Abstract
Introduction: Numerous studies show the benefits of vitamin D: in the prevention of bone disease, supporting the immune system and the prevention and mitigation of cancer. Until recently, supplementation has been deemed unnecessary. Nonetheless, in the light of emerging evidence, some practitioners are adding vitamin D and its analogues (Anatomic Therapeutic Chemical (ATC) classification code A11CC) to their prescriptions. Therefore, the aim was to determine the medical insurance prescribing patterns of vitamin D in South Africa.
Methods: A retrospective, cross-sectional drug utilisation study was conducted on a South African medical insurance administrator database for 2018. Products in ATC subgroup A11CC (vitamin D and analogues) were extracted and analysed.
Results: A total of 302 patients received 1 164 prescriptions for a vitamin D or analogue product during 2018. The average age of patients was 47.14 (SD = 24.03) years, and the majority were female (58.28%). Very young patients and middle-aged patients received most of the prescriptions. Ergocalciferol (A11CC01) was the most frequently prescribed (59.79%), followed by alfacalcidol (A11CC), colecalciferol (A11CC05) and calcitriol (A11CC04). Ergocalciferol 50 000 IU tablets comprised the most frequently prescribed trade name product (59.45%), followed by alfacalcidol capsules (21.31%).
Conclusion: Vitamin D was used across the age range. Vitamin D supplementation was primarily prescribed in the very young and older age groups, suggesting their need for additional supplementation. As the cost of additional supplements is relatively small compared with the treatment of deficiency disorders, vitamin D supplementation could have broad and positive effects on long-term health for very little outlay.
Introduction
There are two forms of vitamin D. Vitamin D2 (ergocalciferol) is derived from the irradiation of ergosterol and found in food sources such as fortified foods, plant oils and mushrooms, and vitamin D3 (cholecalciferol) is derived from animal food sources such as oily fish and egg yolk and the action of sunlight on the subcutaneous layer of the skin.Citation1 There are numerous studies on the benefits of vitamin D, the role that vitamin D plays in the prevention of bone disease and more recently in the immune system and the prevention and mitigation of cancer. The action of vitamin D is that of a neuro-hormone that regulates both cell growth and immunomodulation.Citation1 In the former role, vitamin D is well established in its action on bone growth and repair, and the prevention of rickets and osteoporosis.Citation1–4 Other studies have implicated vitamin D in the mitigation of bronchiectasis,Citation5 prevention of early age-related macular degeneration,Citation6 and in support of the immune system in people living with human immunodeficiency virus (HIV).Citation7
As an immune modulator, vitamin D3 has been found to be a factor in the prevention and mitigation of several forms of cancer including breast, ovarian, colorectal, oral, small-cell lung and prostate cancers.Citation8–20 The emerging evidence for the therapeutic use of vitamin D in the treatment of cancer warrants attention.Citation11,Citation19,Citation21,Citation22 Cancer costs across the world are inestimable, and not all countries can afford to test and treat for the multiple cancers arising within the population. A report on the World Health Organization (WHO) Global Action Plan for the most conservative and cost-effective testing and treatment of breast cancer alone for the east sub-Saharan African region was an estimated US$ 1 635 per 10 million people per annum, in 2010.Citation23
The addition of vitamin D and phenylbutyrate to the standard treatment of tuberculosis (TB) has been found to be more effective than standard treatment alone.Citation24 Vitamin D has also been found to be effective alongside vitamin C, zinc and echinacea for the prevention and treatment of the common cold.Citation25 The worldwide increase in fragility fractures in the elderly has been described as catastrophic and potentially directs the cost of medicine away from other critical areas of health.Citation26 As people live longer and women live longer than men, the cost of treating osteoporosis in those at high risk is considerable. Clinical guidelines in the United Kingdom are based on the cost-effective use of bisphosphonates in women over 50 years who are at high risk but do not take into consideration the cost of the longer-term side effects and possible complications.Citation27 Australia, which has a similar climate and number of sunlight hours to South Africa, has focused on both initial fracture management and re-fracture prevention and management. These two strategies reduced the costs of fracture treatment from AU$ 1.76 billion (US$ 1.21 billion) to AU$ 1.58 billion (US$ 1.09 billion).Citation26
Vitamin D supplementation, however, has until recently been deemed unnecessary and is still not without controversy.Citation28 This factor, alongside the reduction in sunlight-derived vitamin D due to fears of skin cancer, and the increased use of sunscreens, has resulted in an increase in osteoporosis in vulnerable populations.Citation29,Citation30 In moderately and heavily pigmented immigrants to countries with fewer hours of sunlight, supplementation of vitamin D has been found to surpass the effectiveness of sunlight exposure for osteoporosis prevention.Citation31 In the light of emerging medical evidence of the benefits of vitamin D, some primary care practitioners have recently been prescribing vitamin D and vitamin D analogues for a number of reasons,Citation32 including proactive and preventative use for the multiple effects of deficiency in children and young adults.Citation33 The prescribing of vitamin D for older women to prevent osteoporosis,Citation3 and the use of vitamin D alongside probiotics for the mitigation of asthma and allergy is not uncommon.Citation34
