Abstract
Introduction
Exposure to hazardous substances in the workplace can result in injuries and fatalities. This study aimed to investigate the characteristics and trend of occupational exposures reported to the Dutch Poisons Information Centre and to investigate whether the COVID-19 pandemic had an impact on the trend.
Methods
A retrospective analysis of all acute occupational exposures reported to the Dutch Poisons Information Centre between 1 January 2016 and 31 December 2022 was performed. Data on patient and exposure characteristics, symptoms and treatment recommendations were analyzed.
Results
Between 2016 and 2022, the Dutch Poisons Information Centre received 5,508 calls regarding acute occupational exposures. The annual number of calls on acute occupational exposures almost doubled over the years studied (from 475 in 2016 to 936 in 2022). During and after the COVID-19 pandemic (March 2020-December 2022), the number of calls stabilized, but the upward trend was not significantly affected. There were an estimated 0.20 calls per 1,000 human exposure calls per month (95 per cent confidence interval: −0.14; 0.53). Victims were often exposed through multiple routes, with inhalation being the most common route (44 per cent), followed by ocular (32 per cent) and dermal contact (30 per cent). Acids (1,138 exposures) and alkalis (912 exposures) were often involved. The Dutch Poisons Information Centre had information on 6,334 patients, although the total number of exposed patients was not known as some victims did not seek medical assistance, or were treated by healthcare professionals who did not consult our Centre. At the time of contact, 13 per cent (n = 795) of the patients reported no symptoms, 76 per cent (n = 4,805) reported mild to moderate symptoms and 3 per cent (n = 183) reported potentially severe symptoms. Information on symptoms was missing for 9 per cent (n = 551) of the patients. Hospital observation and treatment were recommended for 5 per cent (n = 325) of the patients.
Discussion
This study highlights the necessity for poisoning prevention strategies to reduce the number of work-related incidents involving hazardous substances.
Conclusion
The continuing increase in the number of workplace incidents involving hazardous substances is of concern. A comprehensive and multidisciplinary approach should be taken to gain a full understanding of occupational exposure to hazardous substances and to identify risk factors.
Introduction
Acute or chronic exposure to hazardous substances at work is a serious public health challenge. Acute exposure often directly results in health effects, whereas in chronic exposure, health effects are often delayed. According to the International Labour Organization, more than 650,000 deaths per year worldwide are caused by exposure to hazardous substances at work. These are mostly the result of work-related diseases, such as cancers and respiratory disorders [Citation1, Citation2]. Furthermore, incidents with exposure to hazardous substances at work can cause fatal and non-fatal injuries, leading to absenteeism from work and significant health and socio-economic costs. In many countries, it is a legal requirement to report workplace incidents that result in hospitalization, permanent injury, or death [Citation3, Citation4]. In the European Union, fatal incidents at work and incidents at work resulting in more than three days of absence from work must be reported to Eurostat [Citation5]. According to the European Statistics on Accidents at Work, there were 2,886,807 non-fatal and 3,347 fatal incidents in European Union countries in 2021. Less than 4% of these incidents were classified as “poisonings and infections” (105,052 non-fatal and 176 fatal cases) [Citation6]. In 2022, the Dutch Inspectorate of the Ministry of Social Affairs and Employment investigated 2,418 notifiable occupational incidents, of which 96 (4%) involved hazardous substances [Citation7].
In occupational health surveillance, governments and labour organizations rely mainly on data on incidents that result in hospitalization, permanent injury, or death. However, this approach has a major limitation as it disregards relatively minor injuries that only require first aid treatment. As a result, the true number of acute occupational exposures to hazardous substances is likely to be much higher. To identify risk factors and fully understand the impact of occupational exposure to hazardous substances, a comprehensive approach should be taken.
Many poison centres routinely collect data on acute occupational exposures, providing valuable insight into demographic aspects, exposure characteristics (i.e., substances involved, routes of exposure), health effects and treatments. An important advantage is that poison centres also capture cases involving relatively minor injuries that are not reported to the authorities.
