Abstract
Introduction
The deliberate inhalation of volatile substances for their psychotropic properties is a recognised public health issue that can precipitate sudden death. This study aimed to describe the epidemiological characteristics and survival outcomes of patients with out-of-hospital cardiac arrests following volatile substance use.
Methods
We conducted a retrospective cohort analysis of all out-of-hospital cardiac arrest attended by the Queensland Ambulance Service over a ten-year period (2012-2021). Incidents were extracted from the Queensland Ambulance Service cardiac arrest registry, which collects clinical information using the Utstein-style guidelines and linked hospital data.
Results
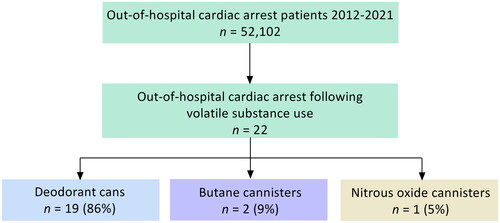
During the study period, 52,102 out-of-hospital cardiac arrests were attended, with 22 (0.04%) occurring following volatile substance use. The incidence rate was 0.04 per 100,000 population, with no temporal trends identified. The most commonly used product was deodorant cans (19/22), followed by butane canisters (2/22), and nitrous oxide canisters (1/22). The median age of patients was 15 years (interquartile range 13–23), with 14/22 male and 8/22 Indigenous Australians. Overall, 16/22 patients received a resuscitation attempt by paramedics. Of these, 12/16 were bystander witnessed, 10/16 presented in an initial shockable rhythm, and 9/16 received bystander chest compressions. The rates of event survival, survival to hospital discharge, and survival with good neurological outcome (Cerebral Performance Category 1–2) were 69% (11/16, 95% CI 41–89%), 38% (6/16, 95% CI 15–65%) and 31% (5/16, 11–59%), respectively. Eight patients in the paramedic-treated cohort that used hydrocarbon-based products were administered epinephrine during resuscitation. Of these, none subsequently survived to hospital discharge. In contrast, all six patients that did not receive epinephrine survived to hospital discharge, with 5/6 having a good neurological outcome.
Conclusion
Out-of-hospital cardiac arrest following volatile substance use is rare and associated with relatively favourable survival rates. Patients were predominately aged in their adolescence with Indigenous Australians disproportionately represented.
Introduction
Acknowledged as a significant public health issue amongst adolescent populations, volatile substance use is characterised by the intentional inhalation of a vaporous chemical to achieve a state of disinhibition and euphoria [Citation1,Citation2]. Used recreationally for their psychoactive effects, exposure to these substances can result in irreversible neurocognitive impairment and cardiac aberrancy inducing sudden out-of-hospital cardiac arrest [Citation3–5].
Volatile substance use is an umbrella term that encompasses the inhalation of a diverse group of compounds found typically in household or industrial products. The chemical structure and pharmacological properties of these substances are heterogenous in nature and unlike other classifications of drugs, are categorised by their route of administration – inhalation [Citation6]. Commonly used products include nail polish remover (acetone), deodorant/hairspray (butane), petrol (hydrocarbons) and glue/adhesives (toluene) [Citation7,Citation8]. Inhalation primary occurs through three main modalities, these being: (i) “bagging” (pouring or spraying the substance into a plastic bag; (ii) “huffing” (placing a cloth soaked in the substance over the mouth or nose); and (iii) “sniffing” (directly inhaling the substance from a container) [Citation4,Citation9,Citation10]. Unlike other recreational drugs, use peaks in adolescence, before sharply declining in adulthood as illicit substances become more readily accessible [Citation2]. In Australia, it is estimated that 4.8% of the population aged 14 years and older have used a volatile substance at least once in their life, nearly four times higher than rates of heroin use [Citation11].
