Abstract
Objective
Poisonings contribute significantly to morbidity and mortality of patients. Some patients have numerous contacts to a poison information center, indicating repeated poisoning exposures. Information on the involved substances is necessary to explore methods to prevent self-harm and reduce mortality. The objective of this study was to characterize the patient population with repeated poison exposures in Denmark and identify the substances involved.
Methods
This study was a retrospective cohort study of enquiries to the nationwide Danish Poison Information Centre and the Danish National Patient Registry. The databases were used to identify patients with more than five individual poisoning episodes within a 12-month-period between 1 January 2013, and 31 December 2017.
Results
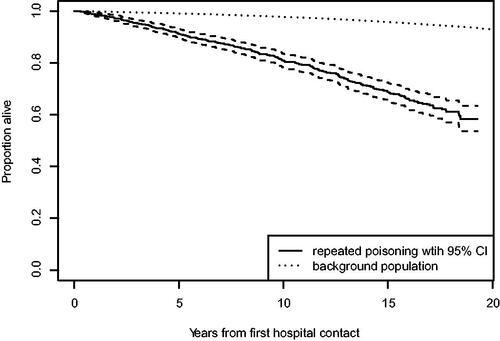
One hundred and thirty-seven patients and 995 patients met the inclusion criteria in the Danish Poison Information Centre and the Danish National Patient Registry, respectively. The majority were women (82.5% and 66.3% for the Danish Poison Information Centre and the Danish National Patient Registry cohorts, respectively). The mean age was 24.7 and 29.5 years. Psychiatric comorbidities were frequent with 74.5% and 67.0% suffering from personality disorders and 70.1% and 54.5% from affective disorders in the Danish Poison Information Centre and the Danish National Patient Registry cohorts, respectively. One thousand seven hundred and fifty-two poisoning episodes were identified in the Danish Poison Information Centre database, and the most common types of substance were ‘pharmaceuticals’ (1,420 episodes). The most common medications ingested were quetiapine, paracetamol and cyclizine. Median number of contacts to the Danish Poison Information Centre was 10. Patients with one or more poisoning episodes involving cyclizine had on average 11.4 poisoning episodes involving cyclizine. In the Danish National Patient Registry cohort 80.9% were alive after 10 years compared to 97.7% in the background population.
Conclusion and Implications
Most poisonings were intentional and occurred among younger women. Psychiatric comorbidity was frequent. Most often, pharmaceuticals were the toxic substance, mainly quetiapine, paracetamol and cyclizine. Changing the status of cyclizine from over the counter to prescription only medication, and implementing stricter rules for prescribing quetiapine, could limit future poisoning incidences.
Introduction
Worldwide, more than 700,000 people die each year of suicide, which is the fourth leading cause of death among people aged 15–29 years [Citation1]. In Denmark, suicides accounted for the death of 524 people in 2021 [Citation2]. For each suicide, there are more than 20 suicide attempts, and self-poisoning is a major concern. Both the characteristics and outcomes of unintentional and intentional poisonings vary largely between low- and high-income countries, but are a cause of major health concern worldwide, demanding intervention [Citation1,Citation3].
Patients who experience repeated poisoning episodes have an increased long-term mortality compared to their age group, and these patients often die as a result of suicides, in many cases due to a new poisoning episode [Citation4,Citation5]. Patients who suffer frequent, repeated poisoning episodes therefore cause a particular concern. Furthermore, health care costs relating to repeated hospital admissions play an important role. Characterisation of patients with repeated poisoning episodes, and the drugs ingested, could help guide implementation of preventive measures to reduce the frequency of repeated poisoning incidences in the future.
The primary aim of this study is to evaluate the characteristics of citizens with repeated poisoning incidents by analysing data from the Danish Poison Information Centre and from the Danish National Patient Register, and to characterise the individual poisoning incidents with regards to the type of exposure, cause of the incident and risk classification in the Danish Poison Information Centre.
Methods
This is a retrospective nationwide Danish study of patients with frequent repeated poisonings (defined as >5 poisoning episodes within a 12-month period). We describe demographic characteristics, outcomes and mortality of all cases identified in the Danish Poison Information Centre database from 1 January 2013 to 31 December 2017 in the Danish Poison Information Centre cohort, and from 1 January 1999 to 31 December 2017 in the Danish National Patient Register cohort.
