ABSTRACT
Background
Myeloid sarcoma (MS) is a very rare hematologic disorder. This study analyzes the early treatment options for patients with different types of MS and explores the prognostic factors of MS.
Methods
Patients aged 15 years and older with MS in the SEER database (diagnosed from 2000 to 2018) were selected, excluding those with an unknown first course of treatment, an unknown location of disease, and less than 1 month of follow-up. Statistical methods used a chi-square test to compare clinical characteristics; Kaplan-Meier analysis to compare survival differences; and Cox proportional risk models to identify prognostic factors affecting overall survival (OS).
Results
Data were collected from 472 patients: 244 patients with isolated myeloid sarcoma (IMS) and 228 patients with non-isolated myeloid sarcoma (non-IMS). IMS patients mostly chose local treatment, while non-IMS patients mostly chose chemotherapy. There was a significant difference in OS between IMS patients treated with combined treatment and those without treatment. For non-IMS, treated patients had longer OS than untreated, but the difference was not statistically significant. Among adult patients, those younger than 60 years had a better prognosis. Patients with the urinary system, digestive system, reproductive system and chest and abdomen as the initial site had a better prognosis.
Conclusions
Early combination therapy in IMS patients had a longer OS, and chemotherapy combined with radiotherapy/surgery should be the treatment of choice. For non-IMS patients, early combination therapy did not show a significant advantage. Age and location of first presentation were independent factors affecting MS patients’ long-term prognosis.
Myeloid sarcoma (MS) is a tumor mass consisting of primitive or immature myeloid cells that occurs at an extramedullary site. It is also known as granulocytic sarcoma and chloroma. MS mostly presents as progression of malignant hematologic diseases, such as acute myeloid leukemia (AML), chronic myelogenous leukemia (CML), myelodysplastic syndrome (MDS) and myeloproliferative disorders (MPD) [Citation1, Citation2]. AML is the most prevalent disease among all of these.
Isolated myeloid sarcoma (IMS) is a special type of MS, defined as the infiltration of myeloblastic tumor cells into a single or multiple extramedullary organs without evidence of bone marrow (BM) infiltration [Citation3]. The incidence of IMS is about 0.7 per 1 million children and 2 per 1 million adults [Citation4]. If IMS is not treated promptly or adequately, it may progress to AML with a median disease duration of only 5–12 months [Citation5].
Under light microscopy, MS is easily misdiagnosed as non-Hodgkin's lymphoma and other solid tumors, with a 75% misdiagnosis rate [Citation6, Citation7]. The combination of clinical manifestations, pathological patterns, immunohistochemical staining and cytogenetics can lead to an early and timely diagnosis of the disease, which is of certain significance to reduce the misdiagnosis rate, especially for non-leukemic MS [Citation8].
MS is a rare hematological malignant disease with rapid progression and a poor prognosis. AML chemotherapy regimens containing cytarabine are mostly recommended as the initial treatment modality for MS patients, with radiotherapy and surgery as adjuvant treatments. Current research in MS is mostly limited to case reports and small sample studies, and studies on treatment decisions are rare and uncertain [Citation9–13]. To explore the impact of early treatment modalities on the survival of MS patients, we conducted a study using the SEER database. It is reported below.
Materials and methods
Patient selection
The SEER database, established by the National Cancer Institute, is one of the largest cancer databases in the world. What needs illustration is that SEER is a public database with no identifying information, so our study was not approved by the Ethics Committee of the Second Hospital of Shanxi Medical University. Data for this study were obtained from the SEER Research Plus data repository, released in April 2021. This database only records the initial treatment of patients, and in order to fully explore the impact of early treatment on patient survival, we applied for chemotherapy access. This study collected data from patients aged 15 years and older with MS, diagnosed from 2000 to 2018. Based on whether the BM was involved at the time of presentation, MS was classified into isolated myeloid sarcoma (IMS) and non-isolated myeloid sarcoma (non-IMS). Considering the possible delay in bone marrow aspiration and reporting, patients who were not involved at the initial diagnosis but had BM involvement within 1 month were designated as non-IMS. The final data of 472 patients were collected, excluding those with unknown 1st means of treatment, unknown site of onset, and less than 1 month of follow-up.
