Abstract
The associations between vaping in young people and alcohol and cannabis co-use remain understudied. The current study examined the effect of vaping frequency on past 30-day alcohol and cannabis use. Using an online survey, regular vapers (N = 1328, aged 16–24) from Canada responded to a demographic and vaping questionnaire and provided information regarding e-cigarette use and alcohol and cannabis co-use. A k-means cluster analysis was used to segment users based on vaping frequency, and a one-way MANOVA tested vaper cluster membership effects on past 30-day alcohol and cannabis use. Pairwise comparisons measured specific mean differences, and crosstabulation with Bonferroni tests examined demographic differences among clusters. Vaper cluster membership had a significant effect on past 30-day alcohol and cannabis use. Daily heavy and binge vapers had higher rates of past 30-day alcohol and cannabis use. Non-daily light vapers were less likely to share their vape and more likely to have never owned a vape. Non-daily light vapers were less likely to use high nicotine concentrations. High vaping frequency places its users at risk for higher alcohol and cannabis use and high-risk vaping behavior. Nicotine caps, among other policies, may be key in reducing high vaping frequency and its negative consequences.
Introduction
Electronic cigarette (e-cigarette) use, also known in lay language as vaping, is popular among youth and young adults (Jamal et al. Citation2017; Health Canada Citation2019a). Past 30-day use by Canadian youth (ages 16–19) increased by more than two-fold over a period of two years—from 8.4% in 2017 to 17.8% in 2019 (Hammond et al. Citation2020). Likewise, past 30-day use by young adults (ages 20–24) exhibited the same trajectory between 2017 at 6% and 2019 at 15% (Health Canada Citation2019a). A similar upward trend in vaping prevalence have been observed for youth and young adults in the US (Jamal et al. Citation2017; Miech et al. Citation2019; Hammond et al. Citation2020) and elsewhere (Bauld et al. Citation2017; Filippidis et al. Citation2017) prior to the COVID pandemic. In recent years, however, there has been a reduction in vaping prevalence (e.g. in Canada, there was a drop in 30-day prevalence for youth to 13% and 12% for young adults; Health Canada Citation2022). Research conducted during the pandemic noted a decrease in vaping frequency of nicotine-based vaping products among most young adults; however, a smaller subset of young adults vaped more frequently and a third subset did not change their frequency of vaping (Parks, Fleischer, et al. Citation2022). Overall, there is a concern regarding the disproportionately higher prevalence of vaping among youth and young adults in comparison to older adult counterparts (e.g. Health Canada Citation2022).
Although vaping is marketed as an effective smoking cessation tool, investigations into the relationship between e-cigarettes and tobacco dual use has revealed that vaping during youth and young adulthood may increase subsequent experimentation with cigarette smoking (Chatterjee et al. Citation2016; Berry et al. Citation2019; Osibogun et al. Citation2020). In a meta-analysis exploring this relationship, Soneji et al. (Citation2017) found that ever users of electronic nicotine delivery systems (ENDS) had 3.5 times higher odds of becoming cigarette smokers versus never users. This risk increased to 4.3 times higher odds for past 30-day e-cigarette users compared to non-past 30-day users (Soneji et al. Citation2017).
Beyond the dual use of e-cigarette and cigarettes, there is a growing trend of polysubstance use among vapers. Vaping devices, in particular, are commonly adapted to deliver different psychoactive, non-nicotine substances (see Breitbarth et al. Citation2018 for a review), with cannabis being the most common substance consumed (Blundell et al. Citation2018). As such, e-cigarette users have increased odds of cannabis and illicit drug use (Mehra et al. Citation2019; Bentivegna et al. Citation2021) compared to non-e-cigarette users. Findings from a national survey of American high school students found that 56% of respondents identified as triple users (e-cigarette, cigarette, cannabis) or dual users (e-cigarette, cannabis), rather than exclusive e-cigarette users (Wills et al. Citation2021). Studies have also linked vaping to problematic alcohol use in youth and young adults (Hershberger et al. Citation2016; Mehra et al. Citation2019; Parks, Maggs, et al. Citation2022). One meta-analytic study assessing the relationship between e-cigarette use and alcohol consumption in adolescents found that e-cigarette users had 6.6 times higher odds of any alcohol use and 6.7 times higher odds of binge drinking compared to non-users (Rothrock et al. Citation2020). Some studies, such as Parks, Maggs, et al. (Citation2022) have shown that alcohol use is associated with both e-cigarette and cannabis use on days where individuals drink more than usual. In all, these studies demonstrate a reliable pattern of e-cigarette use in tandem with other psychoactive substances.