Using the unique personal identifier (civil registration number) assigned to all Danish citizens at birth or upon immigration, the study cohorts were linked to the Danish administrative and health registries. Information concerning death, admission to hospitals with a diagnosis of drug poisoning (International Classification of Diseases 10th Danish revision (ICD-10) codes T36 to T50, T65.9, F10.0 to F19.0 and X60 to X65), and admission to an intensive care unit (ICU) during hospitalisation with a diagnosis of drug poisoning and chronic psychiatric comorbidities (see appendix) was obtained from the Danish National Patient Register and the Cause of Death Register. The Danish National Patient Register contains information about admission data and discharge diagnosis classified according to ICD-10, while the Cause of Death Register records the causes and dates of all deaths in Denmark. For both cohorts, information about the hospital department the patient was admitted to, referral diagnosis, action diagnosis, other diagnoses, date, and time of hospital admission were obtained from the Danish National Patient Register while information about cause of death and date of death was obtained from the Cause of Death Register. Registration of ICD-10 diagnoses in the Danish National Patient Register began in 1999, and permission to access data in the register for this research was granted in 2017, thereby defining the time frame for the Danish National Patient Register cohort. The Danish Poison Information Centre database was updated in 2013 to include more data and make it easier to extract data for research. The same end date as the Danish National Patient Register cohort (31 December 2017) was chosen for the Danish Poison Information Centre cohort, thereby defining the inclusion period for the Danish Poison Information Centre cohort [Citation6–10].
Danish Poison Information Centre cohort
Poison information centres have been established to advise on and assist with the prevention, diagnosis, and management of poisonings. The Danish Poison Information Centre is a nationwide centre serving the total population of Denmark, Greenland, and the Faroe Islands (approximately 6 million people). The Danish Poison Information Centre provides 24-h guidance for the public and for healthcare professionals regarding the diagnosis and management of acute poisonings. The Danish Poison Information Centre records all enquiries systematically allowing for accurate registration of information (e.g., type of exposure, substances, cause of incident and risk classification) that is not available in the national health registries. From the Danish Poison Information Centre, we obtained complete demographic information about patient characteristics (civil registration number, date, age, gender), number of poisoning episodes within the study period, risk assessment, name of substance ingested (e.g., drug name), type of ingestion (i.e., medication, alcohol, recreational drugs or other), reason for poisoning and whether the ingested drug was part of the patient’s medication list. The reasons for ingestion were divided into six categories: suicide attempt, abuse, recreational, incorrect use/unintentional, unknown, and other. These six categories were grouped into “intentional” poisonings (suicide attempt and abuse), “unintentional” (recreational and incorrect use) and “unclear” (unknown and other). Severity of a poisoning episode was evaluated by the Danish Poison Information Centre personnel when contact to the Danish Poison Information Centre was made regarding a poisoning episode. The severity of the poisoning episode was based on type of drug and amount ingested, and the Danish Poison Information Centre personnel assessed expected patient outcome if a patient was not treated and classified the incidents into one of two categories, either ‘mild’ or ‘severe’.
To evaluate the populations with frequent, repeated poisoning incidents we extracted information from Danish Poison Information Centre registrations and combined them with data from Danish National Patient Registry and Cause of Death Registry.
A case was defined as an individual with >5 contacts to the Danish Poison Information Centre within a 12-month period within the study period (2013–2017). All poisoning episodes in the Danish Poison Information Centre cohort were extracted into Microsoft Excel, in which data were manually processed. If several enquiries in the Danish Poison Information Centre concerning the same episode were found, they were merged into a single event. Enquiries with uncertainty of an actual ingestion of a substance were not included. The date of the first contact was used as the index date. Hospital admissions due to poisoning were defined as continuous in-hospital stays with a duration of 12 h or longer occurring up to 14 days after the index date based on data obtained from the Danish National Patient Registry. Intensive care unit treatment was defined as ICU treatment from 2 days before the index date to 14 days after and was identified using procedure codes in the Danish National Patient Registry.
Danish National Patient Registry cohort
The Danish National Patient Registry is one of the world’s oldest nationwide hospital registries. It contains health care data from the Danish population, and includes administrative data and information on diagnoses, treatments and examinations [Citation10,Citation11]. We established the Danish National Patient Registry study cohort using data from the Danish National Patient Registry and linked the study cohort to Danish administrative and health registries using the civil registration number. By extracting data from the Danish National Patient Registry and the Danish Civil Registration System [Citation12], we obtained complete information on demographic patient characteristics (civil registration number, date, age, gender), number of hospitalisations due to poisoning within the study period, chronic psychiatric comorbidity, admission to ICU, and date of death (if any). Detailed information on the individual poisoning episodes (i.e., ingested substances, severity of poisoning and reason for ingestion) was not available in the Danish National Patient Registry cohort.