In some quarters, however, there is still resistance to both testing for deficiency and prescribing of vitamin D, which is viewed as unnecessary health expenditure.Citation35 The safety and efficacy of high doses of vitamin D are also still in question.Citation36 These factors, notwithstanding the adequacy of the current recommendation for the fortification of foods and the supplementation of vitamin D, particularly for children, are being questioned.Citation37 The American Academy of Paediatrics (AAP) has recently doubled its recommended dosage of vitamin D from 200 IU to 400 IU per day for infants, children and adolescents.Citation38
Requirement for vitamin D in South Africa
Adequate blood levels of vitamin D for children in South Africa are considered to be =/> 30 ng/ml acquired through a combination of sunlight and food intake.Citation39 A study conducted in the Western Cape of South Africa found that 16.2% of children on antiepileptic medication required additional vitamin D, due to the possible destruction of vitamin D as a side effect of their treatment.Citation39 This notwithstanding that 8.8% of non-epileptic children with no history of bone metabolism disorders in the control group were also vitamin D deficient.Citation39 A study conducted among hypertensive adults in an urban black community in Mangaung found that, despite the relationship between body mass index (BMI) and hypertension, vitamin D status appeared to have a protective effect, and those with an adequate vitamin D status appeared to be less vulnerable to hypertension despite an elevated BMI.Citation40 There appears to be a requirement for increased vitamin D among those with darker skin due to the decreased conversion of vitamin D from sunlight and a reciprocal relationship between vitamin D status and the rate of sputum culture conversion,Citation41 and seasonal reporting of TB, with higher incidences of TB in the winter months of reduced sunlight.Citation42 The need for vitamin D supplementation for all adult South Africans is still under review.Citation43 Variations in pigmentation and vitamin D receptor gene, and changes in lifestyle that reduce sunlight exposure need to be taken into consideration when making recommendations on vitamin D intake and supplementation.Citation43 Considering the connection between vitamin D and immune function, it has been postulated that recommendations for supplementation require a rethink in order to reduce the burden of suffering and the related healthcare costs.Citation43
Prescribing of vitamin D in South Africa
A previous study on the dispensing of vitamins by retail/community pharmacies in South Africa found that ergocalciferol (Anatomic Therapeutic Chemical (ATC) classification code A11CC01), which is available only on prescription, was the most often dispensed (37.48%) of all prescription vitamin products in 2013.Citation32,Citation44 Public health prescribing is more difficult to ascertain, as public hospitals and community health centres and clinics do not utilise retail/community pharmacies, medication is given free of charge by the facility and electronic records are not nationally linked; however, there is a tendency for the private healthcare sector to lead the way in the prescribing of nutraceuticals. Establishing private healthcare prescribing patterns may provide an indication of the trend in prescribing of vitamin D and, consequently, the possible future public healthcare prescribing, expenditure and the cost–benefit ratio of vitamin D supplementation on a broader scale. The primary aim of the study was, therefore, to determine the prescribing patterns of vitamin D and analogues (ATC code A11CC) in a private healthcare setting in South Africa. As South Africa moves into the introduction of the new National Health Insurance (NHI) provision, prescribing of supplements may become public/state expenditure. Knowledge of what is being prescribed and to whom, and for which reasons, will enable future planning of the public needs and government expenditure required for preventive medicine.
Methods
A retrospective, cross-sectional drug utilisation study was conducted on a South African medical insurance administrator database for accepted and paid claims for the year 2018. The administrator oversees the claims for several medical insurance schemes. The database contained 4 191 138 records for medicine, medical devices and procedures. The ATC,Citation45 Monthly Index of Medical Specialities (MIMS)Citation46 and the South African Medicines FormularyCitation47 were used to classify medicines. Products in ATC subgroup A11CC (vitamin D and analogues) were extracted and analysed. As this study relates only to prescribed medications and the diagnoses of the individual patients were not disclosed the authors assumed that the prescriptions were given due to there being a clinical indication for their use. It must also be noted that the study did not include the numerous multivitamin products containing low-dose vitamin D that are available over the counter (OTC) from pharmacies, health shops and other distributors in South Africa. The focus of this study was specifically to determine which products containing vitamin D or a vitamin D analogue were prescribed to patients and paid for by the medical insurance schemes.
The study focused only on the private healthcare sector, which constitutes about 17.4% of the total healthcare sector in South Africa.Citation48 Data for the public healthcare sector are not readily available.
Each medication record contained information on the age and gender of the patient, with a unique number to identify each patient, the date of the prescription, detailed information on the dispensed drug (name, package size, formulation, strength and quantity) and gross sales value. The diagnostic ICD-10 codes were not available in the database. Microsoft Access® and Excel® (Microsoft Corp, Redmond, WA, USA) were used to analyse the data. Descriptive statistics were calculated using SPSS V 20® (IBM Corp, Armonk, NY, USA).
Ethical approval to conduct studies on prescription databases has been obtained from the Research Ethics Committee (Human) of the Nelson Mandela University (ethics clearance number: H08-HEA-PHA-005).
