach, and duodenum as assessed via esophagogastroduodenoscopy (EGD).
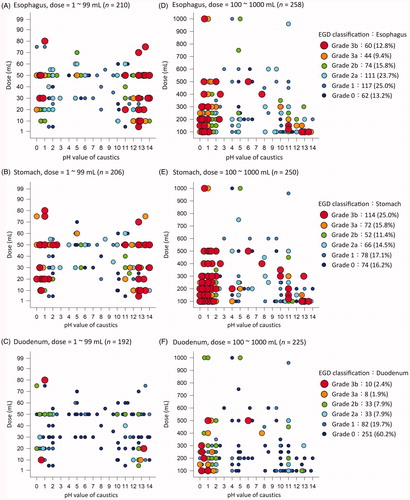
Table 3. Risk assessment of dose, pH, endoscopic findings, complications, and long-term survival outcomes.
For strong alkali (pH > 12) ingestion, the severity of damage under EGD was simply pH-dependent (). The risk of severe injury in the esophagus and stomach was increased by 10.8- (OR = 10.80) and 4.0-fold (OR 4.00), respectively, by strong alkalis. The risks of duodenal injury were insignificantly associated with pH (p = 0.153) or dose (p = 0.583). The absence of a dose-dependent trend in this study was consistent with the small number of severe injuries in patients who experienced large-dose alkaline ingestion () compared with the findings for acid ingestion.
Impacts on complications
presents the results of multivariate logistic regression analyses focused on complications. Perforation was dose-dependently related to acids (OR = 1.348, per 100 mL) and pH-dependently related to alkalis (OR = 10.71). Bleeding (OR = 1.21) and aspiration injury (OR = 1.22) were related to the acid dose (per 100 mL). Stricture formation was pH-dependently related to both acids (OR = 20.88) and alkalis (OR = 7.09), as well as additional acid doses (OR = 1.27, per 100 mL). Sepsis (OR = 17.58) and DIC (OR = 11.97) were linked to the pH of alkalis. Of note, hepatic (OR = 0.26) and renal injuries (OR = 0.35) were less frequently observed in patients who ingested strong acids, whereas no difference in risk was noted between acid and alkaline substances.
Impacts on overall survival outcomes
The log-rank test and Kaplan–Meier method were performed for univariate survival analyses. The risk of mortality among cases of acid ingestion did not differ between strong and weak substances (p = 0.392, ), whereas the ingestion of ≥100 mL of acids carried significant mortality risks (p = 0.034, ). By contrast, strong alkali ingestion was linked to significantly poorer survival outcomes than weak alkali ingestion (p < 0.001, ). However, the alkaline dose had no effect on survival (p = 0.768, ).
Figure 5. Kaplan–Meier method: long-term survival outcomes were dose-dependent for acids and pH-dependent for alkalis.
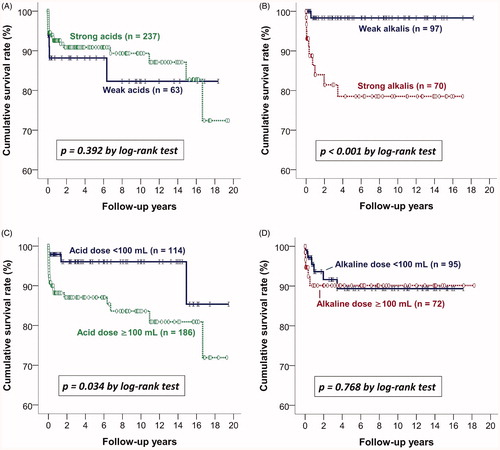
Multivariate Cox proportional hazards models were further used to examine the risk of mortality (). A dose-dependent trend for acid ingestion and a pH-dependent trend for alkaline ingestion were discovered. Every additional 100 mL of acidic substance ingestion was linked to an approximately 1.3-fold higher risk of injury (HR = 1.28, p < 0.001), whereas the pH of acids had no significant effect (p = 0.566). Regarding alkaline ingestion, strong alkalis were associated with a 31.0-fold higher risk of mortality than weak alkalis (HR = 30.99, p = 0.013). The alkali dose did not significantly (p = 0.141) affect survival outcomes.
Table 4. Multivariate Cox proportional hazards models of overall survival in patients with caustic substance ingestion.