Corresponding to the Danish Poison Information Centre cohort, a case was defined as an individual with >5 hospitalisations due to poisoning within a 12-month period, but within the longer study period (1999–2017). The date of the first hospital admission was used as the index date. Hospital admissions due to poisonings were defined as an admission to hospital with a diagnosis of drug poisoning (International Classification of Diseases 10th Danish revision (ICD-10) codes T36 to T50, T65.9, F10.0 to F19.0 and X60 to X65) and was identified in the Danish National Patient Registry.
Data analysis
Statistical analyses were performed using R (version 3.2.3). Continuous variables were reported as median and interquartile range (IQR). Mortality curves were calculated with the use of the Kaplan–Meier method. Patients that were still alive on 11 April 2018 (last follow-up date) were censored on this date. The expected mortality rate was calculated from the age- and gender-specific mortality rates from 1999 to 2018 obtained from StatBank Denmark.
The specific poisoning episodes in the Danish National Patient Registry were not characterised regarding type of exposure, risk classification of poisoning, cause of poisoning and substances as the level of detail in the Danish National Patient Registry does not allow for such analysis.
Results
Between 2013 and 2017, 137 unique subjects with a combined 1752 recorded enquiries were identified for patients with >5 poisonings within a 12-month period in the Danish Poison Information Centre database. Between 1999 and 2017, 995 unique subjects with a combined 19,492 hospitalisations with a diagnosis of poisoning (>5 episodes in a 12-month period) were identified in the Danish National Patient Registry cohort. The number of patients with repeated poisoning enquiries was stable over the examined five-year period (data not shown). Age, gender, and civil registration number were obtained in all cases. Demographic patient characteristics are presented in . The gender distribution in the Danish National Patient Registry was more even compared with the Danish Poison Information Centre cohort (66.3% female vs. 82.5% female). Ingestions occurred in all age groups from young infants to the elderly but occurred most frequently in young adults (i.e., 20–30 years old, see ), and the patients in the Danish National Patient Registry had a slightly higher median age (29.5 years (IQR 20.4–41.3) vs. 24.7 (IQR 19.4–37.3) in the Danish Poison Information Centre cohort). Both cohorts had a high incidence of patients with psychiatric comorbidity.
Figure 1. Age histogram highlighting the overrepresentation of patients with repeat poisoning episodes aged 15–30 years.
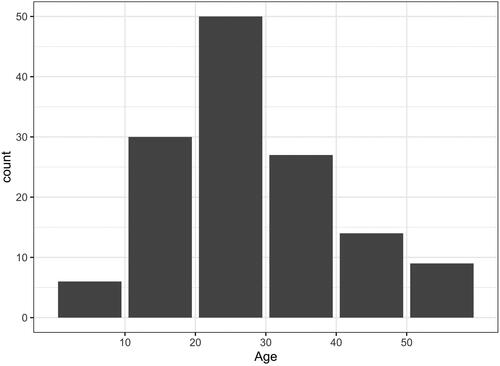
Table 1. Patient characteristics.
The number of hospitalisations due to poisoning episodes compared to number of contacts to the Danish Poison Information Centre is shown in Supplementary Figure S1. The median number of poisoning episodes for a patient in the study periods was 10 (IQR 8–15) for the Danish Poison Information Centre cohort and 14 (IQR 10–22) for the Danish National Patient Registry cohort. Data on poisoning episodes are presented in . Single-substance poisonings were far more frequent than mixed-substances poisonings, and “medications” were the predominant type of ingestion in both cohorts. The total number of ingestions exceeds the total number of poisoning episodes (1752 in the Danish Poison Information Centre cohort and 19,492 in the Danish National Patient Registry cohort, respectively) as some episodes included ingestion of multiple substance types (e.g., alcohol and medications) and are therefore registered as more than one type of ingestion. In cases when the same type of ingestion was recorded multiple times (e.g., ingestion of various medical drugs) within the same episode, the type of ingestion (e.g., “ medications”) was only counted once per episode.