Results
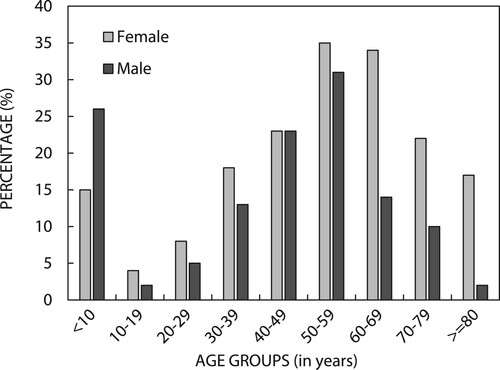
A total of 302 patients (176 female and 126 male) received a total of 1 164 prescriptions for a vitamin D or analogue product during 2018 (an average of four [3.85 SD = 3.77] products per year per patient) (). The median age of patients was 47.14 (SD = 24.03) years. The age and gender distribution of patients are given in .
Figure 1: Age and gender distribution of patients who were prescribed a vitamin D or analogue product (n = 302).
In total, 123 patients received a single prescription, 238 patients received six or fewer products, and 7 patients received more than 12 prescriptions over the period of one year ().
Table 1: Frequency distribution of vitamin D or analogue products prescribed per patient during the year (n = 302)
Providers of products and cost of claims
indicates the provider where each prescription was dispensed. As expected, most prescriptions (69.76%) were dispensed by retail or community pharmacies. This was followed by private hospitals (21.82%), where it was vitamin D drops especially that were dispensed to young children.
Table 2: Providers of vitamin D and analogues (n = 1 164)
Pharmacy dispensing of private practitioner prescriptions outweighed all other dispensers of vitamin D products (69.76% of all prescriptions), suggesting that most vitamin D was prescribed to ambulatory patients as opposed to hospitalised patients (). Private hospitals would dispense to inpatients in addition to patients leaving the hospital on discharge, although no distinction between these patients was made or was possible in this study. The private medical insurers received claims for vitamin D or analogue products to the value of ZAR 152 243, of which ZAR 119 337 was covered by the insurer, and the rest constituted out-of-pocket expenses for patients. Given the number of prescriptions dispensed, this constitutes a relatively small average expenditure for the individual (ZAR 28.27 or US$ 2.02) per prescription.
Active ingredients dispensed
shows the four different ATC groups of products that were dispensed, according to gender.Citation47 Ergocalciferol constituted 59.79% of all prescriptions. shows that the most often prescribed trade name product was ergocalciferol 50 000 IU tablets (59.45%), followed by alfacalcidol 0.25 µg capsules (21.31%) and colecalciferol (400 IU/0.5 ml) drops (6.27%). With respect to the number of dosage units dispensed, most prescriptions (65.95%) for ergocalciferol tablets were for only four or five tablets, while 67.19% of prescriptions for alfacalcidol were for 30 capsules. All seven prescriptions for calcitriol were for 60 capsules.
Table 3: Number of trade-name products dispensed in the different ATC groups to female and male patients
Most prescriptions shown in (64.26%) were for tablets, followed by capsules (27.92%) and drops (7.39%). Orodispersible films accounted for 0.24% of prescriptions and effervescent products for only 0.09% (one product). Most drops were dispensed to children, while the prescriptions for the orodispersible film were dispensed to older patients. No capsules were dispensed to children.
Table 4: Dosage forms and quantities dispensed
A significant number of prescriptions were given to younger patients; the average number of repeat prescriptions was four in the 10–19-year age group. Nonetheless, there is a direct positive correlation between the number of repeat prescriptions given to any individual patient and the age of the patient (r = 0.826 p = 0.006) (Pearson's two-tailed correlation).
Discussion
Vitamin D appears to be prescribed across the age range. Although a significant number of prescriptions were dispensed to children, the largest number of prescriptions appears to be among women in the 50–59-year age group. Younger patients received vitamin D in the form of drops, which are easier to administer for very young children, while older persons received more capsules or tablets and the soluble orodispersible film was given only occasionally to those in late middle age. Except for patients under the age of 10 years where prescriptions were more common for young boys and the 40–49-year age group where the prescriptions were equal for both genders, vitamin D is more commonly given to women.
