?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Introduction:
Diabetes self-management education (DSME) and medical nutrition therapy (MNT), provided by diabetes educators and registered dietitians respectively, considerably improve glycaemic control. However, it is unknown what interventions exist in many African countries and the impact thereof.
Aim:
To determine the impact of existing DSME interventions on knowledge, attitudes and practices (KAP) of adults with type 2 diabetes attending public health care facilities in Harare, Zimbabwe.
Methods:
A cross-sectional, researcher-administered survey was designed to assess DSME KAP at eight outpatient diabetes clinics that provide diabetes services. Participants were conveniently sampled. Associations between mean scores for knowledge, attitudes and practices were compared between characteristics of DSME interventions.
Results:
A total of 154 participants were recruited and divided evenly between two tertiary (n = 77) and six primary outpatient clinics (n = 77). The mean age was 61.8 years (SD ± 12.7), mean years since diagnosis with diabetes was 8.1 years (SD ± 8.3) and the majority were females (66.9%, n = 103). Most participants (90.3%, n = 139) reported receiving some DSME. Participants most frequently cited a tertiary clinic as the place where DSME was received. Fewer had consulted a dietitian (49.0%, n = 76) or diabetes educator (52.0%, n = 80). Higher levels of diabetes knowledge were observed for tertiary clinic attendees (p = 0.00), consultation with a dietitian (p < 0.01) and diabetes educator (p = 0.00). Only those who had consulted a dietitian reported better adherence to dietary guidelines (p = 0.00) and physical activity (p = 0.02) self-care behaviours.
Conclusion:
Dietitian-led interventions significantly improved both knowledge and practices, highlighting a need to scale up dietetic intervention, particularly in primary clinics where limited interventions occur.
Introduction
Diabetes mellitus is a chronic progressive condition that demands intensive daily self-care to achieve optimum glycaemic targets. Type 2 diabetes is the most common form of diabetes, accounting for more than 90% of cases worldwide.Citation1 The importance of achieving glycaemic targets has been demonstrated by several landmark studies, which show that the risks of diabetes-related complications decrease significantly with every point decline in haemoglobin A1c (HbA1c).Citation2–4 Diabetes self-management education (DSME) is defined as the process of facilitating the acquisition of knowledge and skills necessary for individuals with diabetes to make daily self-management decisions.Citation1 DSME is a fundamental strategy to reduce the incidence of complications, healthcare costs and societal burden of diabetes.Citation1,Citation5
The prevalence of diabetes in Zimbabwe is currently estimated at 8.5% and has more than doubled in the past 30 years.Citation6 Moreover, Zimbabwe has the third highest estimated per person cost of diabetes care in sub-Saharan Africa.Citation7 These costs are related to the management of diabetes complications, including hospitalisation, which can potentially be reduced by effective DSME interventions.Citation1,Citation7 However, the reality of the situation is inadequate funding for non-communicable disease education programmes and non-availability of qualified health personnel to deliver DSME in most African countries, including Zimbabwe.Citation7,Citation8
DSME interventions led by diabetes educators or registered dietitians have been shown to reduce HbA1c by 1% and 2% respectively, while also improving other important clinical outcomes such as abnormal lipid profile, weight management, blood pressure management, and in some cases the need for pharmacological treatment.Citation1,Citation9 Most of these data originate from North America and Europe, and very little is documented concerning the impact of DSME led by both types of health professionals in sub-Saharan Africa.Citation8,Citation10
A major contributor to the lack of evidence to support specialist DSME interventions in Africa is the severe shortage of registered dietitians and diabetes educators, particularly in public health facilities. According to the health professionals’ council, Zimbabwe has under 20 registered dietitians in practice and only two of them are stationed at the two tertiary hospitals in Harare.Citation11 Although there are no recognised diabetes educator certification programmes in the country, some nurses, particularly those working at tertiary hospital outpatient clinics, are referred to as diabetes educators and may have received some in-service DSME training.