The aim of this study was to gain insight into the characteristics of occupational exposures to harmful substances reported to the Dutch Poisons Information Centre between January 2016 and December 2022 and to examine trends in the rate of calls. During the COVID-19 pandemic, several measures were taken to prevent the spread of the virus, including lockdown of businesses and industries. It is possible that changes in work practices influenced the rate of calls on occupational exposures. Therefore, we examined the trends in the rate of calls before and after the start of the COVID-19 pandemic (trend from January 2016 to February 2020 compared to the trend from March 2020 to December 2022.
Method
Study design and study population
The Dutch Poisons Information Centre offers a 24/7 telephone service to provide expert advice to healthcare professionals in the Netherlands on the diagnosis and treatment of patients exposed to potentially toxic substances. In a limited number of cases, the Dutch Poisons Information Centre is consulted by members of the public. In these cases, first-aid advice is given, and patients are advised to contact their physician for further medical assistance.
A retrospective analysis was performed of all cases classified as acute occupational exposures and reported to our Centre between 1 January 2016 and 31 December 2022. We defined acute occupational exposures as single or short-term exposures to dangerous substances while performing professional work. Patients with chronic occupational exposures (longer than 1 day) were excluded. Data were obtained from our database, which includes all telephone inquiries. In this database, anonymous information is recorded in a standard data format to ensure consistent data collection. For each case, the following parameters were examined: type of enquirer (such as general practitioner, emergency department, ambulance, member of the public), patient characteristics (number of patients, age, gender), exposure characteristics (route of exposure, involved substance), reported symptoms at the time of consultation, and treatment recommendations (wait-and-see policy, examination by a physician, hospital observation). The involved substances were identified using the product information provided by the enquirer. In case specific product names were known, legally supplied information on the chemical composition of hazardous products was used (Classification, Labelling and Packaging regulation) [Citation8].
Limited information is available on the total course of the health effects over time and the treatments performed after consulting the Dutch Poisons Information Centre, as no routine follow-up of all cases is performed.
Multiple inquiries regarding the same case were treated as a single inquiry. The accredited Medical Research Ethics Committee of the University Medical Centre Utrecht did not consider the Dutch Medical Research Involving Human Subjects Act to be applicable to this study.
Statistical analyses
Calculations and data analysis were performed using Microsoft Excel version 16.0 (Redmond, USA) and R Studio® version 2023.06.2 for Windows® (version R 4.2.2). Descriptive statistics, including percentages, medians, interquartile ranges, and full ranges, were used to provide an overview of patient and exposure characteristics, clinical course and treatment recommendations.
Our primary outcome was the monthly rate of inquiries on acute occupational exposures received by the Dutch Poisons Information Centre. The rate was defined as the monthly number of acute occupational exposure calls divided by the total monthly number of human exposure calls. We use a rate to exclude the possible trends that are caused by overall changes in the total number of calls to our centre.
To test the existence of an increasing trend over time or not, the data were treated as a time series, as the data may be autocorrelated, as is usually the case with observational data. We tested for the presence of an increasing trend over time using a Sieve-bootstrap Student’s t-test and a first order autoregressive process within the R package “funtimes” [Citation9]. The null hypothesis, “no trend”, was tested against the alternative hypothesis, “increasing trend.”
Subsequently, an interrupted time series analysis was used to analyze the data. We had 84 months of observations (January 2016 to December 2022), which we divided into “before” (January 2016 – February 2020) and “after” the event (March 2020-December 2022), for which the “event” was the start of the COVID-19 pandemic. We created a dummy variable for “after the event” (called “immediate change”), with a value of zero up to and including February 2020 and one thereafter. We also created a variable representing a constant increasing change over time (called “slope change”), which had a value equal to zero up to and including February 2020 and increasing value from 1 to 36 after that (we had 34 months of data “after the event”). The choice of March 2020 as the date for the start of the COVID-19 pandemic was based on the official timeline of the Dutch government [Citation10].
We searched for a suitable autoregressive integrated moving average (ARIMA) model for the data by using the auto.arima function (forecast package). We included the two variables we had created as external regressors. The autoregressive integrated moving average model assumes that once the series is stationary, by removing the trend and differentiating to remove its integrated part, it is a linear combination of shifts of observations (autoregression) and error lags (moving average). We checked the normality of the residuals and we used the Ljung-Box test (“checkresiduals” function) to assess the goodness of fit. Predictions were then made to see how the call rate would have changed if the COVID-19 pandemic had not occurred.