It is the very young and the older predominantly female population that appear to be the recipients of higher dose prescriptions for calciferol. Infants are often born with low levels of vitamin D, which were not a concern when breastfed and exposed to sunlight; this situation, however, is no longer the norm.Citation49 As the vitamin D content of breast milk is dependent on maternal vitamin D status, which is often low, and sun exposure may be restricted for infants living at higher latitudes or for cultural or other reasons, infants are particularly vulnerable to vitamin D deficiency.Citation49 The prescribing of vitamin D in the youngest age group, and for boys, may be in line with the increased recommendations for children, which doubled from 200 IU to 400 IU for infants, children and adolescents to accommodate the decrease in sunlight exposure and increased incidence of rickets for inner-city children.Citation38 The problem of vitamin D deficiency during pregnancy, which can increase the risk of pre-term and low birthweight infants, has arisenCitation50 and in light of concerns over possible risks of giving pregnant women higher doses of vitamin D, supplementation for preterm and low-birthweight infants has been recommended to curb the complications of infant vitamin D deficiency.Citation51 Breastfeeding under such circumstances may not be protective if mothers have low vitamin D levels.Citation49 The WHO has added its voice to the recommendations for infant supplementation.Citation49 The guidelines are, however, not implemented across the board, and less than half of United States primary care practitioners recommend paediatric supplementation.Citation33 Not everyone agrees with the necessity for childhood supplementation, and in the United Kingdom, where costs of testing and supplementation are borne by the state, there are concerns about unnecessary testing and prescribing, and the concomitant additional expenditure.Citation35
At the other end of the age scale, there is research proposing that vitamin D supplementation is associated with decreased cardiovascular mortality, diabetes, risk of infection and multiple cancers,Citation12,Citation13,Citation36,Citation52 all associated with increasing age. Vitamin D has been found to play a crucial role in the health of the immune system and in promoting the production of antimicrobial monocytes and neutrophils, which tends to decline with increasing age.Citation1 With increasing age, exposure to sunlight may be limited due to reduced outdoor activity and increased skin sensitivity, and dermal production of vitamin D is reduced because of atrophic skin changes and decreased renal function.Citation53 The changes place both genders at risk and have been postulated to lead to severe adverse consequences such as osteoporosis, breast, colon and prostate cancers and hypertension.Citation53 Chronic kidney disease equally places both genders at increased risk of osteoporosis and increased requirement for vitamin D.Citation54 Clinical trials have demonstrated that 800 IU (20 μg) per day of vitamin D in combination with 1 200 mg calcium reduced the risk of fractures due to falls in the institutionalised elderly, who are not ambulatory or exercising, and that single doses of 100 000 IU orally every fourth month, without calcium, reduces fracture risk in mobile community-dwelling individuals over 65 years of age.Citation53 Another study suggested a three-year combined programme of denosumab (a monoclonal antibody) and vitamin D supplementation for the treatment of osteoporosis and rheumatoid arthritis.Citation55 Vitamin D and calcium combinations are frequently self-prescribed for osteoporosis but were not investigated for this study as the aim was to focus on the increased and multiple prescribing recommendations for vitamin D alone. It is acknowledged, however, that vitamin D and calcium combinations with or without other pharmaceuticals are often prescribed for women concerned about osteoporosis.Citation55
Age-related vitamin D deficiency has been found to be prevalent in South Africa, with those over 65 years being particularly vulnerable to deficiency.Citation43 This study showed that private practitioner prescribing of vitamin D in South Africa increased with age and, except for the 40–49-year age group, prescriptions for women outweighed those for men. This might suggest that practitioners are reacting to older female patient concerns regarding the impact of vitamin D deficiencies, or are themselves concerned about vitamin D deficiencies in this population group, thus initiating the conversation about supplementation of vitamin D. Vitamin D deficiency has been associated with higher incidences of breast cancer among women and lower survival rates.Citation16,Citation17,Citation52 Women have a lower bone density than men and are more prone to fall-related fractures due to osteoporosis, particularly in the post-menopausal years.Citation56 Vitamin D-related osteopenia and osteoporosis are not uncommon, and vitamin D deficiency appears to be more common in women, but treatable with supplementation.Citation57 There is a case for additional vitamin D for older people, of both genders;Citation53 however, in this study, prescriptions were more frequently given to women.
There is a lack of consensus on the appropriate vitamin D supplement dosage.Citation1 Although the higher dose of 50 000 IU capsules or tablets appears to be the predominant prescribing practice for South Africa, not all researchers agree that this is necessary. One study found that a single loading dose followed by a low daily maintenance dose was equally effective with the possibility of fewer high-dose risks.Citation36 Another study by Kearns et al. (2014), however, found that daily intake may be difficult to comply with and larger single doses were more effective for eradication of vitamin D deficiency.Citation58 They also found that single vitamin D3 doses in excess of 300 000 IU are most effective at improving vitamin D status and suppressing compensatory parathyroid hormone concentrations, which draw calcium from bones, although gastrointestinal complaints were reported by a few patients at higher doses of vitamin D intake.
In South Africa, there is a wide population group variation in vitamin D receptor genes, ethnicity, and ability to absorb ultraviolet rays and synthesise vitamin D, in addition to variations in disease or treatment responses.Citation43 South Africa spans latitudes from 22.34 S to 34.28 S and has a wide variation in ultraviolet light exposure, which further impacts upon the synthesis of vitamin D, a situation that demonstrates the complex interactions between genetics and the environment.Citation43 Although there appears to be a correlation between frequent sun exposure and a reduction in certain cancers, such as colorectal, prostate, breast cancer and non-Hodgkin's lymphoma, this may or may or may not be due to the effects of the conversion of sunlight to vitamin D.Citation59 Sunlight also has an effect on circadian rhythms and the degradation and utilization of folic acid, the beneficial effects of which may not have been taken into account.Citation59 It should also be considered that in the right hands prescribed supplementation is generally safe, but high doses of Vitamin D have the potential for cumulative toxicity. The public perception of need might drive potentially dangerous over-the-counter self-medication.Citation60 Whether vitamin D plays an important role in protection against the range of diseases that currently constitute a burden on the health services in South Africa or whether there are more complex factors at play needs further investigation before global population-based recommendations can be made.Citation43
The study had limitations in that it covered a period of only one year, and focused only on private prescribing of vitamin D and vitamin D analogues and with a single medical aid administrator, which did not disclose the patient ICD-10 codes and as such can only provide a snapshot picture of the total vitamin D prescribing practice for this specific population. Furthermore, no clinical information, such as the patient vitamin D blood levels, were available in the database. There are also numerous registered and unregistered products available OTC in South Africa that contain low doses of vitamin D in combination with other vitamins, minerals and/or herbal products. This is a large market in South Africa and difficult to quantify as these products are sold through various distribution channels. The use of these products did not form part of this study.
