ABSTRACT
Introduction
Hodgkin lymphoma (HL) involving the Waldeyer's ring (WR) and other extranodal head and neck sites are rare. We report our experience and PubMed literature review.
Methods
Retrospective single institution cohort study using lymphoma data base and PubMed literature search using twenty-six various search terms.
Results
Twenty-nine patients were treated in our institution (1975–2018). Male:Female 22:7, median age at diagnosis 33 years (15–64), stages I–II:III–IV 25:4. Sites were nasopharynx (10), tonsil (9), parotid (5), mandible (2) and others (3). 20/29 patients received radiation therapy, 22/29 received chemotherapy. Ten years overall-survival and progression-free survival are 92% and 66% respectively. PubMed search showed 8766 citations and identified 357 patients including our patients. Male:Female 199:131, median age 45 years (5-89). Stages I–II in 286 (80%). Involvement was nasopharynx 109 (30.5%), tonsil 67 (18.8%), parotid 58 (16.2%), thyroid 45 (12.6%), adenoid 10 (2.8%), mandible 10 (2.8%) and others in 58 (16.2%). Pathology: mixed cellularity 99 (27.7%), nodular sclerosis 88 (24.6%), nodular lymphocyte-predominant 56 (15.7%), lymphocyte rich 25 (7%), classical-HL-not otherwise specified 16 (4.5%) and lymphocyte depleted 7 (2%) patients. Treatment details are available for 233 patients; 165 (46%) received radiation therapy, 137 (38%) chemotherapy. Complete remission in 208 (58%), progressive disease 14 (4%), no information 135 (38%). Overall, treatment failure in 54 (15%). Thirty (8.4%) have died; 21 disease related. KM overall-survival at 5 and 10 years was 88.5% and 77.6% respectively.
Conclusion
This largest report showed that HL involving extranodal head and neck sites is not very uncommon and has excellent prognosis.
Introduction
Hodgkin lymphoma (HL) represents 3.5% of all the cancers diagnosed in the Kingdom of Saudi Arabia [Citation1]. Most HL arises in a lymph node and current multiagent anthracycline-based chemotherapy with or without radiation therapy (RT) can cure 73%–98% patients depending on the stage and other risk factors [Citation2]. Waldeyer’s ring (WR) is an anatomical term collectively describing the lymphoid tissue in the pharynx. WR consists of pharyngeal tonsils (adenoid), tubal tonsil (where each Eustachian tube open), palatine tonsils (commonly called ‘the tonsils’ in the oropharynx), and lingual tonsils (on the posterior part of the tongue). It is considered an extranodal site but not an extralymphatic site [Citation3]. Although the head and neck area lymph nodes are the most common site of disease, unlike non-Hodgkin lymphoma, the involvement of extranodal head and neck sites (ENHNS) including WR is an uncommon observation.
There are only limited case series of five or more patients addressing the extranodal head and neck HL and especially WR involvement by HL [Citation4–16]. Most of the literature are case reports. It is difficult to conclude the clinical presentation, management, and outcome of these cases due to the paucity of literature and missing information. Another limitation is that cases are reported as unique findings without reporting and documenting proper risk factors, detailed treatment, and long term outcomes, needed for outcome prediction for HL. In this paper, we report our experience and provide a comprehensive search of the available literature, and showed the limitation of the literature.
Methods
Patients, material, and methods
This study was part of a prospective/retrospective non-Hodgkin and Hodgkin lymphoma database, approved by the Institutional Research Advisory Council (RAC)’ of King Faisal Specialist Hospital & Research Center, Riyadh, Kingdom of Saudi Arabia. (Clinical Trials.gov Identifier: NCT00538551). Hospital Tumor Registry (data captured since 1975) was used to identify the patients. The manuscript was also approved by the RAC and all the authors. All patients and/or their guardians provided informed consent for all treatments and procedures as per institutional requirements. All HL patients seen at our institution from 1975 to December 2014 were identified from the Oncology Research Unit based Hospital Tumor Registry. Using Lymphoma Data Base, additional patients from 2015 to 2018 were captured. All pathology slides were reviewed at the initial diagnosis by experienced hematopathologists. Paper and electronic charts were reviewed to collect the required data. Kaplan-Meier (KM) method was used to calculate overall survival (OS) and progression-free survival (PFS).
