Abstract
Objective:
The purpose of this study was to adapt a diabetes nutrition education programme (NEP) developed for a primary healthcare setting for implementation in a tertiary healthcare setting. This manuscript describes the processes and considerations that were made.
Methods:
Four key steps for adapting interventions identified from the literature were used. The steps included (i) assessing the needs and logic model of change, (ii) assessing the applicability of the NEP components to the new setting, (iii) making adaptations, and (iv) planning for implementation and evaluation. In the various steps, patients and health professionals were involved mainly using qualitative methods: needs assessment (n = 28 and n = 10), making adaptations (n = 10 and n = 10) respectively, and patients (n = 5) in step four.
Findings:
Knowledge, self-efficacy and outcome expectations were identified as the main behaviour determinants in tertiary patients; therefore, the adapted NEP retained social cognitive theory as its foundation. The adapted NEP included new behaviour change techniques, particularly self-monitoring (behaviour and outcome) and vicarious learning using testimonials of successful management. The adapted NEP retained the original NEP components except the vegetable gardening demonstration. By incorporating monthly, instead of weekly group training sessions, a session for setting individual goals, provision of a workbook and additional relevant information, the adapted NEP catered for the tertiary patients’ needs.
Conclusion:
The comprehensive adaptation process involved input from key stakeholders, which increases the chances of intervention effectiveness. The adapted NEP is being implemented through a randomised controlled trial and its evaluation will illuminate the impact of the changes made to the original NEP.
Introduction
Despite diabetes being a global health problem, low- and medium-income countries experience greater mortality associated with the condition than their higher income counterparts.Citation1 Treating and managing diabetes relies heavily on lifestyle modification with or without pharmacotherapy.Citation2 This requires patients to be proficient self-managers, making self-management education critical.Citation3 Diabetes self-management education (DSME) is considered a feasible intervention as it is simple, relatively inexpensive and culturally acceptable.Citation4,Citation5
Diabetes self-management education, including nutrition education, is known to improve behaviour mediators, promote self-care, improve glycaemic control and other health outcomesCitation3 even in developing countries.Citation6,Citation7 Yet, for patients to reap the full benefits from educational encounters, the education should be offered in a structured manner.Citation8,Citation9 However, structured DSME is limited in developing countries, including those in Africa, where most structured DSME programmes are concentrated in primary care.Citation7,Citation10 In developing countries, there is a need to intensify DSME as a means to prevent or slow down diabetes complications.Citation11 Poor diabetes control, and consequent complications, is of concern at secondary and tertiary levels of health care in South Africa.Citation12,Citation13 Implementing DSME at these levels will fill the gap in structured DSME beyond primary health care.
Although there is a need to intensify DSME, developing lifestyle interventions is a complex, slow and expensive process,Citation14 which can even be more challenging in resource-limited settings such as those in sub-Saharan Africa. Using established programmes that have been proven to be effective can save time and money, while increasing the chance of achieving successful outcomes. However, implementing an existing intervention from one setting or population group to another may require adapting the intervention to meet the needs of the new population.Citation15 Programmes can be adapted by deleting or adding components, modifying existing components, changing the manner or intensity of components to account for cultural or local circumstances.Citation16
To successfully adapt evidence-based interventions, various adaptation frameworks suggest a systematic approach.Citation15–17 The starting point, according to Card et al.,Citation15 is to select a suitable effective programme, which is a challenge in developing countries since effective DSME programmes are scarce.Citation18 In South Africa, one of the few available interventions is a nutrition education programme (NEP) implemented among adults with type 2 diabetes mellitus (T2DM) in a primary setting at two community health centres.Citation19 The NEP was theory based and customised to the needs of the target population.Citation20 The programme was implemented using a randomised controlled trial (RCT) design over 12 months and comprised four components: eight-weekly group training sessions, group follow-up sessions (four monthly and two bimonthly), vegetable gardening demonstrations and take-home education materials (wall/fridge poster and pamphlet). The control group participants received the same education materials as the intervention participants with no other educational encounters. The NEP improved dietary behaviours; reduction of starchy food intake at both 6 and 12 months and energy intake at 12 months,Citation19 as well as diabetes knowledge.Citation21 This NEP is considered effective and evidence based because at least one targeted outcome, namely a critical diabetes dietary behaviour, improved and was sustained beyond six months;Citation22 additionally, HbA1C levels were reduced by a clinically meaningful margin (∼0.6%).Citation23 The improvements in HbA1c levels are comparable to other non-pharmacological interventions conducted in developing countries for preventing complications in people with T2DM.Citation6 Furthermore, participants had low attrition rates and high satisfaction with the programme and recommended that the programme be offered to other people with diabetes.Citation19,Citation24 The NEP meets most of the criteria for suitable effective intervention programmes as described by Card et al.,Citation15 including nutrition education interventions.Citation25 Thus, the NEP was considered suitable for adapting for use in people with T2DM in diverse settings, particularly in resource-limited settings. In this manuscript, the researchers report on the systematic process used to adapt the NEP from a primary healthcare setting to a tertiary healthcare setting in South Africa.