Out-of-hospital cardiac arrest precipitated by volatile substance use has been reported in the medical literature since the early 1970s, with this phenomenon colloquially referred to as “sudden sniffing death syndrome” [Citation12]. The pathophysiology behind this is poorly understood, though ventricular dysrhythmias and myocardial toxicity are commonly postulated mechanisms. There is growing evidence that the inhalation of volatile substances sensitises the myocardium to circulating catecholamines, to an extent where a sudden surge in endogenous catecholamines following physical exertion or excitement may induce fatal dysythmias [Citation13]. These agents are also believed to generate malignant rhythms by precipitating conduction abnormalities such as QT interval prolongation or triggering coronary spasm [Citation5,Citation14,Citation15]. These pathways have been demonstrated to occur in the absence of chronic or repetitive exposure, with 36% of sudden deaths believed to occur in first-time users [Citation16]. Current literature on this topic is limited to hospital-based case reports and coronial death registries, with limited out-of-hospital data available [Citation17,Citation18]. Examining this patient cohort specifically may assist in identifying at risk groups, developing harm mitigation initiatives and guide clinical management strategies.
We report the epidemiological characteristics and survival outcomes of patients that experience an out-of-hospital cardiac arrest following volatile substance use. Additionally, we describe the out-of-hospital clinical management provided including the administration of epinephrine.
Methods
Study design
This is a retrospective analysis of all out-of-hospital cardiac arrests that occurred following volatile substance use attended by paramedics in Queensland over a ten-year period (1 January 2012 − 31 December 2021). The study cohort was extracted from the Queensland Ambulance Service out-of-hospital cardiac arrest registry, which prospectively records the demographic characteristics and clinical management provided to all consecutive out-of-hospital cardiac arrests attended in the state of Queensland. This study was approved by the Children’s Health Queensland Hospital and Health Service Human Research Ethics Committee (HREC/21/QCHQ/89486).
Setting
The Queensland Ambulance Service is the sole acute ambulance agency within Queensland, Australia and provides universal emergency healthcare to a population of approximately 5.3 million. Providing clinical services from 302 unique response locations, the Queensland Ambulance Service is responsible for a geographical region of 1.7 million km2. The Queensland Ambulance Service utilises a two-tier response model that consists of Advanced Care Paramedics and Critical Care Paramedics, both of which require registration with the Australian Health Practitioner Regulation Agency. When attending an out-of-hospital cardiac arrest, Advanced Care Paramedics are authorised to provide advanced life support interventions (i.e., intravenous drug administration, intravenous epinephrine and amiodarone, supraglottic airway devices) while critical care paramedics provide additional supplementary therapies (i.e., intraosseous drug administration, endotracheal intubation). Both Advanced Care Paramedics and Critical Care Paramedics can autonomously decide to withhold commencing a resuscitation attempt if any of the following circumstances are met: (i) the patient presents with obvious signs of death such as decomposition, hypostasis and/or rigor mortis; (ii) the patient presents with injuries that are incompatible with life such as decapitation, cranial destruction or incineration; (iii) commencing cardiopulmonary resuscitation (CPR) may endanger the attending paramedic; and (iv) where a lawful direction to withhold CPR is provided [Citation19]. All Queensland Ambulance Service paramedics use the corpuls3 defibrillator and monitor unit, which provides biphasic waveform electrical shocks at a fixed 200j. All Queensland Ambulance Service paramedics provide clinical care in accordance with an overarching out-of-hospital cardiac arrest clinical practice guideline which is informed by the treatment recommendations of the Australian Resuscitation Council (https://www.anzcor.org/) and International Liaison Committee on Resuscitation (https://ilcor.org/publications). Briefly, this involves an adapted standard advanced life care support regime that recommends the administration of intravenous or intraosseous epinephrine after six minutes of resuscitation and the administration of amiodarone to patients that remain in a shockable rhythm that is refractory to defibrillation.