Discussion
Based on 468 cases of caustic substance ingestion, we proposed a new perspective for risk assessment for clinical physicians. Combining the pH and dose of caustic substances, our analyses discovered a series of differences between acids and alkalis. Risks of mortality and perforation were dose-dependent for acids and pH-dependent for alkalis. In the alkaline setting, “pH > 12” was linked to severe esophageal and gastric injuries. Of note, we were unable to demonstrate a significant association between dose of alkali and EGD grade or complication rates. Regarding acid ingestion, both “pH < 2” and the “dose itself” significantly predicted severe injuries in the esophagus, stomach, and duodenum.
Behavior-related etiology played an essential role in the relationships between pH and dose. Strong caustics (pH <2 or >12), especially strong alkalis, rapidly damage the alimentary tract surface [Citation18,Citation19,Citation26]. Immediate oral pain limited the dose during ingestion [Citation19]. The doses of weak caustics massively varied by patient. By contrast, patients could only ingest up to 100 and 200 mL of strong alkalis and acids, respectively.
Based on multivariate Cox proportional hazards models, it could be inferred that acids caused mortality at high large doses, whereas alkalis caused mortality at high pH. Although patients rarely ingested >100 mL of strong alkalis, they still carried a 31-fold higher risk of mortality. Regardless of the dose, cases of strong and weak alkaline ingestion were dramatically separated concerning long-term survival. Conversely, the cumulative survival curves were counterintuitive among cases of acid ingestion. The aforementioned behavior-related etiology might help explain such a phenomenon. Patients experienced immediate oral pain, which prevented from further ingestion. Given the dose-dependent risk of acid ingestion, large doses of weak acid also worsened survival.
Focusing on the dose of acids, the stomach appeared to be relatively more resistant to large doses (+1.3-fold/Δ100 mL), followed by the esophagus (+1.4-fold/Δ100 mL) and duodenum (+1.7-fold/Δ100 mL). The functions of the organs [Citation19] precipitated such differences. Serving as a canal, the esophagus was injured by increased contact duration in high-dose ingestion. Stomach, particularly the pylorus and antrum, was destined to collect caustic substances that easily caused serious damage via prolonged contact. This dose-dependent concept could explain the traditional contradiction. Conventional acceptance (which has recently been questioned) indicates that acids preferentially damage the stomach [Citation18]. However, a retrospective cohort study reported a high rate of extensive esophageal damage in patients with high-dose acid ingestion [Citation27]. Both arguments are tenable in different dose settings, namely the former in low-dose settings and the latter in high-dose settings. In addition, the historical phrase describing acid tendency “lick the esophagus and bite the pyloric antrum” [Citation28] fits the setting of “low dose” acid substance ingestion. Likewise, the duodenum appeared more sensitive (+1.7-fold/Δ100 mL) to acids, but it should be interpreted that large-dose acids are required to cause serious duodenal injuries. The pylorospasm and neutralization of duodenal contents played roles in lessening the damage [Citation19].
The pH of acidic caustics was identified as another critical factor predicting the severity of GI tract damage in this study. At the same dose, the duodenum was especially vulnerable to strong acids, followed by stomach and esophagus. In contrast, the esophagus and stomach were more sensitive to strong alkaline substances, compared to the duodenum. The aforementioned behavior-related etiology enormously limited the ingested volume. Taken together, “pH < 2” was most strongly linked to duodenal damage, whereas “pH > 12” threatened the esophagus massively.
Perforation is always considered the most critical complication in clinical situations [Citation1,Citation2,Citation8,Citation9,Citation11,Citation18,Citation24,Citation29]. Cheng et al. [Citation3] emphasized the importance of early EGD classification to identify patients with grade 3b injuries, which predicted perforation. We have further provided physicians with novel insights into hazardous time prior to the availability of examination results. Large doses are dangerous for both weak and strong acids. Meanwhile, a high pH value (or high concentration) is rather noteworthy for alkalis.