Study setting and population
The study was conducted at a diabetes outpatient clinic of a public tertiary academic hospital affiliated with a South African university. Patients seen at the diabetes clinic are usually referred from other hospitals or clinics due to poorly controlled diabetes or the presence of diabetes complications. Most patients are on insulin therapy. At the time of the study no structured diabetes education was offered to the patients. Generally, most of the education at the clinic is offered on an individual basis according to the patients’ needs, which are assessed by the physician. Patients who need lifestyle intervention are referred to hospital dietitians for further counselling. The study was approved by the Faculty of Health Sciences, Research Ethics Committee, University of Pretoria (No. 4/2016). Patients were personally recruited. Details of the study were given to potential participants and only eligible and consenting participants were included.
Methods
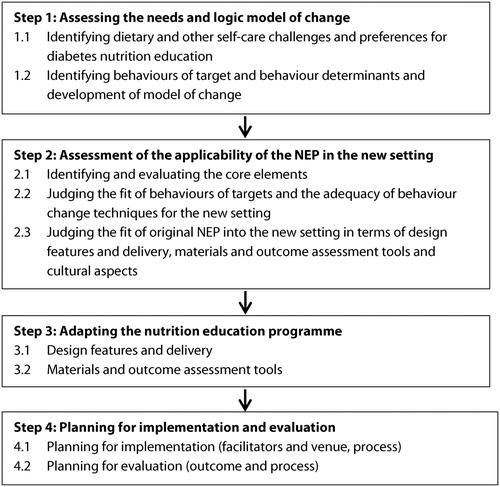
The researchers identified common key elements for adapting interventions to a new setting or population.Citation15–17,Citation26 The main steps identified and employed in this study were: (i) assessing the needs and model of change, (ii) assessment of applicability of the NEP to the new setting, (iii) making adaptations, and (iv) planning for implementation and evaluation. These steps are shown in .
Step 1: needs assessments and logic model of change
This step involved: (i) identifying dietary and other self-care challenges of T2DM patients at the tertiary healthcare setting as well as the preferences for diabetes nutrition education, and (ii) identifying the NEP target behaviours and behaviour determinants as well as developing the model of change.
Identifying dietary and other self-care challenges and preferences for diabetes nutrition education
Qualitative research was used with key stakeholders. Stakeholders comprised T2DM adults (n = 28, 40–70 years; 11 females) who had lived with diabetes for at least one year and could understand English and 10 health professionals (3 doctors, 2 nurses, 5 dietitians) who had worked with the patients for at least six months. Five focus-group discussions were held with the patients using semi-structured questions, while self-administered open-ended questions in a paper-format questionnaire obtained data from the health professionals (HPs). Researcher-designed questionnaires based on the previous NEP and relevant literature were used for the two groups of participants. Data were analysed using the thematic framework approach.Citation27 The comprehensive report of the needs assessment has been published elsewhere.Citation28
Identifying behaviours of target and behaviour determinants and development of model of change
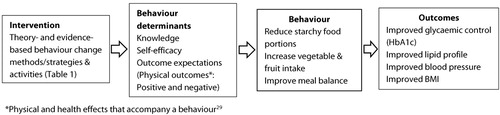
The needs assessment results and evidence from the literature were used to identify the behaviours for intervention targets and behaviour determinants. Behaviours are actions or practices or activities (risk/and or protective) which people undertake that have the potential to influence health.Citation29,Citation30 Behaviours for intervention targets are the health risk behaviours that need to be targeted in an intervention programme.Citation29 Behaviour determinants are the factors that influence the behaviours, i.e. causal factors.Citation29 The logic model of change is a graphic representation of the relationships among the intervention (strategies/activities), behaviour determinants and the intended outcomes.Citation15,Citation16 The logic model of change shows how a programme will work under certain conditions to solve identified problems.Citation15,Citation29 In this study, the logic model of change was developed to show how the theory-based change methods/strategies were proposed to influence first the determinants of behaviour, and thereafter the identified behavioural problems, i.e. intervention targets to produce the intended health outcomes ().