Results
Trends in occupational exposures reported to the Dutch Poisons Information Centre (2016–2022)
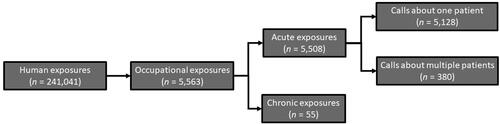
The flowchart () summarizes the total number of telephonic information requests to the Dutch Poisons Information Centre regarding human exposures over the entire study period (2016–2022), the total number of calls on occupational exposures (chronic and acute) and the number of calls on acute occupational exposures with one or more than one patient.
Figure 1. Summary of the total number of calls to the Dutch Poisons Information Centre regarding human exposures (veterinary exposures excluded) and the number of calls on chronic and acute occupational exposures over the entire study period (January 2016–December 2022).
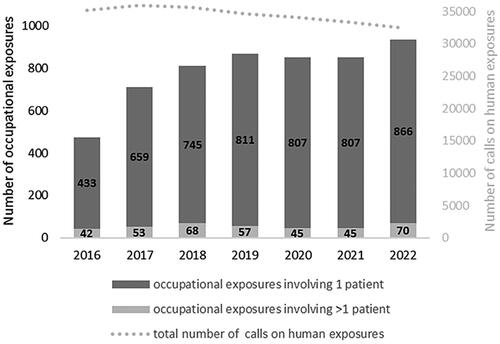
Over the 7-year study period, there was a 97% increase in the number of acute occupational exposures reported (from 475 in 2016 to 936 in 2022). There was a rise in calls regarding acute occupational exposures from 2016 to 2019, followed by a period of stabilization during the COVID-19 pandemic (2020–2021) and a further increase in 2022. In contrast, the total number of calls to the Dutch Poisons Information Centre for all categories of human exposures decreased by 8% over the same period (from 35,120 in 2016 to 32,415 in 2022) (). The monthly rate of calls on acute occupational exposures received by the Dutch Poisons Information Centre exhibited a significant increase over time (Sieve-bootstrap Student’s t-test = 10.03; P < 0.001).
Figure 2. Number of calls to the Dutch Poisons Information Centre on human exposures and acute occupational exposures per year.
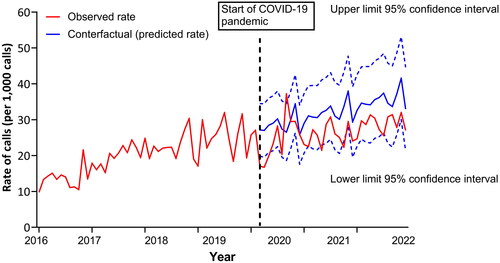
shows the result of the interrupted time series analysis. The values predicted by the autoregressive integrated moving average model based on data between January 2016 and February 2020 are compared with the observed values. With the fitted autoregressive integrated moving average model, the residuals were uncorrelated over time (Ljung-Box test: P = 0.38); the estimated immediate change in the rate was −1.71 calls per 1,000 human exposure calls per month (95% CI: −6.77; 3.35) and the estimated slope change over time was 0.20 calls per 1,000 human exposure calls per month (95% CI: −0.14; 0.53). Therefore, the analysis showed neither a significant immediate change nor a significant slope change in the rate in March 2020–December 2022 compared to January 2016–February 2020.
Figure 3. Rate of calls on acute occupational exposures (presented per 1,000 calls on human exposure). The red line represents the observed rate. The blue line represents the predicted rate (values predicted by the autoregressive integrated moving average model, including 95% confidence interval in dotted lines). Data are predicted from the start of the COVID-19 pandemic (March 2020).
Exposure characteristics (route of exposure and substances involved)
Patients were often exposed via multiple routes, most commonly involving inhalation (44%), followed by ocular (32%), dermal (30%), and oral exposures (10%). As a result, the sum of the individual percentages exceeds 100%. Parenteral exposures were also reported (3%), mainly due to needlestick injuries during vaccination or euthanasia of animals or the injection of substances under high pressure. Oral exposure was mostly limited to contact with oral mucous membranes due to splashes in the face.