Evidence on DSME in Africa also shows that DSME in low-resource settings is not consistent in structure, and outcomes thereof are not routinely monitored or measured.Citation8,Citation10 Therefore, there is paucity of information on the outcomes of existing DSME interventions. This study assessed the impact of existing interventions in outpatient diabetes clinics by comparing patient knowledge, attitudes and practices related to nutrition and other self-management parameters between patients who have received DSME compared with those who had not. Knowledge, attitudes and practices (KAP) are process outcomes of DSME interventions and are prerequisites for achieving optimal glycaemic control and other clinical parameters. It was hypothesised that patients attending clinics where diabetes educators and/or dietitians led DSME interventions would have higher levels of diabetes knowledge, attitudes and adherence to diet and physical activity self-care behaviours compared with patients attending clinics without these interventions.
Methods
Study design and population
A cross-sectional survey was conducted in eight public health outpatient diabetes clinics (six primary clinics and two tertiary hospital-based clinics) in Harare, Zimbabwe. Both primary and tertiary clinics were included to ensure adequate representation of the general diabetes patient population.
The inclusion criteria were adults aged over 18 years old, diagnosed with type 2 diabetes, who gave informed consent. Individuals under the age of 18 and with other types of diabetes (e.g. type 1 diabetes and gestational diabetes) were excluded.
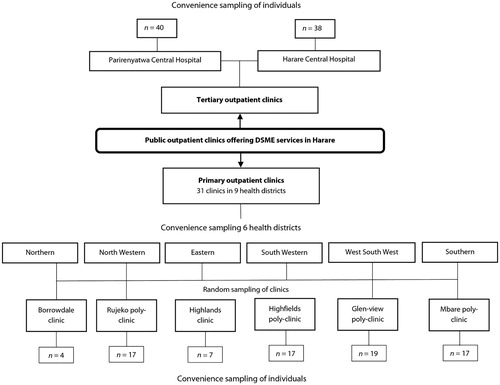
Two (of two) tertiary hospital outpatient clinics in Harare were conveniently selected. Six of 31 primary clinics were selected using multistage sampling (). Primary clinics are stratified into nine health districts, of which six health districts were conveniently sampled. Four of the six health districts were selected because the highest number of patients with diabetes were recorded from previous year attendance statistics. The remaining two districts were selected to represent the clinics with the lowest attendance to avoid bias. Clinics within districts were selected by random sampling. Individuals from both tertiary and primary outpatient clinics who fulfilled the inclusion criteria were included.
Power analysis was performed to determine a sample size that would detect an effect size of 0.4 between mean KAP scores of primary and tertiary clinic attendees. Sixty-seven participants per clinic group (total of 140) were required to demonstrate 90% power at a 5% significance level. The final sample included 156 (77 participants per group). The number of subjects selected per clinic is proportional to attendance statistics ().
Data collection
The KAP questionnaire was administered by final-year Nutrition students from the University of Zimbabwe, trained in the survey techniques. The tool was developed by the researcher through a process of reviewing existing literature and peer reviewed by local diabetes experts. Constructs/domains for knowledge, attitudes and practices necessary for the management of type 2 diabetes were identified through review of recent position papers on DSME.Citation1,Citation9,Citation12 The constructs were grouped into diet self-management and general self-management subscales. Question items relevant to the constructs identified were derived from existing validated instruments.Citation13–15 The KAP constructs and items were also peer reviewed by local diabetes experts. The tool was translated into Shona by a language expert and back-translated for semantics by the local DSME experts. Pre-testing was done on 11 subjects who were not included in the final sample.
The final questionnaire () included 42 items, starting with 11 demographic items, then 11 knowledge items, 13 attitude items and 7 practice items. Demographic items included age, gender, education level, duration of diabetes and DSME received. Knowledge was assessed using multiple-choice questions. A score of 1 was assigned to each correct answer. The maximum possible knowledge score was 11. The two subscales within the final knowledge score—diet self-management and general self-management maximum scores—were 5 and 6, respectively. No cut-offs were used to determine levels of knowledge and no clinical outcomes were measured.
Attitude responses were measured on a five-point Likert scale. A numerical value was assigned to each response choice. The highest possible score for each characteristic was 5, indicating a desirable/positive attitude and a score of 1 indicated an undesirable/negative attitude. Diet and physical activity adherence items were measured on a seven-day frequency scale.