Step 2: assessment of the applicability of the NEP in the new setting
This step involved: (i) identifying and evaluating the core elements, (ii) judging the fit of behaviours of targets and the adequacy of behaviour change techniques for the new setting, and (iii) judging how well the original NEP fitted into the new setting in respect of design features and delivery, materials and instruments and cultural aspects.
Intervention core elements or active ingredients are critical programme components considered to make an intervention effective.Citation16,Citation31 Evidence from the literature,Citation25,Citation31 supported by qualitative evaluations of participants during implementation of the original NEP,Citation24 guided the identification of core elements. The applicability of the NEP in the new setting was assessed by combining results of the needs assessment with consultations with HPs including dietitians and doctors, and evidence from the literature. The researchers considered the main differences between the two populations or settings, and compiled a list of elements that would need to be modified.
Step 3: adapting the nutrition education programme
The researchers presented the results of the needs assessment together with the preliminary adapted NEP and education tools to eight dietitians, four of whom had participated in the needs assessment, and two doctors, both whom had participated in the needs assessment. In addition, the expert opinion of a nutrition and health education expert who evaluated the original NEP was used. A small sample of T2DM patients (n = 10), different from the needs assessment sample, was engaged in pre-testing of the education materials and outcome assessment tools.
Step 4: planning for implementation and evaluation
Planning for implementation involved: (i) identifying programme facilitators and a venue for group meetings, and (ii) piloting the process of recruitment, data collection and the first NEP session. The latter was done with a different T2DM sample (n = 5). Planning for evaluation involved planning for outcome measurements, as well as process evaluation.
Findings
Step 1: needs assessment and logic model of change
Self-care challenges and preferences for diabetes nutrition education
The results from the HPs and patients related to self-care challenges and preferences for diabetes NEP were similar in most casesCitation28 and comparable to those of the original NEP.Citation20 Briefly, regarding self-care challenges the needs assessment revealed that patients (i) experienced knowledge deficits, (ii) struggled with adhering to diet (portion control, low consumption of vegetables and fruits, inappropriate dietary choices, irregular meals, and problems with balancing diet and insulin), exercise, medication and appointment keeping, and (iii) they faced multiple barriers to self-care (financial constraints, unsupportive social and physical environments, and personal factors). They also perceived the challenges to greatly impact on their quality of life.Citation28
Regarding preferred characteristics of the NEP, the needs assessment revealed the following. Participants would prefer (i) monthly education meetings coinciding with collection of medication; (ii) content on self-discipline for lifestyle behaviours (diet and exercise), content on diabetes basics, e.g. causes and complications, healthy eating, carbohydrate distribution, glucose monitoring, management of hypoglycaemia and stress management; (iii) group education sessions; (iv) a delivery approach to enhance learning such as demonstrations, food tasting sessions and easy to understand education materials; and (v) a delivery approach that would enhance motivation and support behaviour change, for example through vicarious learning by using examples from peers and successful management testimonials. Participants also requested a competent facilitator with positive personal attributes.
Behaviours of targets, behaviour determinants and logic model of change
Following the diet challenges identified in the needs assessment, intake of vegetables and fruit, control of starchy food portions and balance in meals were identified as the behaviours of target for the adapted NEP. Improving these behaviours was deemed likely to aid glycaemic control (HbA1c), since the adapted NEP targets patients with poorly controlled diabetes.Citation32 The identified behaviours of target were also aimed to address multiple dietary challenges. For example, the researchers were of the opinion that irregular eating, which appeared to be associated with prior overeating in the target population, would potentially be dealt with through addressing starchy food portion control and meal balance.
Knowledge, self-efficacy and outcome expectations (physical outcomes), which are constructs of the social cognitive theory (SCT),Citation33 were identified as the major behaviour determinants for dietary and related self-care behaviours in the target population. Self-efficacy is defined as an individual’s confidence in being able to carry out behaviour or overcome the barriers to engage with a desirable behaviour while outcome expectations is the beliefs concerning the anticipated outcomes (positive or negative) of a person’s behaviours.Citation29,Citation33
The logic model of change that was developed () shows that the identified theory-based behaviour change techniques (BCT) and strategies () would be applied to first improve the behaviour determinants i.e. knowledge, self-efficacy and outcome expectations. Consequently, the targeted behaviours (dietary and other self-care) ought to improve glycaemic control (HbA1c) and other clinical outcomes (blood lipids, blood pressure, BMI) ().