Our study was limited by its retrospective nature. Concerning memory lapses or clerical errors during chart recording, information bias might have existed within the ingested dose and actual pH of caustic substances. The chart review process might have led to potentially distorted conclusions. Besides, each excluded case might have caused the selection bias. Nevertheless, the large number of enrolled patients and strict exclusion criteria for uncertain data during full chart review could have minimized the inevitable bias. Additionally, the dose-dependent conclusions of the risk assessment analyses were drawn as the fold risk, with the increasing unit being “Δ100 mL”. pH was categorized as strong (pH < 2 or pH > 12) or weak (pH = 2–12). This strategy was employed to reduce the magnitude of influence originating from incidental information bias. Simultaneously, such scaling for dose estimation and binary pH intervals would also be more practical in clinical situations. Second, the etiology of caustic ingestion exhibits geographic differences. Caustic substances are available to different populations under a variety of commercial formulas. Hence, the statistical analyses focused on pH and dose instead of the types and percentages of chemical substances. A chart review study permits investigation of issues for which randomized trials are difficult to conduct because of ethical reasons [Citation30]. Our study earned its strengths because of the large sample size, the fact that most EGDs were performed by the same endoscopist, the strict inclusion and exclusion criteria, the double-checking process for data extraction, and the long-term follow-up. This new perspective with a retrospective nature requires further validation. Future studies based on worldwide populations are essential to comprehensively understand the association among pH, dose, and caustic injuries.
Conclusions
Combining pH and dose, we proposed a new perspective for the risk assessment of caustic substance ingestion. Risks of mortality and perforation were dose-dependent for acids and pH-dependent for alkalis. The severe EGD findings (grade ≥ 2b) in this study were pH-dependent for both substances and additionally dose-dependent for acids. Such clinical information provides physicians predictive insights prior to the availability of examination results. Large acid doses and high alkaline pH both deserve special attention. Despite being based on a large sample size, this new perspective with a retrospective nature requires further validation.
Author contributions
Study concept and design by Yu-Jhou Chen, Chen-June Seak, Shih-Ching Kang, and Hao-Tsai Cheng. Acquisition of data by all authors. Analysis and interpretation of data by all authors. Drafting the manuscript by Yu-Jhou Chen, Chen-June Seak, and Hao-Tsai Cheng. Critical revision of the manuscript for important intellectual content by all authors. Study supervision by Tsung-Hsing Chen, Chien-Cheng Chen, Chip-Jin Ng, Chao-Wei Lee, Ming-Yao Su, Hsin-Chih Huang, Pin-Cheng Chen, Chun-Hsiang Ooyang, Sen-Yung Hsieh, and Hao-Tsai Cheng.
Ethical approval
Our research protocol had been approved by Chang Gung Medical Foundation Institutional Review Board (IRB number: 202000583B0; executing institution: Linkou Chang Gung Memorial Hospital, Taoyuan, Taiwan). The IRB reviewed and determined that it is expedited review according to personal information, data, documents, or specimens collected from legal biological databases without hyperlink or identifiable information can be used for research, but cannot be involved in the interests of individuals or groups. On the basis of aforementioned statements, the IRB approves the waiver of the participants’ consent in the present study.
Acknowledgments
Thanks for all the colleagues from the Department of Gastroenterology and Hepatology, Department of Psychiatry, Department of Emergency Medicine, Department of Medical Image and Intervention, Division of Trauma and Emergent Surgery, and Division of General Surgery of Linkou Chang Gung Memorial Hospital to help us caring the patients.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Hoffman R, Burns M, Gosselin S. Ingestion of caustic substances. N Engl J Med. 2020;382(18):1739–1748.
- Hall AH, Jacquemin D, Henny D, et al. Corrosive substances ingestion: a review. Crit Rev Toxicol. 2019;49(8):637–669.
- Cheng H-T, Cheng C-L, Lin C-H, et al. Caustic ingestion in adults: the role of endoscopic classification in predicting outcome. BMC Gastroenterol. 2008;8(1):31.
- Chen C-M, Chung Y-C, Tsai L-H, et al. A nationwide population-based study of corrosive ingestion in Taiwan: incidence, gender differences, and mortality. Gastroent Res Pract. 2016;2016:1–7.
- Johnson CM, Brigger MT. The public health impact of pediatric caustic ingestion injuries. Arch Otolaryngol Head Neck Surg. 2012;138(12):1111–1115.
- Gumaste VV, Dave PB. Ingestion of corrosive substances by adults. Am J Gastroenterol. 1992;87(1):1–5.