Data sources and definitions
The Queensland Ambulance Service out-of-hospital cardiac arrest registry is a statewide, population-based database that contains 234 unique variables that are collected in accordance with the Utstein-style guidelines [Citation20]. An in-depth description of the registry has been described previously [Citation21,Citation22]. Briefly, the registry is comprised of information from various data sources which include the initial emergency call-talking process, clinical documentation detailing the circumstances of the out-of-hospital cardiac arrest and management provided during the index event, and linked hospital records. To ensure the veracity of data, information is entered into the registry by trained data-entry officers who utilise a strict coding dictionary.
In this study, out-of-hospital cardiac arrests were defined as having occurred following volatile substance use if there was clear evidence the cardiac arrest was preceded by deliberate exposure to a volatile substance. Incidents were considered to meet this criterion if the attending paramedic documented the presence of corresponding paraphernalia on scene (e.g., patient found with an open petrol container; patient found with a deodorant can and cloth material) or detailed clear circumstantial evidence indicating volatile substance use occurred immediately prior to the out-of-hospital cardiac arrest (e.g., bystander on scene stated the patient was inhaling a volatile substance before collapsing). Patients were initially flagged for inclusion in this study by text mining clinical information contained within the Queensland ambulance service out-of-hospital cardiac arrest registry. This occurred using search terms developed a priori after reviewing known cases and terminology used in published literature. An additional chart review was then performed independently by two authors (BVS, AR) to confirm the inclusion criterion was met, with complete consensus reported.
The survival outcomes of patients that received a resuscitation attempt by paramedics (paramedic-treated) were analysed, with the following variables reported: “survived event” (defined as a return of spontaneous circulation on hospital arrival), “survived to hospital discharge” (defined as discharged alive following the hospital episode of care), and “survived with good neurological outcome” (defined as a Cerebral Performance Category score of 1-2 on discharge). Patients of Aboriginal and/or Torres Strait Islander heritage were described as Indigenous Australians [Citation23]. Resuscitation duration was defined as the period between initiation of resuscitation to the achievement of sustained return of spontaneous circulation or the discontinuation of resuscitative measures [Citation24].
Statistical analysis
Categorical variables were reported as counts and percentages, while continuous variables were described as medians and interquartile range (IQR). Temporal trends of the annual prevalence rate were examined using the Cochran-Armitage test for trends. Survival rates were reported as proportions with 95% confidence intervals (CI). Crude incidence rates were calculated using the Australia Bureau of Statistics population estimates (https://www.abs.gov.au). Geographical remoteness was determined using the postcode of the address where the out-of-hospital cardiac arrest incident occurred, as defined by the Australia Statistical Geography Standard [Citation25]. Consistent with our prior work, regional and remote locations were combined and described as “rural” [Citation26]. The relative socio-economic status of the geographical area where the out-of-hospital cardiac arrest occurred was determined using the Australia Bureau of Statistics Index of Relative Socio-economic Advantage and Disadvantage. Briefly, this index defines the accessibility to material and social resources in a particular geographical area. In this study, we defined areas with an Index of Relative Socio-economic Advantage and Disadvantage decile of 9-10 as the most relatively advantaged while locations with a decile of 1-2 were considered the most disadvantaged [Citation27]. All statistical tests were two-sided, with a P value less than 0.05 considered statistically significant. All analyses were undertaken using SPSS (version 28, IBM, New York, USA).
Results
Patient characteristics
During the ten-year study period, 52,102 out-of-hospital cardiac arrests were attended of which 22 (0.04%) were identified to be volatile substance use-related. The most commonly used product was deodorant cans 19/22 (86%), followed by butane canisters (9%) and nitrous oxide canisters (5%) (). Use was predominately performed by “huffing” (82%), with “sniffing” (14%) and “bagging” (5%) the other modalities observed. The overall incidence rate across the period of the study was 0.04 per 100,000 population, with no significant changed observed over time (P for trend = 0.752). The median age of patients was 15 years (IQR 13-23 years), with 14 (64%) males and eight (36%) Indigenous Australians. Most incidents occurred in metropolitan areas (64%), with eight (36%) occurring in areas of socioeconomic disadvantage (). Automated external defibrillators were not used on any patients prior to the arrival of paramedics. Overall, 73% (16/22) patients received a resuscitation attempt by paramedics with the remaining six patients declared deceased on arrival and presented with obvious signs of death.