Table 1: Behaviour change techniques based on social cognitive theory and the Health Belief Model in the original and adapted programmes
Step 2: applicability of NEP components
Identified core/effective elements and their applicability
Six elements thought to contribute to the success of the original NEP were identified. These elements possibly contributed to positive dietary behaviour by enhancing behaviour mediators, namely self-efficacy, knowledge and skills, and outcomes expectations. The elements include (i) the group delivery format,Citation34 (ii) face-to-face delivery plus provision of education materials in the form of a wall/fridge poster,Citation24,Citation35 (iii) hands-on activities and demonstrations,Citation36 (iv) cultural appropriateness of the NEP,Citation36,Citation37 (v) follow-up intervention,Citation35 and (vi) the use of multiple BCT evidenced to change dietary behaviour.Citation38 All of these elements could be carried over into the new setting.
Behavioural determinants and change strategies fit
Behaviour change targets, behaviour determinants and BCT, and strategies of the original NEP were found to be applicable to the new setting. However, additional BCT and strategies were deemed necessary in order to enhance the existing ones in meeting the needs of patients in the new setting ().
SCT was retained as the major theory underpinning the adapted NEP. In addition, ‘cues to action’, a construct of the Health Belief Model,Citation39 was maintained since the take-home education materials were meant to serve as constant reminders of desirable behaviours. summarises the details of the BCT/strategies used in the original NEP and the additional ones for the adapted programme.
Design features, delivery, materials and instruments and cultural fit
Design features and delivery
The original NEP components, including curriculum training sessions, follow-up sessions, take-home education materials and food tasting sessions were suitable for the new setting. However, vegetable gardening demonstration and cooking sessions were not feasible due lack of facilities, and hence were dropped. The RCT design using two groups (intervention and control) was also applicable for the new setting.
The face-to-face delivery in group format in conjunction with provision of education materials was suitable for the new setting. However, participants in the new setting preferred monthly instead of weekly meetings.
Materials and outcome assessment tools
Health professionals in the new setting deemed the existing education tools, i.e. the diabetes basics and South African Food Based Dietary guidelines (SAFBDGs) flip charts, and take-home education materials to be culturally and practically appropriate.
Regarding tools and techniques for evaluating the NEP, dietary assessment using face-to-face 24-hour recalls was feasible since both the training and working dietitians at the tertiary healthcare use this approach. The knowledge measurement tool was assessed as inadequate, while including a tool to measure diabetes management self-efficacy was considered necessary. The reason for the latter is because self-efficacy was identified as one of the behaviour determinants in the target population, and dietary self-efficacy is evidenced to play a crucial role in diabetes control.Citation40
Cultural fit
The language of instruction in the original NEP (isiTswana) was not suitable for the new setting because of cultural diversity in the new setting. English was therefore chosen as the language of instruction for the NEP. English is the universal language taught in South African schools and is the medium of teaching and learning from grade 4 onwards.Citation41 It would be expected that most patients who have at least some primary school education would have some understanding of English.
Step 3: adaptations of the nutrition education programme
summarises the adaptations that were made to the original NEP and the rationale thereof, as well as features of the adapted NEP. The key adaptations are outlined below.
Table 2: Summary of the original nutrition education program (NEP), adapted NEP and rationale for changes
Design features and delivery
The curriculum component was restructured to fit into monthly meetings. Critical content and activities were fitted within the first four months in view of HbA1c,Citation42 the primary outcome and the outcome assessment at six months. Two topics, namely diabetes and its treatment and dietary guidelines, each previously offered in two sessions, were compressed and set for one session; each covered over 2.5 hours. The additional time to complete a session’s activity in view of the preferred 2 hours was rationalised as follows. Only two sessions would have the additional time, all sessions would have a break and 2.5 hour sessions were successfully used in the original NEP. An additional topic on preventing complications and improving quality of life was added to meet the tertiary patients’ needs.
Due to the difficulties in setting personal goals in the original NEP, content on the importance of goal setting and how to set good (SMART)Citation29 goals as well as a one-on-one session for personal goal setting was added. Other changes included incorporation of a workbook for participants to complete at home, a strategy to engage, educate and sustain motivation between the extended training sessions. Further, additional BCT and strategies, namely individual goal-setting sessions, use of testimonials to promote vicarious learning and self-monitoring of behaviour and outcomes, including blood glucose levels (), were added. The latter was possible since patients in the new setting owned glucometers for self-monitoring of blood glucose, unlike their primary healthcare counterparts. In addition, the adapted NEP retained the bi-monthly follow-up meetings post-training until one year since the NEP aimed to sustain behavioural changes and to minimise attrition. Follow-up meetings will focus on motivating positive behaviour change or its maintenance through group problem-solving of ongoing barriers, sharing of success stories and social support ().