There is a wide variety of substances involved in occupational accidents, and patients may be exposed to several substances. We found that acids (13%, 1,138 exposures, frequently sulfuric acid) and alkalis (11%, 912 exposures, most commonly sodium hydroxide and potassium hydroxide) were often involved in occupational exposures. Inhalation of chlorine gas, mostly formed after mixing sodium hypochlorite with acids, was also frequently reported. An overview of the most common substances involved is given in .
Table 1. Most common substances involved in occupational exposures reported to the Dutch Poisons Information Centre (January 2016 December 2022).
Demographics, clinical effects and treatment recommendations
Between 2016 and 2022, the Dutch Poisons Information Centre mainly received calls relating to a single patient (5,128). There were 380 calls relating to incidents involving more than one patient, although the exact number of exposed patients was not always known, as we were mainly called by a healthcare professional treating a specific patient. The other patients involved in the incident did not always seek medical assistance or they were treated by a healthcare professional who did not contact the Dutch Poisons Information Centre. In total, information was available on some 6,334 patients. Patients were predominantly males (64%), with a median age of 32 years (interquartile range: 20 years, full range: 13–85 years). The exact age of 2,459 patients was unknown.
The Dutch Poisons Information Centre was most commonly consulted by general practitioners (72%, 3,983 calls), followed by emergency departments (9%, 513 calls), the general public (4%, 227 calls), hospital doctors (4%, 213 calls) and ambulance services (4%, 194 calls). Occupational physicians were rarely involved (1%, 52 calls).
Because most patients had multiple routes of exposure, it is difficult to assign symptoms to a particular exposure route. Therefore, in the total number and percentage of symptoms for all routes of exposure (n = 6,334 patients), as reported to the Dutch Poisons Information Centre at the time of consultation, is presented. We were usually consulted soon after the incident took place (median 1.5 h, interquartile range 23.5 h). There is limited information on the course of the health effects over time, as the Dutch Poisons Information Centre does not routinely perform follow-up of all cases.
Table 2. Symptoms reported at the time of consultation for all routes of exposure (n = 6,334 patients).
No information on symptoms was available for 551 patients (8.7%). At the time of consultation, 13% of patients (n = 795) were asymptomatic, and 76% (n = 4,805) reported mild to moderate symptoms. Patients mainly developed effects on the skin, such as redness (8%), irritation (6%), and pain (5%) and on the eyes, such as irritation (17%), pain (5%), and decreased vision (4%). Dyspnoea (10%), cough (6%) and mucous membrane irritation (6%) were the most prevalent respiratory effects. Central nervous system effects, such as headache (10%) and dizziness (8%) and gastrointestinal effects, such as nausea (9%), pain in the mouth or throat (5%), and vomiting (4%) were also reported.
Approximately 3% of the patients (n = 183) reported potentially severe symptoms, including stridor, hypoxaemia, chemical pneumonitis, acute respiratory distress syndrome, coma, corneal damage, burns, and tissue necrosis. Corneal damage was observed in 31 patients: 11 patients were exposed to an alkali (four to sodium hydroxide), three patients to an acid (two to phosphoric acid) and three patients to an adhesive. It is unknown whether any of these patients developed permanent eye damage. Burns and tissue necrosis were reported in 77 and 48 patients, respectively. Of the patients with tissue necrosis, 19 patients were exposed to an alkali, such as sodium hydroxide (n = 8) and potassium hydroxide (n = 6), and 14 patients were exposed to an acid, such as nitric acid (n = 5) and sulfuric acid (n = 3).
Following inhalation, 14 patients experienced stridor and four developed hypoxemia. From the patients with stridor, five inhaled chlorine gas. One patient developed acute respiratory distress syndrome after inhalation of freon, and another patient developed chemical pneumonitis after inhalation of nitric acid. Detailed information on the course of the clinical effects and recovery of these patients was lacking.
