Abstract
Context
Childhood and adolescent misuse and abuse exposures remain a serious public health challenge in the United States. This study aimed to describe recent trends and patterns of intentional substance misuse and abuse exposures among school-aged children and adolescents in the United States.
Methods
This study was a retrospective cohort study of intentional misuse and abuse exposures in children 6 through 18 years reported to the National Poison Data System (NPDS) from January 1, 2000, through December 31, 2020. Demographic trends, reported clinical effects, treatments, management sites, and health outcomes were assessed overall and within four age categories: 6–9, 10–12, 13–15, and 16–18.
Results
Between 2000 and 2020, there were 338,727 cases regarding intentional misuse and abuse exposures for children ages 6 through 18 years old. Overall, misuse/abuse ingestions fluctuated over time, with a peak in 2011. The majority of intentional misuse/abuse ingestions occurred in males (58.3%), and more than 80% of all reported exposure cases occurred in youth aged 13 to 18. 32.6% of ingestions resulted in worse than minor clinical outcomes. Older age groups had a greater number of severe medical outcomes compared to younger age groups. Major or life-threatening exposures (including those resulting in death) were more common in males. Overall, deaths were rare (n = 450), 0.1%). Male sex, older age, abuse ingestions, exposure site of a public area or other residence, and multiple ingested substances were other factors associated with increased mortality. Marijuana exposure rates had the highest average monthly increase overall, with the most dramatic rise occurring from 2017 to 2020. Edible marijuana preparations accounted for the highest increase in call rates compared with all other forms of marijuana.
Discussion and Conclusion
With over 330,000 poison center cases reported during the 20-year study period, intentional substance misuse and abuse exposures substantially impact the pediatric population. The substances most commonly misused/abused are more widely available substances such as over-the-counter medications, household products and pharmaceuticals commonly prescribed to youth. Differences in age and sex were evident, with males and adolescents more likely to abuse and misuse substances. Our study describes an upward trend in marijuana misuse/abuse exposures among youth, especially those involving edible products. These findings highlight an ongoing concern about the impact of rapidly evolving cannabis legalization on this vulnerable population.
Introduction
Substance misuse and abuse are significant public health threats. While national survey data helps track substance use trends among young people, it often lags behind current trends and information about impacts on the healthcare system. These surveillance methods are usually limited to adolescents and adults and rarely include school-aged children. Earlier initiation of substance use is an important predictor of developing a substance use disorder later in life. As such, clinicians who care for children and adolescents should be well-informed about emerging and shifting patterns of drug abuse and misuse to offer early identification and intervention for problematic substance use. Additionally, age-specific substance misuse/abuse trends may provide further insight and direction for future prevention efforts. This study aimed to identify recent outcomes and trends in intentional substance misuse and abuse among school-aged children and adolescents using a national source of poison center case data over 20 years.
Methods
This is a retrospective cohort study of intentional misuse and abuse exposures in school-aged children and adolescents reported to the National Poison Data System (NPDS) from January 1, 2000, through December 31, 2020. NPDS is maintained by the American Association of Poison Control Centers (AAPCC). Data are collected at each certified regional U.S. Poison Control Center (PCCs). Currently, 55 PCCs serve the entire U.S. population, territories, and Washington DC. Poison centers receive calls from the public, health professionals, and public health agencies for exposure to various substances through a 24-hour poison helpline. PCCs are staffed 24 h a day by health professionals with specialized training in toxicology. These trained specialists in poison information collect and code case data entered into an electronic health record collection system that is uploaded to NPDS in near real-time.
We received coded, de-identified NPDS data for all intentional abuse and misuse cases in individuals aged 6 through 18 years old. Intentional misuse is defined as an exposure resulting from the intentional improper or incorrect use of a substance for reasons other than the pursuit of a psychotropic effect. Intentional abuse exposures are from the intentional improper or incorrect use of a substance in which the patient was likely attempting to gain a “high,” euphoric effect or some other psychotropic effect, including recreational use of a substance for any effect. Only coded data were available to the investigators, not free text fields. We excluded cases from unknown geographic regions and those with missing age. The data were a mix of single-substance and polysubstance exposures; however, the number of single substance exposures was explicitly reported.