Study variables
Key patient information was obtained from the database, including age, sex, race, site of onset, follow-up time, survival status, and 1st course of treatment information, and the available information was collated to obtain relevant information such as disease classification, initial site, and number of sites. Onset sites were determined according to the ICD-0-3 site/histology validation list. Age was categorized as 15–59 years, 60–79 years, and 80–85 + years. Race was categorized as white, black, and other. The sites of first attack were divided into 12 groups, specifically: hematopoietic, digestive, thoracic and abdominal (except digestive system), head and neck, lymph nodes, skin, connective and soft tissues, nervous system, reproductive system, urinary system, bone, and other (meaning multiple sites of involvement were found within 1 month of initial diagnosis). The number of sites involved was divided into 3 groups, specifically: 1 site, 2 sites, and 3 or more sites. The focus was on early treatment selection, and treatment was classified as untreated, chemotherapy only, local treatment only, or chemotherapy combined with local treatment, based on information related to the 1st course of treatment.
Statistical methods
Descriptive statistics were used to summarize clinical features. A chi-square test or rank sum test was used to compare clinical characteristics between different groups. Kaplan-Meier curve analysis was used to estimate OS in groups, and log-rank tests were used to compare differences between survival curves. Univariate and multivariate Cox proportional risk models were performed to analyze the prognostic factors of MS patients. OS was defined as the time from the disease was diagnosed until the patient died from any cause. Differences were considered statistically significant at a two-sided p value <0.05. SEER*Stat 8.4.0 was used to collect all of the data for this study. SPSS 26.0 was used for all statistical analyses.
Results
Demographic and clinical characteristics
A total of 472 patients with MS were collected in the SEER database, with a follow-up time of 1–219 months and a median follow-up time of 30.5 months. Of the 472 patients, 244 had IMS and 228 had non-IMS. The median follow-up time for IMS and non-IMS patients was 33 months and 28.5 months, respectively. MS was predominantly male, with a male to female ratio of 1.5:1. MS could occur at any site. The first site in non-IMS patients was mostly in the hematologic system and 86% involved a second site; IMS was seen in connective/soft tissue, reproductive system, chest and abdomen, digestive system, lymph nodes, and skin, and was mostly confined to a single site. Non-IMS patients preferred chemotherapy over local therapy. There were no statistically significant differences in gender, race, and survival status at the end of follow-up between IMS and non-IMS patients, but there were statistically substantial distinctions in terms of age, initial site of disease, number of involved sites, and treatment options (see for details).
Table 1. All of MS patients characteristics.
The effect of MS type on OS has been a hot topic in research on this disease, and this study showed that although IMS patients had longer OS, the difference was not statistically significant, with median OS of 36 and 34 months for IMS and non-IMS patients, respectively (P = 0.178).
Impact of early treatment modalities on patient OS
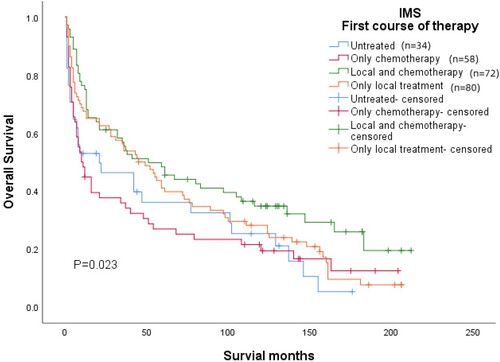
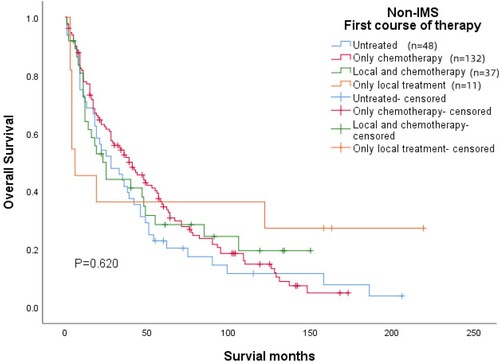
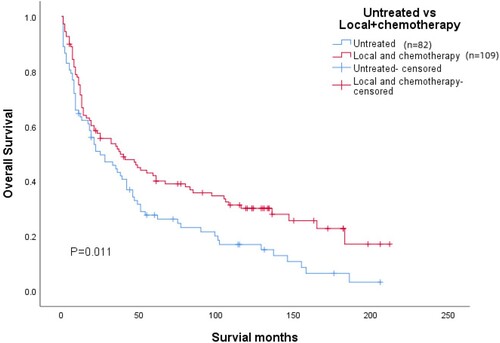
Patients with an unknown treatment modality were excluded, and all patients were included in this analysis. Patients were divided into four groups based on early treatment modality: the untreated group, the chemotherapy group, the local combination chemotherapy group, and the local treatment group. The difference in the effect of different early treatment modalities on patients’ OS was statistically significant (P = 0.024) (see ). Although OS was better in patients with early combination therapy, local treatment, and chemotherapy than in untreated patients, the difference was statistically significant (P = 0.011) in those with combination therapy only ().