Statistical analysis
Data were entered using Statistica Version 11© (Tibco Software Inc, Palo Alto, CA, USA). Demographic data were presented as frequencies and percentages. Mean scores () and standard deviations (SD±) for knowledge, attitudes, diet and physical activity adherence were calculated for demographic characteristics: clinic group, education level, previous consultation with dietitian or diabetes educator and primary source of diet information. Non-parametric, Mann–Whitney U- and Kruskall–Wallis H-tests were performed for comparing paired observations and multiple observations respectively. The chi-square test was used to compare categorical data. All tests were two sided and a p-value of less than 0.05 was considered significant.
Ethical approval
The study was approved by the Health Research Ethics Committee at Stellenbosch University (S14/03/063) and the Medical Research Council of Zimbabwe (MRCZB021).
Results
Demographics
In total, 154 participants were recruited. The mean age was 61.8 years (SD ± 12.7) and most subjects were female (66.9%, n = 103). Participants were clustered between primary level education (53.2%, n = 83,) and secondary level education (37.2%, n = 57). The self-reported time since diagnosis of diabetes ranged from 2 months to 45 years ( 8.1 years, SD ± 8.3 years) with no differences observed between clinic groups (p = 0.77). Most patients were on oral glucose-lowering medication alone (77.9%, n = 120). Tertiary clinic respondents were 5.2 years younger than primary clinic respondents (p = 0.02) ().
Characteristics of diabetes education
shows that most (90.3%, n = 139) participants reported receiving some diabetes nutrition education from a public health facility. More tertiary clinic participants (96.1%, n = 74) reported receiving DSME than primary clinic participants (84.4%, n = 65). Also, most respondents who reported receiving DSME were educated at tertiary clinics (94.6%, n = 123) compared with primary clinics (3.1%, n = 4). A health professional (doctor, nurse, dietitian) was cited as the primary source of diabetes nutrition information for most respondents (85%, n = 131). More tertiary clinic respondents had consulted a dietitian (χ2 = 10.61, p = 0.00) or diabetes educator (χ2 = 12.31, p = 0.00) compared with primary clinic respondents.
Table 1: Knowledge, attitudes and practices questionnaire items
Table 2: Demographic characteristics of participants.
Diabetes knowledge
summarises and compares the mean knowledge scores for characteristics of DSME received and other demographic variables. Tertiary clinic participants had higher levels of overall DSME knowledge (p = 0.00), nutrition self-management knowledge (p = 0.00) and general self-management knowledge (p = 0.02) compared with primary clinic participants. Knowledge in all domains assessed was also higher for participants who reported consulting a dietitian or diabetes educator. Respondents who cited dietitians as their primary source of knowledge had higher final knowledge marks than all other primary sources of diet information (p < 0.01), while participants with higher levels of education showed better knowledge on diabetes management (p = 0.01).
Table 3: Mean diabetes knowledge scores, characteristics of diabetes education, clinic type and education level.
Diabetes attitudes
No significant differences between clinic groups for overall mean attitudes (p = 0.10), diet (p = 0.05), and general self-management attitudes (p = 0.17) were observed (). Mean attitude scores for subjects who consulted a dietitian or diabetes educator did not differ significantly from those who did not for all domains. Additionally, the sources of diet information (p = 0.13) and education level (p = 0.41) did not change mean attitude scores.
Table 4: Mean attitude scores, history of diabetes self-management education, clinic type and education level.
No significant differences were observed between participants who attended tertiary clinics and those who were at primary clinics for mean days of dietary (p = 0.11) and physical activity adherence (p = 0.98) (). Participants who had consulted a dietitian reported more days of adherence to dietary guidelines (4.45, SD ± 1.47) compared with those who did not (
2.93, SD ± 1.75) (p = 0.00). Days of physical activity adherence were also higher in those who had consulted a dietitian (
3.03, SD ± 2.07) compared with those who had not (
2.64, SD ± 2.27) (p = 0.02). No differences were observed in both parameters for consultation with a diabetes educator. Subjects who cited a dietitian as the primary source of information reported more days of dietary adherence than all other sources of primary diet information (p = 0.00). The level of education of participants was not associated with mean days of dietary adherence (p = 0.24) or physical activity (p = 0.53).
Table 5: Diet and physical activity practices.
