Abstract
Introduction
The use of new psychoactive substances (NPSs) has markedly increased worldwide; thus, it is important to monitor NPS-related effects. The Taiwan Emergency Department Drug Abuse Surveillance (TEDAS) project aims to assess the patterns of recreational drug use in patients presenting to emergency departments (EDs) across the country. Here, we report the preliminary results of this project.
Methods
This observational study included the collection and analysis of urine samples and assessment of the clinical presentation of patients from 79 EDs across Taiwan. Clinical features were recorded through a questionnaire filled by attending doctors or nurses who collected urine samples for clinical diagnosis. Urine samples were analyzed for 110 drugs and metabolites using electrospray ionization liquid chromatography-tandem mass spectrometry (LC-MS/MS).
Results
Between February and November 2019, a total of 2649 patients were enrolled for urine drug analysis. A total of 675 cases older than 12 years (males, n = 480) had NPS or other illicit drugs detected in their urine samples. Overall, 1271 counts of drugs, among which 717 (56.4%) were NPS. At least one NPS was detected in 340 patients (50.4%), and 292 cases were positive for multiple drugs. The most frequently detected drug was methamphetamine/amphetamine, followed by synthetic cathinones, ketamine and its two analogs, and opioids. The most common drug combination was cathinones plus ketamine and/or its analogs (n = 56). Younger patients (OR = 3.3, p≤.0001) and women (OR = 1.5, p = .01) were more likely to have NPS detected in their urine samples. NPS-positive cases frequently experienced chest pain (OR = 2.6, p = .03), tachycardia (OR = 2.6, p = .0002), and suicide attempt/non-suicidal self-harm (OR = 1.8, p = .004), whereas depressed consciousness (OR = 0.5, p = .001) was less frequent among NPS-positive cases than among other illicit drug-positive cases.
Conclusions
The TEDAS project provides a nationwide epidemiological profile of recreational drug use in Taiwan. More than half of the recreational drugs were NPSs, which were comprehensively detected using LC-MS/MS.
Introduction
The United Nations Office on Drugs and Crime documented more than 1000 new psychoactive substances (NPSs) by the end of 2020 [Citation1]. NPS abuse, reported globally in 117 countries and territories, has rapidly emerged as a public health problem in recent decades [Citation2]. The increasing availability of NPS primarily through internet-based trade (“Internet drugs”) has led to a significant global drug problem and health concern [Citation3]. Difficulties in the analytical detection of NPSs further complicate the control of NPS use due to rapidly evolving structural diversity, unavailability of reference standards [Citation4], and absence of detection with routine immunoassay drug screenings [Citation5–7]. This could lead to a lack of knowledge concerning clinical presentations or toxicity of NPS drugs. Severe poisoning cases have been reported for several NPSs [Citation8–10]. Unexpected and undesired clinical symptoms and potential severe harm associated with NPS use resulted in a significant burden on emergency departments (EDs) [Citation11].
Data reported by EDs on emerging NPS-related adverse events may play essential roles in tackling this public health threat. The European Drug Emergencies Network (Euro-DEN) was established in 2013 to collect data across a broad group of European countries for acute toxicity due to NPS use in ED patients [Citation11]. In Sweden, the STRIDA project is a nationwide study that involved collecting and evaluating clinical effects of NPS use in intoxicated patients admitted to EDs or intensive care units (ICUs) from 2011 to 2016 [3]. The Psychoactive Surveillance Consortium and Analysis Network (PSCAN) in the USA has gathered clinical data and substance identification data from NPS users who visited EDs since 2016 [12]. These projects can help in identifying patients who use illicit substances and clarifying the definition of toxidromes associated with NPS by collecting clinical data based on analytical results using biological samples. Most epidemiological studies that examined the effect of these drugs focus on user reports or lack comprehensive analysis, which may underestimate the intensity of the epidemic owing to under-reporting of drug adulteration and drug substitution [Citation4,Citation12,Citation13].