Table 2. Characteristics of recorded episodes in the Danish Poison Information Centre and the Danish National Patient Registry for patients with repeated poisoning behaviour in Denmark from 2013 to 2017.
Reliable detailed data of the individual episodes (specification of ingested drug, reason for ingestion and risk assessment) were obtainable only in the Danish Poison Information Centre database. The reason for ingestion was obtained in 1694 of the episodes. Intentional poisoning, including suicide attempt (n = 1289) and abuse (n = 230) accounted for 86.7% of the cases.
In , the 20 most frequently ingested medications in the Danish Poison Information Centre cohort are listed. Quetiapine was the most frequently ingested medication (n = 258), appearing in 18% of all recorded episodes with medication ingestions. Of the six most frequently used medications, three were over the counter medications. The second and third most frequently ingested medications were paracetamol (n = 183) and cyclizine (n = 177), and the sixth most used medication was ibuprofen (n = 120). Of the medications ingested, over the counter medication accounted for more than 25% ().
Table 3. The most commonly ingested medications in patients with repeated poisoning episodes.
There did not appear to be a pattern indicating that patients with repeated poisonings episodes consistently utilise the same medication in all their poisoning episodes. Instead, different medications are used by a patient from episode to episode. In the example of patients with at least one poisoning episode involving quetiapine, the mean number of episodes with repeated episodes of ingestion of the same drug (repeated incidences of quetiapine poisoning episodes) for a patient is 3.6, while the total mean number of repeated poisoning episodes (involving any substance) for the same patient is 12.7 episodes. Notably, one exception is the group of patients with poisoning episodes involving ingestion of cyclizine, in which the average number of poisoning episodes with cyclizine was 11.1 episodes for an individual patient, compared to a total mean of 19.3 poisoning episodes with any substance in this patient group. This indicates that cyclizine is utilised repeatedly by this group in recurrent poisoning episodes.
The frequency of hospitalisation following a poisoning episode in the Danish Poison Information Centre cohort is high (frequency of hospitalisation after ingestion of a specific medication is 63%–92%, see ) and is relatively consistent across the 20 different medications. Poisoning episodes involving the use of paracetamol or cyclizine have the lowest ICU admission rates (both 1%) in the Danish Poison Information Centre cohort, while episodes involving the use of aripiprazole have the highest ICU admission rate (15%).
Mortality
Our study showed that the Danish National Patient Registry population with repeated drug poisonings had a markedly increased mortality rate compared to the age- and gender-matched background population in Denmark (). After 10 years 80.9% of the study population were alive, compared to 97.7% of the background population.
Discussion
Our aim was to show the patterns of poisoning in patients with frequently repeated poisoning episodes in Denmark by combing two separate registries–the Danish Poison Information Centre cohort (2013–2017) and the Danish National Patient Registry cohort (1999–2017). Poisonings occurred in all age groups and ranged from minor to severe and life threatening. Co-ingestions with drugs or other substances were common. The repeated ingestions predominantly occurred in young adult females with psychiatric comorbidity. More than half the patients suffered from affective disorders, primarily depression, and over two thirds of the patients were diagnosed with personality disorders, most often borderline personality disorder. One third to half the patients were diagnosed with addictive disorders, and almost half the patients were diagnosed with schizophrenia.
Another important finding is the high rate of ICU admissions for cases involving antipsychotics ranging from 7.9% (chlorprothixene) to 15% (aripiprazole). The relatively high rate of ICU admissions should raise concern and could be due to numerous factors such as high dose ingested and the severe adverse effects of ingestion of the drug. Ingestion of antipsychotic medication can be associated with hemodynamic instability, cardiac conduction disturbances, central nervous system depression, extrapyramidal effect, and sudden death. This finding is supported by a study by Toft and colleagues [Citation5], in which mortality was significantly increased with a standardised mortality ratio of 9.0 for patients poisoned with antipsychotics compared to the background population. Quetiapine ingestion of more than 1500 mg, as well as the ingestion of two or more other drugs simultaneously, have been shown to increase severity of the poisoning episode. The co-ingestion of benzodiazepines and antidepressants were associated with increased severity. Importantly, treatment of patients with acute quetiapine poisoning is symptomatic as no antidote for quetiapine currently exists [Citation13]. Another study also found increased risk of intubation when the poisoning episode involved antipsychotics or anticonvulsants [Citation14].
