Abstract
Background
Public health emergencies often affect Poison Control Centre (PCC) operations. We examined possible effects of the coronavirus disease 2019 (COVID-19) pandemic on call volume, call characteristics, and workload in European PCCs.
Method
All 65 individual European PCCs were requested to supply data on the number of calls and call characteristics (caller, age groups, reason and specific exposures) from March to June in 2018, 2019, and 2020 (Part 1). Number of calls with specific characteristics was normalised to all calls. Calls (N) and call characteristics (%) were compared between 2020 and 2018/2019 (average), within PCCs/countries and grouped. Correlation between call volume and COVID-19 cases per PCC/country was examined. All PCCs received a survey on workload (Part 2). Parts 1 and 2 were independent.
Results
For Part 1, 36 PCCs (21 countries) supplied 26 datasheets. PCCs in the UK and in France merged data and supplied one datasheet each with national data. Summed data showed an increase of 4.5% in call volume from 228.794 in 2018/2019 (average) to 239.170 in 2020 (p < 0.001). Within PCCs/countries, calls significantly increased for 54% of PCCs/countries (N = 14/26) and decreased for 19% (N = 5/26), three of which (N = 3/5) only serve medical professionals. Correlation between call volume and COVID-19 cases was (non-significant) positive (Rho >0.7) in 5/26 PCCs/countries (19%), and negative in 6/26 (23%). Call characteristics (median proportion of grouped data in 2018/2019 vs. 2020) changed: fewer medical professionals called (40 vs. 34%, p < 0.001), calls on intentional exposures decreased (20 vs. 17%, p < 0.012), as did calls on patients between 13 and 17 years (5 vs. 4%, p < 0.05). Calls on specific exposures increased; disinfectants from 1.9 to 5.2%, and cleaning products from 4.4 to 5.7% (p < 0.001). For Part 2, 38 PCCs (24 countries) filled the survey on workload (number/length of shifts and time on PCC duties), which increased in 23/38 PCCs (61%), while 10/38 (26%) worked with fewer employees.
Conclusions
Obtaining aggregated European PCC data proved challenging but showed an increase in overall call volume and workload during the first COVID-19 wave. Call characteristics changed including fewer calls from professionals and more calls on specific exposures. Within single PCCs/countries a variety of effects was observed.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has affected the lives of many and put a heavy burden on health care systems worldwide. During the first wave of the pandemic, national restrictions and lockdowns were ordered in most European and other countries, mostly from March 2020 onwards [Citation1]. Furthermore, cleaning and disinfectant protocols were recommended. Poison Control Centres (PCCs) in the United States (US) and in Europe have reported more accidental exposures to disinfectants in young children in March and April 2020 [Citation2,Citation3]. Furthermore, calls to PCCs on cleaners and disinfectants increased across all age groups in the US, Canada, France and Italy [Citation4–8].
National organisation of PCCs varies widely across Europe. Some countries have a single PCC, while others have several PCCs that sometimes use a national database (UK and France). Furthermore, the documentation and logging of calls are diverse, for example different categorisations of age groups and classifications of exposures are applied. Although efforts initiated by the European Commission were made to harmonise documentation amongst European PCCs in the early 1990s [Citation9], no European database of PCCs exists, nor do datasets exist that collect comparable data.
Consequently, investigating the effect of COVID-19 on the epidemiology of poisoning is challenging. This study started a collaborative network between European PCCs, catalysed by the European Association of Poisons Centres and Clinical Toxicologists (EAPCCT). The methodology, feasibility of the data collection and the time required for data collection from multiple PCCs was evaluated by a limited cohort of PCCs [Citation10]. Based on this pilot, categories and parameters of interest were selected for the more comprehensive study presented here.
This study investigated the effect of the first wave of COVID-19 on the work of European PCCs by examining call volume, call characteristics and workload in European PCCs.
