ABSTRACT
Objectives
POEMS syndrome is a rare disorder which has been increasingly recognized. The clonal origin is controversial. Some people argue that POEMS syndrome originates from abnormal plasma cell clones. So, treatment frequently targets the plasma cell clone. Nevertheless, others believe that both plasma cells and B cells can be the potential culprit in POEMS syndrome.
Methods
A 65-year-old male came to the emergency department of our hospital with the complaints of bilateral soles numbness and weight loss for half a year, abdominal distension for half a month, and chest tightness and shortness of breath for one day. He was then diagnosed as POEMS syndrome complicated with monoclonal B-cell lymphocytosis (non-CLL type). A standard bendamustine plus rituximab (BR) regimen combined with low dose of lenalidomide was administered.
Results
After four cycles of treatment, the ascites of the patient was absent and the neurological symptom disappeared. The renal function, the IgA level, and the VEGF level all returned to normal.
Discussion
POEMS syndrome, a multi-system disorder, is easily misdiagnosed. The clonal origin of POEMS syndrome is controversial and needs further study. For now, there are no approved treatment regimens. Treatments mainly target the plasma cell clone. This case suggested that other therapy besides anti-plasma cell treatment may also be effective in POEMS syndrome.
Conclusion
We report a patient with POEMS syndrome who achieved complete response after treatment with the combination of a standard BR regimen and low dose of lenalidomide. POEMS syndrome's pathological mechanisms and therapies warrant further studies.
Introduction
PΟΕMS syndrome is the acronym for a paraneoplastic syndrome characterized by polyneuropathy (P), organomegaly (O), endocrinopathy (E), monoclonal protein (M), and skin changes (S). It is a rare disorder, which has been increasingly recognized. A 2015 nationwide study in Japan found a prevalence of 0.3 per 100,000 people [Citation1]. According to the criteria in 2019, two mandatory criteria (polyneuropathy and monoclonal plasma cell proliferative disorder), one major criterion (sclerotic bone lesion, Castleman’s disease, or VEGF elevation), and one minor criterion (organomegaly, edema, endocrinopathy, skin changes, papilloedema or thrombocytosis) are required to establish the diagnosis [Citation2].
The clonal origin of PΟΕMS syndrome is controversial. It has long been considered to be an abnormal clonal disease of plasma cells. Recently, it has been incorporated into the spectrum of monoclonal gammopathy of clinical significance (MGCS) with a characterized small plasma cell clone [Citation3]. However, in some cases of POEMS syndrome, cell clones other than plasma cell clones can also occur [Citation4–8]. As a result, others believe that both plasma cells and B cells can be the potential culprit in PΟΕMS syndrome [Citation9,Citation10].
We present a case of POEMS syndrome complicated by B lymphocyte proliferative disease that had full remission after anti-B cell therapy with bendamustine and Rituximab, as well as the immunomodulator lenalidomide at a low dosage.
Case description
A 65-year-old male came to the emergency department of our hospital on November 15, 2021, with the complaint of bilateral soles numbness and weight loss for half a year, abdominal distension for half a month, and chest tightness and shortness of breath for one day. He was a migrant worker with no history of hypertension or diabetes. Since May 2021, he began to feel numbness on the soles of both feet, pain on the instep, and swelling of both lower limbs. He was initially diagnosed as fasciitis in a local hospital. However, after symptomatic treatment, the symptoms did not mitigate. Then he went to the Neurology department of our hospital at the end of September 2021. Electromyography examination showed peripheral nerve damage of upper and lower limbs, with more obvious findings in both lower limbs (distal movement, sensory fiber involvement, axonal injury). It also showed that the nerve conduction velocity decreased, indicating that the myelin sheath was damaged. Moreover, his fasting blood glucose level was 7.9 mmol/L (normal range: 3.9–6.0 mmol/L). He was then diagnosed to have peripheral neuropathy caused by diabetes. However, after nutritional neurotherapy for 12 days, numbness of both lower extremities worsened instead of alleviating. To make matters worse, he developed face edema, abdominal distention, decreased urine, and chest tightness over time. He began to experience shortness of breath one day before arriving at our emergency department.