Table 1. Characteristics of all patients (paramedic-attended).
Amongst the paramedic-treated cohort, 12/16 (75%) were bystander witnessed, 10/16 (63%) presented with an initial shockable rhythm (ventricular fibrillation/tachycardia), and nine (56%) received bystander CPR. The median response time to these patients was 6 min (IQR 4–8 min), while the median resuscitation duration was 19 min (IQR 10–36). Epinephrine was administered to 10 (63%) patients, with the median dose provided 5 mg (IQR 0-1mg). Two patients (12.5%) were administered amiodarone during resuscitation. Physical exertion immediately prior to the cardiac arrest was witnessed by bystanders present on scene for six (38%) patients. This included four patients who were observed to run a short distance before collapsing and two patients who were involved in a physical altercation ().
Table 2. Characteristics of paramedic-treated cohort of patients.
Survival outcomes
For patients in the paramedic-treated cohort, the rates of event survival, survival to hospital discharge and survival with good neurological outcome were 69% (11/16, 95% CI 41–89%), 38% (6/16, 95% CI 15–65%) and 31% (5/16, 11–59%) respectively. Patients that survived to hospital discharge had a shorter median duration of resuscitation in comparison to patients who died (11 min vs 26 min). Amongst the paramedic-treated cohort, eight patients that used hydrocarbon-based products were administered epinephrine during resuscitation. Of these none survived to hospital discharge. In contrast, all patients who did not receive this therapy (6) survived to hospital discharged, and 5/6 survived with good neurological outcome.
Discussion
Out-of-hospital cardiac arrest following volatile substance use appears to be rare, representing 0.04% of all paramedic-attended cardiac arrests in Queensland over the ten-year study period. Patients that experienced these events were predominately male and aged in their adolescence, with Indigenous Australians disproportionately overrepresented. Although Indigenous Australians represent approximately 5% of the general population in our jurisdiction, they comprised 36% of the study cohort [Citation28]. Rates of volatile substance use are known to be inordinately high amongst this cohort and is believed to be influenced by a myriad of psychosocial factors [Citation29]. Consequently, the overrepresentation of Indigenous Australians in our study reinforces the ongoing requirement for robust data collection and evidence-informed primary prevention strategies
The majority of patients in our study received a resuscitation attempt by paramedics with surprisingly favourable survival outcomes observed. In patients who received resuscitative measures, 69% survived the index event with 38% subsequently surviving to hospital discharge. Notably, 31% of patients were discharged from hospital with a favourable neurological outcome. This suggests that patients who experience an out-of-hospital cardiac arrest following volatile substance use are a highly salvageable cohort that are responsive to resuscitative measures. These favourable survival outcomes are likely attributable to a high proportion of patients (63%) presenting in an initial rhythm amenable to defibrillation which is acknowledged as the strongest predictor of survival following an out-of-hospital cardiac arrest [Citation30,Citation31]. Additionally, a high number of these events were witnessed by a bystander (75%) and subsequently received bystander CPR (56%). Early recognition of a cardiac arrest and the commencement of bystander-initiated resuscitation are key components of the chain of survival and are known determinants of survival [Citation32–34]. In our jurisdiction, it is estimated that approximately 70% of the adult population have received some form of training in basic resuscitation [Citation35]. Given the relatively young age of patients, it can also be assumed the prevalence of significant comorbidities were low which may also have attributed to the high survival rates.