Poisoning episodes with medications are a major concern, and data shows a steady rise in antipsychotic related deaths since 1993 [Citation15]. In our study, quetiapine was the most frequently ingested medication and has a high hospitalisation rate (81%) and high rate of admission to the ICU (11.2%). In our study population, patients were often young adult females, and a high frequency of psychiatric comorbidities were found. This should provide important knowledge to raise awareness of these risk factors, and preventive efforts within this patient group should be prioritised. One way to target these patients could be to flag patients with more than five contacts per year, so the Danish Poison Information Centre personnel may recommend preventive measures for the patient on subsequent contacts to the Danish Poison Information Centre. Though our study was not able to show a 1-to-1 correlation between number of contacts to the Danish Poison Information Centre and hospitalisations due to poisonings, there seems to have been a trend that more contacts to the Danish Poison Information Centre was related to more hospitalisations (see Supplementary Figure S1).
Our results show a markedly increased risk of death associated with repeated poisoning episodes (see ). Limited data were previously available on the mortality for patients with repeated poisonings episodes. As mentioned, we know that patients with a poisoning episode have an increased long-term mortality, and that patients in this group that commit suicide often do so by method of self-poisoning [Citation4,Citation5]. A Dutch study [Citation16] investigated mortality and two-year survival after acute intoxications admitted to the ICU and found a mortality rate of 2.8% after one month, rising to 9.3% after two years, highlighting the severity of ICU admission after a poisoning episode. No data on specific drug groups were provided [Citation16]. A Bolivian study [Citation17] of readmissions following an admission with an acute poisoning episode found a high rate of readmissions (20.6% had at least one readmission). They found several risk factors for readmission during the first year including type of toxin (drugs of abuse), history of addiction and psychiatric history. However, they did not study mortality [Citation17]. A Norwegian study [Citation18] investigated mortality and repeated poisonings of patients with intake of drugs of abuse over a one-year period. They showed a mortality rate of 1.7% (3.4% for patients discharging themselves prematurely) [Citation18]. In our study, 80.9% of patients were alive after 10 years, compared to 97.7% in the background population, clearly demonstrating that patients with repeated poisoning episodes have markedly increased mortality.
Interestingly, our study only showed a pattern of repeated use of the same medication for patients with poisoning episodes with cyclizine. Poisoning episodes with other medications showed only few repeated episodes with the same medication. This indicates that patients with repeated poisoning episodes and contact to the Danish Poison Information Centre utilise different medications in each poisoning episode, which makes preventive efforts more difficult to implement.
Over the counter medications: the most frequent poisonings
The most frequent medications used in poisoning episodes were quetiapine, paracetamol and cyclizine. Among patients with repeated poisoning behaviour the use of over the counter medications was most common with paracetamol and cyclizine. Both types of poisonings had high rates of hospital admissions (74% and 86% respectively) and for patients poisoned with cyclizine we found evidence of repeated use of cyclizine in repeated poisoning episodes.
In 2010, the Global Allergy and Asthma European Network (GA2LEN) assessed the use of first generation antihistamines, including cyclizine. They did not support the status of first generation antihistamines as over the counter medications, especially since safer alternatives, non-sedating antihistamines, are available [Citation19]. Since 2012, there has been an increased awareness of the use of the first generation antihistamine promethazine in Denmark, and data from the Danish Poison Information Centre showed an increase in the numbers of enquiries regarding promethazine. Therefore, the legal status of promethazine was changed from an over the counter medication to a prescription only medication during the study period in 2014 [Citation20]. Even though promethazine is now classified as a prescription only medication in Denmark, the analogue first generation antihistamine cyclizine is still available in Denmark as an over the counter medication. In January 2018, the Danish Medicines Agency imposed new rules to regulate sales of cyclizine over the counter, and in April of 2022 they reduced the allowed number of doses in packages sold over the counter to 10 [Citation21,Citation22]. The indications for which first generation antihistamines can be used (e.g., insomnia, motion sickness), are rarely acute problems. Patients needing first generation antihistamines for these indications can obtain a prescription from their doctor, and safer alternatives for treating allergic reactions are widely available. Thereby, a doctor can evaluate if the patient is at risk of poisoning themselves (e.g., has risk factors shown in our study such as being a young female and having psychiatric comorbidities). Based on our findings, it would be advisable to change the status of cyclizine from an over the counter medication to a prescription only medication like the analogue first generation antihistamine promethazine.
