ABSTRACT
Background
No consensus has been reached yet concerning treatment strategies for a sequential classic Hodgkin lymphoma (CHL) following gray zone lymphoma (GZL). Prognosis of GZL after a failed autologous hematopoietic stem-cell transplantation (auto-HCT) is poor and treatment strategy is very limited. As yet there are limited data showing clinical outcomes of brentuximab vedotin (BV) for GZL, especially for sequential CHL after GZL.
Case presentation
We report a case of CHL following primary refractory GZL after a failed auto-HCT and showed favorable response to first-line CHL-directed chemoradiotherapy consisting of BV plus doxorubicin, vinblastine, and dacarbazin (AVD) followed by irradiation. The sequential cases with an early evolution, whose diagnosis of second lymphoma was made within a year, have been recently reported very poor survival shorter than a year. Whether a sequential CHL following GZL should be treated as a primary or relapsed disease has not been clearly elucidated. Our patient showed favorable response to first-line CHL-directed chemoradiotherapy without allogenic hematopoietic stem-cell transplantation and has in continuous remission for 2 years.
Conclusions
The management of our case could help for physicians to make better treatment decisions and provide insights for further exploration in future studies.
Abbreviations::
Introduction
Gray zone lymphoma (GZL) is a rare tumor defined as B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma (DLBCL) and classic Hodgkin lymphoma (CHL) in WHO classification. GZL usually represents an aggressive lymphoma subtype and worse outcomes compared to CHL and DLBCL. DLBCL and CHL are also coexisting and diagnosed as composite or sequential lymphomas [Citation1–3]. A recent report showed the sequential cases with an early evolution, whose diagnosis of second lymphoma was made within a year, have very poor survival shorter than a year [Citation2]. Many efforts have been made to understand molecular biology of DLBCL and CHL as well as GZL, however, the precise diagnosis and clinical significance remain challenging to both pathologists and hematologists because their differential diagnosis has direct implications for treatment strategies.
Brentuximab vedotin (BV), an antibody–drug conjugate targeting CD30, is an effective therapeutic agent for CHL and other CD30-positive lymphomas including GZL, which frequently expresses CD30 [Citation4,Citation5]. As yet there are limited data showing clinical outcomes of BV for GZL, and especially for those of sequential CHL after GZL, the efficacy of BV is not well defined. We report a case of CHL following primary refractory GZL after a failed autologous hematopoietic stem-cell transplantation (auto-HCT). Our patient showed favorable response to BV with chemotherapy followed by localized radiotherapy.
Case presentation
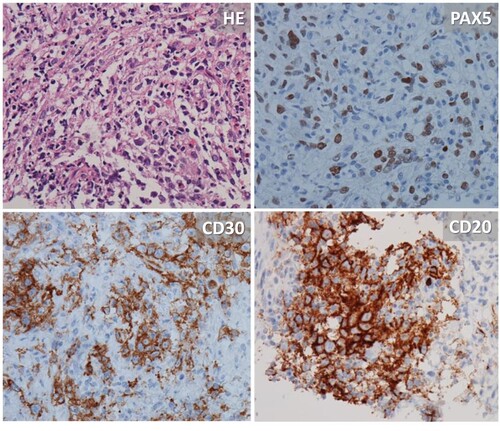
A 29-year-old Japanese man contacted his general practitioner with symptoms of persistent cough for two weeks. He has no past medical history of any comorbidity. In this patient, there was no family history of cancer including lymphoma. Chest radiography during a medical examination showed a light lung nodule. He referred our hospital. A computed tomography demonstrated a bulky mediastinal tumor, lymphadenopathy, and lung tumor (). FDG uptake in the cervical was observed, however, cervical lymphadenopathy, which was indication for an excisional biopsy, could not be found. Core needle biopsy of the lung showed aggregation of large lymphoid cells resembling Hodgkin/Reed-Sternberg (HRS) cells in a background of infiltration of small lymphocytes, neutrophils, and eosinophils (). Fibrosis was also seen. Tumor cells were positive for CD30, CD20, PAX-5, and PD-L1 and negative for CD3 and CD79a. Epstein–Barr virus (EBV) was negative using EBV-encoded RNA in-situ hybridization. Rosetting T cells in large neoplastic ‘lymphocyte predominant’ (LP) cells were not observed. The sample contained abundant neoplastic lymphocytes and background nodular structures containing non-neoplastic B-cells were not found. Considering the feature, the other diagnoses including nodular lymphocyte-predominant Hodgkin's lymphoma (NLPHL) and lymphocyte-rich classical Hodgkin's lymphoma (LRCHL) have been ruled out. Overall the features were consistent with GZL, which was established by an institutional hematopathology expert according to WHO definition.