As prior literature on this patient cohort is limited to hospital-based case reports, comparison of survival outcomes and epidemiological characteristics are not possible. With consideration to the Utstein template, patients that deteriorate into out-of-hospital cardiac arrest following volatile substance use can be considered a unique subset of the “overdose” aetiology classification. Briefly, this category is used to encompass cardiac arrests that occur following the deliberate or unintentional overdose of prescribed medications, recreation drugs or ethanol [Citation20]. In a recently published meta-analysis, the pooled survival with a favourable neurological outcome for patients that experience an out-of-hospital cardiac arrest precipitated by drug overdose was 6%, nearly five-times lower than results reported in our study [Citation36]. This significant discordance may be explained by the underlying mechanism of action of the substances involved. The vast majority of cardiac arrests that occur secondary to drug overdoses involve opioids or synthetic derivatives which induce respiratory depression and progressive hypoxaemia [Citation37]. Consequently, these patients predominately present in a non-shockable rhythm, a discernible difference to the cohort we report and likely explains the differences in survival rates.
Interestingly, we report that patients who used hydrocarbon-based products and received epinephrine had lower survival rates than those who did not receive this therapy. Previous literature suggests the administration of epinephrine and other sympathomimetic drugs during resuscitation should be avoided given volatile substances hypothesised mechanism of action [Citation5,Citation13]. This recommendation is based on expert opinion and driven by the biological plausibility that further exogenous epinephrine to already sensitised myocytes may worsen cardiac dysfunction [Citation17]. To date, we are unaware of any prior research that has reported on the utility of epinephrine in this patient cohort. We believe our results provide weak evidence that epinephrine should be withheld to these patients, though acknowledge the limitation of observational data that is prone to resuscitation time bias [Citation38]. This can result in interventions that are provided during cardiac arrest being biased towards a negative treatment effect. In this study, patients that responded to defibrillation were not administered epinephrine and consequently the provision of this drug infers a prolonged period of resuscitation which likely contributes to the negative association with survival that is reported [Citation39]. We recommend further research is undertaken to confirm these findings.
Aerosol deodorant cans were the predominant used product and were implicated in 86% of the out-of-hospital cardiac arrests reported. Comprised of organic hydrocarbons compounds which are used for their propellant effect, deodorant cans are a common household product that can be readily purchased at most supermarkets or general retailers. In comparison, other household and industrial products were rarely used by patients in our study, with butane canisters and nitrous oxide canisters involved in just two and one cases, respectively. As these products can only be purchased from select specialty stores or online through the internet in our jurisdiction, it is possible that the low number of out-of-hospital cardiac arrests we observed involving these products may be due to the reduced accessibility rather than a reflection of their perceived lethality when used. In a recent analysis of the national coronial death registry, aerosol propellants were reportedly attributable to only 13% of all volatile solvent use-related fatalities [Citation18]. Interestingly, cigarette lighter canisters and petrol (gasoline) were responsible for the majority of deaths reported to the national coronial service, however neither of these products were misused by patients in our cohort. The discordance between our results and the findings of this study may be the result of supply disruption and production modification strategies that have been enacted in our jurisdiction in comparison to other states and territories in Australia. In a number of communities in Queensland, low aromatic fuel has been introduced which has resulted in a significant reduction in petrol misuse [Citation40].
The overall incident rate of out-of-hospital cardiac arrest due to volatile substance use has remained unchanged over the ten-year study period. While this is a positive finding, we believe further harm mitigation actions are required to minimise the likelihood of future events. An often-overlooked element of ameliorating out-of-hospital cardiac arrest survival is implementing targeted strategies to prevent the index event from occurring [Citation41]. We believe this is particularly pertinent for this cohort of patients given these events occur secondary to preventable misadventure. In our jurisdiction, it is currently a criminal offence for a vendor to sell a potentially harmful volatile substance to another individual if they believe the individual intends to inhale or ingest the product [Citation42]. This has resulted in aerosol deodorant cans being stored in locked cabinets in retail stores that are located in areas that are known to have high rates of volatile substance use [Citation43]. Implementing strategies to reduce misappropriation and consequently minimise the likelihood of further out-of-hospital cardiac arrest that occur secondary to this require a multifaceted and targeted response by the broader healthcare system.