In general, these studies have primarily considered differences in dual and polysubstance use across non-vapers and vapers. However, differential patterns of polysubstance use have also been observed across various e-cigarette users based on vaping frequency. In one study, 70% of frequent e-cigarette users, defined as vaping more than 20 times over a 30-day period, reported having ever vaped cannabis compared to less than half of less frequent users (i.e. 1–19 times in 30 days; Farsalinos et al. Citation2021). In a national sample of adolescents, frequent e-cigarette users were found to be more likely than daily users to have consumed cannabis and/or alcohol in the past 30 days (Rigsby et al. Citation2019). Given the close association between vaping and polysubstance use in youth and young adults, in conjunction with differential polysubstance use patterns, additional research is needed to elucidate the relationship between frequency of vaping and polysubstance use among youth and young adults.
The current study
This study extends past findings by looking beyond prevalence and examining how the frequency of vaping (days vaped per week, vaping episodes per day, and puffs per episode), among regular vapers influences both alcohol and cannabis use in the past 30 days. Specifically, we clustered regular vapers by vaping frequency measures to determine whether certain groups were at higher risk of more alcohol or cannabis co-use in the past 30 days. The aim was to understand whether frequent vaping places youth and young adults at higher risk of more frequent alcohol or cannabis co-use.
Method
Data collection
Participants for this study were recruited using paid Facebook and Instagram ads that targeted the demographic of interest. Data collection for the convenience sample took place in April and May of 2020. When they engaged with the online ads, prospective participants were linked to an online Qualtrics survey (Provo, UT). All responses to the survey were collected anonymously. Ethics approval was received from Saint Mary’s University (REB #19-105).
Sample
To be eligible to participate in the survey, respondents had to be between the ages of 16 and 24 and be regular vapers (have vaped at least once a week for the past three months). Past research on e-cigarette users have used similar ‘regular vaper’ eligibility criterion (see Al-Hamdani et al. Citation2021; Davidson et al. Citation2021). The rationale behind choosing the 16–24-year-old age range was to focus on youth and young adult groups with distinctively high prevalence rates—older adolescents (16–18 years old) represent the typical age for high school students who have higher vaping prevalence rates than younger adolescents (Government of Canada 2019). Furthermore, the 20–24 age bracket represents young adults who also have specifically high vaping prevalence rates from older young adults (Government of Canada 2019).
Participants in the sample included regular vapers from Alberta, British Columbia, Manitoba, Ontario, and Saskatchewan. A sample size of N = 528 was required to detect a small effect size (Cohens F2 = 0.02) as determined by a global effect MANOVA, power = 0.95, alpha = 0.05, for four groups (four vaper clusters) and two outcomes (alcohol and cannabis use in the past 30 days). G*power was used to calculate this effect size (Faul et al. Citation2007). A total of 1328 participants completed the survey.
Survey
The first page of the survey displayed an informed consent form. If participants provided consent, they were invited to complete the survey in its entirety. Each participant was eligible to provide their email address to be entered into a prize draw to win one of five $100 gift cards, regardless of survey completion. Participants who complete the survey in its entirety were provided an additional incentive in the form of a $10 Starbucks gift card.
The survey employed several closed-ended questions. First, a series of demographic and vaping behavior-related questions were asked to characterize the sample and provide a basis for comparing the sample on these characteristics. These questions explored various participant attributes include age, gender, area of residence, employment status, vaping frequency, the use of flavors at vaping onset, sharing behavior, and the level of nicotine content used. Three further questions were asked to provide pertinent information about vaping frequency for the purpose of clustering participants into vaping groups.