NPS use has gradually become popular since the early 2000s in Taiwan [Citation14]. Although the lifetime prevalence (approximately 1.4%) of drug use by a self-reported survey in 2014 in Taiwan was similar to the prevalence in 2005, the use of “club drugs” (mainly NPS) increased dramatically [Citation15]. Weng et al. confirmed NPS-using patients at two EDs from 2017 to 2018 using liquid chromatography-tandem mass spectrometry (LC-MS/MS) [Citation16]. However, there was no nationwide collection of NPS-related data, including epidemiology, acute drug/NPS toxicity, or hospital presentation, in Taiwan. The Taiwan Emergency Department Drug Abuse Surveillance (TEDAS) project was established in 2019. This project aimed to conduct nationwide surveillance of recreational drug-using patients who presented to EDs. Urine samples were subjected to electrospray ionization liquid chromatography-tandem mass spectrometry (LC-MS/MS) analysis and then used to determine clinical effects associated with NPS use. We have been executing the TEDAS project since 2019 and are currently conducting the fourth-year project. We hope to extend the TEDAS project to 2023 and beyond so that it can help the long-term surveillance of ED recreational drug use in Taiwan. This study aimed to present the preliminary results of the TEDAS project.
Methods
Development of the TEDAS project
The TEDAS project was established to monitor acute toxicity owing to the recreational use of drugs in EDs in Taiwan since 2019. After acquiring oral consent from patients or their family members, emergency physicians ordered a pre-specified urine toxicological screening (including 110 compounds listed in the Supplementary table). Patients aged below 12 years were not included in this study. Patients were enrolled if they self-reported recreational drug use, or manifested clinical presentations consistent with acute toxicity of recreational drug abuse such as unexplained consciousness change, acute delirium/hallucination, violent behavior, suicide attempt/non-suicidal self-harm, or other symptomatology that fulfilled the inclusion criteria. All urine samples were collected and de-identified at participating EDs and refrigerated without additives until they were sent to one of the two TEDAS laboratories for analysis. Clinical and laboratory data were anonymized and only linked to the case by the staff who performed the de-identification during urine sample collection. Urine samples were submitted in a particular form that enabled the recording of patient’s clinical characteristics, and the analysis was free of charge. The study was approved by the Ethics Committee of Chang Gung Memorial Hospital (approval no: 202000500B0, date of approval: 2020/03/31).
Analytical investigations
Urine samples were collected and sent to either of the two toxicological laboratories, National Taiwan University Hospital and Taipei Veterans General Hospital, for toxicological analysis. Analysis was performed using LC-MS/MS in multiple reaction monitoring mode. At least two ion transitions were monitored for each analyte. Chromatographic separation of all substances was achieved using a Phenomenex Kinetex Biphenyl column (Phenomenex, Torrance, CA) and gradient elution. For urinary analysis, samples were diluted 10 fold, with an internal standard solution containing methamphetamine-d11 50 ng/mL, amphetamine-d11 50 ng/mL, and 7-aminoflunitrazepam-d7 in 50% methanol/water with 0.5% formic acid. Quantitative detection of 110 compounds (details of the 110 substances are listed in Supplementary Table 1) was performed on all samples. We selected 110 compounds based on the following considerations: data from customs seizures, criminal charges, and forensic autopsies were collected to understand the drug market in Taiwan. We also selected compounds that have not been found in Taiwan but have been reported in neighboring countries. Quality of the analysis of both laboratories was confirmed by cross-validation of three positive blinded samples each month during the study period.
Table 1. Clinical features of 675 cases with positive LC-MS/MS results in their urine samples.
Clinical characteristics of the cases
All data from special forms were collected by emergency physicians or nurses who were in charge of these patients. A letter of general instructions was e-mailed from the research team to the directors of the joined EDs. On-site training regarding protocol implementation by the research team was provided to EDs before recruitment. The special forms sent with urine samples had the following information regarding clinical characteristics of the patients: age, sex, chief complaints, initial vital signs at the ED triage, self-report of drug/alcohol use, physical examinations, drug treatments provided by the emergency physicians, and case disposition. Any drugs detected in the urine samples that were confirmed to be administered by emergency physicians were excluded from the final analysis.