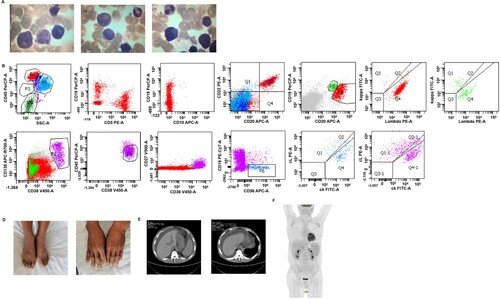
Several examinations were taken in the emergency department. Blood analysis showed that the levels of white blood cells, platelet, and hemoglobin were in the normal ranges. CT showed splenomegaly, peri-splenic varices, and a large amount of peritoneal effusion (shown in (E)). He was then transferred to the Gastroenterology department on November 17. Gastroscopy and enteroscopy examinations were normal. Morphology of ascites fluid showed a few heterosexual cells, suspicious of tumor cells. A multidisciplinary consultation involving the Gastroenterology, Cardiology, Endocrinology, Nephrology, and Hematology departments was arranged. Further examination showed as follows: The serum immunoglobulin (Ig) A level was 6.05 g/L (normal range: 0.44–4.41 g/L), with the level of IgG, IgG4, IgM, C3, C4, and RF within normal ranges. Immuno-electrophoresis revealed monoclonal IgA, λ light chain type. Thyroid-stimulating hormone (TSH), free triiodothyronine, and free thyroxine levels were 7.39 mIU/L (normal range: 0.56–5.91 mIU/L), 2.68 pmol/L (normal range: 3.28–6.47 pmol/L), and 11.11 pmol/L (normal range: 7.64–16.03 pmol/L), respectively. Low proliferative lymphohematopoietic disorders was identified by PETCT examination (shown in (F)). Finally, he was transferred to the hematology department. Lymph nodes of the size of a bean were seen on both sides of the neck, clavicle, armpit, and groin during physical examination. Also, the patient exhibited a distended abdomen, obvious concave edema in the lower limbs, and dark coloration of the dorsal of the hands and ankles were dark (shown in (D)). Sex hormones examinations showed estradiol 45 pg/ml (normal range: 0–38.95 pg/ml), pituitary prolactin 595 mIU/L (normal range: 56–278.4 mIU/L) and testosterone 1.5 ng/ml (normal range:1.75–7.81 ng/ml). Of note, the level of serum VEGF was elevated as 574.42 pg/ml (normal range: 0–142.2 pg/mL). Bone marrow aspiration revealed 3% monoclonal B lymphocytes which expressed CD19+/CD20++/CD10−/CD38−/CD5−/CD138-, with no monoclonal plasma cell proliferation identified (shown in (A,B,C)). Bone marrow FISH examination of the patient showed IgH rearrangement and bone marrow biopsy showed light chain restriction expression using IHC. However, a biopsy of the lymph node on the left neck was negative due to poor sampling. The patient was then diagnosed with POEMS syndrome complicated with monoclonal B-cell lymphocytosis (non-CLL type) based on the criteria established by Dispenzieri et al and 2016 WHO classification of lymphoid neoplasms [Citation11].
Figure 1. Clinical manifestation and laboratory examinations of patients at diagnosis. (A) The morphological analysis of the patient’s bone marrow. The cell body is larger than normal, the cytoplasm is rich and blue, the nuclear chromatin is rough and irregular, and the nucleolus is not clear. (B + C) Flow cytometry showed 3% monoclonal B cells in bone marrow, expressing CD19+/CD20++/CD10−/CD38−/ CD5−/CD138−. (D) Pigment deposition in the dorsum of hands and ankles. (E) Computed tomography scans showed massive ascites. (F) 18F-FDG PET/CT was performed and showed multiple lymphadenopathy in the cervix and axilla with no hypermetabolic lesions.