Statistical analysis
Data were received from the NPDS in Excel (Microsoft, Redmond, WA) format. Data analysis was largely descriptive and included summary statistics for demographic trends, reported clinical effects, treatments, management sites, and health outcomes. We assessed trends of intentional abuse/misuse exposures overall and within four age categories: 6–9, 10–12, 13–15, and 16–18. The top 10 most ingested substances were determined for each year of the study and plotted over time. Additionally, the substances with the highest average monthly increase in exposure rates were determined overall and for each age group using linear regression. We also analyzed marijuana exposures by type of marijuana preparation for all ages and by age group, sorted by the average monthly increase. Multivariable logistic regression of odds of death after a misuse/abuse ingestion was also performed. To correct for multiple testing, we calculated adjusted p-values using the Hochberg and Benjamini adaptive step-up Bonferroni method [Citation1]. To test for multicollinearity, we calculated the variance inflation factor (VIF) for each variable, and to check model fit and specification, we calculated the c-statistic (AUROC) and Hosmer–Lemeshow goodness-of-fit statistic.
Clinical outcome was coded using a priori definitions from the NPDS coding manual: no effect, minor effect, moderate effect, major effect, or death [Citation2]. This study was determined exempt by the institutional review board of Oregon Health and Sciences University (OHSU). Data management and analysis was performed in SAS 9.4 (SAS Institute, Cary, NC, USA), and analysis and creation of figures was performed in R 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient characteristics
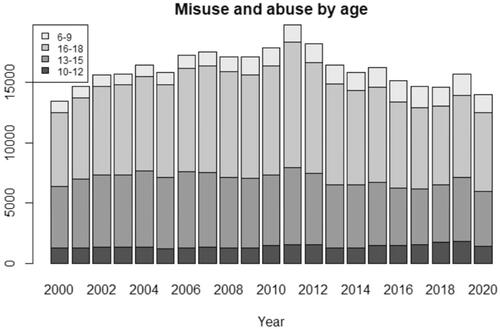
Between 2000 and2020, US Poison Control Centers (PCCs) consulted on 338,727 cases regarding intentional misuse and abuse exposures for children ages 6 through 18 years old. Characteristics of exposures are described in . Overall, the frequency of misuse/abuse ingestions fluctuated over time, with a peak in 2011 (). The majority of intentional misuse/abuse ingestions occurred in males (58.3%), and more than 80% of all reported exposure cases occurred in youth aged 13 to 18 (). The greatest proportion of misuse/abuse cases involved exposures in adolescents aged 16–18 (48.5%). Overall, intentional abuse cases were more frequent than misuse (57.4% vs. 42.6%). Misuse ingestions were more common in younger age groups, while abuse ingestions occurred more frequently in older age groups. A single substance was involved in 81.2% (275,144) of misuse/abuse exposures ().
Table 1. Population characteristics, clinical effects, therapies, and outcomes of abuse and misuse ingestions, n = 338,727.
Substance trends
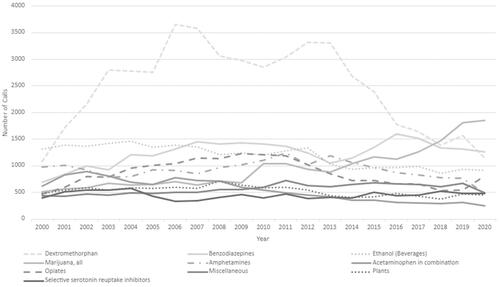
illustrates trends in total misuse/abuse cases for the most reported substances per year over the 20-year period. In 2000, the largest number of misuse/abuse cases involved exposure to ethanol (1318, 9.8%). Dextromethorphan was the most reported misused/abused substance from 2001 to 2016. Since 2018, the most reported misused/abused substance involved exposure to marijuana. Dextromethorphan had the highest total number of exposure cases (51,667, 15.25%) over the study period, followed by cases for benzodiazepines (26,037, 7.68%). Intentional misuse/abuse ingestions of diphenhydramine alone have been steadily increasing, with the number of cases reported in NPDS increasing from a low of 193 cases in 2000 to 668 cases in 2020.