Data analysis
Categorical variables are expressed as absolute values and percentages, whereas continuous variables are presented as median and ranges. We used the Mann–Whitney U test to compare age between male and female patients. We divided patients into two groups: NPS group and other illicit drug group. The NPS group included cases in which urine samples had traces of NPS. The remaining cases were included in the other illicit drug group. Comparisons of data between groups were performed using univariable and multivariable logistic regression (LR). Variables with p values ≤.2 in the univariable analysis were included in the multivariable LR, and we conducted forward selection to select variables for LR models. Statistical Package for the Social Sciences Statistics 25 (IBM Corp., Armonk, NY) was used for analysis, and p values <.05 were considered statistically significant.
Participants
EDs from 97 hospitals joined the TEDAS project and 79 EDs were recruited during the study period (February 2019–November 2019). The recruiting-case EDs had 3,521,335 visits, accounting for 56.63% of all 6,217,892 ED visits in Taiwan during the study period. The locations of the ED recruiting cases are shown in the Supplementary figure.
Results
Demographics of cases with positive drug detection
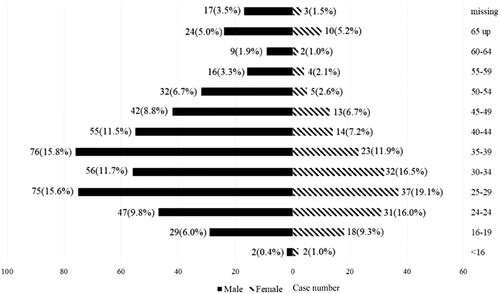
A total of 2649 cases (0.075% of recruiting-case ED visits) were enrolled in this study, and at least one drug was detected in the urine samples from 676 patients. After excluding one case of potential child abuse, 675 cases were further analyzed. Among the 675 cases with positive LC-MS/MS results (positive cases), the majority were men (n = 480, 71.1%). The median ages for men and women were 36.0 (27.0, 45.0) years and 30.0 (24.0, 40.0) years, respectively. Women were significantly younger than men (p = .03). As shown in , most cases were young adults (262 men and 106 women, aged 25–44 years).
Substances detected in urine samples
Among the tested 110 drugs, 44 were detected (35 NPS and 9 other illicit drugs) in urine samples. A total of 1271 counts of drugs (717 counts of NPS, 56.4% of total detected counts) were detected in urine samples from 675 positive cases. In 340 cases (50.4%), at least one NPS was detected in urine samples. shows the “top 20” most commonly detected drugs. The most frequently detected drugs were methamphetamine/amphetamine (n = 308, 24.2%), followed by 23 synthetic cathinones (n = 440, 34.6%), ketamine and its two analogs (deschloroketamine and deschloro-N-ethyl-ketamine) (n = 232, 18.3%), and opioids (heroin/codeine/morphine, n = 177, 13.9%). The most frequently detected cathinone among the 23 synthetic cathinones was mephedrone (n = 113, 8.9%), followed by ephylone (n = 69, 5.4%), eutylone (n = 52, 4.1%), and dibutylone (n = 47, 3.7%). A total of 383 (56.7%) and 292 (43.3%) urine samples were detected to have single and multiple agents (2–10 agents), respectively. There were 152 (22.5%), 58 (8.6%), 43 (6.4%), 18 (2.7%), and 12 (1.8%) cases involved two, three, four, five, and six agents, respectively.
Figure 2. The Top 20 most commonly detected drugs. MDA: 3, 4-Methylenedioxyamphetamine; MDMA: 3,4-Methylenedioxymethamphetamine; 4-MEAPP: 4-Methyl-α-ethylaminopentiophenone; 4-Chloro-N-N-DMC: 4-chloro-N,N-dimethylcathinone; 5-MeO-MIPT: N-(2-(5-methoxy-1H-indol-3-yl)ethyl)-N-methylpropan-2-amine. The other less reported drugs (detected counts) were as following: Cathinones: 3, 4-Methylenedioxy-α-Pyrrolidinohexanophenone (7), N,N-Dimethylamphetamine (6), Pentylone (4), 4-Ethylmethylcathinone (3), Methedrone (3), Methylpentedrone (3), Benzedrone (2), 4-Bromoethcathinone (1), 3,4-Methylenedioxy-α-pyrrolidinobutyrophenone (1), Methylethcathinone (1), 4-Chloro-α-pyrrolidinovalerophenone (1), α-Ethylaminohexanophenone (1). Ketamine and ketamine analogs: Deschloro-N-ethyl-ketamine (1). Others: 11-nor-9-Carboxy-Δ9-THC (4), Phenazepam (3), 1-(benzo[d][1, 3]dioxol-5-yl)-N, N-dimethylpropan-2-amine (2), 2-(4-bromo-2, 5-dimethoxyphenyl)-N-(2-methoxybenzyl) ethan-1-amine (2), AB-PINACA (1), Etizolam (1), Cocaine (1).
