ABSTRACT
Objectives
Health-related quality of life (HRQL) is a key factor in making anticoagulant treatment decisions. The objective of this study was to assess the HRQL of patients with nonvalvular atrial fibrillation by treatment type: direct oral anticoagulants (DOACs) or vitamin K antagonists (VKAs).
Methods
We carried out a cross-sectional observational study with clinical practice data, gathering demographic and clinical variables. HRQL was measured using the 5-level 5-dimension EuroQol questionnaire (EQ-5D-5L). Differences between the study groups in HRQL as measured by the EQ-5D-5L were analyzed using two-part multivariate regression models. First, using logistic regression, the adjusted probability, p(x), of having perfect health was estimated in each subgroup. Secondly, generalized linear models were used to estimate mean disutility values, w(x), in a population that does not have perfect health, i.e. utility less than 1 or 1-w(x).
Results
We recruited 333 patients, of whom 126 were on DOACs and 207 on VKAs. A significant difference was observed in the EQ-5D-5L anxiety/depression dimension, with a higher percentage of patients classified in the ‘no problems’ category in the DOAC group. The same type of analysis did not identify significant differences in any of the other dimensions (mobility, self-care, usual activities or pain/discomfort).
Discussion
In the multivariate model, utility was significantly higher in the DOAC group than in the VKA group, although the difference was small (0.0121). This difference is attributable to patients on DOACs having less anxiety/depression.
Conclusion
Patients treated with DOACs report a slightly better quality of life than those treated with VKAs.
Introduction
The prevalence of nonvalvular atrial fibrillation increases with age, up to 9% among 80- to 90-year-olds [Citation1]. Its diagnosis and treatment are essential to reduce the risk of thromboembolic stroke, which is 5-fold higher due to stasis of blood in the left atrium [Citation2]. Anticoagulation therapy is the treatment of choice; this is a long-term treatment seeking to reduce the risk of stroke, which for some years has been based on vitamin K antagonists (VKAs) such as warfarin and other coumarin derivatives [Citation3]. Nonetheless, the use of VKAs requires strict monitoring to ensure both its effectiveness in terms of stroke risk reduction and patient safety, given the risk of bleeding associated with over-anticoagulation [Citation4]. Anticoagulation therapy places few limitations on patient lifestyle but does require a certain level of self-discipline in some areas of daily life such as diet and physical activity, as well as attendance to healthcare appointments for international normalized ratio (INR) monitoring. These features of the treatment may impair health-related quality of life (HRQL) [Citation5].
The term HRQL refers to the physical, psychological and social domains of health, perceived as different areas that are influenced by a person's experiences, beliefs, expectations and perceptions [Citation6]. Each of these domains can be measured in objective terms, such as assessing individuals’ functioning, or in subjective terms, assessing patients’ perception of how their objective status is experienced personally [Citation7]. Qualitative studies have confirmed that laboratory tests, frequent medical appointments and anxiety related to potential adverse effects have a negative impact on HRQL [Citation8], and this negative impact may be long term as patients may stay on oral anticoagulation therapy for a long time, sometimes for life.
The treatment scenario has changed since direct oral anticoagulants (DOACs) have become available [Citation4]. DOACs have shown to be effective for the prevention of stroke in patients with atrial fibrillation [Citation9]. Although more expensive, they have the advantage that their follow-up does not require close monitoring [Citation4]. On the other hand, the reduction in healthcare appointments required is sometimes perceived by patients as abandonment, this in itself generating stress. The risk/benefit balance of the two treatment options is currently the subject of debate and patients’ perception of their quality of life is one of the main criteria considered [Citation5]. For this reason, the assessment of HRQL as a function of treatment type is a key factor in clinical decision-making about anticoagulation. On the other hand, to date, there is insufficient data on the satisfaction and HRQL of patients on anticoagulants and the impact new treatments have had in the real world. Studies based on patients treated in clinical practice allow us to measure the real effectiveness achieved with the provision of anticoagulation therapy [Citation10,Citation11]. The organization of the check-ups required while on anticoagulants is also a factor in the perception of patient satisfaction with treatment. Hence, data gathered in this field may be useful for improving the way healthcare services are delivered. The objective of this study was to assess the HRQL of patients with nonvalvular atrial fibrillation treated with DOACs and compare it with that of those treated with VKAs.