In summary, the adapted NEP comprises (i) seven sessions of curriculum component instead of eight, (ii) two bi-monthly follow-up sessions, (iii) one individual goal-setting session (15–30 minutes), and (iv) take-home education materials (fridge/wall poster and pamphlet) and a workbook. The adapted NEP requires 10 face-to-face contacts instead of 14, with an anticipated contact time of 19.5 hours instead of 26.5 hours.
Materials and outcome measurement tools
For the adapted NEP, the take-home education materials were presented only in English. Additional information on these materials included among others the target levels for the HbA1c test.Citation43 The manual was edited to reflect the changes in the curriculum sessions, and was made more attractive by a graphic designer. The content on dietary guidelines was updated to match the current SAFBDGs.Citation44 The adapted NEP includes an attractive and easy-to-use workbook for patients in the tertiary healthcare setting. The workbook contains a theme and key points for each education session, goal setting and action plan activities, review questions for selected topics and log pages for recording self-monitored blood glucose.
A different diabetes knowledge assessment tool will be used in the adapted NEP.Citation45 This tool is easy to use (true and false format)Citation45 by self-administration or with the help of an interviewer. The knowledge items in this tool correspond to the current diabetes management guidelines and also reflect the NEP content and the needs of diabetes in tertiary healthcare, for example regarding diabetes complications and HbA1c. The Diabetes Management Self-Efficacy Scale (DMSES)Citation46 will be used for assessment of self-efficacy. The DSMES was selected because the majority of its items focus on nutrition and more so on healthy eating in line with the SAFBDGs, the main NEP dietary content. The tools were simplified and assessed by HPs working with people with diabetes for content and face validity to ensure cultural and conceptual equivalence of the original tools. The tools were adjusted as needed after pre-testing with patients.
Step 4: planning for implementation and evaluation of the adapted NEP
Planning for implementation
Facilitators and venue
The adapted NEP will be facilitated by a qualified dietitian, who was involved in developing both the original and the adapted NEPs. A research assistant in nutrition or a related field will assist during education sessions. The researchers will try to create a platform for sustaining the NEP beyond the research phaseCitation25 by inviting relevant hospital HPs to participate in the sessions whenever possible. The education sessions will be held in a hospital venue as per the preference of the target group. The venue will be located far from the diabetes outpatient clinic to prevent close interactions between the control and intervention participants, which could lead to contamination.Citation47
Piloting the implementation process
The piloting of the intervention process (recruitment, data collection and the first session of the curriculum component) indicated that the intervention process was feasible. However, a possible concern of patients finding it difficult to attend three days of 24-hour dietary data collection was revealed, posing a challenge since three days are considered optimal for dietary energy intake estimation.Citation48 The pilot also revealed an appropriate time for starting the education sessions post medicine collection by participants. Participants also indicated they understood the content of the workbook and the expected homework activities.
Planning for evaluation
Planning for outcome evaluation
The adapted NEP will be evaluated by measuring glycaemic control (HbA1c) as the primary outcome. Secondary outcomes will include the lipid profile (total cholesterol, HDL cholesterol, LDL cholesterol and triglycerides) and dietary behaviour measures including starchy food intake, vegetable and fruit intakes, and meal balance (based on acceptable macronutrient distribution). Behaviour mediators including diabetes knowledge and diabetes management self-efficacy will also be measured. The primary and secondary outcomes will be measured at baseline, 6 months and 12 months to indicate sustained change.