Material and methods
Participants from European countries
All European PCCs were invited to participate, based on the World Health Organisation (WHO) list of managers of PCCs [Citation11] combined with the list of countries of the WHO Regional Office for Europe [Citation12]. Participation was requested via email to managers of 65 PCCs on 8 January 2021, and two reminders were sent (29 January and 6 March 2021). PCCs could contribute data up to 19 March 2021. All PCCs managers were also asked to participate in a survey on changes in organisational aspects during the COVID-19 pandemic. In countries with more than one PCC, each (single) PCC was invited to participate. Data on COVID-19 cases per country were obtained from the European Centre for Disease Prevention and Control (ECDC) on 2 August 2021 [1]. To investigate the correlation between changes in PCC workload and COVID-19 incidence, the highest number of COVID-19 cases per 100,000 inhabitants within 2 weeks (data available via ECDC) was categorised by ECDC categories as high (≥120), medium (61–119) and low (≤60) [Citation1].
Epidemiological data – calls to Poison Control Centres
Data collection
Data were collected in a standardised Excel template. We defined the first wave of the pandemic as the four-month period of March through June (inclusive) 2020 corresponding with the first major lockdowns in various countries. We compared this interval to the same interval in 2018 and 2019 to correct for possible seasonal effects on PCC calls. All 32 European countries surveyed by the ECDC had restrictions from March 2020 onwards [Citation1]. Data were collected on calls to PCCs, not on website consultations. Only calls with at least 1 patient with at least one exposure were included. Parameters included the total number of calls taken and patients involved. In addition, data were collected on call characteristics, including the type of caller (medical professional or public), reason for exposure (accidental, intentional (all), intentional suicide attempt), age groups (0–4, 5–12, 13–17, 18–65, 66–75 and ≥76 years), and specific exposures. Specifically, the number of calls on disinfectants (biocides to apply on skin (ECHA category PP-BIO-1) or surfaces (PP-BIO-2)), household cleaning products (all-purpose cleaners (PC-CLN-2) and bleaching products (PC-CLN-3)), see Supplemental Methods 1.1 for ECHA categories [Citation13]) – and specific drugs used in COVID treatment (e.g. (hydroxy)chloroquine and antivirals) were collected.
Deviations from data collection
Where merged national data (of >1 PCC) were supplied, they were included in the analysis. Not all PCCs could supply all requested data. Please see Supplemental Methods 1.2 for deviations in data collection. Since not all PCCs could supply the number of patients affected by poisonings, these data are not presented.
Data analysis
France and UK have supplied one datasheet for their country (2 datasheets), although both countries have several PCCs. Single PCC data were not available in this case and therefore, country data were analysed. All other datasheets concern data from single PCCs, also if ≥1 PCC from the same country supplied a datasheet (24 datasheets). Both (26 datasheets) are referred to as PCC/country. Per PCC/country, the absolute numbers for 2018 and 2019 were averaged. The number of calls was compared between years (2020 vs. average of 2018–2019 (100%)) within PCCs/countries, and as summed data of all PCCs/countries (grouped). For visualisation purposes only, PCCs were categorised in three groups based on the number of calls from March to June 2020: small (<1000 calls), medium (1000–10,000 calls) and large PCCs (>10,000 calls). To investigate the correlation between changes in PCC call volume and COVID-19 incidence per PCC/country, the number of COVID-19 cases per month [Citation1], during the 4-month study period, was compared to the change in call volume per month per PCC/country. Spearman’s rho correlation coefficient was used to assess correlation, which was defined as Spearman’s rho >0.7 (positive) or < −0.7 (negative).
For all other characteristics, proportions were calculated per PCC/country relative to the total number of calls (or patients if available) of the corresponding time period (e.g. the number of calls with accidental exposures in March 2020, was expressed as a proportion of the total number of calls in March 2020, while the number of calls on accidental exposures from March to June 2020 (4-month study period) was expressed as a proportion of the total number of calls from March to June 2020). This corrects for general changes in the number of calls. Proportions were only calculated for variables with N ≥ 5 and compared between years (2020 vs. average of 2018 − 2019) within PCCs/countries, and for all PCCs/countries (grouped). Data were tested for normality using the One-Sample Kolmogorov − Smirnov test with p < 0.05. Differences between 2020 and 2018 − 2019 (average) within a PCC/country were assessed using the Pearson’s Chi-square test (p < 0.05). Differences between 2020 and 2018 − 2019 (average) for all PCCs/countries (grouped) were assessed using the Wilcoxon Signed-Rank test (dependent samples, exact sig. (t-tailed), p < 0.05). Grouped data are presented as median [first quartile; third quartile]. Data were analysed using IBM SPSS Statistics version 26.0.0.1 (IBM SPSS, Armonk, NY, USA), GraphPad Prism version 9 (Graphpad Software Inc., La Jolla, CA, USA) and Microsoft Excel version 2016 (Microsoft Corporation, Redmond, WA, USA). SAMPL guidelines for basic statistical reporting were applied [Citation14].