![Figure 2. The Top 20 most commonly detected drugs. MDA: 3, 4-Methylenedioxyamphetamine; MDMA: 3,4-Methylenedioxymethamphetamine; 4-MEAPP: 4-Methyl-α-ethylaminopentiophenone; 4-Chloro-N-N-DMC: 4-chloro-N,N-dimethylcathinone; 5-MeO-MIPT: N-(2-(5-methoxy-1H-indol-3-yl)ethyl)-N-methylpropan-2-amine. The other less reported drugs (detected counts) were as following: Cathinones: 3, 4-Methylenedioxy-α-Pyrrolidinohexanophenone (7), N,N-Dimethylamphetamine (6), Pentylone (4), 4-Ethylmethylcathinone (3), Methedrone (3), Methylpentedrone (3), Benzedrone (2), 4-Bromoethcathinone (1), 3,4-Methylenedioxy-α-pyrrolidinobutyrophenone (1), Methylethcathinone (1), 4-Chloro-α-pyrrolidinovalerophenone (1), α-Ethylaminohexanophenone (1). Ketamine and ketamine analogs: Deschloro-N-ethyl-ketamine (1). Others: 11-nor-9-Carboxy-Δ9-THC (4), Phenazepam (3), 1-(benzo[d][1, 3]dioxol-5-yl)-N, N-dimethylpropan-2-amine (2), 2-(4-bromo-2, 5-dimethoxyphenyl)-N-(2-methoxybenzyl) ethan-1-amine (2), AB-PINACA (1), Etizolam (1), Cocaine (1).](/cms/asset/3de8b256-6f2a-4350-9145-fe3ce4fa1e85/ictx_a_2038793_f0002_b.jpg)
Clinical features of positive cases
The clinical features of positive cases are summarized in . Most positive cases had tachycardia and tachypnea. Only 10% of patients had high body temperature (≥38 °C) and 26% had high systolic blood pressure (SBP ≥140 mmHg). More than half of the positive cases expressed cardiac complaints and 46% had neurological/psychiatric symptoms. The most frequent clinical presentations of neurological/psychiatric symptoms were depressed consciousness disturbance, delirium, agitation, hallucinations, and bizarre behavior. Approximately 17% of cases had violent behavior and 14% exhibited self-injury. Approximately 30% of cases exhibited sweating or flushing. Regarding drug history, 32% (n = 213) of positive cases reported illicit drug use while 11% self-reported non-illicit drug use. Nearly 7% of positive cases reported concurrent use of alcohol. The 213 cases with self-reports of using illicit drugs were found to have at least one illicit drug in their urine samples. We present the relationship between the drug of self-report and the drug detected by LC-MS/MS in . After excluding self-reports of marijuana, the agreement percentages of the self-reported drug and drug detected in the urine sample ranged from 57% to 83% (ketamine: 57%, opioid: 77%, amphetamine: 82%, and cathinone: 83%). However, drugs other than self-reported drugs were also frequently detected in the self-reporting patients’ urine samples.
Table 2. Common (more than 10 cases) drug combination patterns of different classes of drugs in 292 urine samples.