Methods
Study design
We conducted a cross-sectional observational study based on clinical practice data, comparing two samples of patients, on VKAs or DOACs, sequentially recruited in Araba Integrated Healthcare Organisation haematology appointments between 1 March 2018 and 30 June 2019. Data were collected on demographic, clinical and HRQL variables. The study protocol was approved by the Araba Clinical Research Ethics Committee (reference number 2017-088).
The study inclusion criteria were: (1) being a patient with nonvalvular atrial fibrillation who had been on anticoagulant therapy for at least 6 months; (2) being at least 18 years old; and (3) providing written informed consent. Patients were excluded if they met any of the following criteria: (1) having difficulties in understanding the language required to participate; (2) being under palliative care; or (3) having mild cognitive impairment defined as more than four errors on Pfeiffer's Short Portable Mental Status Questionnaire (SPMSQ) [Citation12]. The SPMSQ is a brief questionnaire that provides a quantitative objective measure of cognitive functioning of elderly people by counting the number of errors, a score of zero indicating no impairment. It was used to exclude patients who could not reliably complete the survey, four errors being taken to indicate mild cognitive impairment.
Variables
For each patient, we collected data on the following: age, sex, level of education, employment status (yes/no) and type, body mass index (BMI), comorbidities, cardiovascular risk (CHA2DS2-VASc score) [Citation13], as well as current type of anticoagulant therapy, dosage prescribed, date of starting the therapy, history of anticoagulant therapy (type) and concomitant medications (number of drugs). HRQOL was measured using the 5-level 5-dimension format of the EuroQol questionnaire (EQ-5D-5L) [Citation14].
The CHA2DS2-Vasc score was calculated assigning 1 point each for having a history of congestive heart failure, hypertension and/or diabetes mellitus, and 2 points each for being aged ≥75 years old or having a history of stroke or peripheral embolism or transient ischemic attack [Citation13]. The EQ-5D-5L is a standardized generic instrument for measuring HRQL that assesses self-reported health status across five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) and five levels of severity (no problems, slight problems, moderate problems, severe problems and extreme problems). The Spanish version provides utility scores between 0 and 1 based on the preferences assessed in the Spanish general population [Citation14,Citation15]. There are 3125 possible health states, from 11111 (a state of perfect health) to 55555 (a state equivalent to dead). These health states can be converted into a utility index by applying an algorithm developed and validated in the Spanish population by Ramos-Goñi et al. [Citation16].
Statistical analysis
The statistical significance of differences between groups was assessed using Student's t test for normally distributed data and the non-parametric Wilcoxon test for non-normally distributed and ordinal data. The level of significance was set at p < 0.05. Chi-square tests were used to compare contingency tables. Statistical analysis was carried out using R v3.6.1.
Utility measures of HRQL are preference values that patients attach to their overall health status. In clinical trials, utility measures summarize both positive and negative effects of an intervention into one value between 0 (equal to death) and 1 (equal to perfect health) [Citation17]. When quality of life scores are close to 1, and hence, the data are not normally distributed, ordinary least square regression models are not recommended [Citation17]. For this reason, we carried out a two-part regression analysis to compare quality of life measured using the EQ-5D-5L in the two treatment groups under study [Citation17,Citation18]. These models take into account the high percentage of cases in which patients indicated that they were in perfect health, in their responses to the EQ-5D-5L (utility of 1 or level 1 in all five dimensions), a pattern which hinders the use of conventional multivariate models, and they allow us to calculate utilities for each group, u(x). First, using logistic regression, the adjusted probability, p(x), of having perfect health was estimated in each subgroup, perfect health meaning that the patient did not report any limitations in any of the five dimensions of the EQ-5D-5L. Secondly, generalized linear models were used to estimate mean disutility values, w(x), in a population that does not have perfect health, i.e. utility less than 1 or 1-w(x). In the assessment of quality of life with the EQ-5D-5L, disutility is used as the dependent variable instead of utility to avoid negative values. We defined disutility as 1-utility, i.e. w(x) = 1−u(x). Finally, the two parts were combined to calculate utility values using the expression: u(x) = p(x)⋅1 + (1−p(x))⋅(1−w(x)).