Conclusion
Vitamin D is used across the age range, and there are numerous prescribers and dispensers. Most patients received their prescriptions from a pharmacy as opposed to a hospital or medical practitioner. The number of patients receiving prescribed vitamin D or vitamin D analogues was directly correlated with increasing age. The practice appears to be that of repeat and long-term use of vitamin D, in older age groups and particularly women, suggesting the perceived efficacy of the additional supplementation. Preventing the most common cancers and fragility fractures with better nutritional intervention could potentially save not only lives but a large amount of money that could be redirected towards other prevention and treatment strategies. As the cost of additional supplements is relatively small compared with treatment of deficiency disorders, vitamin D could have broad and positive effects for very little outlay (ZAR 130.79/US$ 9.06 per prescription), thus the strategy of a wider cost-effective rollout of supplementation may be worth consideration. Further investigations of the current total use and possible future benefits of vitamin D supplementation may be warranted.
Acknowledgements
The authors would like to thank the medical aid administrator for providing the data for the study.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Bivona G, Agnello L, Ciaccio M. The immunological implication of the new vitamin D metabolism. Cent Eur J Immunol. 2018;43(3):331–4. doi:https://doi.org/10.5114/ceji.2018.80053. PubMed PMID: 30588177; PubMed Central PMCID: PMCPMC6305614.
- Holick MF. Resurrection of vitamin D deficiency and rickets. J Clin Invest. 2006;116(8):2062–72. Available from: http://www.jci.org. doi: https://doi.org/10.1172/JCI29449
- Owusu JE, Islam S, Katumuluwa SS, et al. Cognition and vitamin D in Older African-American Women- Physical performance and Osteoporosis prevention with vitamin D in older African Americans Trial and Dementia. J Am Geriatr Soc. 2019;67(1):81–6. doi:https://doi.org/10.1111/jgs.15607. PubMed PMID: 30359476.
- Dhaliwal R, Mikhail M, Usera G, et al. The relationship of Physical performance and Osteoporosis prevention with vitamin D in older African Americans (PODA). Contemp Clin Trials. 2018;65:39–45. doi:https://doi.org/10.1016/j.cct.2017.11.015. PubMed PMID: 29221945; PubMed Central PMCID: PMCPMC5803298.
- Bartley J, Garrett J, Camargo CA, Jr., et al. Vitamin D3 supplementation in adults with bronchiectasis: a pilot study. Chron Respir Dis. 2018;15(4):384–92. doi:https://doi.org/10.1177/1479972318761646. PubMed PMID: 29490469; PubMed Central PMCID: PMCPMC6234573.
- Millen AE, Voland R, Sondel SA, et al. Vitamin D status and early age-related macular degeneration in postmenopausal women. Arch Opthalmol. 2011;129(4):481–9. doi: https://doi.org/10.1001/archophthalmol.2011.48
- Jiménez-Sousa MÁ, Martínez I, Medrano LM, et al. Vitamin D in human immunodeficiency virus infection: influence on immunity and disease. Front Immunol. 2018;9(458). doi:https://doi.org/10.3389/fimmu.2018.00458.
- Aggarwal A, Feldman D, Feldman BJ. Identification of tumor-autonomous and indirect effects of vitamin D action that inhibit breast cancer growth and tumor progression. J Steroid Biochem Mol Biol. 2018;177:155–8. doi:https://doi.org/10.1016/j.jsbmb.2017.07.003. PubMed PMID: 28710021; PubMed Central PMCID: PMCPMC5764828.
- AlFaris NA, ALkehayez NM, AlMushawah FI, et al. A descriptive study of vitamin D and other nutritional factors in breast cancer patients in Saudi Arabia. Saudi Med J. 2018;39(6):564–71. doi: https://doi.org/10.15537/smj.2018.6.21902. PubMed PMID: 29915850; PubMed Central PMCID: PMCPMC6058747.
- Baumann M, Dani SU, Dietrich D, et al. Vitamin D levels in Swiss breast cancer survivors. Swiss Med Wkly. 2018;148:w14576. doi:https://doi.org/10.4414/smw.2018.14576. PubMed PMID: 29376548.
- Bintintan VV. Vitamin D as a potential therapeutic target and prognostic marker for colorectal cancer. EBioMedicine. 2018;31:11–12. doi:https://doi.org/10.1016/j.ebiom.2018.04.015. PubMed PMID: 29724656; PubMed Central PMCID: PMCPMC6013779.