Cases regarding abuse or misuse of marijuana have steadily increased over the study period (). There were 510 and 1761 marijuana exposure cases in 2000 and2020, respectively, corresponding with a 245% increase during the 20 years (). Marijuana exposure cases remained relatively stable from 2000 to 2009 (mean: 636.7, range: 510–713), then steadily rose beginning around 2011, with an even more dramatic rise in cases from 2017 to 2020. This upward trend contrasts with ethanol exposure cases, which have gradually declined over the study period. There were a total of 1318 ethanol cases in 2000 and 916 in 2020, with an average linear decrease of 28.1 exposures each year (95% CI 21.8 to 34.4, p < 0.01) across the study period. Ethanol misuse/abuse cases exceeded the number of marijuana cases every year from 2000 through 2013. In 2014, marijuana misuse/abuse exposure cases surpassed ethanol cases, and since then, marijuana exposure cases have exceeded ethanol cases every year, and by a greater amount each year than the prior.
lists those substances with the highest average monthly increase in exposure rate overall and for each age group. There were differences in the types of exposures that accounted for the increased case rates across each age group. Marijuana (all preparations) exposure rates had the highest average monthly increase overall, followed by cannabidiol (CBD), diphenhydramine-alone, eCigarettes (nicotine), and benzodiazepines (all p < 0.01). Exposures from vitamins, plants, melatonin, and hand-sanitizers increased during the study period in younger age groups. In contrast, marijuana, diphenhydramine-alone, hand sanitizers, CBD, e-cigarettes (nicotine), and benzodiazepine exposures accounted for the highest increase in case rates amongst older age groups.
Table 2. Substances with highest monthly average increase, 2000-2020 across n = 338,727 cases.
lists the top two marijuana preparations with the highest monthly average increase by age group. Edible marijuana preparations had the highest average monthly increase in call rates compared with all other forms of marijuana overall and within each age group except the 6 through 9-year-old group. Overall, there was an increase in edible marijuana exposures by 11.7 cases per month from 2000 to 2020 (95% CI 9.7-13.8, p < 0.0001). Adolescents (age 13–18 years) had an increase in exposures to concentrated extracts during the study period.
Table 3. Top 2 marijuana preparations with highest monthly average increase by age group, 2000-2020 across n = 338,727 cases.
Clinical effects
Several clinical effects occurred at similar rates across all the age groups, including seizures, hypotension, ventricular tachycardia/fibrillation, and dysrhythmia (). One-third (32.6%) of ingestions resulted in worse than minor clinical outcomes. Older age groups had a greater number of severe medical outcomes compared to younger age groups. Major or life-threatening exposures (including those resulting in death) were more common in males. Overall, deaths were rare (n = 450, 0.1%). Most deaths occurred in those 16 through 18 years old (n = 368, 81.7%), with only three deaths in children aged 6 through 9 years (). lists those factors associated with the highest increase in odds of death. After controlling for patient demographics and substances ingested, we found that opioid exposures were associated with the highest increase in odds of death (15.6, 95% CI: 12.6–19.3, p < 0.01). Opioids were associated with 286 instances of death (). No documentation of laboratory verification were available in these facilities, but fatality cases undergo a second level of review during the NPDS process to determine the contribution of the substance with the death and to maximize coding accuracy. Male sex, older age, abuse ingestions, exposure site of public area or other residence, and multiple ingested substances were other factors associated with increased mortality (). In the final regression model, there was no evidence of multicollinearity (all VIF < 1.5), and diagnostics indicated good model fit (Hosmer-Lemeshow p = 0.736; c-statistic = 0.894).