Measures
The vaping frequency questions included the number of days vaped per week (‘How many days per week do you vape?’) with seven options to choose from (one day to seven days). They also included two open-ended questions with numeric validation: number of vaping episodes per day (‘On the days you vape, how many times do you use it each day?’), and the number of puffs per vaping episode (‘When taking your vape out of your pocket/purse/backpack, how many puffs do you usually take in a single sitting before putting it away?’). These questions were used in prior published research (e.g. see Al-Hamdani et al. Citation2021; Davidson et al. Citation2021).
In order to measure the effect of vaping cluster membership on substance use behavior outcomes, participants were also asked to describe their alcohol (‘In the last 30 days, on how many days did you drink any alcoholic beverage?’) and cannabis (‘In the last 30 days, on how many days did you use cannabis/marijuana?’) use over the last 30 days.
Sharing behavior was measured by asking participants (‘Have you ever offered to share your vape with someone else (even for one puff)?’) If they answered yes, then they were asked (‘How many people do you think you have shared your vape with (even for one puff)? Please enter a number only (e.g. 5))’ as an open-ended question with numeric validation. Nicotine level was measured through the question (‘How much nicotine is in the vape juice you use? This should be listed on the package’) with options: 10–20 mg/mL (1.5% nicotine strength), 35 mg/mL (3.5% nicotine strength), 50–60 mg/mL (5.0% nicotine strength), or Other (please indicate either mg/mL or nicotine strength %).
Data analysis
The three vaping frequency measures (days vaped per week, vaping episodes per day, and puffs per episode) were used in a k-means cluster analysis. Using the elbow method, we graphed the within-cluster sum of square errors on the y-axis and the cluster number on the x-axis in R (Version 3.6.2) in order to determine the ideal number of cluster groups (R Core Team 2019). According to the elbow method, a bend indicates a notable decrease in errors at which point the overall differences diminish (Tripathi et al. Citation2018). The bend occurred at four solutions and therefore a four-cluster solution [iterations 6] was chosen for analysis.
A one-way MANOVA was then used to test the effect of vaper cluster membership (four-cluster solution) on substance use in the past 30-days, and follow-up univariates analyses were conducted to determine individual cluster effects on 30-day alcohol use and 30-day cannabis use specifically. Subsequent pairwise comparisons of each were carried out using post-hoc LSD tests to compare specific mean differences between each cluster. The vaper cluster groups were then compared by demographic and vaping variables using crosstabulation tests, and any significant differences were further assessed using Bonferroni difference tests to identify cluster over or underrepresentation within each level of significant differences in demographic and vaping variables. All data analyses, except where noted, were conducted using SPSS Version 25.
Results
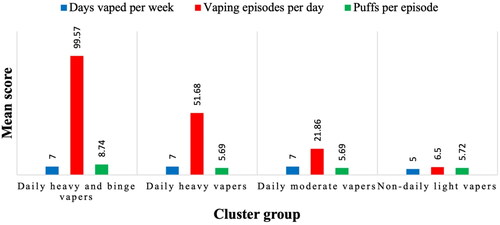
presents the results of the k-means cluster analysis. Days vaped per week, vaping episodes per day, and puffs per episode all contributed significantly to the differentiation of the groups into a four-cluster solution. The four groups generated by the k-means cluster analysis were labeled based on the means of the three vaping frequency measures within each group. displays the mean scores of each vaping frequency measure for each group. The first cluster, daily heavy and binge vapers (14.1%), was characterized by daily vaping, an exceptionally high number of vaping episodes per day, and a high number of puffs per episode. The second cluster, daily heavy vapers (15.5%), was characterized by daily vaping, a high number of vaping episodes per day, and a moderate number of puffs per episode. The third cluster, daily moderate vapers (28.7%), was characterized by daily vaping, a moderate number of vaping episodes per day, and a moderate number of puffs per episode. The fourth cluster, non-daily light vapers (41.7%), was the only group that did not vape daily and was characterized by a small number of vaping episodes per day and a moderate number of puffs per episode.
Table 1. The four-cluster solution with the main effect and mean scores for each cluster by variable.