Organisation of PCCs
Data were collected using SurveyMonkey® (see Supplementary Methods 1.3). Questions were included on changes in shifts (tasks of) employees, financials and the implementation of protocols for a shortage of staff due to sick leave and for a hygienic working place (safe working) were queried. Workload for PCCs was defined as the number and length of shifts and the time spent on PCC duties. Activities outside the usual PCC duties (“other activities”) involved redeployment in hospital or other duties directly related to the COVID-19 wave. Data were analysed using Microsoft Excel (2016).
Results
The effect of the first wave of COVID-19 on the work of European PCCs was examined using two independent methods. Epidemiological data on call volume and characteristics to PCCs were collected using a datasheet (Part 1), which was returned by 36 PCCs from 21 countries (for participating countries and PCCs see ). Data on workload were collected using a survey (Part 2), which was returned by 38 PCCs in 24 countries (for participating countries see Supplemental Table 2). 28 PCCs in 18 countries responded to both the epidemiological and operational surveys. Seven PCCs in 4 countries responded only to the epidemiological survey, and 12 PCCs in 8 countries responded only to the operational survey.
Table 1. Characteristics of European Poison Control Centres (PCCs) in this study.
Table 2. Changes in the number of calls to European Poison Control Centres (PCCs) in 2020 vs. 2018/2019: grouped by PCCs with increasing or decreasing calls.
Epidemiological data – calls to Poison Control Centres
Of the 65 PCCs invited to contribute data, 36 PCCs from 21 countries responded, with 26 datasheets (). PCCs in the UK and in France merged data and supplied one datasheet each with national data. During the 12 months included in this analysis (4 months in 2018, 2019 and 2020) 696,699 calls were handled.
Number of calls
To compare the number of calls during the COVID pandemic to those pre-COVID, the numbers in 2020 were compared to the average numbers in 2018 and 2019 (monthly, or 4-monthly (the study period)).
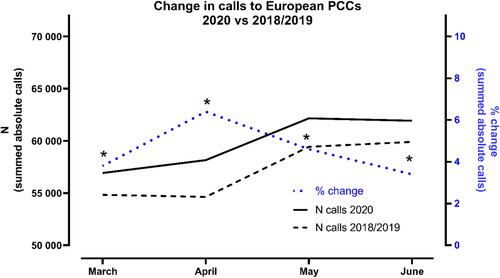
When summing the number of calls of all PCCs/countries during the 4-month study period (March–June), 228,794 calls were handled in 2018/2019 (average of years) and 239,170 calls in 2020 (). Significant increases in summed calls of all PCCs/countries were observed during the 4-month study period (4.5%), and in all single months with the largest increase in April (6.4%) (, , p < 0.001).
Figure 1. Change in calls to European Poison Control Centres in 2020 vs. 2018/2019. The monthly number of calls to all PCCs/countries (26 datasheets) in 2020 was summed. For 2018/2019, the monthly number of calls in 2018 and the monthly number of calls in 2019 were averaged per PCC/country, and subsequently summed for all PCCs/countries (26 datasheets). Note that UK and France supplied nationwide data representing >1 PCC. *The number of calls (summed data) was significantly higher in 2020 compared to 2018/19 (p < 0.0005, χ2 test).
Since large differences were observed in the number of calls between PCCs/countries ranging from 48 to nearly 60,000 calls in the 4-month study period (), we also examined changes within PCCs/countries, monthly and for the 4-month study period (26 datasheets, , and ). The number of calls during the 4-month study period (March-June) increased for 54% PCCs/countries (N = 14/26, p < 0.05, median increase 10% [7;20]), while for 27% of PCCs/countries (n = 7/26) the number of calls remained stable (). Five PCCs/countries (19%, N = 5/26) received fewer calls during the 4-month study period (p < 0.05, median decrease 7% [−13;−6], ): Italy-Bergamo, Italy-Pavia, the Netherlands, Slovenia and the UK, three of which only serve medical professionals (). Median changes in the number of calls per month are presented in , showing the largest increase in calls in April of 21% [16;46] (8 PCCs). Since changes within PCCs/countries range from increased to decreased call volumes during the 4-month period, monthly changes of individual PCCs/countries are also presented (). The variability in changes was particularly present in smaller PCCs and less pronounced in larger PCCs. The largest decrease in call volume was observed by The Republic of North Macedonia in March (−42%), while the largest increase was observed by Bosnia and Herzegovina in May (89%) ().
