Pain is the most common symptom in sickle cell disease (SCD) patients [Citation1]. In the acute setting, SCD patients may have painful crises that require hospitalization [Citation2]. However, these patients also suffer chronic pain, the etiology of which is not fully understood [Citation3].
Opioids remain the mainstay of management for both acute and chronic pain in SCD patients despite risks of physical dependence, withdrawal, tolerance, and possible overdose and death [Citation4,Citation5]. Chronic opioid use also alters intestinal microbial community [Citation6] and leads to increased risks for the development of Clostridioides difficile infection [Citation7]. Despite potential adverse outcomes in chronic opioid use and specific limitations in SCD patients, there are no clear guidelines for the management of chronic pain in SCD patients. In this study, we sought to determine the risks for and clinical characteristics associated with chronic opioid use to identify the at-risk patients so that they may be offered early interventions to avert these complications.
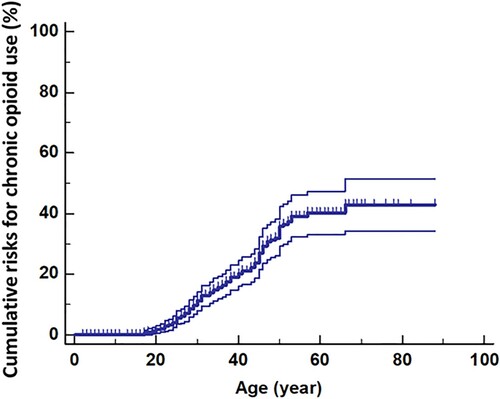
Following approval from the Institutional Review Board, data from 449 patients were collected. There were 258 females and 191 males; 98% were Black/African-American. Their median age was 39 years (range 3–88). Their phenotypes were HbSS (284/449) (63%), HbSC (101/449) (22.5%), HbSβ0thal (54/449) (12%), and unknown or others (10/449). The prevalence rate of chronic opioid use was 22.5% (95% CI: 18.3–27.3). The lifetime cumulative risks for chronic opioid use (with 95% CI) are shown in . Not surprisingly, the risks increase steadily from age 20 years to 55 years.
We next examined the clinical factors associated with chronic opioid use among those age 18 and over (). In univariate analysis, we identified that chronic opioid users are more likely to be female (p < 0.0001) and have higher baseline total white cell count (median 10 × 109/L vs 9 × 109/L) (p = 0.0009), non-HbSC phenotype (p = 0.034), been prescribed hydroxyurea (p = 0.000047), and concurrent psychiatric illness (p = 0.018). Lower hemoglobin (8.5 g/dL vs 8.9 g/dL) (p = 0.055) and presence of chronic arthritis (p = 0.06) trend towards significance for chronic opioid use. Multivariate analysis found that patients with higher total white cell count (p = 0.0007), psychiatric illness (p = 0.0059), and users of hydroxyurea (p = 0.0001) were particularly at risk. Patients with a total white cell count of 15 × 109/dL or above were 2.2 (95% CI: 1.45–3.37) times more at risk (p = 0.0024) for chronic opioid use than those whose total white cell counts were below 15 × 109/dL.
Table 1. Comparison of characteristics of patients.
In this study, we have identified a group of adult sickle cell patients who are at risk for chronic opioid use. The data from our univariate analysis suggests that, in addition to concurrent psychiatric illness, patients with more severe disease are at higher risks for chronic opioid use. These patients tend to have higher total white cell counts, be more anemic, have chronic arthritis, and be more likely to have been prescribed hydroxyurea. The association between chronic opioid use and higher total baseline white cell count is consistent with data showing that this is also the same group of patients who are at higher risks for strokes [Citation8] and early death [Citation9]. This association may reflect elevated levels of baseline systemic inflammation and its contribution to chronic pain. Not unlike adult patients in the general population [Citation10], SCD patients with mental health disorders are significantly more at risk for chronic opioid use than those without mental health disorders.
In conclusion, chronic opioid use is prevalent among adult SCD patients. The identification of the clinical characteristics that are associated with the development of chronic opioid use provides the framework for healthcare providers to recognize these patients early and be pro-active in their intervention. The chronic use of opioids most likely reflects the lack of mechanistic management of pain. For these at-risk patients, a multidisciplinary approach early in their disease course may be beneficial. The approach may include the implementation of non-opioid pain management methods such as the use of cannabinoids and intranasal ketamine, and early orthopedic intervention in those with chronic arthritis and avascular necrosis to curtail the duration of use of opioid analgesia. Psychosocial support and patient/family education should also be offered at the onset of the use of opioid analgesia in the outpatient setting.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Carroll CP. Opioid treatment for acute and chronic pain in patients with sickle cell disease. Neurosci Lett. 2020;714:134534.
- Borhade MB, Kondamudi NP. Sickle cell crisis. Treasure Island (FL): StatPearls; 2021.
- Sagi V, Mittal A, Tran H, et al. Pain in sickle cell disease: current and potential translational therapies. Transl Res. 2021: S1931–5244(21)00057-8.
- Baldini A, Von Korff M, Lin EH. A review of potential adverse effects of long-term opioid therapy: a practitioner’s guide. Prim Care Companion CNS Disord. 2012;14:PCC.11m01326.
- Benyamin R, Trescot AM, Datta S, et al. Opioid complications and side effects. Pain Physician. 2018;11(2 Suppl):S105–S120.
- Akbarali HI, Dewey WL. Gastrointestinal motility, dysbiosis and opioid-induced tolerance: is there a link? Nat Rev Gastroenterol Hepatol. 2019;16:323–324.
- Lichtbroun M, Jafri F, Chaudhary RC, et al. High incidence of healthcare facility-acquired Clostridium difficile infections in chronic opioid users. J Intern Med. 2021;289:129–130.
- Ohene-Frempong K, Weiner SJ, Sleeper LA, et al. Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood. 1998;91:288–294.
- Platt OS, Brambilla DJ, Rosse WF, et al. Mortality in sickle cell disease: life expectancy and risk factors for early death. N Engl J Med. 1994;330:1639–1644.
- Tran H, Gupta M, Gupta K. Targeting novel mechanisms of pain in sickle cell disease. Blood. 2017;130:2377–2385.