Planning for process evaluation
The NEP will be evaluated in respect of reach, completeness of each session, implementation fidelity and participants’ experiences with the programme through a comprehensive process evaluation.Citation29 Process evaluation data will be gathered through session attendance lists, focus-group discussions, individual questionnaires and recording of the education sessions. Researcher-designed data collection tools informed by relevant literature will be used in the process evaluation.Citation29
Discussion
The current study describes the process of adapting a theory-based NEP developed for a primary healthcare setting to a tertiary healthcare setting. The process was guided by consolidated evidence from available intervention adaption frameworks, ensuring comprehensive adaptation, and increasing the potential for an effective NEP. The researchers conducted a needs assessment to ensure that needs of patients with diabetes in a tertiary healthcare setting are met.Citation16 Patients and HPs in the tertiary care setting were engaged to customise the adapted programme and ensure programme fit. Ensuring the fit and meeting the needs of stakeholders should promote potential effectiveness, increase ownership and ensure that the NEP is sustainable beyond the research phase.Citation49
A key step whilst adapting interventions is identifying the theory and the core elements of the intervention. Behaviour change interventions,Citation50 including nutrition education,Citation51 should be developed and implemented using theory to ensure effectiveness.Citation50 Theory provides insights into the mediators of behaviour change, which, if appropriately addressed, can lead to successful interventions. In this study, the researchers developed an NEP grounded in SCT, which is one of the most widely used theories in behavioural interventions,Citation50,Citation52 including successful interventions specific to diabetes.Citation36 The SCT proposes that behaviour, personal factors and the environment interact to explain and predict behaviour.Citation33,Citation39 The SCT is useful in motivational and action phases of behaviour change, and when coupled with target personal and environmental factors is suitable for improving lifestyle behaviours including diet.Citation29
The main change to the adapted NEP was the restructuring of the teaching component because patients in the tertiary healthcare setting considered weekly meetings an extra burden. In the adapted NEP, the teaching component was reduced from weekly to monthly meetings with consequent reduction in the overall number of contact sessions. Although reduced intensity of meetings could impact on the outcomes,Citation35 evidence from comparing a condensed DSME programme, with fewer hours of contact, to an extended programme, with more hours of contact, did not show any differences except for those who attended at least 50% of the extended programme.Citation53 In this study, it was argued that customising the programme to the participants’ preference could result in increased participation. Furthermore, the adapted NEP had the requisite number of sessions, contact time and intervention duration reported to contribute to DSME effectiveness.Citation35, Citation37
A strength of this study is the fact that the researchers developed the original NEP and drove the adaptation process. Their experience regarding the development, implementation and evaluation of the original programme provided insight into possible effective elements that should be maintained and/or strengthened, given the challenge of isolating the effective ingredients of complex interventions.Citation14
There are certain limitations to this study. First, in the needs assessment, open-ended questionnaires were used with the HPs rather than individual interviews or focus-group discussions. This potentially limited the engagement with the HPs. The benefit of the questionnaire was that it could be completed at convenience, negating the need to arrange interviews around tight work schedules. Second, the adapted NEP was modified to meet the needs of T2DM patients at one tertiary hospital, and may not be generalisable to other settings. Last, the researchers were unable to conduct a more extensive pilot study due to project timelines, and additional changes may be required during implementation. This may particularly be an issue for the dietary intake assessment, for which the small pilot study revealed a concern regarding the feasibility of conducting the optimal number of 24-hour diet recalls per participant.Citation48 Despite these limitations, the study describes a process that could be used to adapt other existing interventions to different settings.
Conclusion
This study demonstrates a systematic approach to adapting NEP guided by evidence from adaptation frameworks. Several considerations and choices were made. Sharing these with other researchers and health professionals can help extend our current knowledge regarding adapting health promotion programmes. The adapted NEP will be evaluated for effectiveness, which will provide insight regarding the impact of the adaptations made.
Ethics committee
Faculty of Health Sciences Research Ethics Committee, University of Pretoria.
Acknowledgements
The authors gratefully acknowledge Deborah M. Kupolati for assisting in the focus-group discussions and Cheryl Tosh (University of Pretoria) for assisting with manuscript editing. They also thank the patients and health professionals who participated in the study. Marizanne Booyens and Mmatlhapi Mhlakaza of Creative Studios, Department for Education Innovation, University of Pretoria are thanked for the design and production of the education materials. Nestlé Nutrition Institute Africa is acknowledged for a previous scientific award to Jane Muchiri, which enabled the production of the education materials.
Disclosure statement
No potential conflict of interest was reported by the authors.
The Claude Leon Foundation is acknowledged for the postdoctoral fellowship support for Jane Muchiri.
Additional information
Funding
References
- World Health Organization. Global report on diabetes. Geneva: World Health Organization; 2016.
- America Diabetes Association. Lifestyle management: standards of medical care in diabetes—2018. Diabetes Care. 2018;41(1):S38–S50.
- Powers MA, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American diabetes Association, the American Association of diabetes Educators, and the Academy of nutrition and Dietetics. Diabetes Educ. 2017;43(1):40–53.
- Narayan KV, Gregg EW, Fagot-Campagna A, et al. Diabetes—a common, growing, serious, costly, and potentially preventable public health problem. Diabetes Res Clin Prac. 2000;50:S77–S84.
- Boren SA, Fitzner KA, Panhalkar PS, et al. Costs and benefits associated with diabetes education a review of the literature. Diabetes Educ. 2009;35(1):72–96.
- Rawal LB, Tapp RJ, Williams ED, et al. Prevention of type 2 diabetes and its complications in developing countries: a review. Int J Behav Med. 2012;19(2):121–133.