As well as being easy to interpret, in the context of the EQ-5D-5L, two-part models have shown better predictive power than other regression models and not only indicate whether there are differences in HRQL between groups, but also provide a measure of the size of these differences. The estimated utilities for the groups studied by two-part models depend on the combination of several categories of covariates. To facilitate the interpretation of the results, differences in utilities associated with the treatments of interest were calculated for the most clinically important subgroups. The difference between groups (diff) associated with the treatment given was calculated by subtracting the utilities estimated by the model for patients on VKAs from those for patients on DOACs: diff = u(DOAC)−u(VKA).
Various different models were analyzed, initially including all variables found to show some degree of association (p < 0.25) with the response variables. Starting from a model including all these variables, the final model was obtained by excluding, one at a time, variables that did not show associations in the combined analysis. Finally, the only variables left in the model were those that showed significance (p < 0.05) in the first or second part of the model. The likelihood ratio test and Akaike information criterion were used to select the best model.
Results
We recruited 333 patients, of whom 126 were on DOACs and 207 on VKAs. As shown in , we did not find statistically significant differences between the groups by age, sex, level of education, employment status or CHA2DS2-VASc score. In contrast, patients treated with VKAs had been significantly more days on anticoagulant therapy, took fewer concomitant medications, and showed better cognitive function on the SPMSQ. A history of stroke was significantly more common in the group treated with DOACs.
Table 1. Clinical and sociodemographic characteristics of patients by type of anticoagulant.
In the unadjusted EQ-5D-5L scores (), there is a notable difference in the anxiety/depression dimension, with a higher percentage of patients classified in the ‘no problems’ category in the DOAC group. The same type of analysis did not identify statistically significant differences in any of the other dimensions (mobility, self-care, usual activities or pain/discomfort). Further, no differences were found in the percentage of patients who reported being in perfect health (utility value of 1 or level 1 in the five dimensions): 25% in both cases. On the other hand, the median utility was higher in the DOAC group, because the loss of utility in patients not in perfect health (utility value other than 1) was lower than in patients on VKAs. This was due to the impact of patients having values higher than 1 in certain EQ-5D-5L dimensions. helps to understand the reason for the differences in median utility, the group on DOAC showing higher densities at disutility values close to zero, while the group treated with VKA appears more represented at the other end of the horizontal axis, characterized by greater utility losses.
Figure 1. Distribution of disutility in patients with less-than-perfect health by type of treatment. DOAC: direct oral anticoagulant; VKA: vitamin K antagonist.
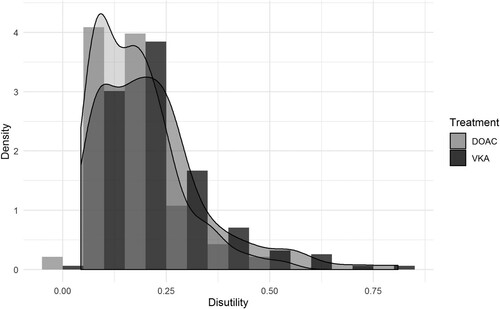
Table 2. Description of EQ-5D-5L results and percentage of level 1 responses in each dimension by type of anticoagulant.
shows the results of the two-part model that included variables which were statistically significant in the univariate analysis, namely, age, sex, number of medications and SPMSQ score as covariates. A history of stroke and having a caregiver were not entered in the final model because they were not significant in an earlier version of the two-part model. As in the unadjusted results, the logistic regression model corresponding to the first step did not indicate significant differences in the probability of perfect health between the treatment groups. In the second part of the model, we adjusted a generalized linear model with a log and gamma family distribution to model the disutilities of patients with less-than-perfect health. Plotting the disutilities of these patients, who reported not having perfect health, showed the highest density of values occurred around 0 (). As indicated in the methods section, we defined disutility as 1-utility. Patients in the VKA group had an OR of 1.30 for having a higher disutility or utility loss, and this was statistically significant.