The search of the literature methods
Using PubMed advanced search, 26 various terms were used and cross-matched with ‘Hodgkin’ (in humans / all languages) to capture all potential extranodal head and neck sites (search date 14 February 2018). These terms were parotid, palate, palatine, tonsil, tonsillar, nose, eye, ear, thyroid, laryngeal, hypopharyngeal, pharyngeal, oropharyngeal, nasopharynx tongue, head and neck, extranodal, nasal, mandible, jaw, face, cheek, oral, maxilla, maxillary and trachea. Relevant abstracts and full text if available (online, purchase from journal site, institution library, or interlibrary loan) were reviewed by the team to identify the clinical presentation, management, and outcome in a uniform way and entered into a table. Cross-references were also reviewed as needed. References in each article were reviewed and e-mails for full text were sent to the principal author whenever possible. For our analysis, any citation / abstract/full text that provided at least three out of the following seven characteristics was included; pathology, site, gender, age, stage, treatment, and outcome (alive/dead / follow up information). Individual data were extracted from these papers/abstract / Mesh search. Stages were assigned if it was not provided in the paper but sufficient clinical/staging information was available to stage. Kaplan-Meier (KM) method was used to calculate both OS (death from all causes) and disease-specific OS (DS-OS); death due to disease. DS-OS was chosen as five papers with very long follow-up also reported patients who died of non-disease related causes. When survival outcome was reported for the entire group, but not specifically for the individual patient, it was recorded but reported for the group only that was included in the entire analysis and the individual patient/site was marked as unknown.
Results
Institutional data
Patients’ characteristics
From 1975 to 2014, Hospital Tumor Registry identified 3275 HL patients, diagnosed/treated in our institution. Twenty-three patients (0.7%) met the defined criteria of WR and other extranodal HL of head and neck. From January 2015 to January 2019, another 6 patients (using Lymphoma DataBase) met the inclusion criteria, bringing the total to 29 patients. The patient’s characteristics at diagnosis and treatment details are shown in . Male:female ratio is 3:1 (22 (76%) males and 7(24%) females). Median age at diagnosis was 33 years (range 15–64 years); 12 (41%) out of 29 patients were <30 years at diagnosis. Eight patients had no lymph node involvement at presentation. 2/29 had extranodal involvement at relapse only (occipital and nasopharynx). Before 2003, all patients had a CT scan with or without gallium for staging. As the 18F-fluorodeoxyglucose positron emission computer tomography (FDG-PET/CT scan) became available and approved in the institution for HL staging and response evaluation, from 2004 onwards, 14 out of 17 patients had FDG-PET/CT scan for staging and response evaluation.
Table 1. Patient’s characteristic of our institution.
Treatment, response, and outcome
Details are summarized in . Primary chemotherapy was adriamycin, bleomycin, vinblastine, and dacarbazine (ABVD) in 19 patients, 3 others (1 each) received mechlorethamine, vincristine, procarbazine, prednisone (MOPP)/ABVD (in 1986), MOPP/ABV (in 1993), and cyclophosphamide, vincristine, procarbazine, prednisone (COPP)/ABVD (in 2016) (she had ABVD × 6 in 2011 as 1st line treatment and relapsed in 2016 with nasopharynx involvement). Response to treatment was complete response (CR) in 27 patients (93%) and partial response (PR) or progressive disease (PD) in 2 (7%). Treatment failure was observed in six patients: Three had extranodal involvement (chin in 2 and parotid in 1) and three had WR involvement. Two had progressive disease (PD)/refractory diseases and four had relapsed disease (one relapsed within 3 months). Three patients underwent high dose chemotherapy (HDC) and autologous stem cell transplantation (auto-SCT) and all are alive in CR. Two relapsed patients received salvage chemotherapy without HDC auto-SCT, one achieved CR (refused HDC auto-SCT) and the other progressed and died.
20/29 patients received RT. Nine (45%) patients received their treatment before 1994 and 5 of them received RT alone as the primary treatment. Only one patient in 2001 (completely excised right parotid gland HL) was treated with RT alone. The dose of radiation varied from 30.6 to 40Gy, with a trend towards dose de-escalation in recent years. RT dose was 30.6Gy in 10 patients, 34 to 36Gy in 5 patients, 40Gy in 4 patients, and in one patient the RT dose could not be identified. Patients who achieved CR on chemotherapy received RT dose around 30Gy, whereas those with PR on chemotherapy or treated with RT alone received higher RT dose. Extended RT field (EFRT) was used in the early years of the study in 3 patients, involved field (IFRT) in 15, and later involved site (ISRT) in 3 patients. Over the years of the study, RT treatment technique has evolved from conventional 2D (8 patients), to 3D-conformal in 6 patients, and intensity-modulated RT (IMRT) / Rapidarc (RA) in 6 patients.