Two patients were exposed to an unknown substance in a container of wood pellets. Both patients became unwell; one patient recovered after receiving oxygen, while the other died. The symptoms the patients developed could suggest carbon monoxide exposure [Citation11]. This is the only fatality reported to the Dutch Poison Information Centre during the study period.
In total, the Dutch Poisons Information Centre provided treatment recommendations for 6,092 patients. In 41% (n = 2,501) of patients, a wait-and-see approach was recommended, with instructions to contact a physician if further symptoms occurred. In 54% of patients (n = 3,266), examination by a physician was advised. Hospital observation and/or treatment were recommended in 5% of patients (n = 325).
Discussion
Between 2016 and 2022, the number of occupational exposures reported to the Dutch Poisons Information Centre nearly doubled (from 475 to 936 cases). The annual reports of the Swiss Toxicological Information Centre (Tox Info Suisse) and data from the National Poison Data System, which includes information from 55 United States poison centres, also showed an increase in the number of occupational cases during this period. The increase was less pronounced in Switzerland (from 1,017 in 2016 to 1,145 in 2022) and in the United States (from 28,041 in 2016 to 31,351 in 2022) [Citation12, Citation13].
However, the increase shown by the Dutch Poisons Information Centre, the Swiss Toxicological Information Centre and the National Poison Data System, was not uniform across all years. In response to the COVID-19 pandemic, measures were implemented to limit the spread of the virus. Economic activities were either halted or restricted. Changes in working conditions (such as working hours and location) led to an overall decrease in the number of occupational accidents reported in the European Union [Citation14] and the United States [Citation15]. Also, a decrease was observed in the number of occupational cases reported by poison centres. Compared to 2019, the number of occupational cases reported by United States poison centres decreased by 22% and 15% in 2020 and 2021, respectively [Citation12]. Over the same period, the number of acute occupational exposures reported to the Dutch Poisons Information Centre decreased by 2% (). The Swiss Toxicological Information Centre observed a decrease of about 21% (from 1,142 reports in 2019 to 907 in 2020) [Citation13]. It is unclear why the United States and Switzerland reported a greater decline in the number of occupational cases compared to our Centre. A possible explanation could be that the Dutch Poisons Information Centre is mainly consulted by healthcare professionals, whereas United States poison centres and the Swiss Toxicological Information Centre also regularly handle calls from the general public. Another possible explanation is the differences between these countries in the type of workplace measures taken to control the spread of the coronavirus (including lockdowns of businesses and industries).
An interrupted time series analysis was used to estimate the impact of the COVID-19 pandemic on the occupational poisoning rate (calls for occupational exposures as a proportion of the total number of calls for all types of human exposure). On the time plot, the rate appeared to decrease slightly at the beginning of 2020 and remained lower until 2022. However, neither the immediate nor the slope change in the rate was significant. It can, therefore, be concluded that the COVID-19 pandemic did not significantly alter the upward trend.
The underlying reasons for the continued increase in occupational exposures is unclear. However, it is possible that changes in the composition of the working population in the Netherlands, such as an increase in the number of self-employed workers and migrant workers, are contributing factors [Citation16, Citation17]. We have recently shown that important root causes of acute occupational exposures are organizational factors such as lack of work instructions and poor communication or planning, and personal factors such as disregarding work instructions, not (adequately) using personal protective equipment and personal circumstances, such as time pressure or fatigue [Citation18]. Self-employed workers may face higher workloads, potentially increasing the risk of exposure to hazardous substances. In addition, migrant workers may be at higher risk of occupational exposure due to communication difficulties, e.g., not fully understanding work instructions.
Poison centre data are a valuable source of information on the characteristics of acute exposure to hazardous substances in the workplace. This retrospective study showed that victims were often exposed by multiple routes. Inhalation (44%), ocular (32%) and dermal contact (30%) were the most common routes of exposure. A similar exposure pattern was found in another poison centre study [Citation19]. Similar to our study, other poison centre studies also show that a variety of chemical compounds are involved in occupational incidents, with acids and alkalis ranking high in the number of reported exposures [Citation20–23].