Figure 2. Change in calls within European Poison Control Centres or countries in 2020 vs. 2018/2019 and COVID-19 cases in 2020 per country. The monthly number of calls in 2018 and the monthly number of calls in 2019 were averaged per PCC/country. For each PCC/country, the monthly number of calls in 2020 was expressed relative to the average monthly number of calls in 2018 and 2019 (represented by 0% effect). For better visualisation, PCCs are grouped according to the number of calls from March to June 2020 in (A) <1000, (C) 1000–10,000 and (E) >10,000 calls. Note the different y-axes and that UK and France supplied nationwide data representing ≥1 PCC. B, D and F represent COVID-19 cases during the study period (March–June) per 100,000 inhabitants per country (cumulative number for 14 d, ECDC). Correlation between change in calls and the number of COVID-19 cases in the same month is listed for all PCCs/countries (R = Spearman’s rho, N = 4 XY pairs (March, April, June, and July)). For a colour version, please read online.
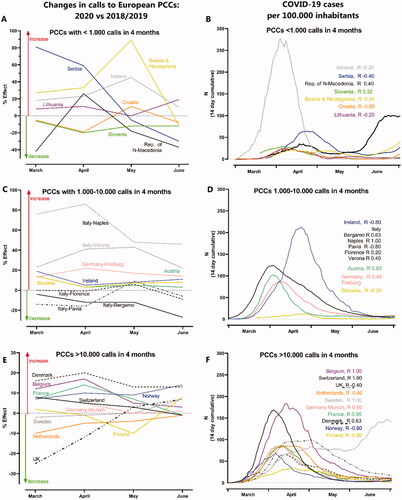
The peak in COVID-19 incidence during the 4-month study period was often limited to 1–2 month(s), but peaked in different months in different countries (). A positive correlation (Rho >0.7) was observed between call volume and COVID cases in 5/26 PCCs/countries (19%; Belgium, France, Italy-Naples, Sweden and Switzerland), while 6/26 (23%; Croatia, Finland, Ireland, Italy-Pavia, The Netherlands and Norway) observed a negative correlation (Rho < −0.7) and in 15/26 (58%) no correlation was observed (). None of the correlations were significant.
Type of caller
Four PCCs that only (or mainly) take calls from medical professionals (Netherlands, Slovenia, UK and The Republic of North Macedonia) were excluded for this analysis. The proportion of calls on type of caller (relative to all calls) during the 4-month study period of all PCCs/countries in 2020 was compared to those in 2018/2019. The median proportion of medical professionals calling decreased from 40% [33;57] in 2018/2019 to 34% [28;45] in 2020 (p < 0.001). The median proportion of the public calling increased from 59% [41;69] in 2018/2019 to 64% [56;72] in 2020 (p = 0.002).
Within PCCs/countries no significant changes were observed in the proportion of calls on type of caller during the 4-month period. The absolute number of calls from medical professionals (4-month period) significantly decreased in 50% of PCCs/countries (N = 11/22), and increased in 32% of PCCs/countries (N = 7/22).
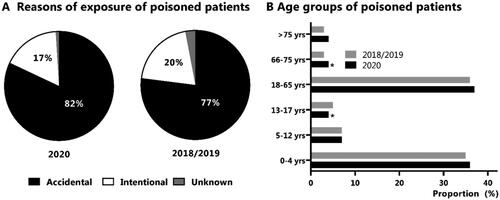
Reason for exposure
The proportion of calls on intentional or accidental exposures (relative to all calls) during the 4-month study period of all PCCs/countries in 2020 was compared to those in 2018/2019. The median proportion of intentional exposures decreased from 20% [14;24] in 2018/2019 to 17% [14;23] in 2020 (p = 0.012). The median proportion of accidental exposures increased from 77% [70;84] in 2018/2019 to 82% [75;85] in 2020 (p = 0.016, ). No significant changes were observed in the median proportion (nor in median absolute numbers) of exposures due to a suicide attempt.