- Chen Y, Sun Z, Xu J, et al. Vitamin D and DDX4 regulate the proliferation and invasion of ovarian cancer cells. Oncol Lett. 2018;16(1):905–9. doi:https://doi.org/10.3892/ol.2018.8718. PubMed PMID: 29963162; PubMed Central PMCID: PMCPMC6019908.
- de La Puente-Yague M, Cuadrado-Cenzual MA, Ciudad-Cabanas MJ, et al. Vitamin D: and its role in breast cancer. Kaohsiung J Med Sci. 2018;34(8):423–7. doi:https://doi.org/10.1016/j.kjms.2018.03.004. PubMed PMID: 30041759.
- Fathi N, Ahmadian E, Shahi S, et al. Role of vitamin D and vitamin D receptor (VDR) in oral cancer. Biomed Pharmacother. 2019;109:391–401. doi:https://doi.org/10.1016/j.biopha.2018.10.102. PubMed PMID: 30399574.
- Ferrer-Mayorga G, Larriba MJ, Crespo P, et al. Mechanisms of action of vitamin D in colon cancer. J Steroid Biochem Mol Biol. 2019;185:1–6. doi:https://doi.org/10.1016/j.jsbmb.2018.07.002. PubMed PMID: 29981368.
- Hu K, Callen DF, Li J, et al. Circulating vitamin D and overall survival in breast cancer patients: a dose-response meta-analysis of cohort studies. Integr Cancer Ther. 2018;17(2):217–25. doi:https://doi.org/10.1177/1534735417712007. PubMed PMID: 28589744; PubMed Central PMCID: PMCPMC6041929.
- Ismail A, El-Awady R, Mohamed G, et al. Prognostic significance of serum vitamin D levels in Egyptian females with breast cancer. Asian Pac J Cancer Prev. 2018;19(2):571–6. doi:https://doi.org/10.22034/APJCP.2018.19.2.571. PubMed PMID: 29481024; PubMed Central PMCID: PMCPMC5980952.
- LaRocca CJ, Warner SG. A new role for vitamin D: the enhancement of oncolytic viral therapy in pancreatic cancer. Biomedicines. 2018;6(4):104. doi:https://doi.org/10.3390/biomedicines6040104. PubMed PMID: 30400571; PubMed Central PMCID: PMCPMC6316500.
- Maj E, Filip-Psurska B, Milczarek M, et al. Vitamin D derivatives potentiate the anticancer and anti-angiogenic activity of tyrosine kinase inhibitors in combination with cytostatic drugs in an A549 non-small cell lung cancer model. Int J Oncol. 2018;52(2):337–66. doi:https://doi.org/10.3892/ijo.2017.4228. PubMed PMID: 29345296; PubMed Central PMCID: PMCPMC5741374.
- Santucci KL, Baust JM, Snyder KK, et al. Dose escalation of vitamin D3 yields similar cryosurgical outcome to single dose exposure in a prostate cancer model. Cancer Control. 2018;25(1):107327481875741. doi:https://doi.org/10.1177/1073274818757418. PubMed PMID: 29480024; PubMed Central PMCID: PMCPMC5933822.
- Zhu Y, Chen P, Gao Y, et al. MEG3 activated by vitamin D inhibits colorectal cancer cells proliferation and migration via regulating clusterin. EBioMedicine. 2018;30:148–57. doi:https://doi.org/10.1016/j.ebiom.2018.03.032. PubMed PMID: 29628342; PubMed Central PMCID: PMCPMC5952405.
- Shahvazi S, Soltani S, Ahmadi SM, et al. The effect of vitamin D supplementation on prostate cancer: a systematic review and meta-analysis of clinical trials. Horm Metab Res. 2019;51(1):11–21. doi:https://doi.org/10.1055/a-0774-8809. PubMed PMID: 30522147.
- Ralaidovy AH, Gopalappa C, Ilbawi A, et al. Cost-effective interventions for breast cancer, cervical cancer, and colorectal cancer: new results from WHO-CHOICE. Cost Eff Resour Alloc. 2018;16(38). doi:https://doi.org/10.1186/s12962-018-0157-0. PubMed PMID: 30450014; PubMed Central PMCID: PMCPMC6206923.
- Rekha RS, Mily A, Sultana T, et al. Immune responses in the treatment of drug-sensitive pulmonary tuberculosis with phenylbutyrate and vitamin D3 as host directed therapy. BMC Infect Dis. 2018;18(1):303. doi:https://doi.org/10.1186/s12879-018-3203-9. PubMed PMID: 29973153; PubMed Central PMCID: PMCPMC6033279.
- Rondanelli M, Miccono A, Lamburghini S, et al. Self-care for common colds: the pivotal role of vitamin D, vitamin C, zinc, and echinacea in three main immune interactive clusters (physical barriers, innate and adaptive immunity) involved during an episode of common colds—practical advice on dosages an. Evid Based Complement Altern Med. 2018;2018:1–36. doi:https://doi.org/10.1155/2018/5813095.
- Major G, Ling R, Searles A, et al. The costs of confronting osteoporosis: cost study of an Australian fracture liaison service. JBMR Plus. 2019;3(1):56–63. doi:https://doi.org/10.1002/jbm4.10046. PubMed PMID: 30680364; PubMed Central PMCID: PMCPMC6339551.