Another interesting observation is that poisoning episodes with acetylsalicylic acid, another over the counter medication, have a much higher rate of ICU admission (10.5%) than any other over the counter medications (disregarding promethazine which changed status from an over the counter medication to a prescription only medication during the study in 2014). Episodes with acetylsalicylic acid are, however, much less frequent (38 episodes in the period 2013–2017).
In Denmark, the Danish Poison Information Centre has a close collaboration with the Danish Medicines Agency, notifying them if new trends or patterns in (mis)use of medications emerge. Results from this study could therefore be important to guide implementations of new regulations in the prescription of cyclizine. Likewise, regulations should be discussed regarding prescription of quetiapine, and specialists should be consulted on whether a closer follow up for certain patients could be recommended.
Limitations
There are some limitations to this study. The number of enquiries to the Danish Poison Information Centre only accounts for the cases of poisonings that are reported by the public or by health care professionals, and the number of hospitalisations with a poisoning diagnosis depends on correct ICD-10 procedure-coding by the clinicians. Contact to the Danish Poison Information Centre for advice is not mandatory and therefore we do not have nationwide data of all poisoned patients, e.g., patients found dead due to a suspected poisoning are not discussed with Danish Poison Information Centre. Fatal cases are not discussed or reported to the Danish Poison Information Centre. However, the validity of the Danish National Patient Registry is high [Citation11]. Number of contacts to the Danish Poison Information Centre could be affected by multiple factors, e.g., doctors or patients only contacting the Danish Poison Information Centre with rare poisonings or poisonings of special interest or concern. If some poisonings are seen frequently in the emergency department, the doctors may not feel the need to consult the Danish Poison Information Centre with each case. Some poisonings might never be reported and/or admitted to hospital (e.g., fatal cases) and the actual number might be even higher in both cohorts. Therefore, both minor poisonings and fatal cases are likely to be underreported. Additionally, several cases from the Danish Poison Information Centre cohort are probably included in the Danish National Patient Registry cohort, as there is a high frequency of hospitalisations following poisoning episodes in this cohort. These differences are highlighted by the fact that the Danish National Patient Registry cohort found more than seven times as many patients (995 patients compared to 137 patients), even though the study period for this cohort was only four times as long.
In the Danish Poison Information Centre cohort, intentional poisonings (including suicide attempts (73%) and abuse (13%)) were the main reasons for ingestion. However, the chosen category was based on the facts given by the caller, which might not always represent the true reason for the ingestion. Since health care professionals mostly call for counsel on how to treat poisonings, the actual reason for the ingestion is often not the main concern. This may explain why some people are not categorised correctly when registering reasons for ingestion. We would expect the number of intentional poisonings to be near 100% for patients with >5 poisoning episodes in a year. For these reasons, we consider age, gender, co-ingestions, and number of repeated ingestions the most reliable information regarding repeated poisonings. In contrast, reasons for ingestions are considered less reliable in our study.
Conclusions
We have shown that repeated poison ingestions most frequently occur in young adult females and that the frequency of patients with >5 poisoning episodes leading to Danish Poison Information Centre-contact within a year has been stable over the five-year period. Most often, pharmaceuticals were the toxic substance, mainly quetiapine, paracetamol, and cyclizine. Extraordinary attention should be paid to patients with repeated poisonings to reduce the risk of subsequent repeated poisoning episodes and ultimately death. Based on the presented data, we recommend changing the status of cyclizine from an over the counter medication to a prescription only medication, as well as implementing more strict rules for the prescription of quetiapine or closer follow up for patients who are prescribed quetiapine, as this may limit future poisoning incidents. Psychiatric or psychosocial assessment of patients being prescribed these medications may help to reduce the above-mentioned risks by establishing a risk for suicide and helping patients access appropriate services.
Ethical approval
According to the Danish law, ethics committee approval and informed consent were not required.
Supplemental Material
Download PDF (81.7 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- WHO Health Topics - Suicide Prevention. [cited 2022 Aug 8]. Available from: https://www.who.int/health-topics/suicide#tab=tab_1
- Suicides in Denmark. Database by Center for Suicide Research, Denmark. Website available in Danish or English, data available in Danish. [cited 2023 Jan 3] Available from: http://en.selvmordsforskning.dk/foundation-for-data/register-of-suicides/
- WHO News-Room. Fact sheets on suicide. [cited 2022 Aug 8]. Available from: https://www.who.int/news-room/fact-sheets/detail/suicide
- Lindqvist E, Edman G, Hollenberg J, et al. Long-term mortality and cause of death for patients treated in intensive care units due to poisoning. Acta Anaesthesiol Scand. 2019;63(4):500–505.