Figure 3. Median proportion of reasons of exposure (A) and age groups (B) of calls to European Poison Control Centres or countries in 2020 vs. 2018/2019. *The median proportion of calls (grouped data) was significantly higher in 2020 compared to 2018/19 (p < 0.0005, χ2 test). For deviations in data supply regarding age groups, see Supplemental Material 1.2.
Within PCCs/countries the only significant change during the 4-month period was observed for Italy-Naples; the proportion of intentional exposures decreased from 30 to 16% in 2020 (p = 0.038). However, the absolute number of calls on intentional exposures (4-month period) significantly decreased in 50% of PCCs/countries that supplied data on this (N = 10/20), and increased in 25% of PCCs/countries (N = 5/20).
Age groups
The proportion of calls on specific age groups (relative to all calls) during the 4-month study period of all PCCs/countries in 2020 was compared to those in 2018/2019. The highest proportions were observed for calls involving small children (0–4 years, 38% (2020)) and adults (18–65 years, 36% (2020)) (). Changes in the median proportion of calls on specific age groups are presented in (grouped data). The median proportion (as well as the absolute median number) of calls on small children (0–4 years) did not change (grouped data). Also, within PCCs/countries no significant changes were observed during the 4-month study period in the proportion of calls on patients of specific age groups, apart from a significant decrease on calls involving patients of 0–4 years in Serbia. See Supplemental Figure 1 for monthly data on changes in the proportion of calls involving patients of 0–4 years and 18–65 years within PCCs/countries. However, the absolute number of calls on small children within PCCs/countries, did significantly increase in 33% of PCCs/countries (N = 8/24), all of which also observed a significant increase in the total number of calls. The PCCs/countries that observed significant changes in absolute number of calls on patients in specific age groups are listed in Supplemental Table 1.
Specific exposures
In most participating PCCs/countries, proportions of calls on specific exposures (relative to all calls) were low (<5%). Proportions of calls on specific exposures during the 4-month study period of all PCCs/countries in 2020 were compared to those in 2018/2019 (). Significant increases were observed in the median proportion of calls on exposures to disinfectants (ECHA-PP-BIO1, 2, from 1.9 to 5.2%) and household cleaning products (from 4.4 to 5.7%) (p < 0.001). The most distinct increase was observed for disinfectants applied for human use (ECHA-PP-BIO1, from 0.7 to 2.7%, p = 0.002) and to a lesser extent for disinfectants applied on surfaces (ECHA-PP-BIO2, from 1.1 to 1.8%, p < 0.001). For median proportions, see and Supplemental Figure 2 for data per PCC/country. Relatively large increases (8–21%) in median proportions of calls on exposures to disinfectants were observed by relatively small PCCs (Serbia, Lithuania and Croatia).
Table 3. Median proportion of calls on specific exposures to European Poison Control Centres (PCCs) in 2018/19 and 2020.
Only 10 PCCs/countries received calls (>N = 5) on drugs used in COVID-19 treatment, 8 PCCs/countries on antivirals, 2 on hydroxychloroquine, and none on chloroquine. No significant changes were observed in the proportions of calls on exposures to drugs used in COVID-19 treatment during the 4-month period (, Supplemental Figure 3 for data per PCC/country).
Organisation of PCCs
The survey was completed by 38 PCC managers (58%) from 24 countries (Supplemental Method 1.3 for survey and Supplemental Table 2 for participating countries). All their PCCs process calls from medical professionals, 95% also from the public, and 60% also from veterinarians. During the first COVID-19 wave the workload (the number or length of shifts or time spent on PCC duties) increased in 23 PCCs (61%, ). Time spent on PCC duties increased by <25% in 29% of PCCs (N = 11) and by 25–50% in 16% of PCCs (N = 6). Only two PCCs were staffed with more employees (5%). Ten PCCs (26%) worked with fewer employees, and in five of those the number or length of shifts increased. In 21 PCCs (59%) employees worked on other duties more than usual: PCCs staff was redeployed in hospital (17 PCCs) or fulfilled other additional duties (9 PCCs, ). In countries with a high and medium COVID-19 incidence, the proportion of PCCs with an increased workload and redeployment to hospital was higher than in countries with a lower incidence. However, additional tasks directly related to the COVID-19 wave were mainly taken over by PCCs in countries with a medium and lower COVID-19 incidence ().