Vaper cluster membership had a significant multivariate effect on past 30-day substance use [F (3, 1324) = 8.105, p < .001; Pillai’s Trace = 0.038, partial η2 = 0.019]. There was a significant univariate effect for vaper cluster membership on past 30-day alcohol consumption [F (3, 1272) = 12.44, p < .001, partial η2 = 0.028]. Subsequent pairwise comparisons revealed that heavy and binge vapers (M = 8.48, SE = 0.66) had a higher number of alcohol consumption days in comparison to non-daily light vapers (M = 4.81, SE = 0.38, p < .001) and daily moderate vapers (M = 6.17, SE = 0.46, p = .004), but not daily heavy vapers (M = 8.39, SE = 0.63, p = .925). Daily heavy vapers had a higher number of alcohol consumption days in comparison to non-daily light vapers and daily moderate vapers. Lastly, daily moderate vapers had a higher number of alcohol consumption days in comparison to non-daily light vapers.
Vaper cluster membership also had a significant univariate effect on cannabis use [F (3, 1272) = 4.50, p = .004, partial η2 = 0.010]. Subsequent pairwise comparisons revealed that daily heavy and binger vapers (M = 16.05, SE = 1.16) had a higher number of cannabis consumption days in comparison to non-daily light vapers (M = 11.23, SE = 0.68, p < .001), daily moderate vapers (M = 12.89, SE = 0.82, p = .025), and daily heavy vapers (M = 11.90, SE = 1.11, p = .010). No other significant differences emerged in cannabis consumption days.
reveals a comparison of the vaper clusters by demographic and vaping variables. There were no differences among vaping clusters by gender [χ2 (6, N = 1328) = 7.32, p = .292], age [χ2 (3, N = 1328) = 2.89, p = .408], the use of flavors at the onset of vaping [χ2 (3, N = 1328) = 1.65, p = .649], exposure to vaping on social media [χ2 (3, N = 1328) = 3.83, p = .281], and employment status [χ2 (3, N = 1328) = 4.63, p = .201]. However, vaping clusters did differ in sharing a vaping device with someone else [χ2 (6, N = 1328) = 36.65, p < .001]. Specifically, vapers that offered to share their vape with someone else were underrepresented among non-daily light vapers in comparison to all other groups. There was also a greater proportion of users who have never owned their own vape in the non-daily light vaper group relative to the daily heavy and daily moderate vaper groups. Vaping clusters also differed in their most sought nicotine concentration choice [χ2 (12, N = 1328) =115.73, p < .001]. The lowest vaping frequency group, non-daily light vapers, had lower proportions of users that sought high nicotine vaping products (50–60 mg/ml) relative to all the other groups.
Table 2. Cluster profile counts by demographics and vaping experiences.
Discussion
What is already known on this topic
The aim of the current study was to determine if the frequency of vaping among youth and young adults was related to the frequency of polysubstance (in particular, alcohol and cannabis) use. Past research has primarily focused on the dual-use relationship between vaping and tobacco (Blundell et al. Citation2018; Breitbarth et al. Citation2018), as well as research into the association between vaping prevalence and cannabis and illicit drug prevalence (Grant et al. Citation2019; Mehra et al. Citation2019). Findings from the past literature also presented concerns over the increased likelihood of polysubstance use among youth and young adults (e.g. Berry et al. Citation2019). This study extends on past research by demonstrating that young vapers who frequently use their products also tend to use alcohol or cannabis more often than low frequency vapers.
Main findings of this study
The current study found that engaging in daily heavy and binge vaping or daily heavy vaping is associated with a greater risk for more frequent alcohol use in the past 30 days compared to daily moderate and non-daily light vaping. This is in line with past studies that revealed an association between e-cigarette and alcohol co-use (Hershberger et al. Citation2016; Mehra et al. Citation2019; Rothrock et al. Citation2020; Parks, Maggs, et al. Citation2022). Past research has also demonstrated that a susceptibility to e-cigarettes is associated with an increased risk for alcohol use (Nicksic and Barnes Citation2019). This study builds on the existing literature by demonstrating that vaping frequency can also be used to establish risk level for alcohol consumption.