- Harvey NC, McCloskey E, Kanis JA, et al. Cost-effective but clinically inappropriate: new NICE intervention thresholds in osteoporosis (Technology Appraisal 464). Osteoporos Int. 2018;29(7):1511–3. doi:https://doi.org/10.1007/s00198-018-4505-x. PubMed PMID: 29947864; PubMed Central PMCID: PMCPMC6037288.
- Masters N. Overenthusiastic prescribing of vitamin D, the sunlight vitamin. Br J Gen Pract. 2018;68(677):567. doi:https://doi.org/10.3399/bjgp18X699941. PubMed PMID: 30498145; PubMed Central PMCID: PMCPMC6255217.
- Kung AWC, Lee K-K. Knowledge of vitamin D and perceptions and attitudes toward sunlight among Chinese middle-aged and elderly women: a population survey in Hong Kong. BMC Public Health. 2006;6(226). doi:https://doi.org/10.1186/1471-2458-6-226.
- Ferguson LR. Calcium and/or vitamin D supplementation: could they affect your risks of colorectal cancer development or progression? Ann Transl Med. 2018;6(Suppl 1):S4. doi:https://doi.org/10.21037/atm.2018.08.29. PubMed PMID: 30613580; PubMed Central PMCID: PMCPMC6291608.
- Wicherts IS, Boeke AJP, van der Meer IM, et al. Sunlight exposure or vitamin D supplementation for vitamin D-deficient non-western immigrants: a randomized clinical trial. Osteoporosis Int. 2011;22:873–82. doi: https://doi.org/10.1007/s00198-010-1343-x
- Truter I, Steenkamp L. Dispensing of vitamin products by retail pharmacies in South Africa: implications for dietitians. South Afr J Clin Nutr. 2016;29(4):133–8. doi:https://doi.org/10.1080/16070658.2016.1219468.
- DelGiudice NJ, Street N, Torchia RJ, et al. Vitamin D prescribing practices in primary care pediatrics: underpinnings from the health belief model and use of web-based Delphi technique for instrument validity. J Pediatr Health Care. 2018;32(6):536–47. doi:https://doi.org/10.1016/j.pedhc.2018.03.003. PubMed PMID: 29804658.
- Ly NP, Litonjua A, Gold DR, et al. Gut microbiota, probiotics, and vitamin D: interrelated exposures influencing allergy, asthma, and obesity? J Allergy and Clin Immunol. 2011;127(5):1087–94. doi: https://doi.org/10.1016/j.jaci.2011.02.015
- Basatemur E, Hunter R, Horsfall L, et al. Costs of vitamin D testing and prescribing among children in primary care. Eur J Pediatr. 2017;176(10):1405–9. doi:https://doi.org/10.1007/s00431-017-2986-9. PubMed PMID: 28803270; PubMed Central PMCID: PMCPMC5602081.
- Gorris MA, Arora H, Lieb DC, et al. A word of caution when prescribing high-dose vitamin D. Am J Med. 2017;130(4):e129–ee30. doi:https://doi.org/10.1016/j.amjmed.2016.10.025. PubMed PMID: 27894737.
- Moyersoen I, Lachat C, Cuypers K, et al. Do current fortification and supplementation programs assure adequate intake of fat-soluble vitamins in Belgian infants, toddlers, pregnant women, and lactating women? Nutrients. 2018;10(2):223. doi:https://doi.org/10.3390/nu10020223. PubMed PMID: 29462926; PubMed Central PMCID: PMCPMC5852799.
- Armstrong C. AAP doubles recommended vitamin D intake in children. Am Fam Physician. 2009;80(2):196–8.
- Kija E, Gidal BE, Shapson-Coe A, et al. Vitamin D abnormalities and bone turn over analysis in children with epilepsy in the Western Cape of South Africa. Seizure. 2019;69:186–92. doi:https://doi.org/10.1016/j.seizure.2019.04.020. PubMed PMID: 31075750.
- Lategan R, Van den Berg VL, Ilich JZ, et al. Vitamin D status, hypertension and body mass index in an urban black community in Mangaung, South Africa. Afr J Prim Health Care Fam Med. 2016;8(1):e1–e5. doi:https://doi.org/10.4102/phcfm.v8i1.1210. PubMed PMID: 28155313; PubMed Central PMCID: PMCPMC5105600.
- Magee MJ, Sun YV, Brust JCM, et al. Polymorphisms in the vitamin D receptor gene are associated with reduced rate of sputum culture conversion in multidrug-resistant tuberculosis patients in South Africa. PLoS One. 2017;12(7):e0180916. doi:https://doi.org/10.1371/journal.pone.0180916. PubMed PMID: 28700743; PubMed Central PMCID: PMCPMC5507304.
- Martineau AR, Nhamoyebonde S, Oni T, et al. Reciprocal seasonal variation in vitamin D status and tuberculosis notifications in Cape Town, South Africa. Proc Natl Acad Sci USA. 2011;108(47):19013–7. doi:https://doi.org/10.1073/pnas.1111825108. PubMed PMID: 22025704; PubMed Central PMCID: PMCPMC3223428.