Table 3. Odds ratios for each variable included in the two-part model explaining the EQ-5D-5L results.
The combined analysis of the two-part model is reported in . Since the objective of the study was to compare the HRQL between two groups formed based on treatment received, the outcome variable calculated was the difference in utility as a function whether the patients were on DOACs or VKAs for various subgroups. The difference found was small in magnitude but statistically significant. Comparing the two groups combining the entire sample regardless of other characteristics studied (base case), the difference was 0.0121. In all subgroups analyzed, defined by a combination of categories of variables, the differences between utilities estimated for patients on the two types of anticoagulants studied (subtracting the utilities for patients on VKAs from those for patients on DOACs) were greater than 0. Given that the confidence intervals do not include zero, we can state that these differences are statistically significant. This is found both in the overall sample and in each of the subgroups.
Table 4. Differences in utilities between patients treated with DOACs or VKAs overall (whole sample) and in subgroups calculated using the two-part model.
Discussion
The main finding of this study is that patients treated with DOACs report better quality of life than those treated with VKAs. Analyzing the results by treatment group in each of the five EQ-5D dimensions, we observed that the differences in utilities are due to the fact that the patients in the DOAC group had less anxiety/depression. The fact that no differences were found in the other dimensions (mobility, self-care, usual activities or pain/discomfort) could be attributable to the type of anticoagulant used not having any influence on them. On the other hand, the lack of differences in the self-care and usual activities dimensions may be linked to the healthcare provided to anticoagulated patients when they are well organized, as is the case with our institution. According to our results, the demands associated with the need for regular testing of patients on VKAs are not reflected in a great loss of quality of life as assessed by the EQ-5D-5L. This may be in part due to the great majority of our patients (92% of the sample) not being in active employment. In contrast, uncertainty about the amount of monitoring received seems to cause patients on VKAs more concern, this being reflected in the EQ-5D-5L anxiety/depression dimension, which is significantly higher than in patients treated with DOAC. It was noteworthy that the loss of utility in patients in the VKA group was due to a higher disutility or utility loss, when the probability of being in perfect health was the same in both groups.
Another notable finding is that, overall, patients with atrial fibrillation on anticoagulants have a high quality of life, indicated by a utility of 0.87, similar to that of the general population of equivalent age and comorbidities. Given this, we could state that anticoagulant therapy allows patients to maintain a normal lifestyle since their HRQL is similar to that of the general population of equivalent age, sex and comorbidities. Arrospide et al. estimated mean utility values for the general population of 0.85 for 70- to 79-year-olds and 0.75 for 80- to 89-year-olds [Citation20]. On the other hand, the exclusion criteria of the study led to a selection bias, in that the sample did not include patients with cognitive impairment or those under palliative care, both associated with lower utility. The distribution of stroke history between the two groups could have had an influence, it being reported by a significantly higher percentage of patients in the group treated with DOACs. Nonetheless, it was not a statistically significant variable in the early versions of the two-part model, possibly due to the small number of patients with this history in the total sample. On the other hand, patients on DOACs were prescribed a significantly higher total number of medications than patients on VKAs, and this was statistically significant in the two-part model. This could suggest that DOAC patients had a higher degree of comorbidity, which would impact quality of life negatively. These differences might be due to differences in the process of accessing the prescription between the two groups, each prescription of DOAC needing official approval from the Basque Health Service before medication can be dispensed in pharmacies.
The analysis of EQ-5D-5L scores in patients with a good quality of life poses the problem of a ceiling effect, meaning that the instrument lacks sensitivity to changes when the baseline quality of life is very high [Citation19]. This difficulty of measuring differences in HRQL in populations with a chronic condition such as atrial fibrillation and anticoagulation may be due in part to the adaptation process described by Sprangers et al. as a response shift [Citation21,Citation22]. A response shift accounts for improvements in outcomes reported by patients over time despite no changes in their quality of life. This is explained by the psychological phenomenon of patients adapting to cope with their new life circumstances. After the diagnosis of an illness, individuals re-prioritise, altering which issues they consider most important, such as placing less value on physical than cognitive function, reversing the order with respect to before their diagnosis [Citation21,Citation22]. This mechanism may explain why utilities of anticoagulated patients are similar to or higher than those in the general population.