Treatments of positive cases
Among the 675 positive cases, 234 (34.7%) received at least one specific treatment regimen. Among them, 116 patients (17.2%) received sedation with benzodiazepines, 15 (2.2%) received haloperidol, and 64 (9.5%) received benzodiazepines and haloperidol simultaneously. Other treatment modalities included administration of naloxone (n = 16, 2.4%), flumazenil (n = 10, 1.5%), morphine (n = 8, 1.2%), activated charcoal (n = 4, 0.6%), and ketamine (n = 3, 0.4%).
Outcomes of positive cases
Five patients died, including four patients with out-of-hospital cardiac arrest and one patient who died in the ED. After a short observation period (<4 h), 153 patients (22.7%) were discharged from EDs. Furthermore, 285 (42.2%) patients remained in EDs for observation for <1 d, 109 (16.1%) were admitted to general wards, and 91 (13.5%) were admitted to ICUs.
Patterns of drug combinations
After adjusting for age and sex with multivariable LR, NPS group had an adjusted odds ratio (aOR) of 17.2 (95% confidence interval [CI]: 11.4–26.1, p<.0001) compared with other illicit drug group regarding the detection of multiple drugs. Common combinations (case number >10) of different drugs are shown in . The most common combination was cathinones with ketamine and/or its analogs (n = 56). Forty-five cases involved the combination of methamphetamine and opioids, and 44 cases involved the combination of different cathinones. Other common patterns involved combinations of cathinones, ketamine and/or its analogs, methamphetamine, and MDMA.
Comparison between NPS group and other illicit drugs group
We analyzed the demographic and clinical features of NPS group and other illicit drug group using LR. Univariable LR analysis () showed that NPS group were younger (aged ≤39 years) with an OR of 3.3 (95% CI: 2.4–4.7, p<.0001) and with more females (OR: 1.5, 95% CI: 1.1–2.1, p<.01) than other illicit drug group. The clinical features with univariable LR significance were tachycardia (>135 bpm), Glasgow Coma Scale score ≤8, low oxygen saturation (≤94%), chest pain, bizarre behavior/delirium/agitation, and instances of suicide/self-injury. There were no differences in ethanol use or drug histories (self-reported illicit/non-illicit drug use or drug used suspected by others) between the two groups. Both NPS and other illicit drug groups had similar outcomes (death or admission to ICUs). Multivariable LR with adjustment for age and sex was performed. NPS group presented with greater occurrence of chest pain (aOR: 3.0, 95% CI: 1.2–7.5, p = .02), tachycardia (aOR: 2.5, 95% CI: 1.5–4.2, p = .001), and suicide attempt/self-injury (aOR: 1.7, 95% CI: 1.1–2.7, p = .02) and fewer instances of depressed consciousness (aOR: 0.6, 95% CI: 0.4–0.9, p = .01) than other illicit drug group.
Table 3. Results of univariable logistic regression comparing the NPS group and other illicit drug group.
Discussion
The TEDAS project is the first nationwide ED-based surveillance program investigating recreational drug use in Taiwan. Based on the analysis of urine samples using LC-MS/MS, the TEDAS project provides an insight into epidemiological and clinical characteristics of illicit drug use, including NPS and traditional illicit drugs. Our results showed that at least one NPS was detected in 50.4% of positive cases and 43% of positive cases’ urine samples were found to have more than one substance. Cathinones were the most common NPS detected in positive cases. The TEDAS project provided epidemiological information and clinical features of recreational drug users in EDs.
We detected at least one type of NPS in more than half of the positive cases’ urine samples, which is a remarkable frequency for NPS detection. Based on self-reported data, the New York City Poison Center reported that the prevalence of NPS exposure increased from 7.1% in 2011 to 12.6% in 2014 [Citation17]. Self-reported NPS use accounted for 23.7% of cases presented with recreational drug toxicity in a London ED in 2015–2017 [Citation18]. The Euro-DEN, which collects data across a wide group of European countries, revealed that NPS use accounted for 9% of all acute emergency admissions involving illicit drug use. Euro-DEN data were mostly self-reported; however, bio-samples were analyzed using LC-MS/MS in approximately 20% of cases [Citation19]. The prevalence of NPS use obtained by self-reporting without comprehensive toxicological analysis would lead to underestimation of the real prevalence, as patients may not be aware of the exact chemicals they used. The national surveys of the STRIDA project in Sweden [Citation3] and the PSCAN project in the USA [Citation12] included patients with suspected intoxication caused by NPS use presenting at EDs or ICUs. NPS use was identified based on patients’ bio-sample analysis using LC-MS/MS or liquid chromatography-high resolution mass spectrometry. Neither study can reveal the prevalence of NPS use because of the lack of analysis of bio-samples from patients who self-reported using traditional illicit drugs. The TEDAS project performed a comprehensive analysis of ED patients suspected of using illicit drugs and provided another perspective of the drug abuse surveillance system.