Table 4. PCC workload related to COVID-19 incidence.
The financial situation was stable in 82% of PCCs (N = 33). Nearly half of the PCCs (N = 17, 45%) implemented protocols to ensure continuation of work processes upon increasing sick leave. For example, PCCs co-operated with other national PCCs to fill shifts (N = 7). Other PCCs reduced the number of shifts at the workplace and/or prolonged shift duration (N = 9). Also, senior staff was (ready to be) employed at phone shifts (N = 2) and employees were divided into two groups that did not meet at work (N = 1). Safe working procedures involved social distancing (N = 35, 92%), disinfection of the workplace (N = 34, 89%) and working from home when possible (N = 25, 66%). With respect to office sharing, 12 PCCs (32%) no longer shared workplaces, eight PCCs (22%) only allowed one employee per room, while seven PCCs (18%) allowed two employees in a room. Protocols were implemented in all but one PCC.
Discussion
We collaborated with as many European PCCs as possible and received epidemiological data of 36 PCCs (55%) from 21 European countries (). These data provide a thorough insight into the effect of the COVID-19 pandemic on the epidemiology of poisoning, and the activities of PCCs.
Upon summing the data, PCCs processed significantly more calls during the first COVID-19 wave, compared to the years before (+4.5%, , ). Within PCCs/countries, most have observed an increase (54%, median increase of 10%), while 27% processed a stable number of calls (, and ). Five PCCs/countries (19%), among which 3 only serve medical professionals, observed a decrease in the number of calls. This is in line with the decrease in proportion (and absolute numbers) of calls by medical professionals seen in PCCs/countries that serve both the public and professionals (, ). Increases in the number of calls have been reported previously [Citation7]. In contrast, the use of healthcare facilities and emergency department (ED) visits fell dramatically during the pandemic [Citation17,Citation18]. This could have contributed to the increased consultations by the public to PCCs from 59 to 64% for all PCCs/countries during the 4-month period. In this way, PCCs can relieve some of the pressure on health care systems during a pandemic.
While smaller PCCs observed wider deviations in effect on the monthly number of calls compared to larger PCCs (), most changes for smaller PCCs were not significant during the 4-month period (Bosnia, Croatia, Lithuania and The Republic of North Macedonia), likely due to a low number of calls. However, Iceland and Serbia did observe significant increases in the number of calls during the 4-month period, while Slovenia, serving only medical professionals, observed a significant decrease (). In the group of medium size PCCs, comparisons by month showed large differences between countries and even regions, as exemplified by Italian PCCs. In addition, Austria, Germany-Freiburg, Ireland and Slovakia PCCs processed significantly more calls during the 4-month period (6, 16, 11 and 8%, respectively, ). Many of the large PCCs processed higher number of calls (), although the UK and the Netherlands (both serving only medical professionals) processed fewer calls during the first months (−6 and −5%, respectively), despite a large wave of COVID-19 cases. The most stable call volume was observed in Sweden, although a significant increase was observed in June (7%), correlating to the later peak of COVID-19 cases in Sweden in June and a Rho correlation of 1.0 between number of calls and COVID-19 cases (). To examine the correlation between the number of COVID-19 cases and the change in call volume only four data points (4-month period) per PCC/county were available, possibly resulting in no statistical differences. However, high correlation values were obtained for some PCCs/countries (). Both negative (< −0.7) and positive (>0.7) correlations were observed (both ∼20% of all PCCs/countries)).