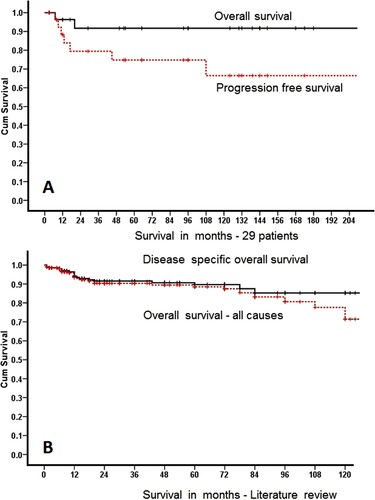
A total of two patients have died; one due to relapsed disease (20 months), the other died in CR (7 months) of pulmonary tuberculosis. The median follow-up of all alive patients is 93 months (12–300); 5/27 alive patients have <24 months follow-up. KM estimate of 5 years OS and PFS is 92% and 75%, while for 10 years, it is 92% and 66% respectively ((A)).
Results of the literature search
Availability of data
We used the search term ‘Hodgkin’ as this resulted in the highest numbers of article search results compared to other terms; Hodgkin’s, Hodgkin lymphoma, Hodgkin’s lymphoma, or Hodgkin disease. The 26 search terms were cross-matched with ‘Hodgkin’ that resulted in 8766 citations (many common citations in various search terms) and all of them were reviewed individually. Total articles identified (in bracket) with each search term on PubMed were: Parotid (222), palate (118), palatine (164), tonsil (236), tonsillar (269), nose (260), eye (485), ear (100), thyroid (838), laryngeal (199), hypopharyngeal (21), pharyngeal (303), oropharyngeal (227), nasopharynx (153), tongue (106), head and neck (725), extranodal (2013), nasal (476), mandible (71), jaw (95), face (209), cheek (24), oral (1226), maxilla (38), maxillary (135) and trachea (53). A total of 150 references were included in the final analysis as they provided the minimum required information. Full texts were available for 108 references. References before 1980 had limited full-text availability. Thirty-one references were only abstracts and 11 references were citation/citation and cross-reference with additional information. Some papers, likely with large numbers of patients were unavailable despite all our efforts [Citation15]. Feinstein et al. published 75 patients with thyroid Hodgkin lymphoma reported to the National Cancer Institute’s Surveillance, Epidemiology, and End Result (SEER) Program Data Base, a collective data of various tumor registries in the USA [Citation16]. This paper is not included due to missing individual patient information.
Patients’ characteristics and site involvement
We identified 357 patients (including our 29 patients) with extranodal HL of head and neck ( and ). A large number of patients had missing variables as shown in Supplemental Table 1. Out of 357 patients, there were 199 (55.7%) male, 131 (36.7%) female, and 27 (7.6%), gender was not available. The median age was 45 years (range 5–89 years). Limited stage (I–II) was reported in 286 (80%) patients. Most common sites were nasopharynx in 109 (30.5%), tonsil in 67 (18.8%), parotid in 58 (16.2%), thyroid in 45 (12.6%), adenoid in 10 (2.8%), mandible in 10 (2.8%), and others in 58 (16.2%) patients.
Table 2. Characteristics of 357 patients.
Table 3. Treatment and outcome of 357 patients.
Pathology
Precise pathology with a specific site was available for 304 patients (85%) ( and Appendix 1). Some papers provided various histological subtypes or detailed pathology as a group without the site. Many reports only mentioned ‘Hodgkin lymphoma’ while some stated classical HL (cHL) without further sub-classification. Reported pathology was mixed cellularity in 99 (27.7%) patients followed by nodular sclerosis in 88 (24.6%), nodular lymphocyte predominant (NLPHL) in 56 (15.7%), lymphocyte rich in 25 (7%), cHL-not otherwise specified in 16 (4.5%), lymphocyte depleted in 7 (2%) patients, ‘Hodgkin lymphoma’ (no other details provided) in 63 (17.6) and HL-interfollicular in 3 (1.5%) patients.