Synthetic cathinones were the most common NPSs found in this study. The use of synthetic cathinones is a severe problem worldwide [Citation20]. Cathinones have become popular because of the lack of legislation and their lower cost in many countries [Citation21]. People can buy different mixtures of cathinones through the internet or retail outlets [Citation22]. Synthetic cathinones were the NPS most seized in 2016 in the EU [Citation23]. In Northeast Asia, the most commonly controlled NPSs are synthetic cannabinoids, synthetic cathinones, and phenethylamines [Citation24]. Cathinones are also popular in the USA [Citation12].
Our results showed that multiple drugs were detected in 43% of positive cases’ urine samples. We found that detection of NPS in urine samples was correlated with the detection of multiple drugs. The Swedish STRIDA project (including cases suspected to be exposed to NPS) revealed that approximately half of the cases were determined with multiple drug intoxication [Citation3]. The prevalence of drug abuse found in Hong Kong from 2011 to 2015 indicated that NPS cases contributed to <5% of all drug seizure cases examined, and only approximately 20% of cases used multiple drugs [Citation25]. In Taiwan, people commonly consume cathinones by drinking a beverage made of “instant coffee packet,” containing a mixture of different cathinones, ketamine and/or its analogs, or other illicit substances. Therefore, multiple substances are usually detected in urine samples [Citation26–28]. As ketamine users sometimes also take “instant coffee packet” [Citation29], the combined use of cathinones and ketamine and/or its analogs was commonly observed in our results. Our results also showed a common combination of opioids and methamphetamine. The combined use of methamphetamine and opioids is quite common [Citation30]. The increase in methamphetamine use among chronic opioid users is probably because of a synergistic high and balanced out the side effects of opioids [Citation31].
The clinical features associated with NPS group and other illicit drug group were different in this study. Younger patients and women were more likely to have NPS detected in their urine samples. Fattore et al. revealed that men were more likely than women to use all types of drugs; in addition, women may be more susceptible to drug toxicity, especially NPS [Citation32]. Exposure to methylone or cathinone was found to induce higher anxiety-related behavior in female rats than in male rats [Citation33,Citation34]. Females are more susceptible than males to ketamine withdrawal symptoms and adverse effects, such as anxiety, dysphoria, and tremors [Citation4]. We propose that female NPS users may visit the ED more frequently due to the adverse effects from NPS use. Patients in NPS group presented with more instances of tachycardia, chest pain, and suicide attempt/self-injury than patients in other illicit drug group. Since “NPS” refers to a mixture of drug classes with different clinical effects owing to variable receptor interactions and varying potencies at these receptors, further investigations are required to explore the clinical features of each NPS drug class.
Limitations
This case series study had some limitations. The recruiting-case EDs accounted for 56.63% of all ED visits in Taiwan during the study period. The number of recruited patients in 79 EDs was 2,649; therefore, we estimated that about 2000 eligible patients were not recruited from non-participating EDs in Taiwan during the study period. The toxicology testing was performed at the discretion of the emergency attending physician. Illicit substance-exposed patients without overt symptoms may not have been included in our analysis. Some eligible patients, even those with overt symptoms, may not have been recruited for any reason (busy shifts, self-discharge, refusal to consent, etc.). In this study, we report a low mortality rate. Patients who died at the scene may have not been transported to a hospital, and we only determined patients who were dead in EDs. Moreover, because of the de-identification of urine samples, we could not follow the outcome of patients after admission. Based on the aforementioned reasons, the mortality rate reported herein may be underestimated. Because over 1000 NPSs have been identified in the illegal drug market, drugs other than these 110 items would be missed during screening.