- Ramasamy K, Gumaste VV. Corrosive ingestion in adults. J Clin Gastroenterol. 2003;37(2):119–124.
- Chirica M, Bonavina L, Kelly MD, et al. Caustic ingestion. Lancet. 2017;389(10083):2041–2052.
- Arunachalam R, Rammohan A. Corrosive injury of the upper gastrointestinal tract: a review. Arch Clin Gastroenterol. 2016;2(2):56–62.
- Gupta SK, Croffie JM, Fitzgerald JF. Is esophagogastroduodenoscopy necessary in all caustic ingestions? J Pediatr Gastroenterol Nutr. 2001;32(1):50–53.
- Hugh TB, Kelly MD. Corrosive ingestion and the surgeon. J Am Coll Surg. 1999;189(5):508–522.
- Hoffman RS, Howland MA, Kamerow HN, et al. Comparison of titratable acid/alkaline reserve and pH in potentially caustic household products. J Toxicol Clin Toxicol. 1989;27(4-5):241–261.
- Vancura EM, Clinton JE, Ruiz E, et al. Toxicity of alkaline solutions. Ann Emerg Med. 1980;9(3):118–122.
- Newman M, Newman D, Ritter F. A clinical and experimental study of corrosive burns of the stomach. Ann Otol Rhinol Laryngol. 1968;77(5):830–842.
- Krey H. On the treatment of corrosive lesions in the oesophagus: an experimental study. Acta Otolaryngol Suppl. 1952;102:1–49.
- Leape LL, Ashcraft KW, Scarpelli DG, et al. Hazard to health-liquid lye. N Engl J Med. 1971;284(11):578–581.
- Ashcraft KW, Padula RT. The effect of dilute corrosives on the esophagus. Pediatrics. 1974;53(2):226–232.
- Contini S, Scarpignato C. Caustic injury of the upper gastrointestinal tract: a comprehensive review. World J Gastroenterol. 2013;19(25):3918–3930.
- Wax PM, Yarema M. Corrosives. In: Shannon MW, Borron SW, Burns MJ, editors. Haddad and Winchester’s clinical management of poisoning and drug overdose. 4th ed. Philadelphia (PA): Saunders/Elsevier; 2007. p. 1407–1414.
- Le P-H, Seak C-J, Chiu C-T, et al. The role of second-look endoscopy in severe esophageal caustic injury. J Gastrointest Dig Syst. 2017;7(518):2.
- Chang J-M, Liu N-J, Pai BC-J, et al. The role of age in predicting the outcome of caustic ingestion in adults: a retrospective analysis. BMC Gastroenterol. 2011;11(1):72.
- Struck MF, Beilicke A, Hoffmeister A, et al. Acute emergency care and airway management of caustic ingestion in adults: single center observational study. Scand J Trauma Resusc Emerg Med. 2016;24(1):45.
- Keh SM, Onyekwelu N, McManus K, et al. Corrosive injury to upper gastrointestinal tract: still a major surgical dilemma. World J Gastroenterol. 2006;12(32):5223.
- Elkaramany M. An overview of corrosive injury of the upper gastrointestinal tract: Discussion of types, clinical evaluation, and management procedures. Adv Dig Med. 2018;5(4):115–120.
- Zargar SA, Kochhar R, Mehta S, et al. The role of fiberoptic endoscopy in the management of corrosive ingestion and modified endoscopic classification of burns. Gastrointest Endosc. 1991;37(2):165–169.
- Kirsh MM, Ritter F. Caustic ingestion and subsequent damage to the oropharyngeal and digestive passages. Ann Thorac Surg. 1976;21(1):74–82.
- Arévalo‐Silva C, Eliashar R, Wohlgelernter J, et al. Ingestion of caustic substances: a 15-year experience. Laryngoscope. 2006;116(8):1422–1426.
- Marks I, Bank S, Werbeloff L, et al. The natural history of corrosive gastritis. Digest Dis Sci. 1963;8(6):509–524.
- Bonavina L, Chirica M, Skrobic O, et al. Foregut caustic injuries: results of the world society of emergency surgery consensus conference. World J Emerg Surg. 2015;10(1):44.
- Kaji AH, Schriger D, Green S. Looking through the retrospectoscope: reducing bias in emergency medicine chart review studies. Ann Emerg Med. 2014; 64(3):292–298.