- Toft S, Horwitz H, Dalhoff KP. Long-term mortality after poisoning with antipsychotics. Clin Toxicol. 2017;55(4):267–274.
- Helweg-Larsen K. The danish register of causes of death. Scand J Public Health. 2011;39(7 Suppl):26–29.
- Schmidt M, Schmidt SAJ, Adelborg K, et al. The danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol. 2019;11:563–591.
- Thygesen LC, Daasnes C, Thaulow I, et al. Introduction to danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scand J Public Health. 2011;39(7 Suppl):12–16.
- Pottegård A, Schmidt SAJ, Wallach-Kildemoes H, et al. Data resource profile: the Danish National Prescription Registry. Int J Epidemiol. 2017;46(3):798–798.
- Lynge E, Sandegaard JL, Rebolj M. The Danish national patient register. Scand J Public Health. 2011;39(7 Suppl):30–33.
- Schmidt M, Schmidt SAJ, Sandegaard JL, et al. The Danish national patient registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490.
- Pedersen CB. The danish civil registration system. Scand J Public Health. 2011;39(7 Suppl):22–25.
- Peridy E, Hamel J-F, Rolland A-L, et al. Quetiapine poisoning and factors influencing severity. J Clin Psychopharmacol. 2019;39(4):312–317.
- Nagashima K, Hosono H, Watanabe M. Relationship between tracheal intubation and the drugs used by patients with drug overdose due to self-harm. J Pharm Health Care Sci. 2022;8(1):2.
- Handley S, Patel MX, Flanagan RJ. Antipsychotic-related fatal poisoning, England and Wales, 1993–2013: impact of the withdrawal of thioridazine. Clin Toxicol. 2016;54(6):471–480.
- Brandenburg R, Brinkman S, de Keizer NF, et al. In-hospital mortality and long-term survival of patients with acute intoxication admitted to the ICU. Crit Care Med. 2014;42(6):1471–1479.
- Muñoz Romo R, Borobia Pérez AM, Mayayo Alvira R, et al. Acute poisoning readmissions to an emergency department of a tertiary hospital. Evaluation through an active toxicovigilance program. J Clin Med. 2022;11:4508.
- Vallersnes OM, Jacobsen D, Ekeberg Ø, et al. Mortality and repeated poisoning after self-discharge during treatment for acute poisoning by substances of abuse: a prospective observational cohort study. BMC Emerg Med. 2019;19(1):5.
- Church MK, Maurer M, Simons FER, et al. Risk of first-generation H 1 -antihistamines: a GA2 LEN position paper. Allergy. 2010;65(4):459–466.
- Nyt om bivirkninger. Årgang 5 December 2014. Available from: https://laegemiddelstyrelsen.dk/∼/media/AB4629EDD76C4ECC8DA33451B897CD8A.ashx.
- Danish Medicines Agency - Ændring af udleveringsgruppe for lægemidler indeholdende cyclizin (Marzine og Gotur) fra 1. januar 2018 [cited 2022 Oct 27]. Available from: https://laegemiddelstyrelsen.dk/da/nyheder/2017/aendring-af-udleveringsgruppe-for-laegemidler-indeholdende-cyclizin-marzine-og-gotur-fra-1-januar-2018/
- Lægemiddelstyrelsen - Sløvende antihistaminer ændrer udleveringsbestemmelse og kan fra i dag kun købes på apoteket. Danish Medicines Agency. April 4th 2022. [Article in Danish]. Available from: https://laegemiddelstyrelsen.dk/da/nyheder/2022/sloevende-antihistaminer-aendrer-udleveringsbestemmelse-og-kan-fra-i-dag-kun-koebes-paa-apoteket/
Appendix
List of chronic psychiatric diagnoses evaluated in this study
Addictive disorders (F10.2 − 15.2 + 19.2).
Schizophrenia (F20), skizotypia (F21) and schizoaffective psychosis (F25).
Affective disorders (F30 − 33).
Anxiety disorders (F411 + F42).
Personality disorders (F601 − 603 + 606 + 608 + 609).
Pervasive mental developmental disorders (F84).
ADHD (F90).