Conclusions
The nationwide TEDAS project provided an epidemiological profile of recreational drug use in Taiwan. More than half of the recreational drugs in this project were NPS, which were comprehensively detected using LC-MS/MS.
Geolocation information
Taiwan Society of Emergency Medicine, Taipei, Taiwan. 25.046621°N, 121.515596°E.
Supplemental Material
Download MS Word (57.5 KB)Supplemental Material
Download MS Word (81 KB)Acknowledgments
The authors thank the Taiwan Society of Emergency Medicine for assistance with the TEDAS project.
Disclosure statement
The authors report there are no competing interests to declare. Chih-Chuan Lin and Te-I Weng: Conceptualization; formal analysis; investigation; methodology; visualization and writing–original draft. Chip-Jin Ng: funding acquisition and investigation. Chia-Pang Shih: Methodology and data curation. Jui Hsu and Yuan-Chun Lia: data curation, funding acquisition, investigation and project administration, supervision. Chen-Chang Yang and Cheng-Chung Fang: Conceptualization, data curation, funding acquisition, investigation, methodology, project administration, supervision, validation, and approval of the final manuscript as submitted.
Additional information
Funding
References
- UNODC. What are NPS? 2020. [cited 2021/8/2]. Available from: https://www.unodc.org/LSS/Page/NPS
- EMCDDA U. June 2019 – EMCDDA. European Drug Report describes a complex NPS market. [cited 2020 22 June]. Available from: https://www.unodc.org/LSS/Announcement/Details/af9c6b26-5715-4043-86e6-f6d7a2acad50
- Helander A, Backberg M, Hulten P, et al. Detection of new psychoactive substance use among emergency room patients: results from the Swedish STRIDA project. Forensic Sci Int. 2014;243:23–29.
- Brandehoff N, Adams A, McDaniel K, et al. Synthetic cannabinoid “black mamba” infidelity in patients presenting for emergency stabilization in Colorado: a P SCAN cohort. Clin Toxicol (Phila). 2018;56(3):193–198.
- Begeman A, Franssen EJF. Lack of detection of new Amphetamine-Like drugs using conventional urinary immunoassays. Ther Drug Monit. 2018;40(1):135–139.
- Pettersson Bergstrand M, Helander A, Hansson T, et al. Detectability of designer benzodiazepines in CEDIA, EMIT II plus, HEIA, and KIMS II immunochemical screening assays. Drug Test Anal. 2017;9(4):640–645.
- Regester LE, Chmiel JD, Holler JM, et al. Determination of designer drug cross-reactivity on five commercial immunoassay screening kits. J Anal Toxicol. 2015;39(2):144–151.
- Logan BK, Mohr ALA, Friscia M, et al. Reports of adverse events associated with use of novel psychoactive substances, 2013–2016: a review. J Anal Toxicol. 2017;141(7):573–610.
- Kraemer M, Boehmer A, Madea B, et al. Death cases involving certain new psychoactive substances: a review of the literature. Forensic Sci Int. 2019;298:186–267.
- Kronstrand R, Guerrieri D, Vikingsson S, et al. Fatal poisonings associated with new psychoactive substances. Handb Exp Pharmacol. 2018;252:495–541.
- Wood DM, Heyerdahl F, Yates CB, et al. The european drug emergencies network (Euro-DEN). Clin Toxicol (Phila). 2014;52(4):239–241.
- Monte AA, Hopkinson A, Saben J, et al. The psychoactive surveillance consortium and analysis network (PSCAN): the first year. Addiction. 2020;115(2):270–278.
- Vallersnes OM, Persett PS, Oiestad EL, et al. Underestimated impact of novel psychoactive substances: laboratory confirmation of recreational drug toxicity in Oslo, Norway. Clin Toxicol (Phila). 2017;55(7):636–644.
- Feng LY, Li JH. New psychoactive substances in Taiwan: challenges and strategies. Curr Opin Psychiatry. 2020;33(4):306–311.