Daily heavy and binge vaping was also related to more frequent cannabis use in comparison to daily heavy vaping, daily moderate vaping, and non-daily light vaping. Our findings accord with the literature on cigarette smoking and cannabis co-use (Weinberger et al. Citation2018; Lemyre et al. Citation2019; Reboussin et al. Citation2021; Wills et al. Citation2021). Studies have found that cigarette smokers are at an increased risk of using cannabis compared to nonsmokers (Weinberger et al. Citation2018; Miech Citation2022; Parks, Maggs, et al. Citation2022), with heavy cigarette smokers being thirty-times more likely to engage in polysubstance co-use (Badiani et al. Citation2015). Likewise, our study was in line with past findings showing that vaping is associated with increased cannabis use among youth and young adults (Mehra et al. Citation2019; Nicksic and Barnes Citation2019; Bentivegna et al. Citation2021). Together, these findings suggest that policies to reduce nicotine content in vaping products may be useful in not only reducing vaping among youth and young adults, but also in reducing alcohol and cannabis use among young e-cigarette users.
What this study adds
The vaping frequency groups demonstrated two interesting differences in their vaping behavior. First, non-daily light vapers had a lower proportion of vapers who engaged in offering their devices for others to share. This suggests that non-daily vapers engage in safer vaping practices, including less device sharing and in turn less salivary and respiratory secretions, which is important to prevent communicable diseases, especially during pandemics (Majmundar et al. Citation2020). Contrarily, non-daily light vapers had a higher proportion of vapers who did not own their own devices, which suggests that they are more likely to use the devices of other vapers, but given the low percentage (under 5%) of such vapers in this group, the practice is unlikely to be detrimental.
Second, non-daily light vapers had lower proportions of high nicotine concentration use (50–60 mg/ml) in comparison to all other groups. Together, these findings suggest that lower vaping frequency is associated with safer vaping practices. The findings also emphasize the need for additional vaping control policies to protect high frequency vapers. For instance, emerging evidence suggests that capping nicotine levels in vaping products reduces the frequency of vaping among heavier vapers (Health Canada Citation2019b; Hammond et al. Citation2020). Furthermore, the findings suggest that spreading awareness about the risks of sharing devices among high frequency vapers through social marketing campaigns is crucial to reduce communicable disease spread (Tan et al. Citation2018).
Lastly, it should be important to note that this study provides further evidence for the utility of measuring regular vaping as the use of vaping devices at least once a week for a period of three consecutive months. Past research has utilized a similar definition for regular vaping to generate meaningful findings about regular vapers (Al-Hamdani et al. Citation2021; Camara-Medeiros et al. Citation2021; Conner et al. Citation2021; Davidson et al. Citation2021). For instance, Camara-Medeiros et al. (Citation2021) found that vapers who engaged in vaping behavior several times a week were found to have higher levels of perceived addiction than those who vaped less frequently. Moreover, a study by Conner et al. (Citation2021) found an association between early onset regular vaping and subsequent cigarette uptake. Furthermore, Amato et al. (Citation2017), found that vaping more than 5 days in the last 30 days was associated with continued use. This study not only supports the definitions of regular vaping used in these studies, but also extends their findings by demonstrating that regular vaping is also associated with polysubstance use.
Limitations of this study
There are at least three limitations to this paper. First, it did not use a longitudinal design to examine the trajectory of vaping, alcohol, and cannabis co-use, and which substance use commenced first, thus causation cannot be inferred (e.g. Nkansah-Amankra and Minelli Citation2016). However, the results at least suggest that high frequency vaping and alcohol and cannabis use are associated with each other. Future studies with longitudinal and controlled designs are needed to better understand the relationship between vaping, alcohol, and cannabis use. Nevertheless, the current study provides a good first step toward understanding the relationship between these substances. Second, the study recruited a convenience sample of youth and young adult vapers from Canada that were recruited using social media platforms. and the results may not be fully generalizable to this population in other regions. Despite this limitation, studies have shown consistency in vaping prevalence and motives for use (e.g. Mantey et al. Citation2017; Hammond et al. Citation2019, Citation2020; Health Canada Citation2019a), thus alleviating these concerns. Third, the study examined youth and young adults who vape at least once a week on a regular basis. Other age groups, such as older adults, have different vaping behavior patterns and preferences (e.g. Patel et al. Citation2016; Harrell et al. Citation2017). Similarly, occasional vapers may be quite distinct and exhibit a different relationship with alcohol and cannabis use. Therefore, future studies on other age groups and vapers with lower vaping frequency are important to paint a fuller picture for the relationship between vaping, alcohol, and cannabis use.