From analyzing the different EQ-5D dimensions, we found that anxiety/depression is the dimension of quality of life that accounts for differences in the value of the utilities in both groups. In contrast, patients have almost the same rates of perfect health in the mobility, self-care, usual activities and pain/discomfort dimensions. The scientific literature indicates that the quality of anticoagulation with VKAs is related to the intensity of monitoring [Citation23,Citation24]. Further, it has been found that only just over half of patients with atrial fibrillation are well monitored, despite these patients being at high risk of thromboembolic events [Citation25]. The differences compared to our results may be attributable to our patients being monitored in a well-managed dedicated hospital anticoagulant clinic and most of them being resident in an urban environment, close to the hospital. Nonetheless, in many ways, attendance at the clinic is a predictor of ‘acceptance’ of anticoagulation. Patients uncomfortable with anticoagulation treatment would be likely to stop attending the clinic and, therefore, not be recruited for the study, this introducing a selection bias that could explain the good HRQL in this sample. Further, it has been found that INR self-monitoring improves HRQL in patients on VKAs because they gain independence and spare time [Citation26]. For this reason, risk-benefit assessment of these treatment options should take into account the risk of a cardiovascular event associated with difficulties in patient monitoring as well as reductions in benefit in terms of quality of life. Regarding the latter factor, it tends to be reported that the degree of lifestyle limitation is the factor that most reduces the quality of life of patients on oral anticoagulation due to its impact on dissatisfaction [Citation27]. In our study, it is shown that despite good quality in anticoagulation care, patients on VKA treatment suffer greater stress and concern than patients on treatment with DOACs.
Some limitations should be recognized. First, we did not collect data on either adverse events, such as bleeding complications, before enrolment in this study or the intensity of INR monitoring, which could underlie differences in HRQL. Second, patients only reported HRQL using a generic questionnaire. It might have been useful to also administer a treatment-specific questionnaire, e.g. the Perception of Anticoagulant Treatment Questionnaire (PACT-Q) [Citation28]. Third, follow-up intensity and INR testing were not assessed which did not allow to test how frequency of INR monitoring influences HRQL.
The conclusion of this study is that patients treated with DOACs report better quality of life than those treated with VKAs. This difference is attributable to patients on DOACs experiencing less anxiety/depression.
Authors’ contributions
MA, GP and JL conceived, designed the research and wrote the first version of introduction and discussion. OC and NZ obtained the data, and interpreted the data, helping to write results and discussion. AG and JM designed the methods, performed the analyses, interpreted the data and wrote the methods and results. All authors revised the manuscript for important intellectual content and approved the final manuscript.
Availability of data and materials
The dataset used and analyzed during the current study is available from the corresponding author on reasonable request.
Ethics approval
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human subjects/patients were approved by the Clinical Research Ethics Committee of Araba (code number 2017-088).
Acknowledgements
We would like to acknowledge the help of INC in improving the use of English in the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Kannel W, Wolf P, Benjamin E. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am J Cardiol. 1998;82(8A):2N–9N.
- Lane DA, Skjøth F, Lip GYH, et al. Temporal trends in incidence, prevalence, and mortality of atrial fibrillation in primary care. J Am Heart Assoc. 2017;6:e005155.
- Hankey GJ. Stroke treatment and prevention. An evidence-based approach. Cambridge: Cambridge University Press; 2005.
- Kovacs RJ, Flaker GC, Saxonhouse SJ, et al. Practical management of anticoagulation in patients with atrial fibrillation. J Am Coll Cardiol. 2015;7(65):1340–1360.
- Arribas Ynsaurraiga F, Peinado Peinado R, Ormaetxe Merodio JM. Atrial fibrillation and quality of life related to disease and treatment: focus on anticoagulation. Future Cardiol. 2014;10(3):381–393.
- Testa MA, Simonson DC. Assessment of quality-of-life outcomes. N Engl J Med. 1996;334(13):835–840.
- Bergner M. Quality of life, health status, and clinical research. Med Care. 1989;27:S148–S156.