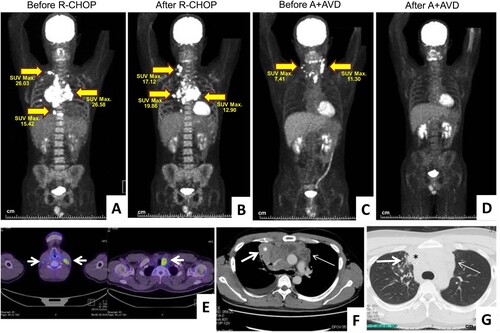
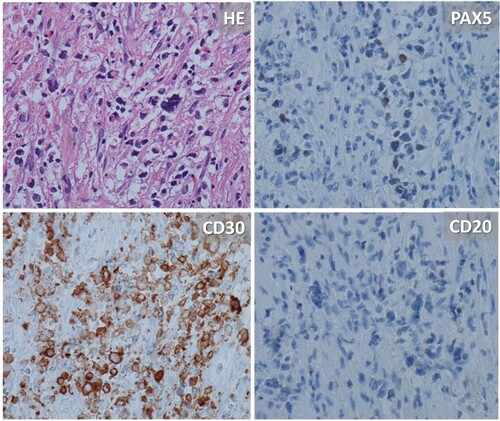
Figure 1. (A) and (F–G) Pre-treatment FDG PET/CT scan showed disseminated hypermetabolic lesions involving the supraclavicular lymph node, mediastinum, lungs, pleura, and bone marrow. (B) One month after completion of last dose of R-CHOP therapy, the patients had right cervical lymph node swelling with positive finding on FDG PET/CT. (C) and (E) Four months after autotransplantation, cervical lymphadenopathy was observed with positive finding on FDG PET/CT. (D) Complete metabolic response was obtained after 2 cycles of BV + AVD. (H) Pathological features of GZL before R-CHOP. Core needle biopsy of the lung showed aggregation of large lymphoid cells resembling Hodgkin/Reed-Sternberg (HRS) cells in a background of infiltration of small lymphocytes, neutrophils and eosinophils. Fibrosis was also seen. Tumor cells were positive for CD30, CD20, and PAX-5 (×400). (I) Pathological features of nodular sclerosis/lymphocyte depletion CHL at second relapse of GZL after autotransplantation failure. Considerable fibrous thickening and large lymphocytes resembling HRS cells were observed with massive necrosis. The tumor cells showed negativity for CD20 antigen, positivity for CD30, and were weekly positive for PAX5 (×400).
He was diagnosed as stage IV GZL. The baseline International Prognostic Index score was low/intermediate-risk. He was treated with standard R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisolone) therapy. One month after completion of last dose of the therapy, he complained fever and right cervical lymph node swelling. Re-biopsy of the lymph node revealed that the patient developed nodular sclerosis/lymphocyte depletion CHL (CHL-NS/LD) from GZL. The tumor cells showed loss of CD20 expression and weekly positive for PAX-5. The end of treatment response was progressive disease according to response assessment of Hodgkin and non-Hodgkin lymphoma (the Lugano Classification). He was diagnosed as stage IV and received four cycles of salvage chemotherapy (CHASE therapy: cyclophosphamide, high-dose cytarabine, etoposide, and dexamethasone) [Citation6]. Complete metabolic remission was obtained and he proceeded to high-dose chemotherapy (LEED regimen [Citation7]) with auto-HCT. LEED regimen consists of cyclophosphamide 60 mg/kg on days −4 and −3, etoposide 500 mg/m2 on days −4 to −2, melphalan 130 mg/m2 on day −1 and dexamethasone 40 mg/body on days −4 to −1. The patient received auto-HCT on day 0. Four months after the transplant, cervical, supraclavicular, parathyroid, and peritracheal lymphadenopathy was observed. He was diagnosed with tumor biopsy-confirmed stage II CHL without B symptoms (). The 3rd biopsy (relapsed after auto-HCT) was similar with 2nd biopsy (progressed after R-CHOP) in terms of immunohistochemistry. In consideration of his decision for sparing allogeneic hematopoietic cell transplantation (allo-HCT), we offered two cycles of BV + AVD (doxorubicin, vinblastine, and dacarbazin) followed by consolidative involved-node radiation therapy. Total doses of 30 Gy were given in 15 fractions. Complete metabolic remission was achieved after BV + AVD and he has in continuous remission for 2 years.
Discussion and conclusion
GZL has high rates of relapses showing that 33% had primary refractory disease and 58% relapsed disease with a median time to relapse of 7 months [Citation8]. Auto-HCT is generally thought to be effective in around 80% of the 2-year survival [Citation8], however, treatment strategies are limited after auto-HCT failure. BV is effective for relapsed/refractory GZL achieving objective responses in more than half of patients [Citation5,Citation9]. A single-agent BV produced complete remission for 3 years in a relapsed GZL patient with local skin lesion after auto-HCT failure [Citation10], while, the duration of remission was relatively short using both as single-agent and combination therapy with BV in patients with nodal lesions [Citation9]. BV administration is suggested to be used as bridging therapy before allo-HCT in transplant-eligible patients [Citation5,Citation9]. Our patient remains in remission for, at least, 2-year after BV combined therapy followed by consolidative radiation without allo-HCT. Chemotherapy-resistant GZL is reported to be managed with salvage chemotherapy plus radiation without allo-HCT [Citation4]. Similarly, our case suggested that chemotherapy including BV plus consolidative radiation might be effective for GZL after early auto-HCT failure. There is a paucity of data on the role of allo-HCT in patients with GZL. The best time to do allo-HCT after achieving remissions with salvage regimen is still under discussion. Careful follow-up should be needed for patients to miss an opportunity to access allo-HCT.