Concluding remarks
The findings of this study build on what is known about polysubstance use in young people. In particular, the results suggest that vaping frequency can be meaningfully used to cluster young vapers and consequently determine risk levels for alcohol and cannabis use. The combination of these findings and the extant literature suggests a need to consider vaping behavior when examining risk for alcohol and cannabis uptake and maintenance in youth and young adults. Given the identified associations between e-cigarette use and alcohol and cannabis co-use in young people, policies that target e-cigarettes may serve to reduce polysubstance use in this demographic.
Ethics statement
Ethics approval was received from Saint Mary’s University (REB #19-105).
Author contributions
M. Al-Hamdani secured the grant, administered the project, conceptualized the study, and led the paper. M. Al-Hamdani also wrote the majority of the initial draft and conducted the analysis. M. Davidson assisted with the initial draft and revisions for the discussion section. J. McArthur assisted with the literature review and revisions for the introduction section. All authors contributed to the revisions and response to the reviewers.
Acknowledgements
Open Access funding provided by the Qatar National Library. The authors of this study would like to thank the Heart & Stroke Foundation of Canada for providing funding for this project.
Disclosure statement
Some of the authors have past affiliations with the Lung Association of Nova Scotia and Prince Edward Island (M. Al-Hamdani and M. Davidson). There may be a perceived conflict of interest due to this affiliation.
Data availability statement
The data underlying this article cannot be shared publicly due an agreement with the Heart & Stroke Foundation of Canada that permitted data use to fulfill the objectives of the project only.
Additional information
Funding
References
- Al-Hamdani M, Hopkins DB, Hardardottir A, Davidson M. 2021. Perceptions and experiences of vaping among youth and young adult e-cigarette users: considering age, gender, and tobacco use. J Adolesc Health. 68(4):787–793.
- Amato MS, Boyle RG, Levy D. 2017. E-cigarette use 1 year later in a population-based prospective cohort. Tob Control. 26(e2):e92–e96.
- Badiani A, Boden JM, De Pirro S, Fergusson DM, Horwood LJ, Harold GT. 2015. Tobacco smoking and cannabis use in a longitudinal birth cohort: evidence of reciprocal causal relationships. Drug Alcohol Depend. 150:69–76.
- Bauld L, MacKintosh AM, Eastwood B, Ford A, Moore G, Dockrell M, Arnott D, Cheeseman H, McNeill A. 2017. Young people’s use of e-cigarettes across the United Kingdom: findings from five surveys 2015-2017. Int J Environ Res Public Health. 14(9):973–985.
- Bentivegna K, Atuegwu NC, Oncken C, DiFranza JR, Mortensen EM. 2021. Electronic cigarettes associated with incident and polysubstance use among youth. J Adolesc Health. 68(1):123–129.
- Berry KM, Fetterman JL, Benjamin EJ, Bhatnagar A, Barrington-Trimis JL, Leventhal AM, Stokes A. 2019. Association of electronic cigarette use with subsequent initiation of tobacco cigarettes in US youths. JAMA Netw Open. 2(2):e187794.
- Blundell M, Dargan P, Wood D. 2018. A cloud on the horizon–a survey into the use of electronic vaping devices for recreational drug and new psychoactive substance (NPS) administration. QJM. 111(1):9–14.
- Breitbarth AK, Morgan J, Jones AL. 2018. E-cigarettes – an unintended illicit drug delivery system. Drug Alcohol Depend. 192:98–111.
- Camara-Medeiros A, Diemert L, O'Connor S, Schwartz R, Eissenberg T, Cohen JE. 2021. Perceived addiction to vaping among youth and young adult regular vapers. Tob Control. 30(3):273–278.
- Chatterjee K, Alzghoul B, Innabi A, Meena N. 2016. Is vaping a gateway to smoking: a review of the longitudinal studies. Intern J Adolesc Med Health. 30(3):20160033.