This study should be interpreted in the context of the following limitations. Chiefly, the unavoidable methodological constraints associated with the retrospective study design. Additionally, as incidents were identified for inclusion by text mining the clinical documentation of paramedics completed for purposes other than research, it is possible some incidents may have been inadvertently excluded or under-reported. As this study does not include linked post-mortem toxicology results or autopsy reports, the concordance between incidents included and national coronial datasets cannot be quantified. The findings reported in this study are limited by the small sample size which has prohibited more sophisticated analysis being performed. We intend to address this in future works through collaborating with other ambulance services.
Conclusion
Out-of-hospital cardiac arrest following volatile substance use is a rare event that is associated with relatively favourable survival outcomes when out-of-hospital resuscitation is performed. Patients were predominately aged in their adolescence with Indigenous Australians disproportionately represented. Targeted public education and risk mitigation initiatives may assist in preventing future out-of-hospital cardiac arrests secondary to this cause.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Alunni V, Gaillard Y, Castier F, et al. Death from butane inhalation abuse in teenagers: two new case studies and review of the literature. J Forensic Sci. 2018;63(1):330–335. doi: 10.1111/1556-4029.13520.
- Sironi L, Amadasi A, Zoja R. Recreational inhalation of butane and propane in adolescents: two forensic cases of accidental death. Forensic Sci Int. 2016;266:52–58.
- Bowen S. Two serious and challenging medical complications associated with volatile substance misuse: sudden sniffing death and foetal solvent syndrome. Subst Use Misuse. 2011;46(sup1):68–72. doi: 10.3109/10826084.2011.580220.
- Dell C, Gust S, MacLean S. Global issues in volatile substance misuse. Subst Use Misuse. 2011;46(sup1):1–7. doi: 10.3109/10826084.2011.580169.
- Ford J, Sutter M, Owen K, et al. Volatile substance misuse: an updated review of toxicity and treatment. Clin Rev Allergy Immunol. 2014;46(1):19–33. doi: 10.1007/s12016-013-8371-1.
- Balster RL, Cruz SL, Howard MO, et al. Classification of abused inhalants. Addiction. 2009;104(6):878–882. doi: 10.1111/j.1360-0443.2008.02494.x.
- Konghom S, Verachai V, Srisurapanont M, et al. Treatment for inhalant dependence and abuse (review). Cochrane Database Syst Rev. 2010;(12):CD007537. doi: 10.1002/14651858.CD007537.pub2.
- Lubman DI, Hides L, Yucel M. Inhalant misuse in youth: time for a coordinated response. Med J Aust. 2006;185(6):327–330. doi: 10.5694/j.1326-5377.2006.tb00588.x.
- Baydala L. Inhalant abuse. Paediatr Child Health. 2010;15(7):443–454.
- Lubman DI, Yucel M, Lawrence AJ. Inhalant abuse among adolescents: neurobiological considerations. Br J Pharmacol. 2008;154(2):316–326. doi: 10.1038/bjp.2008.76.
- Australian Institute of Health and Welfare. National drug strategy household survey 2019. Canberra, Australia; 2023 [cited 2023 Sep 15]. Available from: https://www.aihw.gov.au/reports/illicit-use-of-drugs/national-drug-strategy-household-survey-2019/contents/summary.
- Bass M. Sudden sniffing death. JAMA. 1970;212(12):2075–2079.
- Adgey AA, Johnston PW, McMechan S. Sudden cardiac death and substance abuse. Resuscitation. 1995;29(3):219–221. doi: 10.1016/0300-9572(95)00854-m.
- Beckley J, Woodward J. Volatile solvents as drugs of abuse: focus on the cortico-mesolimbic circuity. Neuropsychopharmacology. 2013;38(13):2555–2567. doi: 10.1038/npp.2013.206.