While the early sequential cases show very poor survival, patients with early evolution of DLBCL to CHL could survive after second-line treatment including radiation only [Citation2]. The evolution of DLBCL to CHL occurs usually with the non-irradiated mediastinum [Citation1–3]. A recent study demonstrated that biology of GZL differs depending on lesion locations. The genetic alteration of thymic GZL largely overlaps with that of CHL and primary mediastinal large B-cell lymphoma, on the other hand, half of non-thymic GZL have abnormalities affecting apoptosis-related genes [Citation11]. The second and third biopsies of cervical lymph nodes revealed that our patient was diagnosed as CHL from GZL. The patient with CHL who relapsed after auto-HCT was successfully treated using fist-line CHL-based treatment. The molecular biology of sequential CHL is largely unknown and whether a sequential CHL following GZL should be treated as a primary or relapsed disease has not been clearly elucidated. The incidence of CHL after GZL is probably underestimated, because a second and especially a third biopsies are rarely performed, particularly among refractory and early relapsed cases. Biopsy at relapse setting may help for physicians to make treatment decisions. GZL could present with a broad spectrum of morphologies with features of CHL and DLBCL in the same tumor tissue sample, and thus physicians should try to obtain an extensive sampling for the correct diagnosis. A better understanding of the underlying biology is needed in our quest to improve clinical outcomes of GZL.
Statement of ethics
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent to the publication of the manuscript was obtained from the patient. This study included use of brentuximab vedotin plus AVD in classic Hodgkin lymphoma following GZL and was approved by institution review board of Aichi Cancer Center, approval number 2022-0-010.
Acknowledgements
The authors would like to thank all medical professionals and staff for their excellent patient care. We also like to thank Junko Ozeki, Mako Hagino, and the clinical research staff for their technical assistance and Yuka Owaki for her excellent secretarial assistance. Author contributions: U.N. and H.K. wrote the first draft of the manuscript; S.K. and W.H. responsible for the pathological discussion; H. Tachibana and T.K. created the overall radiation treatment plan; K.Y supervised the research; and all authors provided patient data, contributed to the discussion, and approved the final manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
All data used during this study are included in this article. Further enquiries can be directed to the corresponding author on reasonable request.
Additional information
Funding
References
- Traverse-Glehen A, Pittaluga S, Gaulard P, et al. Mediastinal gray zone lymphoma: the missing link between classic Hodgkin's lymphoma and mediastinal large B-cell lymphoma. Am J Surg Pathol. 2005;29(11):1411–1421.
- Aussedat G, Traverse-Glehen A, Stamatoullas A, et al. Composite and sequential lymphoma between classical Hodgkin lymphoma and primary mediastinal lymphoma/diffuse large B-cell lymphoma, a clinico-pathological series of 25 cases. Br J Haematol. 2020;189(2):244–256.
- Vassilakopoulos TP, Piperidou A, Hadjiharissi E, et al. Development of classic Hodgkin lymphoma after successful treatment of primary mediastinal large b-cell lymphoma: results from a well-defined database. Leuk Res. 2021;100:106479.
- Wilson WH, Pittaluga S, Nicolae A, et al. A prospective study of mediastinal gray-zone lymphoma. Blood. 2014;124(10):1563–1569.
- Jacobsen ED, Sharman JP, Oki Y, et al. Brentuximab vedotin demonstrates objective responses in a phase 2 study of relapsed/refractory DLBCL with variable CD30 expression. Blood. 2015;125(9):1394–1402.
- Oki Y, Ogura M, Kato H, et al. Phase II study of a salvage regimen using cyclophosphamide, high-dose cytarabine, dexamethasone, etoposide, and rituximab in patients with relapsed or refractory B-cell non-Hodgkin's lymphoma. Cancer Sci. 2008;99(1):179–184.
- Kagami Y, Yamamoto K, Shibata T, et al. R-CHOP-14 versus R-CHOP-14/CHASER for upfront autologous transplantation in diffuse large B-cell lymphoma: JCOG0908 study. Cancer Sci. 2020;111(10):3770–3779.
- Evens AM, Kanakry JA, Sehn LH, et al. Gray zone lymphoma with features intermediate between classical Hodgkin lymphoma and diffuse large B-cell lymphoma: characteristics, outcomes, and prognostication among a large multicenter cohort. Am J Hematol. 2015;90(9):778–783.
- Li J, Sim J, Leung AYH, et al. Favorable response of relapsed/refractory gray-zone lymphoma to brentuximab vedotin. Ann Hematol. 2018;97(3):551–554.
- Ebisawa K, Masamoto Y, Koya J, et al. Long-term remission by brentuximab vedotin for non-mediastinal gray zone lymphoma refractory to autologous stem cell transplantation. Clin Lymphoma Myeloma Leuk. 2019;19(11):e602–e604.
- Sarkozy C, Hung SS, Chavez EA, et al. Mutational landscape of gray zone lymphoma. Blood. 2021;137(13):1765–1776.