In our study, most patients developed mild to moderate health effects, with serious effects being less common. However, the current dataset does not contain detailed outcome data, and it is possible that more severe effects occurred after the call to the poison centre. Hospital observation and treatment were recommended in only 325 (5%) patients. Data from other poison centre studies also show that the majority of occupational incidents had minor to moderate outcomes [Citation23–26].
Governments and labour organizations mainly use injury statistics for health surveillance purposes, but these statistics have several limitations. First, only serious incidents (i.e., those that result in hospitalization, permanent injury or death) must be reported to the authorities, while minor injuries requiring only first aid are not included [Citation3, Citation4, Citation27]. However, small and seemingly insignificant incidents can precede major incidents. Therefore, it is important that these incidents are also taken into account in the development of risk mitigation strategies. In this study, only one fatality was reported, and the majority of the patients reported mild to moderate health effects. Consequently, the overlap between national statistics on work-related incidents and poison centre data is likely to be limited, and the data are considered complementary. Combining these data gives a more accurate picture of the true pattern of occupational accidents. A second shortcoming is the way accidents are classified in the regular European injury statistics. In particular, the classification of accidents is based on the type of injury instead of the type of accident, which makes it difficult to identify that a particular incident is related to exposure to hazardous substances. For example, burns and asphyxiation are often not classified as poisoning, even though these types of injury can be caused by exposure to a hazardous substance. This leads to a significant underestimation of the true number of occupational exposures to hazardous substances.
Our data have several limitations. First, the data are based on voluntary reports to the Dutch Poisons Information Centre, which leads to an underestimation of the true incidence of occupational exposures in the Netherlands. In addition, the Dutch Poisons Information Centre is expected to be consulted mainly for exposures that require medical attention and the expertise of a poison centre. This could lead to an under-reporting of asymptomatic cases. Third, our Centre typically does not routinely perform follow-up of all cases. As a result, there is usually limited information available about the total course of the health effects and the treatments performed after consultation. Consequently, there is a possibility that more severe effects develop later on during the intoxication. Finally, healthcare professionals consulting a poison centre often have little information about the circumstances and possible causes of the occupational incident.
Conclusion
The number of workplace incidents involving hazardous substances reported to the Dutch Poisons Information Centre has continued to increase in recent years despite a brief interruption during the COVID-19 pandemic. In contrast, the total number of calls to the Dutch Poisons Information Centre for all categories of human exposures decreased over the same period. This is concerning as these incidents may not only cause serious physical harm to workers but also may have substantial socio-economic impact. If the data presented reflect a true increase in incidents, it is imperative that measures are taken to prevent a further increase in occupational exposures in the future. A comprehensive and multidisciplinary approach is needed to gain a full understanding of occupational exposure to hazardous substances. This involves collecting information from various data sources and examining not only regular injury statistics but also exposure data. This study clearly demonstrates the value of poison centre data in examining trends and characterizing occupational exposures to harmful substances.
Data availability statement
The participants of the study did not give written consent for their personal data to be shared publicly, so supporting data are not available.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper. APG Wijnands is the first author. AM Thielman and CC Hunault are both second authors because they contributed equally to this work.
Additional information
Funding
References
- WHO. World Health Organization. At least one poison centre in each country: summary for policy makers. 25 May; 2023. https://www.who.int/europe/publications/i/item/WHO-EURO-2023-7578-47345-69489.
- ILO. 2024 International Labour Organization. Occupational Safety and Health. World Statistic. https://www.ilo.org/moscow/areas-of-work/occupational-safety-and-health/WCMS_249278/lang–en/index.htm.
- OSHA-EU. 2022 European Agency for Safety and Health at Work. https://oshwiki.osha.europa.eu/en/themes/hierarchy-prevention-and-control-measures.
- OSHA-US. 2024 Occupational Safety and Health Administration United States Department of Labor. https://www.osha.gov/.
- Regulation (EC.) No 1338/2008 of the European Parliament and of the Council of 16 December 2008 on Community statistics on public health and health and safety at work. https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A32008R1338.
- Eurostat. 2008 onwards. Accidents at work (ESAW). https://ec.europa.eu/eurostat/databrowser/view/hsw_n2_07__custom_9605686/default/table?lang=en.