- Chen WJ, Wu SC, Tsay WI, et al. Differences in prevalence, socio-behavioral correlates, and psychosocial distress between club drug and hard drug use in Taiwan: results from the 2014 national survey of substance use. Int J Drug Policy. 2017;48:99–107.
- Weng TI, Chen LY, Chen JY, et al. Characteristics of analytically confirmed illicit substance-using patients in the emergency department. J Formos Med Assoc. 2020;119(12):1827–1834.
- Palamar JJ, Su MK, Hoffman RS. Characteristics of novel psychoactive substance exposures reported to New York city poison center, 2011–2014. Am J Drug Alcohol Abuse. 2016;42(1):39–47.
- Webb NE, Wood DM, Greene SL, et al. Change in the new psychoactive substances associated with emergency department acute toxicity presentations associated with the introduction of the UK 2016 psychoactive substances act. Clin Toxicol (Phila). 2019;57(1):36–41.
- Euro-DEN. Final report of the European drug emergencies network (Euro-DEN) March 2015 [cited 2021 June 10]. Available from: https://www.emcdda.europa.eu/system/files/attachments/12440/Euro_DEN-final-report-2015.pdf
- Weinstein AM, Rosca P, Fattore L, et al. Synthetic cathinone and cannabinoid designer drugs pose a major risk for public health. Front Psychiatry. 2017;8:156–156.
- Valente MJ, Guedes de Pinho P, de Lourdes Bastos M, et al. Khat and synthetic cathinones: a review. Arch Toxicol. 2014;188(1):15–45.
- Simmons SJ, Leyrer-Jackson JM, Oliver CF, et al. DARK classics in chemical neuroscience: cathinone-derived psychostimulants. ACS Chem Neurosci. 2018;9(10):2379–2394.
- Schifano F, Napoletano F, Arillotta D, et al. The clinical challenges of synthetic cathinones. Br J Clin Pharmacol. 2020;86(3):410–419.
- Lee J, Yang S, Kang Y, et al. Prevalence of new psychoactive substances in northeast asia from 2007 to 2015. Forensic Sci Int. 2017;272:1–9.
- Cheng WC, Dao KL. Prevalence of drugs of abuse found in testing of illicit drug seizures and urinalysis of selected population in Hong Kong. Forensic Sci Int. 2019;299:6–16.
- Chen HY, Chien WC, Huang MN, et al. Analytically confirmed eutylone (bk-EBDB) exposure in emergency department patients. Clin Toxicol (Phila). 2021;59(9):846–848.
- Ling DA, Weng TI, Chen JY, et al. Clinical manifestation and quantitative urinary analysis of N-ethylnorpentylone abuse in patients to the emergency department. Clin Toxicol (Phila). 2020;58(9):935–937.
- Weng TI, Su PI, Chen JY, et al. Analytically confirmed 4-Methyl-N-ethylnorpentedrone (4-MEAP), a synthetic cathinone, in cases presenting to an emergency department. Clin Toxicol (Phila). 2020;58(1):65–66.
- Weng TI, Chin LW, Chen LY, et al. Clinical characteristics of patients admitted to emergency department for the use of ketamine analogues with or without other new psychoactive substances. Clin Toxicol (Phila). 2021;59(6):528–531.
- Chawarski MC, Hawk K, Edelman EJ, et al. Use of Amphetamine-Type stimulants among emergency department patients with untreated opioid use disorder. Ann Emerg Med. 2020;76(6):782–787.
- Ellis MS, Kasper ZA, Cicero TJ. Twin epidemics: the surging rise of methamphetamine use in chronic opioid users. Drug Alcohol Depend. 2018;93:14–20.
- Fattore L, Marti M, Mostallino R, et al. Sex and gender differences in the effects of novel psychoactive substances. Brain Sci. 2020;10(9):606.
- Daniel JJ, Hughes RN. Increased anxiety and impaired spatial memory in young adult rats following adolescent exposure to methylone. Pharmacol Biochem Behav. 2016;146–147:44–49.
- Alsufyani HA, Docherty JR. Gender differences in the effects of cathinone and the interaction with caffeine on temperature and locomotor activity in the rat. Eur J Pharmacol. 2017;809:203–208.