The COVID-19 measures, such as total lockdown, home isolation, increased time at home with children, and fear of the virus [Citation17–19], could affect mental well-being of the population [Citation20]. Luckily, the median proportion of calls concerning intentional poisonings of all PCCs/countries even decreased slightly (median absolute numbers were unaffected), but significantly, during the 4-month period (). Children being at home more often due to COVID-19 measures could also result in more accidental paediatric poisonings. However, the median proportion of calls concerning young children (0–4 years) remained stable at 38% (grouped data) as did proportions of poisoning among most other age groups (). Although the proportion of calls in young children is comparable to that of PCCs in non-European countries [Citation2,Citation21], the lack of a COVID-19 effect is contrasting. Californian PCCs have reported an increase in the absolute number of calls concerning young children during school hours while children were at home due to lockdown [Citation20]. The median absolute number of calls concerning young children (0–4 years) of all PCCs/countries in our study also remained stable, although significant changes were observed within PCCs/countries (33% observed in increase and 17% a decrease). Only few PCCs/countries observed an increase of absolute calls regarding school children 5–12 years (N = 4/23), while none observed an increase in calls for children of 13–17 years Notably, absolute numbers of calls on the large group of adults (18–65 years) increased in 40% of PCC/countries (N = 10/25), reflecting on the significant increase in total number of calls in nine of these PCCs/countries.
Other COVID-19 measures involved disinfecting surfaces and hands frequently. Although the proportion of calls on specific exposures was low (<5%), exposures to disinfectants significantly increased, as did exposures to household cleaning products like bleach, and all-purpose cleaner (). Relatively larger changes were registered by smaller PCCs in Eastern Europe (Supplemental Figure 2). These observations are in line with other studies [Citation3–6]. While outside of Europe, health incidents have been reported due to chloroquine exposures [Citation22], no significant changes were observed on proportions of calls on antivirals or hydroxy(chloroquine), possibly due to low numbers of calls on this in general ().
The pandemic also affected the organisation of European PCCs. Many experienced a higher workload, with fewer staff and no increase in finances (). The higher workload is in line with an increase in the number of calls for 54% of the PCCs (N = 14/26). In addition, in 60% of PCCs staff worked on other duties more than usual, possibly resulting in the staff remaining to work on PCC duties having to cover more or longer shifts. Our survey amongst EAPCCT members (N = 60 unpublished data), showed that 40% worked more shifts and 30% worked longer shifts during the first wave of the pandemic, highlighting the contribution of European PCCs in supporting medical care during the first wave of COVID-19.
Limitations
Our study has several limitations. Only 36 of the 65 PCCs that were invited to participate supplied data, so our data are not representative for the whole of Europe. The ease of data extraction varies largely amongst PCCs, and difficulties in extraction may underlie the lack of participation. Also, PCCs in different countries and/or regions vary strongly in organisation, call volume and timing of the peak in COVID-19 cases, contributing to difficulties in finding an overall conclusion on the effect of COVID-19 on the number of (specific) calls. Furthermore, data were collected using a standardised Excel template and not directly from electronic records, since, unlike in the US, no common European database exists. The PCCs that supplied data were not always able to supply all the requested variables, or categories. For analysis of such data, regrouping was required (See Supplemental Material 1.2). Some PCCs process low numbers of calls, hampering comparison between years when examining small time windows of 1 month, such as in this study. All PCCs, even the ones with large numbers of calls, had low numbers of calls on specific exposures. Though we tried to balance descriptive and statistical analysis, multiple testing increases the probability of false-positive findings. Furthermore, the observed changes in calls could be an underestimation, since the number of calls could be affected by changes in staffing (26% worked with fewer employees), which could prolong waiting times for callers and increase abandoned calls.
Conclusion
International networks, though challenging, are essential to identify changes and trends in poisonings and threats to public health in Europe. Grouped data of all European PCCs/countries showed a small but significant 4.5% increase in call volume during the first COVID-19 wave in 2020. Furthermore, within PCCs/countries comparison showed a distinct increase in call volume of 10% for half of PCCs/countries. Calls from the public represent most calls (∼60%), and the increase in overall calls could be explained by more calls from the public, and fewer calls from medical professionals. This reflected in a reported higher workload for many PCCs, on top of redeployment of staff on other duties related to the COVID-19 wave. A decrease in call volume was observed in 20% of PCCs/countries, most of which exclusively serve medical professionals. Proportions of calls on intentional exposures and age groups remained stable, though changes were observed in absolute call volumes on small children and adults. Finally, proportions of calls on exposures that are likely related to the COVID-19 measures, such as cleaning products and disinfectants, increased.
In conclusion, the COVID pandemic affected the epidemiology of poisonings and the workload of many European PCCs, though a large variety of effects is one of the main observations of our study.