Figure 1. Kaplan-Meier plot for early treatment. Different treatment choices in early stages had a significant impact on patient OS (p = 0.024).
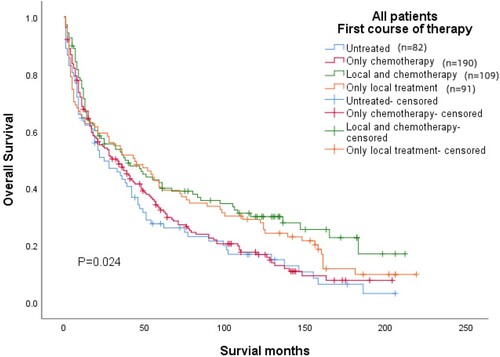
Figure 2. Kaplan-Meier plots for untreated and combined treated patients. OS was substantially prolonged in combination-treated patients over untreated patients (p = 0.011).
Our data showed that IMS patients tended to choose local treatment for disease intervention, and non-IMS patients tended to choose chemotherapy, and both groups of patients used combination therapy as an adjuvant. Using the early treatment modality as the study target, we compared the OS of IMS and non-IMS patients. Notably, IMS patients showed similar results to MS overall (), i.e. the difference in OS between combination-treated and untreated patients was statistically significant (P = 0.023); treated non-IMS patients had longer OS than untreated patients, but the difference was not statistically significant ().
Prognostic factors affecting MS
Based on these results, univariate and multivariate Cox regression analyses were performed to explore independent prognostic factors affecting OS in patients with MS, as shown in . Potential prognostic factors, such as age at diagnosis, gender, race, first site, and first course of treatment, were included in the Cox univariate analysis. The results showed that age, first site, and first course of treatment were factors that influenced OS in MS patients. When the above variables were included in multivariate Cox regression, age and first site were independent prognostic factors affecting OS in MS patients (P < 0.001). Among adult patients, those younger than 60 years had a better prognosis (15–59 years vs. 60–79 years, HR = 2.563, 95%CI = 2.019∼3.253; 15–59 years vs. 80–85 + years, HR = 4.354, 95%CI = 2.875∼6.594). Patients with urinary (HR = 0.305, 95%CI = 0.129∼0.721), digestive l(HR = 0.364, 95%CI = 0.218∼0.607), reproductive system(HR = 0.387, 95%CI = 0.235∼0.636), chest and abdomen(HR = 0.414, 95%CI = 0.251∼0.682) as the first site of the prognosis are good, and the median OS was 98, 89, 61, and 52.5 months, respectively.
Table 2. Univariate and multivariate analysis of OS rates.
Discussion
MS is a rare myeloid tumor characterized by an extramedullary soft tissue mass. It can be a new tumor, and most of it is the manifestation of progression or recurrence of hematologic malignancies. In the FAB Classification of AML, MS is considered a distinctive presentation of AML. It is estimated that 80%–90% of patients with primary MS will have intramedullary AML at the time of diagnosis or later in the course of the disease, while others may have concomitant MDS, MPN, or CML [Citation3].
MS shows male dominance with a male to female ratio of 1.2–1.8:1 [Citation14, Citation15]. The disease could occur at any age, and this study was based on predominantly adult MS, and the results showed a gradual decrease in OS with age. MS can present anywhere in the body, with different clinical presentations depending on the site of onset. The most common sites of MS include the lymph nodes, skin, and soft tissues [Citation16, Citation17]. In addition, MS was more common in the reproductive system and the digestive system, while it was less common in the bone (2.1%), urinary (1.7%), and nervous systems (1.1%).