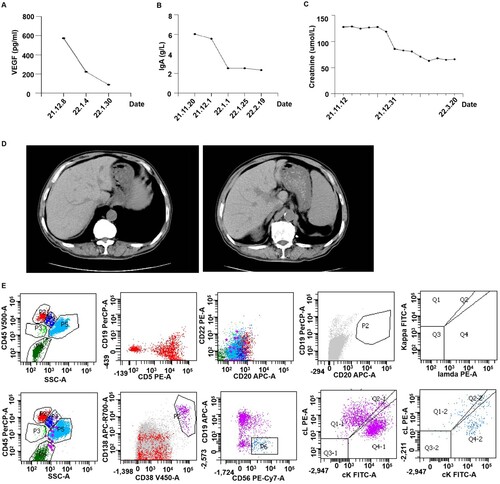
A standard BR regimen consisting of rituximab 375 mg/m2 on d0, bendamustine 70 mg/m2 on d1 and d2 was applied in combination with low dose lenalidomide (10 mg qod). After four cycles of treatment, the ascites of the patient was absent and the neurological symptom disappeared. The renal function, the IgA level, and the VEGF level all returned to normal (shown in ). Furthermore, the patient’s serum IFE lambda decreased from 49.3 to 30.9 mg/L (normal range: 5.71–26.3 mg/L). TSH returned to normal range. PRL decreased from 595mIU/L to 279.5 mg/L (normal range: 56.0–278.4mIU/L).
Figure 2. Clinical manifestation and laboratory examinations of the patient after four cycles of anti-B treatment. (A) Serum VEGF level of the patient decreased significantly after treatment. (B) IgA level in plasma of the patient decreased significantly after treatment. (C) Creatinine level of the patient returned to normal after treatment. (D) Computed tomography scans revealed ascites disappeared after treatment. (E) Flow cytometry showed no monoclonal B cells after four cycles of anti-B treatment.
Discussion
POEMS syndrome is a disorder that affects multiple systems. In the early stages, patients may exhibit peripheral neuropathy, ascites, skin changes, and endocrine modifications, which may be misdiagnosed as nervous, digestive, or endocrine diseases. In this case, the patient initially presented with peripheral neuropathy and hyperglycemia and was misdiagnosed as diabetic peripheral neuropathy. Later, he was misdiagnosed with a digestive disease because of a large amount of ascites and was admitted to the Department of Gastroenterology. After multidisciplinary consultation, he was finally diagnosed with POEMS syndrome. As this case shows, POEMS syndrome is easily misdiagnosed. POEMS syndrome should be investigated in patients who have unexplained peripheral neuropathy and ascites.
VEGF has been used as a surrogate hallmark of POEMS syndrome [Citation12–14]. It is a platelet-derived vascular growth factor and plays an important role in normal and pathological angiogenesis [Citation15]. It is related to several tumors [Citation16,Citation17] and hematologic diseases [Citation18,Citation19]. VEGF targets endothelial cells and causes a rapid and reversible increase in vascular permeability, which might explain some of the clinical signs of POEMS syndrome [Citation20]. However, it is shown that VEGFA expression was not increased in plasma cell clones of POEMS syndrome [Citation21]. Thus, whether VEGF comes from a plasma cell clone and the true mediator of POEMS is yet unknown.
Recently, a partial overlap between chromosomal abnormalities in POEMS syndrome and the monoclonal gammopathy of undetermined significance (MGUS) was shown [Citation21]. As a result, it seemed that POEMS syndrome originated from clonal plasma cells. However, RNA sequencing revealed a transcription profile specific to POEMS syndrome when compared with normal plasma cells, MGUS, and multiple myeloma [Citation21]. Moreover, the level of plasma clone and M-protein produced (mostly IgA λ) are significantly lower in POEMS syndrome than that of multiple myeloma [Citation22]. It is not clear why high levels of IgA λ light chain in multiple myeloma would not manifest POEMS-like symptoms. Castleman disease is characterized by systemic inflammation, lymph node pathology and multi-organ dysfunction resulting from hypercytokinemia, and it can be associated with POEMS syndrome [Citation2,Citation22]. Several cases have shown that lymphoma including DLBCL, T-cell lymphoma, Waldenström macroglobulinemia, primary cutaneous diffuse large B-cell lymphoma (leg type), follicular lymphoma can be manifested as POEMS syndrome [Citation4–8] (shown in ). Furthermore, cases of POEMS syndrome without M-protein and clonal plasma cells were also reported, which were called variant POEMS syndrome [Citation23,Citation24] (shown in ). These facts suggest that further study is needed to reveal the origination of POEMS syndrome.