- Samsa GP, Matchar DB. Relationship between test frequency and outcomes of anticoagulation: a literature review and commentary with implications for the design of randomized trials of patient self-management. J Thromb Thrombolysis. 2000;9:283–292.
- López-López JA, Sterne JAC, Thom HHZ, et al. Oral anticoagulants for prevention of stroke in atrial fibrillation: systematic review, network meta-analysis, and cost effectiveness analysis. Br Med J. 2017 Nov 28;359:j5058.
- Orueta JF, Nuño-Solinis R, Mateos M, et al. Monitoring the prevalence of chronic conditions: which data should we use? BMC Health Serv Res. 2012;12:365.
- Garrison LP, Neumann PJ, Erickson P, et al. Using real-world data for coverage and payment decisions: The ISPOR real-world data task force report. Value Health. 2007;10:326–335.
- Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441.
- Lip GY, Nieuwlaat R, Pisters R, et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137:263–272.
- Badía X, Roset M, Montserrat S, et al. La versión española del EuroQol: descripción y aplicaciones. Med Clin (Barc). 1999;112(supl 1):S79–S86.
- Brazier J, Deverill M, Green C, et al. A review of the use of health status measures in economic evaluation. Health Technol Asses. 1999;3(9):i–iv. 1–164.
- Ramos-Goñi JM, Craig BM, Oppe M, et al. Handling data quality issues to estimate the Spanish EQ-5D-5L value set using a hybrid interval regression approach. Value Health. 2018;21:596–604.
- Arrospide A, Ramos-Goñi JM, Pechlivanoglou P, et al. Application of two-part models and Cholesky decomposition to incorporate covariate-adjusted utilities in probabilistic cost-effectiveness models. Gac Sanit. 2020; 34:91–95.
- López-Nicolás Á, Trapero-Bertran M, Muñoz C. Smoking, health-related quality of life and economic evaluation. Eur J Health Econ. 2018;19:747–756.
- Huang IC, Frangakis C, Atkinson MJ, et al. Addressing ceiling effects in health status measures: a comparison of techniques applied to measures for people with HIV disease. Health Serv Res. 2008;43:327–339.
- Arrospide A, Machón M, Ramos-Goñi JM, et al. Inequalities in health-related quality of life according to age, gender, educational level, social class, body mass index and chronic diseases using the Spanish value set for Euroquol 5D-5L questionnaire. Health Qual Life Outcomes. 2019;17(1):69.
- Sprangers MA, Schwartz CE. Integrating response shift into health-related quality of life research: a theoretical model. Soc Sci Med. 1999;48:1507–1515.
- Rapkin BD, Schwartz CE. Advancing quality-of-life research by deepening our understanding of response shift: a unifying theory of appraisal. Qual Life Res. 2019;28:2623–2630.
- Matchar DB, Samsa GP, Cohen SJ, et al. Improving the quality of anticoagulation of patients with atrial fibrillation in managed care organizations: results of the managing anticoagulation services trial. Am J Med. 2002;113:42–51.
- Samsa GP, Matchar DB. Relationship between test frequency and outcomes of anticoagulation: a literature review and commentary with implications for the design of randomized trials of patient self-management. J Thromb Thrombolysis. 2000;9:283–292.
- Contreras Muruaga MM, Vivancos J, Reig G, et al. Satisfaction, quality of life and perception of patients regarding burdens and benefits of vitamin K antagonists compared with direct oral anticoagulants in patients with nonvalvular atrial fibrillation. J Comp Eff Res. 2017;6:303–312.
- Kulinna W, Ney D, Wenzel T, et al. The effect of self-monitoring the INR on quality of anticoagulation and quality of life. Semin Thromb Hemost. 1999;25:123–126.
- Mani H, Lindhoff-Last E. New oral anticoagulants in patients with nonvalvular atrial fibrillation: a review of pharmacokinetics, safety, efficacy, quality of life, and cost effectiveness. Drug Des Devel Ther. 2014 Jun 17;8:789–798.
- Prins MH, Guillemin I, Gilet H, et al. Scoring and psychometric validation of the perception of anticoagulant treatment questionnaire (PACT-Q). Health Qual Life Outcomes. 2009;7:30.