Discussion
Despite the large body of evidence that supports the positive impact of DSME led by diabetes educators or registered dietitians in developed countries, very little is known about the outcomes of these interventions in Africa.Citation8 This study demonstrates that diabetes knowledge consistently improves with both dietitian and diabetes educator led interventions. However, attitudes towards diabetes were not significantly different in participants who received DSME compared with those without. Only dietitian-led interventions had a positive impact on adherence to diet and physical activity self-care behaviours, which is supported by existing data.Citation1,Citation16 The factors that make dietitian-led DSME more successful are not well understood. However, it is possible that the individualised nature of dietitian-led interventions compared with diabetes educator-led interventions may have a role to play.Citation16
Furthermore, tertiary clinic participants had better knowledge, but not attitudes and practices, than their counterparts at primary clinics. This may be explained by the fact that over 90% of all participants cited a tertiary clinic as their place of education. Tertiary clinic participants were also more likely to have consulted with a dietitian and/or a diabetes educator. This reveals a major gap in the continuity of DSME at primary care level, which may leave patients at primary clinics more vulnerable to unverified sources of DSME. Further to the point, almost one in five primary clinic participants cited a non-health professional source of DSME information.
The results also demonstrate good coverage of DSME interventions in Harare. More than 90% of participants reported receiving DSME at any point in time and about half had consulted either a dietitian or diabetes educator. Another study performed in Zimbabwe also showed that a similar proportion of people (45%) reported consulting a diabetes educator at least once.Citation17 These figures compare favourably to reports from countries with more resources for DSME than Zimbabwe.Citation18 It must be noted that the scope and content of DSME interventions in most Zimbabwean clinics are not documented, nor do standards for DSME exist. This effectively means that patients may consider DSME to be anything from a planned educational talk to spontaneous pieces of information that are subject to variation depending on the time and motivation of the health professional.Citation8,Citation10 This lack of consistency and structure in DSME makes it difficult to determine whether education received by participants was adequate.
The lack of improvement in attitudes towards diabetes in participants who received DSME is consistent with findings in neighbouring South Africa.Citation19 Factors such as the duration and frequency of education, and intrinsic traits of the patient (e.g. self-efficacy) have been shown to impact on patient attitudes towards diabetes and its treatment.Citation5,Citation20 These factors were not considered in the study design and warrant further investigation. The level of knowledge acquisition that would elicit changes in attitudes is also unclear in this study population. Hence, it is possible that the higher levels of knowledge observed in people who have participated in specialist-led DSME may not have been enough to elicit behaviour change.
Limitations of the study
The measuring instrument was not validated in the intended population and was also researcher designed, which limited direct comparability with existing instruments. This also made it difficult to assign cut-off scores for knowledge, attitudes and practices. In addition, the cross-sectional study design made it difficult to establish causation. The possibility of social desirability bias arising from the face-to-face administration of the instrument cannot be ruled out, particularly with reporting of attitudes and self-care practices. The lack of measured clinical outcomes is also a limitation, which should be addressed in future studies.
Conclusion
This study serves as an important baseline for assessing the outcomes of current DSME interventions in Zimbabwe. The growing number of people with diabetes in Zimbabwe warrants more focus on optimising DSME interventions with evidence-based approaches such as specialist DSME educators and registered dietitians. Therefore, this study has demonstrated a positive impact of dietitian- and diabetes educator-led interventions on patient knowledge in a resource-limited setting. The results also highlight the need to scale up both interventions, which may lead to improved attitudes and practices. Continuity of DSME to the primary clinics is a priority to decentralise DSME and improve outcomes for patients at primary clinics.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Beck J, Greenwood DA, Blanton L, Bollinger ST, Butcher MK, Condon JE, et al. 2017 National standards for diabetes self-management education and support. Diabetes Educ. 2018;44(1):35–50. doi: 10.1177/0145721718754797
- Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and Vascular complications in Veterans with type 2 diabetes. N Engl J Med. 2009;360(2):129–139. doi: 10.1056/NEJMoa0808431
- The Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Study Research Group. Intensive diabetes treatment and cardiovascular outcomes in type 1 diabetes: The DCCT/EDIC study 30-year follow-up. Diabetes Care. 2016;39(5):686–693. doi: 10.2337/dc15-1990
- American Diabetes Association. Implications of the United Kingdom prospective diabetes study. Diabetes Care. 2002;25(1):s28–s32.
- Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Educ Couns. 2016;99(6):926–943. doi: 10.1016/j.pec.2015.11.003
- Mutowo M, Gowda U, Mangwiro JC, Lorgelly P, Owen A, Renzaho A. Prevalence of diabetes in Zimbabwe: a systematic review with meta-analysis. Int J Public Health. 2015;60(1):1–11. doi: 10.1007/s00038-014-0626-y
- Mutowo M, Lorgelly P, Laxy M, Renzaho A, Mangwiro J, Owen A. The hospitalization costs of diabetes and hypertension complications in Zimbabwe: Estimations and correlations. J Diabetes Res. 2016;(9):1–9.
- Dube L, Van den Broucke S, Housiaux M, Dhoore W, Mkhosi-Rendall K. Type 2 diabetes self-management education programs in high and low mortality developing countries: A systematic review. Diabetes Educ. 2015;41(1):69–85. doi: 10.1177/0145721714558305
- Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Fischl AH, et al. Diabetes self-management education and support in type 2 diabetes: A Joint position statement of the American diabetes association, the American association of diabetes educators, and the Academy of nutrition and Dietetics. Diabetes Educ. 2017;43(1):40–53. doi: 10.1177/0145721716689694
- Dube L, Van den Broucke S, Dhoore W, Kalweit K. An audit of diabetes self-management education programs in South Africa J Public Health Res 2015;581:176–184.
- Zimbabwe AHPCo. Dieticians & Nutritionists in Zimbabwe 2018 updated 2018. Available from: https://ahpcz.co.zw/wp-content/uploads/2018/11/Diet-and-Nutrition.pdf.
- Franz MJ, MacLeod J, Evert A, Brown C, Gradwell E, Handu D, et al. Academy of nutrition and dietetics nutrition practice Guideline for type 1 and type 2 diabetes in adults: Systematic review of evidence for medical nutrition therapy effectiveness and recommendations for integration into the nutrition care process. J Acad Nutr Diet. 2017;117(10):1659–1679. doi: 10.1016/j.jand.2017.03.022
- Fitzgerald JT, Funnell MM, Anderson RM, Nwankwo R, Stansfield RB, Piatt GA. Validation of the Revised Brief diabetes knowledge test (DKT2). Diabetes Educ. 2016;42(2):178–187. doi: 10.1177/0145721715624968
- Eigenmann C, Skinner T, Colagiuri R. Development and validation of a diabetes knowledge questionnaire. Pract Diab Int. 2011;28(4):169–70d. doi: 10.1002/pdi.1586
- Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943–950. doi: 10.2337/diacare.23.7.943
- Briggs Early K, Stanley K. Position of the academy of nutrition and dietetics: The role of medical nutrition therapy and registered dietitian nutritionists in the prevention and treatment of prediabetes and type 2 diabetes. J Acad Nutr Diet. 2018;118(2):343–353. doi: 10.1016/j.jand.2017.11.021
- Mufunda E, Ernersson Å, Hjelm K. Limited knowledge of diabetes in patients attending an outpatient diabetes clinic at a referral hospital in Zimbabwe: a cross-sectional study. Pan Afr Med J. 2018;29:1–13. doi: 10.11604/pamj.2018.29.144.12301
- Ali MK, Bullard KM, Saaddine JB, Cowie CC, Imperatore G, Gregg EW. Achievement of goals in U.S. diabetes care, 1999–2010. N Engl J Med. 2013;368(17):1613–24. doi: 10.1056/NEJMsa1213829
- Ceronio V, Mbhenyane XG. Dietary management practices for diabetes by dietitians in public hospitals in Limpopo province, South Africa. J Nutri Health. 2017; 3(1):1-6.
- Ganiyu AB, Mabuza LH, Malete NH, Govender I, Ogunbanjo GA. Non-adherence to diet and exercise recommendations amongst patients with type 2 diabetes mellitus attending Extension II Clinic in Botswana. Afri J of Prim Health Care Fam Med. 2013;5(1):1–6. doi: 10.1071/HC13001