- Conner M, Grogan S, Simms-Ellis R, Cowap L, Armitage CJ, West R, Marshall A, Siddiqi A. 2021. Association between age at first reported e-cigarette use and subsequent regular e-cigarette, ever cigarette and regular cigarette use. Addiction. 116(7):1839–1847.
- Davidson M, Al-Hamdani M, Hopkins DB. 2021. Differences in motives by personality risk profiles: examining regular youth and young adult e-cigarette users. Pers Individ Differ. 168:110352.
- Farsalinos K, Barbouni A, Niaura R. 2021. Changes from 2017 to 2018 in e‐cigarette use and in ever marijuana use with e‐cigarettes among US adolescents: analysis of the National Youth Tobacco Survey. Addiction. 116(1):139–149.
- Faul F, Erdfelder E, Lang AG, Buchner A. 2007. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 39(2):175–191.
- Filippidis FT, Laverty AA, Gerovasili V, Vardavas CI. 2017. Two-year trends and predictors of e-cigarette use in 27 European Union member states. Tob Control. 26(1):98–104.
- Government of Canada. 2019. Summary of results for the Canadian Student Tobacco, Alcohol and Drugs Survey 2018-19. Ottawa (ON): Government of Canada; [accessed 2023 Mar 9]. https://www.canada.ca/en/health-canada/services/canadian-student-tobacco-alcohol-drugs-survey/2018-2019-summary.html.
- Grant JE, Lust K, Fridberg DJ, King AC, Chamberlain SR. 2019. E-cigarette use (vaping) is associated with illicit drug use, mental health problems, and impulsivity in university students. Ann Clin Psychiatry. 31(1):27–35.
- Hammond D, Reid JL, Rynard VL, Fong GT, Cummings KM, McNeill A, Hitchman S, Thrasher JF, Goniewicz ML, Bansal-Travers M, et al. 2019. Prevalence of vaping and smoking among adolescents in Canada, England, and the United States: repeat national cross sectional surveys. Br Med J. 365:11219.
- Hammond D, Rynard VL, Reid JL. 2020. Changes in prevalence of vaping among youths in the United States, Canada, and England from 2017 to 2019. JAMA Pediatr. 174(8):797–800.
- Harrell MB, Weaver SR, Loukas A, Creamer M, Marti CN, Jackson CD, Heath JW, Nayak P, Perry CL, Pechacek PF, et al. 2017. Flavored e-cigarette use: characterizing youth, young adult, and adult users. Prev Med Rep. 5:33–40.
- Health Canada. 2019a. Canadian Tobacco and Nicotine Survey (CTNS): 2019 detailed tables; [accessed 2023 Mar 11]. https://www.canada.ca/en/health-canada/services/canadian-tobacco-nicotine-survey/2019-summary/2019-detailed-tables.html on.
- Health Canada. 2019b. Guidance on vaping products not marketed for a therapeutic use. Ottawa, (ON): Health Canada.
- Health Canada. 2022. Vaping in Canada: what we know; [accessed 2020 Mar 11]. https://www.canada.ca/en/health-canada/services/smoking-tobacco/surveys-statistics-research/vaping-what-we-know.html.
- Hershberger AR, Karyadi KA, VanderVeen JD, Cyders MA. 2016. Combined expectancies of alcohol and e-cigarette use relate to higher alcohol use. Addict Behav. 52:13–21.
- Jamal A, Gentzke A, Hu S, Cullen K, Apelberg BJ, Homa DM, King BA. 2017. Tobacco use among middle and high school students - United States, 2011-2016. MMWR Morb Mortal Wkly Rep. 66(23):597–603.
- Lemyre A, Poliakova N, Bélanger RE. 2019. The relationship between tobacco and cannabis use: a review. Subst Use Misuse. 54(1):130–145.
- Majmundar A, Allem JP, Cruz TB, Unger JB. 2020. Public health concerns and unsubstantiated claims at the intersection of vaping and COVID-19. Nicotine Tob Res. 22(9):1667–1668.
- Mantey DS, Harrell MB, Case K, Crook B, Kelder SH, Perry CL. 2017. Subjective experiences at first use of cigarette, e-cigarettes, hookah, and cigar products among Texas adolescents. Drug Alcohol Depend. 173:10–16.