- Monitor arbeidsongevallen. 2022. https://www.rijksoverheid.nl/documenten/rapporten/2023/10/05/monitor-arbeidsongevallen-2022.
- EUR-Lex. Regulation (EC.) No 1272/2008 of the European Parliament and of the Council on classification, labelling and packaging of substances and mixtures. https://eur-lex.europa.eu/eli/reg_del/2020/1677/oj.
- Lyubchich V, Gel Y, Vishwakarma S. 2023. _funtimes: Functions for Time Series Analysis_. R package version 9.1. Description available at: https://cran.r-project.org/web//packages/funtimes/funtimes.pdf. Last accessed on 16 April 2024.
- Coronavirus Tijdlijn. Rijksoverheid. https://www.rijksoverheid.nl/onderwerpen/coronavirus-tijdlijn.
- Golob N, Grenc D, Brvar M. Carbon monoxide poisoning in wood pellet storerooms. Occup Med (Lond). 2018;68(2):143–145. doi: 10.1093/occmed/kqy023.
- National Poison Data System (NPDS). Annual reports. https://www.aapcc.org/annual-reports.
- Tox Info Suisse. Annual reports. https://www.toxinfo.ch/jahresberichte_en.
- Eurostat. 2021 Statistics Explained. Accidents at work statistics. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Accidents_at_work_statistics.
- NSC Injury facts. https://injuryfacts.nsc.org/work/safety-topics/exposure-to-harmful-substances-or-environments/#:∼:text=In%202020%2C%20exposure%20to%20harmful%20substances%20or%20environments,of%20drugs%20or%20alcohol%20resulting%20in%20unintentional%20overdoses.
- Statistics Netherlands (CBS). 2023. https://www.cbs.nl/en-gb/visualisations/labour-market-dashboard.
- SEO economisch onderzoek. Arbeidsmigratie in. 2030. https://www.seo.nl/publicaties/arbeidsmigratie-in-2030/.
- Wijnands APG, de Vries I, Carlier MP, et al. Acute occupational exposures reported to the Dutch Poisons Information Center: a prospective study on the root causes of incidents at the workplace. J Occup Med Toxicol. 2023;17:19. doi: 10.1186/s12995-022-00360-4.
- Woolf A, Alpert HR, Garg A, et al. Adolescent occupational exposures. Arch Pediatr Adolesc Med. 2001;155(6):704–710. doi: 10.1001/archpedi.155.6.704.
- Litovitz T, Oderda G, White JD, et al. Occupational and environmental exposures reported to poison centers. Am J Public Health. 1993;83(5):739–743. doi: 10.2105/ajph.83.5.739.
- Downs JW, Wills BK, Cumpston KL, et al. Descriptive epidemiology of clinically significant occupational poisonings, United States, 2008–2018. Clin Toxicol (Phila). 2021;59:1259–1263. doi: 10.1080/15563650.2021.1892717.
- Schenk L, Öberg M. Comparing data from the poisons information centre with employers’ accident reports reveal under-recognized hazards at the workplace. Ann Work Expo Health. 2018;62(5):517–529. doi: 10.1093/annweh/wxy009.
- Schenk L, Feychting K, Annas A, et al. Records from the Swedish poisons information centre as a means for surveillance of occupational accidents and incidents with chemicals. Saf Sci. 2018;104:269–275. doi: 10.1016/j.ssci.2017.10.021.
- Tustin AW, Jones A, Lopez GP, et al. Occupational chemical exposures: a collaboration between the Georgia Poison Center and the Occupational Safety and Health Administration. Clin Toxicol (Phila). 2018;56(1):55–62. doi: 10.1080/15563650.2017.1338718.
- Rubenstein H, Bresnitz EA. The utility of Poison Control Center Data for assessing toxic occupational exposures among young workers. J Occup Environ Med. 2001;43(5):463–466. doi: 10.1097/00043764-200105000-00006.
- Ziqubu-Page T, Forrester MB. Adolescent workplace exposures reported to Texas poison centers. Int J Adolesc Med Health. 2018;30(3):20160057.
- Arbeidsomstandighedenwet. 2022. https://wetten.overheid.nl/BWBR0010346.