Table 4. Multivariable logistic regression of odds of death after a misuse/abuse ingestion.
Table 5. Substances coded as fatalities.a
Of the 331,993 cases managed in a health care facility (HCF), 168,721 (50.82%) were treated and released, 30,936 (9.31%) were admitted to a critical care unit, 26,198 (7.89%) were admitted to a non-critical care unit, and 16,973 (5.11%) were admitted directly to a psychiatric facility (). The percentage of patients treated in a HCF varied considerably with age. Only 8.36% of children 6-9 years and 8.71% of children between 10 and 12 years were managed in a HCF compared to 34.57% of younger teenagers (13–15 years) and 48.34% of older teens (age 16–18 years).
Discussion
The current study examined trends in US intentional abuse and misuse exposures in school-aged children and adolescents from 2000 to 2020. With over 330,000 poison center cases reported during the 20-year study period, intentional substance misuse and abuse exposures substantially impact the pediatric population. The most commonly misused/abused substances are more widely available substances, such as over-the-counter medications, household products and pharmaceuticals commonly prescribed to youth. Consistent with other studies, our current data indicate higher abuse/misuse among males and older adolescents [Citation3–5].
Developmental and societal factors contributing to pediatric poisoning vary widely from childhood to adolescence, as do the substances involved in these exposures. Effective prevention and treatment efforts require a thorough understanding of the specific vulnerabilities of different pediatric age groups. In the current study, intentional misuse and abuse exposures were significantly less common in children than adolescents, with the majority due to misuse rather than abuse, especially in children aged 6 to 9 years; this is consistent with prior studies [Citation6]. While both misuse and abuse ingestions increased with age, intentional abuse was significantly more common among adolescents than in children aged 6 to 12 years.
Consistent with prior literature, the current data indicate high sustained OTC medication misuse and abuse rates among older children and teens. OTC antihistamines were among the most commonly misused/abused substances in this study. Many OTC medications have a high potential for abuse and misuse since they are legal and easily obtainable without a prescription. Children and teens may perceive OTC drugs as relatively safe; however, a growing body of evidence demonstrates increasing rates of abuse and overdose of OTC medications in the United States [Citation3, Citation7–10].
While dextromethorphan (DXM) was the most reported substance over the study period, with high average monthly increase in misuse/abuse exposures, DXM misuse/abuse rates peaked in 2006 and have decreased since that time (). This observed decline in DXM abuse corresponds to increasing public health efforts and initiatives to reduce and prevent OTC medication abuse. In 2012, California became the first state to prohibit sales of DXM-containing products to minors. Since then, 21 states have adopted similar laws to combat teen abuse of OTC medications containing dextromethorphan.
Our study describes an upward trend in cannabis misuse/abuse exposures. These findings may reflect the impact of rapidly evolving cannabis legalization on this vulnerable population. While legalization of cannabis is primarily restricted to adult populations, it has rendered the drug more accessible to children and adolescents. In Canada, where national legalization occurred, and edibles became available in 2021, the proportion of cannabis-related Emergency Department (ED) visits with hospitalization for children aged 0 to 9 years old increased significantly after the introduction of edibles [Citation11]. This increase occurred despite a decrease in total poisoning-related pediatric ED visits. As the legal landscape around cannabis continues to evolve rapidly, so do the social norms around its use, with an overall steady decline in perceived risk associated with cannabis since 2009 [Citation12,Citation13]. Increased availability and peer norms changes are likely strong drivers of increasing cannabis use.