- Cruz S, Orta-Salazar G, Gauthereau M, et al. Inhibition of cardiac sodium currents by toluene exposure. Br J Pharmacol. 2003;140(4):653–660. doi: 10.1038/sj.bjp.0705481.
- Field-Smith M, Butland B, Ramsey J, et al. Trends in death associated with abuse of volatile substances 1971–2007. St George’s University of London, Report 22, 2009; 2023 [cited 2023 May 1]. Available from: https://www.re-solv.org/wp-content/uploads/2016/02/VSA-annual-report-no22.pdf.
- Berling I, Chiew A, Brown J. Poisonings from hydrocarbon inhalant misuse in Australia. Addiction. 2023;118(7):1370–1375. doi: 10.1111/add.16166.
- Darke S, Zahra E, Duflou J, et al. Characteristics and circumstances of volatile solvent misuse-related death in Australia, 2000–2021. Clin Toxicol. 2023;61(4):260–265.
- Queensland Ambulance Service. Clinical practice guidelines – resuscitation/general guidelines. Brisbane, Queensland; 2023 [cited 2023 Jan 1]. Available from: https://www.ambulance.qld.gov.au/docs/clinical/cpg/CPG_Resuscitation_General%20guidelines.pdf.
- Perkins GD, Jacobs IG, Nadkarni VM, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the utstein resuscitation registry templates for out-of-hospital cardiac arrest: a statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Resuscitation. 2015;96:328–340. doi: 10.1016/j.resuscitation.2014.11.002.
- Schultz B, Doan T, Bosley E, et al. Prehospital study of survival outcome from out-of-hospital cardiac arrest in ST-elevation myocardial infarction in Queensland, Australia (the PRAISE study). Eur Heart J Acute Cardiovas Care. 2021;10(6):616–623.
- Schultz B, Rolley A, Doan T, et al. Epidemiology of out-of-hospital cardiac arrests that occur secondary to chemical asphyxiants: a retrospective series. Resuscitation. 2022;175:113–119. doi: 10.1016/j.resuscitation.2022.03.019.
- Queensland Health. Terminology guide for the use of ‘First Nations’ and ‘Aboriginal’ and Torres Strait Islander’ references. Brisbane, Australia; 2023 [cited 2023 Jan 7]. Available from: https://www.health.qld.gov.au/__data/assets/pdf_file/0031/147919/terminology.pdf.
- Park S, Lee S, Han K, et al. Optimal cardiopulmonary resuscitation duration for favourable neurological outcome after out-of-hospital cardiac arrest. Scand J Trauma Resusc Emerg Med. 2022;30(1):5. doi: 10.1186/s13049-022-00993-8.
- Australian Bureau of Statistics. The Australian Statistical Geography Standard (ASGS) remoteness structure 2021. Canberra, Australia; 2021 [cited 2023 Jan 4]. Available from: https://www.abs.gov.au/statistics/standards/australian-statistical-geography-standard-asgs-edition-3/jul2021-jun2026/remoteness-structure.
- Doan T, Schultz B, Rashford S, et al. Surviving out-of-hospital cardiac arrest: the important role of bystander interventions. Australas Emerg Care. 2020;23(1):47–54. doi: 10.1016/j.auec.2019.12.003.
- Australian Bureau of Statistics. Census of population and housing: Socio-Economic Indexes For Areas (SEIFA). Canberra, Australia; 2016 [cited 2022 Dec 29]. Available from: https://www.abs.gov.au/ausstats/[email protected]/mf/2033.0.55.001.
- Australian Bureau of Statistics. Queensland: aboriginal and Torres Strait Islander population summary. Canberra, Australia; 2022 [cited 2023 Feb 8]. Available from: https://www.abs.gov.au/articles/queensland-aboriginal-and-torres-strait-islander-population-summary#population.