MS, one of the AML types, is treated mostly with AML chemotherapy regimens, with surgery and radiotherapy as elective adjuvants, but the efficacy is unclear. The present study is the first to focus on the role of early treatment on OS in MS patients using the SEER system. Previous studies have demonstrated that early chemotherapy delays the progression of IMS to AML [Citation18, Citation19]. Goyal et al. [Citation15] analyzed the efficacy of early treatment in the US MS patients and showed that early chemotherapy had no effect on OS in younger patients and was associated with higher mortality in older patients. Tsimberidou et al. [Citation20] analyzed 21 cases of MS and the results suggested that chemotherapy combined with radiotherapy prolonged OS in MS patients. Lan et al. [Citation8] performed a retrospective analysis of 24 MS patients, and OS was prolonged in patients treated by chemotherapy combined with radiotherapy or surgery compared to chemotherapy alone. Nonetheless, there was no statistically significant change. In our study group, IMS patients (244 cases) mostly chose local treatment (80 cases, 32.8%), followed by combination therapy (72 cases, 29.5%), and chemotherapy (58 cases, 23.8%). Early treatment in non-IMS patients was dominated by chemotherapy (132 cases, 57.9%), followed by combination therapy (37 cases, 16.2%), and only 4.8% (11cases) of patients chose local treatment. For IMS patients, OS was clearly prolonged in those treated in combination and the differential was a statistical significance; OS was longer in locally treated patients than in untreated patients, but there is no statistical significance. For patients with IMS, early systemic chemotherapy alone was not sufficient, and chemotherapy combined with local therapy should be the treatment of choice for this group of patients. As seen in Kaplan-Meier , for non-IMS patients, OS was better in early chemotherapy patients than in those who chose other treatments, and AML chemotherapy regimens should be preferred as early treatment for non-IMS patients. Since the SEER database only provides information on early treatment and lacks information related to consolidation and maintenance therapy, there is a lack of evidence on long-term treatment benefits, so our conclusions are also only for early treatment.
In addition, we had limited access to the SEER database and did not collect patient radiotherapy details and transplantation-related information for relevant analysis. The International Lymphoma Radiation Oncology Group has recommended that hematopoietic stem cell transplantation (HSCT) and radiation therapy should be considered in patients with an IMS tumor, an inadequate response to chemotherapy, an isolated recurrence after HSCT, and in cases where rapid symptom relief is required due to stress on the vital structure. A low-dose RT regimen of 24 Gy in 12 fractions was recommended for most patients. Although our study lacks transplant-related information, the existing literature has proved that transplantation patients have longer OS, which is an effective treatment for MS [Citation10, Citation16, Citation21].
The current information on MS is mostly case studies or small sample studies, with little analysis of relevant prognostic factors. Recent years have filled the gap with large-sample MS analyses based on public databases. Movassaghian et al. [Citation22] collated and analyzed 345 IMS patient data and found that there was no difference in the OS of MS patients by gender or race, and patients with MS involving the digestive and reproductive systems had a longer OS. Multivariate analysis of data related to MS patients in the US national database (NCDB) showed that women, Caucasians, young adults, and MS patients occurring in the digestive, urinary, and reproductive systems had longer OS [Citation15]. In this paper, multivariate studies showed that gender, race, and early treatment modality had no effect on the prognosis of MS patients, and that age and first site were independent prognostic factors for OS in MS patients. Patients younger than 60 years old and those with digestive, reproductive, urinary, thoracic and abdominal MS as the first site had a good prognosis. Shan et al. [Citation21] collated information on 74 transplant patients and identified the site and number of extramedullary MS episodes as a potential prognostic factor for MS. Our analysis found that the number of disease sites was correlated with survival time, and the number of disease sites increased with survival time, so the number of disease sites was not included in the prognostic analysis in this study.
In conclusion, our study is one of the few analyses of MS data from a large sample to date that addresses the efficacy of early treatment options for patients with different types of MS. Chemotherapy combined with radiotherapy/surgery should be the preferred treatment option for patients with IMS; cytarabine-based AML chemotherapy regimens should be preferred for patients with non-IMS. Patient age and first site are independent prognostic factors for MS. Despite the limitations of the database and retrospective analysis, it is still instructive and informative for the treatment and prognosis determination of MS.