Along with increasing cannabis legalization, we are also seeing the emergence of alternative modes of consumption, especially non-combustible products such as edibles and vaping devices. A significant proportion of youth use alternative methods to consume cannabis [Citation14,Citation15]. In the current study, edible marijuana products had the highest average monthly increase in case rates across all ages compared with any other form of marijuana. This was also true within each age group, except for children 6 through 9. Marijuana concentrates/extracts (e.g. cannabis vaping liquid) were also used at significantly increasing rates by adolescents (aged 13–18 years). These edible products and vaping products are often marketed in ways that are attractive to youth, can be used with more discretion, and are more convenient. A focus group study with teenagers found that edibles were attractive to those concerned about smoking or the smell associated with smoking marijuana [Citation16].
While several studies show that edible cannabis products are increasingly perceived as less harmful by adolescents, concerns exist about their potency and delayed effects [Citation17–19]. Compared to smoking cannabis, which typically results in an immediate and titratable high, intoxication from edibles usually takes several hours, which may lead some individuals to consume greater amounts and cause delayed effects with unexpected and unpredictable highs. A study of marijuana-related Emergency Department (ED) visits in Colorado between 2012 and 2016 found that edible cannabis consumption led to more acute psychiatric symptoms and cardiovascular events than inhaled cannabis and that ED visits due to edibles were 33 times higher than expected, when controlled for product sales in the state [Citation20]. Furthermore, the duration of time since cannabis legalization is associated with earlier age of onset of edible use in adolescents [Citation15].
Marijuana and alcohol are the two most abused substances reported by adolescents [Citation21]. Prior to 2007, Monitoring the Future (MTF) data suggests that alcohol and marijuana use generally fluctuated in parallel; when substance use increased for one, so did the other. Since 2007, trends in reported use of these two substances have changed. While alcohol use declined markedly between 2007 and 2020, marijuana use remained steady or increased for 8th, 10th, and 12th graders [Citation21]. These findings align with the current study, which indicates a gradual decline in poison center cases for alcohol misuse/abuse over the study period with a concomitant rise in marijuana cases. While increased marijuana use may in part account for a reduction in alcohol use, it is unclear if and to what extent the reported change in marijuana leads to a change in alcohol use. These observed trends in poison-center cases mirror MTF surveillance data that indicate an ongoing decline in admitted adolescent binge drinking since the recent peaks reached in the 1990s with a concomitant ongoing rise in admitted marijuana use [Citation21].
Limitations
The National Poison Data System is dependent on voluntary reporting and the data likely underrepresents the actual number of suspected intentional misuse and abuse exposures. The AAPCC maintains the NPDS, which houses only de-identified case records of self-reported cases managed by US poison centers. NPDS data do not reflect the entire universe of exposures to a particular substance nor the opinions of the AAPCC. NPDS data should not be construed to represent the complete incidence of exposures to any substance(s). Exposure does not necessarily represent poisoning or overdose. Not all substances coded are verified by a toxicology laboratory. The accuracy and completeness of the data relies on correct coding within the NPDS database by poison center specialists. Neither AAPCC nor the individual regional poison center can completely verify the accuracy of every report. Our analysis was limited to exposure cases classified as abuse or misuse. It is possible that additional misuse or abuse cases were classified otherwise and thus were missed. Despite these limitations, NPDS data can be a valuable tool for evaluating the epidemiology of substance misuse/abuse at the national level.
Conclusion
U.S. Poison Centers reported greater than 330,000 misuse and abuse exposure cases and 450 deaths over 20 years for school-aged children and adolescents, demonstrating a substantial ongoing health impact on this vulnerable population. The substances most commonly misused/abused reflect widely available substances such as over-the-counter medications, household products and pharmaceuticals commonly prescribed to youth. Differences in age and sex were evident, with males and adolescents more likely to abuse and misuse substances. Although alcohol exposure cases have been slowly decreasing, marijuana exposure cases, especially those involving non-combustible products such as edibles and vaping products, are increasing. This trend has been most apparent in recent years in the wake of legalization and decriminalization in US cannabis laws and future research is needed to better understand how legal cannabis laws may be contributing to these trends.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Hochberg Y, Benjamini Y. More powerful procedures for multiple significance testing. Stat Med. 1990;9(7):811–818.