Supplemental Material
Download MS Word (818.5 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
References
- ECDC (European Centre for Disease Prevention and Control); 2021 [cited 2021 August 2]. Data on country response measures to COVID-19. Available from: https://www.ecdc.europa.eu/en/publications-data/download-data-response-measures-covid-19
- McCulley L, Cheng C, Mentari E, et al. Alcohol-based hand sanitizer exposures and effects on young children in the US during the COVID-19 pandemic. Clin Toxicol. 2021;59(4):355–356.
- Babić Ž, Turk R, Macan J. Toxicological aspects of increased use of surface and hand disinfectants in Croatia during the COVID-19 pandemic: a preliminary report. Arh Hig Rada Toksikol. 2020;71(3):261–264.
- Chang A, Schnall AH, Law R, et al. Cleaning and disinfectant chemical exposures and temporal associations with COVID-19 - National poison data system, United States, January 1, 2020–March 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(16):496–498.
- Yasseen Iii A, Weiss D, Remer S, et al. Increases in exposure calls related to selected cleaners and disinfectants at the onset of the COVID-19 pandemic: data from Canadian Poison Centres. Health Promot Chronic Dis Prev Can. 2021;41(1):25–29.
- Rosenman KD, Reilly MJ, Wang L. Calls to a state poison center concerning cleaners and disinfectants from the onset of the COVID-19 pandemic through April 2020. Public Health Rep. 2021;136(1):27–31.
- Le Roux G, Sinno-Tellier S, Puskarczyk E, et al. Poisoning during the COVID-19 outbreak and lockdown: retrospective analysis of exposures reported to French Poison Control Centres. Clin Toxicol. 2021;59(9):832–839.
- Soave PM, Grassi S, Oliva A, et al. Household disinfectant exposure during the COVID-19 pandemic: a retrospective study of the data from an Italian Poison Control Center. Eur Rev Med Pharmacol Sci. 2021;25(3):1738–1742.
- EC. 2017. European Commission, Commission Regulation (EU) 2017/542 of 22 March 2017 amending Regulation (EC) No 1272/2008 of the European Parliament and of the Council on classification, labelling and packaging of substances and mixtures by adding an Annex on harmonised information relating to emergency health response [cited 2021 October 28]. Available from: https://eur-lex.europa.eu/legal-content/en/ALL/?uri=CELEX%3A32017R0542.
- Hondebrink L, Faber K, Zammit M, et al. The impact of the first wave of COVID-19 on poison Centre (PC) activities in 4 European countries: a pilot study. Clin Toxicol. 2021;59(6):542.
- World Health Organisation (WHO); 2019. [cited 2019 February 28]. List of managers of PCCs. Available from: https://apps.who.int/poisoncentres/
- World Health Organisation (WHO). List of countries of the WHO regional office for Europe. Available from: https://www.euro.who.int/en/countries.
- ECHA (European Chemicals Agency). ECHA classification; 2021. [cited 2021 March 24]. Available from: https://poisoncentres.echa.europa.eu/eu-product-categorisation-system.
- Lang TA, Altman DG. Basic statistical reporting for articles published in biomedical journals: the "statistical analyses and methods in the published literature" or the SAMPL guidelines. Int J Nurs Stud. 2015;52(1):5–9.
- Locatelli C. Italy. In: Woolf A, editor. History of modern clinical toxicology. 1st ed. Cambridge (MA): Academic Press, 2021; Chapter 5.9, p. 451–462.
- The Economist. Tracking the coronavirus across Europe; 2021 [cited 2021 August 2]. Available from: https://www.economist.com/graphic-detail/tracking-coronavirus-across-europe.
- Hartnett KP, Kite-Powell A, DeVies J, et al. Impact of the COVID-19 pandemic on emergency department visits – United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704.
- Thornton J. Covid-19: A&E visits in England fall by 25% in week after lockdown. BMJ. 2020;369:m1401.
- Cellini N, Canale N, Mioni G, et al. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020;29(4):e13074.
- Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920.
- Levine M, Minns A, Ontiveros S, et al. Evaluating the impact of home quarantine during the coronavirus pandemic on pediatric exploratory ingestions. Clin Toxicol. 2021;59(7):673–674.
- Wong A. COVID-19 and toxicity from potential treatments: panacea or poison. Emerg Med Australas. 2020;32(4):697–699.