Geolocation information
Second Hospital of Shanxi Medical University, Wuyi Road, Xinghualing District, Taiyuan City, Shanxi Province, China
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Solh M, Solomon S, Morris L, et al. Extramedullary acute myelogenous leukemia. Blood Rev. 2016;30(5):333–339. doi:10.1016/j.blre.2016.04.001
- Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–2405. doi:10.1182/blood-2016-03-643544
- Shallis RM, Gale RP, Lazarus HM, et al. Myeloid sarcoma, chloroma, or extramedullary acute myeloid leukemia tumor: a tale of misnomers, controversy and the unresolved. Blood. 2021;47:100773. doi:10.1016/j.blre.2020.100773
- Aslam HM, Veeraballi S, Saeed Z, et al. Isolated myeloid sarcoma: a diagnostic dilemma. Cureus. 2022;14(1):e21200. doi:10.7759/cureus.21200
- Sozen M, Vural C, Selek A, et al. Infiltration of thyroid papillary cancer tissue with myeloid leukemic cells: a case report. World J Surg Oncol. 2021;19(1):225. doi:10.1186/s12957-021-02341-z
- Magdy M, Abdel Karim N, Eldessouki I, et al. Myeloid sarcoma. Oncol Res Treat. 2019;42(4):224–229. doi:10.1159/000497210
- Paydas S, Zorludemir S, Ergin M. Granulocytic sarcoma: 32 cases and review of the literature. Leuk Lymphoma. 2006;47(12):2527–2541. doi:10.1080/10428190600967196
- Lan TY, Lin DT, Tien HF, et al. Prognostic factors of treatment outcomes in patients with granulocytic sarcoma. Acta Haematol. 2009;122(4):238–246. doi:10.1159/000253592
- Huang C, Fei S, Yao J, et al. Breast myeloid sarcoma presenting as a palpable breast lump after allogeneic stem cell transplantation for acute myelomonocytic leukemia: a rare case report. World J Surg Oncol. 2021;19(1):289. doi:10.1186/s12957-021-02399-9
- Bianchi S, Capria S, Trisolini SM, et al. Myeloid sarcoma: diagnostic and treatment tools from a monocentric retrospective experience. Acta Haematol. 2021: 1–5. doi:10.1159/000517389
- Slouma M, Rahmouni S, Dhahri R, et al. Epidural myeloid sarcoma as the presenting symptom of chronic myeloid leukemia blast crisis. Clin Rheumatol. 2020;39(8):2453–2459. doi:10.1007/s10067-020-05167-4
- Pasricha TS, Abraczinskas D. Gastrointestinal myeloid sarcoma. N Engl J Med. 2020;383(9):858. doi:10.1056/NEJMicm2001235
- Kaygusuz G, Kankaya D, Ekinci C, et al. Myeloid sarcomas: a clinicopathologic study of 20 cases. Turk J Haematol. 2015;32(1):35–42. doi:10.4274/tjh.2013.0087
- Ullman DI, Dorn D, Jones JA, et al. Clinicopathological and molecular characteristics of extramedullary acute myeloid leukaemia. Histopathology. 2019;75(2):185–192. doi:10.1111/his.13864
- Goyal G, Bartley AC, Patnaik MM, et al. Clinical features and outcomes of extramedullary myeloid sarcoma in the United States: analysis using a national data set. Blood Cancer J. 2017;7(8):e592. doi:10.1038/bcj.2017.79
- Pileri SA, Ascani S, Cox MC, et al. Myeloid sarcoma: clinico-pathologic, phenotypic and cytogenetic analysis of 92 adult patients. Leukemia. 2007;21(2):340–350. doi:10.1038/sj.leu.2404491
- Vardiman JW. The World Health Organization (WHO) classification of tumors of the hematopoietic and lymphoid tissues: an overview with emphasis on the myeloid neoplasms. Chem Biol Interact. 2010;184(1-2):16–20. doi:10.1016/j.cbi.2009.10.009
- Lee JY, Chung H, Cho H, et al. Clinical characteristics and treatment outcomes of isolated myeloid sarcoma without bone marrow involvement: a single-institution experience. Blood Res. 2017;52(3):184–192. doi:10.5045/br.2017.52.3.184
- Imrie KR, Kovacs MJ, Selby D, et al. Isolated chloroma: the effect of early antileukemic therapy. Ann Intern Med. 1995;123(5):351–353. doi:10.7326/0003-4819-123-5-199509010-00005
- Tsimberidou AM, Kantarjian HM, Estey E, et al. Outcome in patients with nonleukemic granulocytic sarcoma treated with chemotherapy with or without radiotherapy. Leukemia. 2003;17(6):1100–1103. doi:10.1038/sj.leu.2402958
- Shan M, Lu Y, Yang M, et al. Characteristics and transplant outcome of myeloid sarcoma: a single-institute study. Int J Hematol. 2021;113(5):682–692. doi:10.1007/s12185-021-03081-2
- Movassaghian M, Brunner AM, Blonquist TM, et al. Presentation and outcomes among patients with isolated myeloid sarcoma: a surveillance, epidemiology, and end results database analysis. Leuk Lymphoma. 2015;56(6):1698–1703. doi:10.3109/10428194.2014.963080