- Npds coding users’ manual v. 3.1. Medical outcome. Virginia: American Association of Poison Centers; 2014.
- Karami S, Major JM, Calderon S, et al. Trends in dextromethorphan cough and cold products: 2000-2015 national poison data system intentional abuse exposure calls. Clin Toxicol (Phila). 2018;56(7):656–663.
- NIDA. 2021. April 13. Sex and Gender Differences in Substance Use. Retrieved from https://www.drugabuse.gov/publications/research-reports/substance-use-in-women/sex-gender-differences-in-substance-use. on 2021, December 15.
- Boys A, Marsden J, Strang J. Understanding reasons for drug use amongst young people: a functional perspective. Health Educ Res. 2001;16(4):457–469.
- Gummin DD, Mowry JB, Beuhler MC, et al. 2019 Annual report of the American association of poison control centers’ national poison data system (NPDS): 37th annual report. Clin Toxicol (Phila). 2020;58(12):1360–1541.
- Ford JA. Misuse of over-the-counter cough or cold medications among adolescents: prevalence and correlates in a national sample. J Adolesc Health. 2009;44(5):505–507.
- Benotsch EG, Koester S, Martin AM, et al. Intentional misuse of over-the-counter medications, mental health, and polysubstance use in young adults. J Community Health. 2014;39(4):688–695.
- Vakkalanka JP, Charlton NP, Holstege CP. Epidemiologic trends in loperamide abuse and misuse. Ann Emerg Med. 2017;69(1):73–78.
- Nemanich A, Liebelt E, Sabbatini AK. Increased rates of diphenhydramine overdose, abuse, and misuse in the United States, 2005–2016. Clin Toxicol (Phila). 2021;59(11):1002–1008.
- Myran DT, Cantor N, Finkelstein Y, et al. Unintentional pediatric cannabis exposures after legalization of recreational cannabis in Canada. JAMA open-Network. 2022;5(1).
- Miech RA, Johnston LD, O’Malley PM, et al. Monitoring the future national survey results on drug use, 1975–2017: volume I, secondary school students. Ann Arbor (MI): Institute for Social Research, The University of Michigan; 2018.
- Miech RA, Johnston LD, O’Malley PM, et al. Monitoring the future national survey results on drug use, 1975–2018: volume I, secondary school students. Ann Arbor (MI): Institute for Social Research, The University of Michigan; 2019.
- Friese B, Slater MD, Battle RS. Use of marijuana edibles by adolescents in California. J Prim Prev. 2017;38(3):279–294.
- Borodovsky JT, Lee DC, Crosier BS, et al. U.S. Cannabis legalization and use of vaping and edible products among youth. Drug Alcohol Depend. 2017;177:299–306.
- Friese B, Slater MD, Annechino R, et al. Teen use of marijuana edibles: a focus group study of an emerging issue. J Prim Prev. 2016;37(3):303–309.
- Giombi KC, Kosa KM, Rains C, et al. Consumers’ perceptions of edible marijuana products for recreational use: likes, dislikes, and reasons for use. Subst Use Misuse. 2018;53(4):541–547.
- Johnson RM, Brooks-Russell A, Ma M, et al. Usual modes of marijuana consumption among high school students in Colorado. J Stud Alcohol Drugs. 2016;77(4):580–588.
- Yoo SR, Dollinger C, Vali M, et al. 2018. Perceptions of the comparative safety of different forms of marijuana use.
- Monte AA, Shelton SK, Mills E, et al. Acute illness associated with cannabis use, by route of exposure: an observational study. Ann Intern Med. 2019;170(8):531–537.
- Johnston LD, Miech RA, O'Malley PM, et al. Monitoring the future national survey results on drug use. Overview Key Findings on Adolescent Drug Use, Institute for Social Research. 2020;1975–2019.