- Dube L, Van den Broucke S, Housiaux M, et al. Type 2 diabetes self-management education programmes in high and low mortality developing countries: a systematic review. Diabetes Educ. 2015;41(1):69–85.
- Jarvis J, Skinner T, Carey M, et al. How can structured self-management patient education improve outcomes in people with type 2 diabetes? Diabetes Obes Metab. 2010;12(1):12–19.
- International Diabetes Federation Guideline Development Group. Global Guideline for type 2 diabetes. Diabetes Res Clin Pract. 2014;104(1):1–52.
- Dube L, Van den Broucke S, Dhoore W, et al. An audit of diabetes self-management education programmes in South Africa. J Public Health Res. 2015;4(3):581. doi:10.4081/jphr.2015.581.
- Ezenwaka C, Eckel J. Prevention of diabetes complications in developing countries: time to intensify self-management education. Arch Physiol Biochem. 2011;117(5):251–253.
- Pinchevsky Y, Shukla V, Butkow N, et al. The achievement of glycaemic, blood pressure and LDL cholesterol targets in patients with type 2 diabetes attending a South African tertiary hospital outpatient clinic. J Endocrinol Metab Diabete S Afr. 2015;20(2):81–86.
- Pillay S, Aldous C, Mahomed F. Diabetic patients served at a regional level hospital: what is their clinical picture? J Endocrinol Metab Diabetes S Afr. 2015;20(1):60–66.
- Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical research Council guidance. Br Med J. 2008;337. doi:10.1136/bmj.a1655.
- Card JJ, Solomon J, Cunningham SD. How to adapt effective programmes for use in new contexts. Health Promot Pract. 2011;12(1):25–35.
- McKleroy VS, Galbraith JS, Cummings B, et al. Adapting evidence–based behavioural interventions for new settings and target populations. AIDS Educ Prev. 2006;18(Suppl A):59–73.
- Lee SJ, Altschul I, Mowbray CT. Using planned adaptation to implement evidence-based programmes with new populations. Am J Community Psychol. 2008;41(3–4):290–303.
- Afable A, Karingula N. Evidence based review of type 2 diabetes prevention and management in low and middle income countries. World J Diabetes. 2016;7(10):209–229.
- Muchiri JW, Gericke GJ, Rheeder P. Effect of a nutrition education programmeme on clinical status and dietary behaviours of adults with type 2 diabetes in a resource-limited setting in South Africa: a randomised controlled trial. Public Health Nutr. 2016;19(1):142–155.
- Muchiri JW, Gericke GJ, Rheeder P. Needs and preferences for nutrition education of type 2 diabetic adults in a resource-limited setting in South Africa. Health SA Gesondheid. 2012;17(1):1–13.
- Muchiri JW, Gericke GJ, Rheeder P. Impact of nutrition education on diabetes knowledge and attitudes of adults with type 2 diabetes living in a resource-limited setting in South Africa: a randomised controlled trial. J Endocrinol Metab Diabetes S Afr. 2016;21(2):26–34.
- Flay BR, Biglan A, Boruch RF, et al. Standards of evidence: criteria for efficacy, effectiveness and dissemination. Prev Sci. 2005;6(3):151–175.
- National Institute for Health and Clinical Excellence. Type 2 diabetes: Newer agents for blood glucose control in type 2 diabetes. NICE Short clinical guidelines. London: NICE; 2009.
- Muchiri J, Gericke G, Rheeder P. Subjects’ experiences of a nutrition education programmeme: a qualitative study of adults with type 2 diabetes mellitus living in a rural resource-limited setting in South Africa. S Afr J Clin Nutr. 2016;29(2):83–89.
- Abram JK, Hand RK, Parrott JS, et al. What is your nutrition programme missing? finding answers with the Guide for effective nutrition interventions and education (GENIE). J Acad Nutr Diet. 2015;115(1):122–130.
- Highfield L, Hartman MA, Mullen PD, et al. Intervention mapping to adapt evidence-based interventions for use in practice: increasing mammography among African American women. BioMed Res Int. 2015; 11 pages. doi:10.1155/2015/160103.
- Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Huberman AM, Mile MB, editors. The qualitative Researcher's Companion. Thousand Oaks: SAGE Publications; 2002. p. 305–329.
- Muchiri J, Gericke G, Rheeder P. Stakeholders’ perceptions of dietary and related self-management challenges and education programme preferences for type 2 diabetes adults. J Endocrinol Metab Diabetes S Afr. 2019;24(1):1–9. doi:10.1080/16089677.2018.1541211.