- Marel C, Maclean S, Milford R. Review of volatile substance use among Aboriginal and Torres Strait Islander people. Australia Indigenous Health Reviews; 2016 [cited 2023 May 1]. Available from: https://vsu.mhc.wa.gov.au/media/1281/aihr-1.pdf.
- Majewski D, Ball S, Bailey P, et al. Long-term survival among OHCA patients who survive to 30 days: does initial arrest rhythm Remina a prognostic determinant? Resuscitation. 2021;162:128–134. doi: 10.1016/j.resuscitation.2021.02.030.
- Soholm H, Hassager C, Lippert F, et al. Factors associated with successful resuscitation after out-of-hospital cardiac arrest and temporal trends in survival and comorbidity. Ann Emerg Med. 2015;65(5):523–531.
- Hessulf F, Bhatt DP, Engdahl J, et al. Predicting survival and neurological outcome in out-of-hospital cardiac arrest using machine learning: the SCARS model. EBioMedicine. 2023;89:104464. doi: 10.1016/j.ebiom.2023.104464.
- Al-Dury N, Ravn-Fischer A, Hollenberg J, et al. Identifying the relative important of predictors of survival in out of hospital cardiac arrest: a machine learning study. Scand J Trauma Resusc Emerg Med. 2020;28(1):60. doi: 10.1186/s13049-020-00742-9.
- Sasson C, Rogers M, Dahl J, et al. Predictors of survival from out-of-hospital cardiac arrest a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3(1):63–81. doi: 10.1161/CIRCOUTCOMES.109.889576.
- Franklin RC, Watt K, Aitken P, et al. Characteristics associate with first aid and cardiopulmonary resuscitation training and use in Queensland, Australia. Prehosp Disaster Med. 2019;34(2):155–160. doi: 10.1017/S1049023X19000104.
- Alqahtani S, Nehme Z, Williams B, et al. The incidence and outcomes of out-of-hospital cardiac arrest precipitated by drug overdose: a systematic review and meta-analysis. Resuscitation. 2019;134:10–18. doi: 10.1016/j.resuscitation.2018.12.020.
- Dezfulian C, Orkin AM, Maron BA, et al. Opioid-associated out-of-hospital cardiac arrest: distinctive clinical features and implications for health care and public responses: a scientific statement from the American Heart Association. Circulation. 2021;143(16):e836–e870. doi: 10.1161/CIR.0000000000000958.
- Andersen LW, Grossestreuer AV, Donnino MW. Resuscitation time bias – a unique challenge for observational cardiac arrest research. Resuscitation. 2018;125:79–82. doi: 10.1016/j.resuscitation.2018.02.006.
- Reynolds J, Grunau BE, Rittenberger JC, et al. Association between duration of resuscitation an favourable outcome after out-of-hospital cardiac arrest: implications for prolonging or terminating resuscitation. Circulation. 2016;134(25):2084–2094. doi: 10.1161/CIRCULATIONAHA.116.023309.
- D’Abbs P, Gillick V, Hodson S, et al. Longitudinal research into petrol sniffing and other substance abuse trends in Indigenous communities: final report. University of Queensland; 2019 [cited 2023 May 3]. Available from: https://www.niaa.gov.au/sites/default/files/publications/laf-de-identified-report-july-2019.pdf.
- Nehme Z, Smith K. It’s time to talk about the ‘prevention of resuscitation. Resuscitation. 2021;163:191–192. doi: 10.1016/j.resuscitation.2021.04.007.
- Summary Offences Act. (Queensland) s23 (1); 2015 [cited 2023 May 10]. Available from: https://www.legislation.qld.gov.au/view/pdf/inforce/current/act-2005-004.
- Nothling L. Woolworths stores lock up aerosol deodorants amid chroming concerns in Queensland. Australia Broadcasting Corporation; 2022 [cited 2023 May 10]. Available from: https://www.abc.net.au/news/2022-09-01/woolworths-locks-up-deodorant-chroming/101348190.