Table 1. Special case reports of POEMS syndrome.
POEMS syndrome has no approved treatment regimens. Treatment mainly targets the plasma cell clone. The most used systemic chemotherapy for POEMS syndrome includes alkylators and steroids, lenalidomide, bortezomib, and high-dose chemotherapy with autologous stem cell transplantation [Citation25–29]. However, in this case, since the B cell monoclone was found in the patient's bone marrow, we adopted a combination therapy with an anti-B cell-based regimen (bendamustine and rituximab) and a low dose of an immunomodulator (lenalidomide). Bendamustine is a unique bifunctional alkylating agent with a benzimidazole ring giving it purine analogue-like properties. It is thought to act by modifying and cross-linking purine bases in DNA, thus inhibiting DNA, RNA and protein synthesis and leading to cell death in rapidly dividing cells. It appears to have a special activity against B cell leukemias and lymphomas [Citation30]. This is the first report about bendamustine containing chemotherapy for POEMS syndrome. After four cycles of treatment, the patient got a complete response [Citation2] with no ascites, negative serum IFE and bone marrow findings, and normalized serum VEGF. It suggested that other therapy other than anti-plasma cell treatment may also be effective in POEMS syndrome, which provide a new angle to the origination of POEMS syndrome.
Conclusion
We report a patient with POEMS syndrome who achieved complete response after combinatory treatment with an anti-B cell-based regimen and low dose lenalidomide. POEMS syndrome's pathological mechanism and therapies warrant further studies.
Statement of ethics
We state that the work has followed the principles outlined in the Declaration of Helsinki for all human or animal experimental investigations. In addition, informed consent has been obtained from the patient involved before the treatment.
Acknowledgements
Lu Zhou and Hongmin Huang conceived the case report. Zenghua Lin and Ruirong Xu performed the clinical treatment and observation. Xinfeng Wang and Lemin Hong coordinated liquoral and serologic analysis. Lu Zhou and Jinfeng Lu wrote the case report. Jinfeng Lu was responsible for manuscript submission. Lan Luo was in charge of critical revision of the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
All data generated during the study appear in the submitted article.
Additional information
Funding
References
- Suichi T, Misawa S, Beppu M, et al. Prevalence, clinical profiles, and prognosis of POEMS syndrome in Japanese nationwide survey. Neurology. 2019;93(10):e975–e983.
- Dispenzieri A. POEMS syndrome: 2019 update on diagnosis, risk-stratification, and management. Am J Hematol. 2019;94(7):812–827.
- Fermand J-P, Bridoux F, Dispenzieri A, et al. Monoclonal gammopathy of clinical significance: a novel concept with therapeutic implications. Blood. 2018;132(14):1478–1485.
- Ngamdu KS, Torabi A, Badri N, et al. Diffuse large B-cell non-Hodgkin's lymphoma and osteosclerotic myeloma with features of POEMS syndrome. Proc (Bayl Univ Med Cent). 2016;29(3):306–308.
- Zou F, Li Z, Ma J-A, et al. T-cell lymphoma with POEMS syndrome. Oncol Lett. 2015;9(3):1313–1316.
- Allegra A, Oteri G, Alonci A, et al. Association of osteonecrosis of the jaws and POEMS syndrome in a patient assuming rituximab. J Craniomaxillofac Surg. 2014;42(4):279–282.
- Nakayama S, Yokote T, Kobayashi K, et al. Primary cutaneous diffuse large B-cell lymphoma, leg type, with features simulating POEMS syndrome. Eur J Haematol. 2010;84(1):79–83.
- Pan Q, Luo Y, Cao X, et al. Posttreated POEMS syndrome with concurrent follicular lymphoma revealed by 18F-FDG and 68Ga-pentixafor PET/CT. Clin Nucl Med. 2020;45(3):220–222.
- Ali T, Qazilbash MH. POEMS syndrome: a multisystem clonal disorder. Eur J Haematol. 2021;106(1):14–18.
- Dao LN, Hanson CA, Dispenzieri A, et al. Bone marrow histopathology in POEMS syndrome: a distinctive combination of plasma cell, lymphoid, and myeloid findings in 87 patients. Blood. 2011;117(24):6438–6444.