- Mehra VM, Keethakumar A, Bohr YM, Abdullah P, Tamim H. 2019. The association between alcohol, marijuana, illegal drug use and current use of e-cigarette among youth and young adults in Canada: results from Canadian Tobacco, Alcohol and Drugs Survey 2017. BMC Public Health. 19(1):1208.
- Miech R, Johnston L, O'Malley PM, Bachman JG, Patrick ME. 2019. Trends in adolescent vaping, 2017-2019. N Engl J Med. 381(15):1490–1491.
- Miech RA. 2022. Adolescent cannabis users who have never smoked a combustible cigarette: trends and level of addictive drug use from 1976 to 2020. Discov Soc Sci Health. 2(1):3.
- Nicksic NE, Barnes AJ. 2019. Is susceptibility to e-cigarettes among youth associated with tobacco and other substance use behaviors one year later? Results from the PATH study. Prev Med. 121:109–114.
- Nkansah-Amankra S, Minelli M. 2016. “Gateway hypothesis” and early drug use: additional findings from tracking a population-based sample of adolescents to adulthood. Prev Med Rep. 4:134–141.
- Osibogun O, Bursac Z, Maziak W. 2020. E-cigarette use and regular cigarette smoking among youth: population assessment of tobacco and health study (2013–2016). Am J Prev Med. 58(5):657–665.
- Parks MJ, Fleischer NL, Patrick ME. 2022. Increased nicotine vaping due to the COVID-19 pandemic among US young adults: associations with nicotine dependence, vaping frequency, and reasons for use. Prev Med. 159:107059.
- Parks MJ, Maggs JL, Patrick ME. 2022. Daily fluctuations in drinking intensity: links with vaping and combustible use of nicotine and marijuana. Drug Alcohol Depend. 233:109347.
- Patel D, Davis KC, Cox S, Bradfield B, King BA, Shafer P, Caraballo R, Bunnell R. 2016. Reasons for current e-cigarette use among U.S. adults. Prev Med. 93:14–20.
- R Core Team. 2019. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; [accessed 2023 Mar 9]. https://www.R-project.org/.
- Reboussin BA, Wagoner KG, Ross JC, Suerken CK, Sutfin EL. 2021. Tobacco and marijuana co-use in a cohort of young adults: patterns, correlates and reasons for co-use. Drug Alcohol Depend. 227:109000.
- Rigsby DC, Keim SA, Adesman A. 2019. Electronic vapor product usage and substance use risk behaviors among US high school students. J Child Adolesc Psychopharmacol. 29(7):545–553.
- Rothrock AN, Andris H, Swetland SB, Chavez V, Isaak S, Pagane M, Romney J, Rothrock SG. 2020. Association of e-cigarettes with adolescent alcohol use and binge drinking-drunkenness: a systematic review and meta-analysis. Am J Drug Alcohol Abuse. 46(6):684–698.
- Soneji S, Barrington-Trimis JL, Wills TA, Leventhal AM, Unger JB, Gibson LA, Yang J, Primack BA, Andrews JA, Miech RA, et al. 2017. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 171(8):788–797.
- Tan ASL, Vaughan WR, Rodgers J, Agudile E, Sokol NA, Yie K, Sanders-Jackson A. 2018. Effects of exposure to anti-vaping public service announcements among current smokers and dual users of cigarettes and electronic nicotine delivery systems. Drug Alcohol Depend. 188:251–258.
- Tripathi S, Bhardwaj A, Poovammal, E. 2018. Approaches to clustering in customer segmentation. Int J Eng Technol. 7(3.12): 802–807.
- Weinberger AH, Pacek LR, Wall MM, Zvolensky MJ, Copeland J, Galea S, Nahvi S, Moeller SJ, Hasin DS, Goodwin RD. 2018. Trends in cannabis use disorder by cigarette smoking status in the United States, 2002–2016. Drug Alcohol Depend. 191:45–51.
- Wills TA, Leventhal AM, Sargent JD, Pagano I. 2021. Concurrent use of e-cigarettes, combustible cigarettes, and marijuana. Pediatrics. 148(4):e2021050749.