- Contento IR. Nutrition education: linking research, theory, and practice. Massachusetts: Jones & Bartlett Learning; 2010.
- New South Wales Department of Health. Public health classifications project- Determinants of health phase two: final report, Sydney. NSW Department of health, 2010.
- Galbraith JS, Herbst JH, Whittier DK, et al. Taxonomy for strengthening the identification of core elements for evidence-based behavioural interventions for HIV/AIDS prevention. Health Educ Res. 2011;26(5):872–885.
- Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycaemic control. Patient Educ Couns. 2016;99(6):926–943.
- Baranowski T, Perry CL, Parcel GS. How individuals, environments and health behaviour interact: social Cognitive theory. In: Glanz K, Rimer BK, Lewis FM, editor. Health behaviour and health education. theory,research and practice. 3rd ed. San Francisco: Josey-Bass; 2002. p. 165–184.
- Steinsbekk A, Rygg L, Lisulo M, et al. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv Res. 2012;12(1):213. doi:10.1186/1472-6963-12-213.
- Fan L, Sidani S. Effectiveness of diabetes self-management education intervention elements: a meta-analysis. Can J Diabetes. 2009;33(1):18–26.
- Rosal MC, Ockene IS, Restrepo A, et al. Randomized trial of a literacy-sensitive, culturally tailored diabetes self-management intervention for low-income Latinos: Latinos en control. Diabetes Care. 2011;34(4):838–844.
- Glazier RH, Bajcar J, Kennie NR, et al. A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care. 2006;29(7):1675–1688.
- Michie S, Ashford S, Sniehotta FF, et al. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health. 2011;26(11):1479–1498.
- Abraham C, Sheeran P. The health belief model. In: Conner M, Norman P, editor. Predicting health behaviour: research and practice with social Cognition Models. 2nd ed. Maidenhead: Open University Press; 2005. p. 28–80.
- Strychar I, Elisha B, Schmitz N. Type 2 diabetes self-management: role of diet self-efficacy. Can J Diabetes. 2012;36(6):337–344.
- Department of Education. Final report: report of the task team for the review of the implementation of the national curriculum statement. Pretoria: Government Printers; 2009.
- Goldstein DE, Little RR, Lorenz RA, et al. Tests of glycemia in diabetes. Diabetes Care. 2004;27(7):1761–1773.
- Iqbal N, Morgan C, Maksoud H, et al. Improving patients’ knowledge on the relationship between HbA1c and mean plasma glucose improves glycaemic control among persons with poorly controlled diabetes. Ann Clin Biochem. 2008;45(5):504–507.
- Vorster HH, Badham J, Venter C. An introduction to the revised food-based dietary guidelines for South Africa. S Afr J ClinNutr. 2013;26(3):S5–S12.
- Collins G, Mughal S, Barnett A, et al. Modification and validation of the revised diabetes knowledge scale. Diabet Med. 2011;28(3):306–310.
- Bijl J, Poelgeest-Eeltink AV, Shortridge-Baggett L. The psychometric properties of the diabetes management self-efficacy scale for patients with type 2 diabetes mellitus. J Adv Nurs. 1999;30(2):352–359.
- Howe A, Keogh-Brown M, Miles S, et al. Expert consensus on contamination in educational trials elicited by a Delphi exercise. Med Educ. 2007;41(2):196–204.
- Ma Y, Olendzki BC, Pagoto SL, et al. Number of 24-hour diet recalls needed to estimate energy intake. Ann Epidemiol. 2009;19(8):553–559.
- Koelen MA, Vaandrager L, Colomér C. Health promotion research: dilemmas and challenges. J Epidemiol Community Health. 2001;55(4):257–262.
- Glanz K, Bishop DB. The role of behavioural science theory in development and implementation of public health interventions. Ann Rev Public Health. 2010;31:399–418.
- Murimi MW, Kanyi M, Mupfudze T, et al. Factors influencing efficacy of nutrition education interventions: a systematic review. J Nutr Educ Behav. 2017;49(2):142–165. e141. doi:10.1016/j.jneb.2016.09.003.
- Spahn JM, Reeves RS, Keim KS, et al. State of the evidence regarding behaviour change theories and strategies in nutrition counseling to facilitate health and food behaviour change. J Am Diet Assoc. 2010;110(6):879–891.
- Brown SA, Blozis SA, Kouzekanani K, et al. Dosage effects of diabetes self-management education for Mexican Americans: the starr county border health initiative. Diabetes Care. 2005;28(3):527–532.