- Jiang M, Bennani NN, Feldman AL. Lymphoma classification update: B-cell non-Hodgkin lymphomas. Expert Rev Hematol. 2017;10(5):405–415.
- D'Souza A, Hayman SR, Buadi F, et al. The utility of plasma vascular endothelial growth factor levels in the diagnosis and follow-up of patients with POEMS syndrome. Blood. 2011;118(17):4663–4665.
- Scarlato M, Previtali SC, Carpo M, et al. Polyneuropathy in POEMS syndrome: role of angiogenic factors in the pathogenesis. Brain. 2005;128(Pt 8):1911–1920.
- Nobile-Orazio E, Terenghi F, Giannotta C, et al. Serum VEGF levels in POEMS syndrome and in immune-mediated neuropathies. Neurology. 2009;72(11):1024–1026.
- Melincovici CS, Boşca AB, Şuşman S, et al. Vascular endothelial growth factor (VEGF) – key factor in normal and pathological angiogenesis. Rom J Morphol Embryol. 2018;59(2):455–467.
- Frezzetti D, Gallo M, Maiello MR, et al. VEGF as a potential target in lung cancer. Expert Opin Ther Targets. 2017;21(10):959–966.
- Manoli A, Katsinis S, Papouliakos S, et al. VEGF- mediated mechanisms in nasopharyngeal carcinoma. J BUON. 2021;26(3):1172.
- Subotički T, Mitrović Ajtić O, Živković E, et al. Vegf regulation of angiogenic factors via inflammatory signaling in myeloproliferative neoplasms. Int J Mol Sci. 2021;22(13):6671–6684.
- Podar K, Anderson KC. The pathophysiologic role of VEGF in hematologic malignancies: therapeutic implications. Blood. 2005;105(4):1383–1395.
- Arimura K. Increased vascular endothelial growth factor (VEGF) is causative in Crow-Fukase syndrome. Rinsho Shinkeigaku. 1999;39(1):84–85.
- Nagao Y, Mimura N, Takeda J, et al. Genetic and transcriptional landscape of plasma cells in POEMS syndrome. Leukemia. 2019;33(7):1723–1735.
- Shi X, Hu S, Yu X, et al. Clinicopathologic analysis of POEMS syndrome and related diseases. Clin Lymphoma Myeloma Leuk. 2015;15(1):e15–e21.
- He T, Zhao A, Zhao H, et al. Clinical characteristics and the long-term outcome of patients with atypical POEMS syndrome variant with undetectable monoclonal gammopathy. Ann Hematol. 2019;98(3):735–743.
- Du HP, Zhang Y, Sun LM, et al. Two cases of special POEMS syndrome without monoclonal protein expression: a case report and literature review. J Int Med Res. 2021;49(4):300060521990967.
- Jurczyszyn A, Castillo JJ, Olszewska-Szopa M, et al. Poems syndrome: real world experience in diagnosis and systemic therapy – 108 patients multicenter analysis. Clin Lymphoma Myeloma Leuk. 2022;22(5):297–304.
- Yang H, Zhao H, Huang X, et al. Improvement of thyroid function in POEMS syndrome after combination therapy of lenalidomide and dexamethasone. Leuk Lymphoma. 2019;60(2):483–487.
- Lestang E, Caristan A, Néel A, et al. Lenalidomide as frontline therapy in polyneuropathy, organomegaly, endocrinopathy, monoclonal protein and skin changes syndrome: a retrospective case series of eight patients. Leuk Lymphoma. 2015;56(6):1895–1896.
- Pramanik R, Sharma A, Sharma A, et al. Poems syndrome: Indian experience from a tertiary-care institute. Clin Lymphoma Myeloma Leuk. 2019;19(9):e536–e544.
- Grandoni F, Stalder G, Borgeat Kaeser A, et al. Successful desensitization to pomalidomide in a patient with POEMS syndrome with delayed-type hypersensitivity to immunomodulatory imid drugs. Leuk Lymphoma. 2019;60(12):3087–3089.
- Amoxicillin. Livertox: clinical and research information on drug-induced liver injury. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012.