Table 4. Pathological distribution of HL at various anatomical sites in 304 patients.
Treatment and outcome of 357 patients
Appendix 1 provides comprehensive patients’ treatment and outcomes. Many large reports discussed only the pathological characteristics of this entity. Treatment details are available for only 233 (65%) patients, with accurate staging in 180 out of 233 patients. A total of 165 (46%) patients received RT; sole management after surgical resection/biopsy in 79 (22%) patients and another 86 (24%) with chemotherapy. Out of 137 (38%) patients who received some type of chemotherapy, details are available for only 90 (25%) patients. ABVD was the most commonly reported chemotherapy, used in 53 (15%) patients, ABVD/ABV in combination with MOPP or COPP in 10 patients, MOPP alone in 12, cyclophosphamide, adriamycin, vincristine, prednisone (CHOP) or CHOP-like in 6 patients and other combinations occasionally.
To check the shift in the treatment paradigm over the last 20 years, we arbitrarily divided these patients into two groups; those reported between 1961 and 1999 and those between 2000 and 2019. For stage I only (73 patients), RT as the sole treatment was reported in 28 out of 36 patients (78%) in the 1961–1999 group compared to 17 out of 37 patients (46%) (P = 0.005). For stage I–II (158 patients), RT as the sole treatment was reported in 46 out of 73 patients (63%) in the 1961–1999 group compared to 22 out of 85 (26%) in the 2000–2019 group (P= <0.001). For 22 patients with stages III–IV, the treatment was similar for all the patients as all received combination chemotherapy with or without RT, except for 2 patients.
After treatment, CR was reported in 208 (58%), progressive disease in 14 (4%) and no information was available in 135 (38%). Overall, treatment failure (progressive disease or relapse) was observed in 54 (15%). A total of 30 (8.4%) patients had died; 21 (6%) due to disease and another 9 (2.5%) due to non-disease related causes. Information related to both treatment failure and stages were available/extracted for 206 patients. Treatment failure for 174 stages I–II patients was 21.3%, significantly lower compared to 46.9% for 32 stages III–IV patients (p = 004). Information related to treatment failure (relapsed or progressive/refractory disease or death due to disease) along with time to failure was available/extracted in 207 patients. For these selected 207 patients, KM OS at 5 and 10 years was 88.5% and 77.6% respectively and KM DS-OS was 90% and 85.3% respectively for these patients ((B)).
As there is a progressive change in the treatment of HL and progressive improvement in the outcome, we grouped these patients into various time frames and checked the reported treatment failure. The observed decrease in treatment failure from 1961–1980 (58.6%), 1981–1990 (41.7%), 1991–2000 (22.9%), 2001–2010 (13%) and 2011–2019 (18%) was clearly showing an improvement over time (p = <0.001). When we grouped various time frames into only two groups, treatment failure during 1961–1985 (57.5%) vs 1986–2019 (18%) remained significant (p = <0.001), indicating that before 1985, significantly higher failure was observed.
An interesting analysis/observation is the finding of the unique distribution of various pathologies at various anatomical sites (). In the nasopharynx area (88 cases), mixed cellularity was present in 38.6% cases but this represented 41.5% of the entire mixed cellularity reported in the cohort of 304 patients. In the parotid gland (56 cases), 44.6% were NLPHL but this represented 52% of the total NLPHL in the entire cohort of 304 patients. Similarly, in the thyroid gland (39 cases), 61.5% of cases were nodular sclerosis, which represented 34% of the total nodular sclerosis in the entire cohort of 304 patients. Reasons for these pathological predilections are not known.
Due to large number of missing variables, we have also created a summary of main clinical presentation and survival outcome finding of all main sites as a quick reference ().
Table 5. Summary of 357 patient’s characteristics and their treatment outcome
Discussion
Our institution is a major tertiary care center in the Kingdom of Saudi Arabia. Hospital Cancer Registry (established in 1975) has a total of > 78,000 cancer patients’ essential data. From 1975 to 2014, Hospital Tumor Registry identified 3275 HL patients, diagnosed/treated in our institution.