- Norval M, Coussens AK, Wilkinson RJ, et al. Vitamin D status and its consequences for health in South Africa. Int J Environ Res Public Health. 2016;13(10):1019. doi:https://doi.org/10.3390/ijerph13101019. PubMed PMID: 27763570; PubMed Central PMCID: PMCPMC5086758.
- Truter I. Dispensing of vitamin products by retail pharmacies in South Africa. Value Health. 2015;18(7):A525. doi:https://doi.org/10.1016/j.jval.2015.09.1615. PubMed PMID: 26532943.
- ATC/DDD Index 2018.Internet World Health Organization Collaborating Centre for Drug Statistics Methodology. 2017.cited 14 May 2018 Available from: https://www.whocc.no/atc_ddd_index/.
- MIMS. Monthly Index of Medical Specialities (MIMS). Saxonwold2016.
- Rossiter D, editor. South African Medicines Formulary (SAMF). Cape Town: Health and Medical Publishing Group of the South African Medical Association; 2016, p. 87–8.
- Pretorius L. Does SA’s private healthcare sector only serve 16% of the population?: Africa Check; 2017.cited 2019 15 October Available from: https://africacheck.org/reports/does-sas-private-healthcare-sector-only-provide-care-for-16-of-the-population/.
- World Health Organisation. Vitamin D supplementation in infants Geneva: World Health Organisation; 2019. Available from: https://www.who.int/elena/titles/vitamind_infants/en/.
- Agarwal S, Kovilam O, Agrawal DK. Vitamin D and its impact on maternal-fetal outcomes in pregnancy: a critical review. Crit Rev Food Sci Nutr. 2018;58(5):755–69. doi:https://doi.org/10.1080/10408398.2016.1220915. PubMed PMID: 27558700; PubMed Central PMCID: PMCPMC6056893.
- Kassai MS, Cafeo FR, Affonso-Kaufman FA, et al. Vitamin D plasma concentrations in pregnant women and their preterm newborns. BMC Pregnancy Childbirth. 2018;18(1):412. doi:https://doi.org/10.1186/s12884-018-2045-1. PubMed PMID: 30348112; PubMed Central PMCID: PMCPMC6198501.
- Going CC, Alexandrova L, Lau K, et al. Vitamin D supplementation decreases serum 27-hydroxycholesterol in a pilot breast cancer trial. Breast Cancer Res Treat. 2018;167(3):797–802. doi:https://doi.org/10.1007/s10549-017-4562-4. PubMed PMID: 29116467; PubMed Central PMCID: PMCPMC6381934.
- Mosekilde L. Vitamin D and the elderly. Clin Endocrinol. 2005;62(3):265–81. doi:https://doi.org/10.1111/j.1365-2265.2005.02226.x.
- Liu C, Li H. Correlation of the severity of chronic kidney disease with serum inflammation, osteoporosis and vitamin D deficiency. Exp Ther Med. 2019;17(1):368–72. doi:https://doi.org/10.3892/etm.2018.6916. PubMed PMID: 30651805; PubMed Central PMCID: PMCPMC6307476.
- Suzuki T, Nakamura Y, Kato H. Calcium and vitamin D supplementation with 3-year denosumab treatment is beneficial to enhance bone mineral density in postmenopausal patients with osteoporosis and rheumatoid arthritis. Ther Clin Risk Manag. 2019;15:15–22. doi:https://doi.org/10.2147/TCRM.S182858. PubMed PMID: 30588001; PubMed Central PMCID: PMCPMC6302805.
- Whitehead D, Keast J, Montgomery V, et al. A preventative health education programme for osteoporosis. J Adv Nurs. 2004;47(1):15–24. doi: https://doi.org/10.1111/j.1365-2648.2004.03058.x
- Shahnazari B, Moghimi J, Foroutan M, et al. Comparison of the effect of vitamin D on osteoporosis and osteoporotic patients with healthy individuals referred to the Bone Density Measurement Center. Biomol Concepts. 2019;10(1):44–50. doi:https://doi.org/10.1515/bmc-2019-0005. PubMed PMID: 30956224.
- Kearns MD, Alvarez JA, Tangpricha V. Large, single-dose, oral vitamin D supplementation in adult populations: a systematic review. Endocr Pract. 2014;20(4):341–51. doi:https://doi.org/10.4158/EP13265.RA. PubMed PMID: 24246341.
- Van der Rhee H, Coebergh JW, De Vries E. Is the prevntion of cancer by sun exposure more than just the effect of vitamin D? A systematic review of epidemiological studies. Eur J Cancer. 2013;49(6):1422–36. doi: https://doi.org/10.1016/j.ejca.2012.11.001
- Rajakumar K, Reis EC, Holick MF. Dosing error with over-the-counter vitamin D supplement: a risk for vitamin D toxicity in infants. Clin Pediatr. 2013;52(1):82–5. doi:https://doi.org/10.1177/0009922812439245. Epub 2012/04/12. PubMed PMID: 22492833; PubMed Central PMCID: PMCPMC3396753.