We have identified 29 patients; 23 patients (0.7%) from 3275 HL reported in the Cancer Registry and another 6 from the Lymphoma Data Base, making our data the largest reported data with individual patient information. Our patients have all the details of clinical presentation, management, and outcome. Like the international literature, the three most common sites were nasopharynx, tonsil, and parotid gland involvement. Despite the PFS of 75%, overall survival is excellent; 92% at both 5 and 10 years. Like any other large study that has collected this type of rare presentation data over decades, our data collection spanned over 40 years. We faced the same evolution of changing in the staging methodology, pathology specimen processing, non-availability of archival specimens, and treatment variability for various stages over time.
There are only limited reports with both clinical and pathological details with five or more patients as referred above. The largest to date report of Iyengar et al. has not provided individual patient information [Citation9]. Iyengar et al. (MD Anderson, Houston, USA) reported 34 patients (focusing on the clinical outcome); 11 of them have already being reported earlier by Quiñones-Avila et al. [Citation11], who reported 22 patients, focusing on the pathological characteristics. He also reported a significantly higher number of LR in the WR area than what we have observed in our case series and in . Both these large reports are included in the analysis with the 11 duplicate cases as they cannot be separated.
Our literature search has identified 357 cases (including our 29 cases) with complete information as per our criteria. Our main focuses were to identify the detailed clinically relevant data from the available literature and review the patient’s characteristics and treatment outcome. This is the largest and most comprehensively collected search of the data to date. It has provided an important insight into this unique presentation of HL. Over a while, with the emergence and superiority of new chemotherapy combinations with less toxic chemotherapy and chemotherapy + RT over RT alone in early-stage HL, there was a clear shift in the management of these patients; less use of RT as sole management for early-stage HL. Not only this, but a progressive decrease in the number of chemotherapy cycles and a relatively smaller radiation field by newer linear accelerators have also decreased the toxicity without compromising the survival.
This study confirms the excellent outcome of HL (mostly early stage) regardless of the extranodal involvement, as only 10% of deaths have been observed in this review. This is similar to all the early stages, low-risk HL reports. Furthermore, progressive change in the management of HL from radiation alone to multimodality treatment is also notably similar to HL management worldwide. Our observation of decrease in the treatment failure after 2001 is similar to what was observed and reported by the investigators from Canada with the use of modern treatment regimen. They also reported improvement in outcome in all risk groups [Citation2].
Limitations
We have performed a literature search and this should not be confused/mixed with a systematic review, which is a high-quality evaluation of a relatively uniform set of reports. This literature search is intended to capture the diversity of case reports ‘as reported’. Like most retrospective analyses, this search has several limitations. Unavailability of the full manuscript resulted in the exclusion of some studies. Not only this, but many papers are primarily focused on the pathological aspects where treatment and outcomes are not reported, others focused on clinical outcomes with no precise pathological subtype. Almost one-third of the patients have no treatment details or outcome. Survival information is not available for 42% of the patients and survival curves included only 207 patients. Due to the short follow-up in most reports, long term therapy-related complications, especially post RT is missing. This is especially true as the technology, technique, and field of radiation have changed over the decades. This simply provides a comprehensive insight into what is available and the ‘sub-optimal’ information that can be extracted from the current literature.
Despite all these limitations, this is the largest literature search on this topic and has provided important insight on the distributions of HL in the head and neck area, pathological distribution of the disease at various sites, treatment trends, and the outcome over half a century. The search is not intended to comment on the outcome, but primarily to show the reported distribution of HL and to show that this is not as uncommon in the ENHNS as thought, Also, due to diverse pathological types of lymphomas, a proper large size biopsy will be the best way for proper pathological evaluation and HL should be in the differential. This paper will also serve as a reference for future investigators to review the historic and current presentation, management, and outcome of HL at various ENHNS. Our supplemental table will hopefully provide a useful reference for investigators reporting various ENHNS.
Ethics approval and consent to participate
Approved by Institutional ‘Research Advisory Council (RAC)’. King Faisal Specialist Hospital & Research Center, Riyadh, Kingdom of Saudi Arabia. RAC project # 2021-048 lymphoma database. Waiver of signed consent as per RAC (no individual patient identified data / no pictures / verbal consent documented on paper or electronic chart). This waiver of signed consent was for participation in the database collection study and subsequent publications as per RAC guidelines. Consent for publication: Approved by Institutional Research Advisory Counsel for publication # 2190193
Availability of data and materials
Data are a ‘retrospective/prospective database’ and is owned by the institution. This data is under the custody of the principal and co-investigators as per the Institutional Research Advisory Counsel and Research Ethics Committee guidelines. It is not available to the public for sharing. Full or part of this data can be shared after an official request/approval of the institutional Research Advisory Counsel and Research Ethics Committee. All authors had full access to all data.
Authors’ contributions
MA and WE reviewed cases from PubMed and collected data of these patients and helped in manuscript writing. WE is currently at Cairo University, Center of Radiation Oncology and Nuclear Medicine. MSR collected data, helped in manuscript writing. YK collected data related to radiation therapy management, helped in manuscript writing, IM collected data, interpreted data, helped in manuscript writing. SA was the principal investigator, designed research, collected data, analyzed and interpreted data, helped in writing the manuscript.
All procedures followed were per the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Supplemental Material
Download MS Excel (48.6 KB)Acknowledgements
We appreciate Dr. Abida Rehman and Ms. Cherry Colcol from Oncology Research Unit for their valuable contribution in data extraction and entry and Haris Syed for providing proofreading.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Rauf MS, Akhtar S, Maghfoor I. Changing trends of adult lymphoma in the Kingdom of Saudi Arabia – comparison of data sources. Asian Pac J Cancer Prev. 2015;16:2069–2072.
- Moccia AA, Donaldson J, Chhanabhai M, et al. International Prognostic Score in advanced-stage Hodgkin’s lymphoma: altered utility in the modern era. J Clin Oncol. 2012;30:3383–3388.
- Bogaerts M, Deggoujf N, Huart C, et al. Physiology of the mouth and pharynx, Waldeyer’s ring, taste and smell. B-Ent. 2012;8(Suppl 19):13–20.
- Agaimy A, Wild V, Markl B, et al. Intraparotid classical and nodular lymphocyte-predominant Hodgkin lymphoma: pattern analysis with emphasis on associated lymphadenoma-like proliferations. Am J Surg Pathol. 2015;39:1206–1212.
- Anselmo AP, Cavalieri E, Cardarelli L, et al. Hodgkin’s disease of the nasopharynx: diagnostic and therapeutic approach with a review of the literature. Ann Hematol. 2002;81:514–516.
- Azzopardi JG, Evans DJ. Malignant lymphoma of parotid associated with Mikulicz disease (benign lymphoepithelial lesion). J Clin Pathol. 1971;24:744–752.
- Chang KL, Kamel OW, Arber DA, et al. Pathologic features of nodular lymphocyte predominance Hodgkin’s disease in extranodal sites. Am J Surg Pathol. 1995;19:1313–1324.
- Cionini L, Bastiani P, Biti GP, et al. Waldeyer’s ring (WR) involvement in Hodgkin’s disease. Radiother Oncol. 1985;3:299–302.
- Iyengar P, Mazloom A, Shihadeh F, et al. Hodgkin lymphoma involving extranodal and nodal head and neck sites: characteristics and outcomes. Cancer. 2010;116:3825–3829.
- Kapadia SB, Roman LN, Kingma DW, et al. Hodgkin’s disease of Waldeyer’s ring. Clinical and histoimmunophenotypic findings and association with Epstein-Barr virus in 16 cases. Am J Surg Pathol. 1995;19:1431–1439.
- Quinones-Avila Mdel P, Gonzalez-Longoria AA, Admirand JH, et al. Hodgkin lymphoma involving Waldeyer ring: a clinicopathologic study of 22 cases. Am J Surg Pathol. 2005;123:651–656.
- Tiplady CW, Taylor PR, White J, et al. Lymphoma presenting as a parotid tumour: a population-based study of diagnosis, treatment and outcome on behalf of the Scotland and Newcastle Lymphoma Group. Clin Oncol (R Coll Radiol). 2004;16:414–419.
- Todd GB, Michaels L. Hodgkin’s disease involving Waldeyer’s lymphoid ring. Cancer. 1974;34:1769–1778.
- Wang SA, Rahemtullah A, Faquin WC, et al. Hodgkin’s lymphoma of the thyroid: a clinicopathologic study of five cases and review of the literature. Mod Pathol. 2005;18:1577–1584.
- Liu YZ. Radiotherapy of Hodgkin’s lymphoma arising from Waldeyer’s ring–an analysis of 16 cases. Zhonghua Zhong Liu Za Zhi. 1984;6:447–449.
- Feinstein AJ, Ciarleglio MM, Cong X, et al. Parotid gland lymphoma: prognostic analysis of 2140 patients. Laryngoscope. 2013;123:1199–1203.