ABSTRACT
Background
Several non-invasive technologies are nowadays available in the market which claim to determine the hemoglobin levels instantly without the requirement of the blood sample. But no study has shown the significance of such non-invasive devices on a routine basis for determining their impact on anemia reduction programs. This study is conducted to determine the impact of regular hemoglobin screening on the women population to determine its potential in reducing anemia, using a digitalized non-invasive device.
Method
A cross-sectional study was conducted on 203 women of reproductive age group, residing in the Moradabad district. Repetitive readings were taken after a time interval of a minimum of 1 month for determining the impact of regular screening. The entire data collection process was carried out using the EzeCheck mobile app.
Results
It was observed that the prevalence of anemia was reduced upon the second time screening and was accepted by the women population. Repetitive testing has a significant impact on reducing anemia prevalence. Also, the simplified non-invasive technology for estimating the hemoglobin values, makes the user more comfortable to take the test.
Conclusion
Non-invasive devices should be used regularly to keep track of hemoglobin levels which will help in the effective treatment of anemia. The mobile app-based testing could help to easily evaluate the reports of the patients from any remote location with instant result interpretation and health assistance.
Introduction
Anemia is a major challenge across the globe. Several geographical regions of the Earth, majorly Africa and South-East Asia, face high prevalence rates of anemia. Estimates from WHO (World Health Organization) have revealed that 40% of children aged 6–59 months, 37% of pregnant women, and 30% of women of age 15–49 years worldwide, are anamic.
Anemia is a medical condition which occurs due to lack/malfunctioning of red blood cells due to the lack of oxygen supply to the organs, affecting overall physical and mental development. As per the WHO guidelines, anemia is defined as the condition where the hemoglobin levels are <12 g/dL for non-pregnant women while <11 g/dL for pregnant women and children aged under 5 years of age [Citation1]. Recent reports from the WHO suggest that in the Southeast Asian Region, a large number of adolescents, constituting 20% of the population of these countries, suffer from malnutrition and anemia, which adversely affect their health and mind development [Citation2]. In India, anemia is a national calamity affecting 50% of the women population and 75% of the children [Citation3].
Anemia in reproductive-aged women is a significant health concern globally. It can be due to iron deficiency, chronic diseases, genetic disorders, inadequate nutrition, etc.. Anemia, among married women, can ultimately lead to serious health consequences for future mothers [Citation4]. Worldwide, more than 1,15,000 maternal deaths are attributed due to anemia annually [Citation5]. Globally, nearly 40% of pregnant women and 33.33% of non-pregnant women within the reproductive age group have anemia [Citation6,Citation7]. Statistical findings have interpreted that the anemia prevalence in reproductive-aged women, is highest in low- and middle-income countries likely due to the relationship with dietary factors, nutrient deficiencies, and increased occurrence of several infectious diseases [Citation8,Citation9]. Among reproductive-aged women, iron deficiency is the most common cause of anemia worldwide, due to menstrual blood loss [Citation10] and increased iron demands during pregnancy [Citation11]. Poor dietary intake of iron-rich foods, such as red meat, leafy green vegetables, and fortified cereals, are other factors which contribute to anemia among reproductive-aged women [Citation12]. Genetic disorders, such as thalassemia and sickle cell disease, can also cause chronic anemia in affected individuals [Citation13]. An anemic woman has an increased risk toward adverse birth outcomes, including the risk of maternal death and pre-term delivery with a low-birth-weight baby [Citation14–16]. It is known that anemic mothers give birth to anemic children. The more acute the anemia of the mother the more severe the child is affected. Studies have also revealed the adverse consequences of anemia on the work capacity due to a diet deficient in calorie, micronutrient, and macronutrient content [Citation17–19]. Improper food patterns having a lack of certain vital nutrients and vitamins along with excessive physical exertion can ultimately lead to anamia. This is the major cause why most of the Indian women, especially from rural set-ups are found to be anemic [Citation20]. Improving access to healthcare services, especially in low-resource settings, is crucial for the early detection and management of anemia in reproductive-aged women.
Several states of India, such as West Bengal, Haryana, Odisha, Jharkhand, Bihar, Punjab, and Rajasthan, are the major states where anemia prevalence is much higher than the other states. Like these states, anemia is a major health problem in Uttar Pradesh, especially among women and children. As per the current statistical findings Moradabad alone contributes to 62% of anemic women aged 15–49 years compared to the entire 52% of the state level. NFHS-5 reports indicate that all other children in the Moradabad district are suffering from anemia [Citation21].
One of the major causes of this is the deprivation of proper healthcare facilities in such areas. Despite several government programs and initiatives like Anemia Mukt Bharat (AMB), POSHAN and National Iron Plus Initiative, the target to reduce anemia prevalence has not been reached. Major bottlenecks, such as lack of awareness, lack of routine screening, phobia of needles among children, the requirement for expensive reagents, etc., are the roadblocks for the above initiatives. Also, due to certain dietary preferences among the women population, the prevalence of anemia is high. As per the findings of a study conducted in Uttar Pradesh, on pregnant women [Citation22], the daily iron intake was unable to meet the recommended dietary allowance and differed by the individual’s diet preferences such as lactovegetarian vs. non-vegetarian, etc.
With the advancement in technology, several hemoglobinometers are available in the market to tackle one or the other bottleneck against government programs. Although devices like HemoCue have reduced the sample processing time and requirement for proper medical setup, it still can’t be used for regular screening purposes since it is an invasive procedure for determining the levels of hemoglobin. Also, these methods of Hb determination are expensive, require skilled personnel, and are not accessible to all parts of the world, particularly in countries like India where several parts have low- and middle-resource settings. Applying a non-invasive point-of-care device solution in such regions can facilitate faster results, with less pain and discomfort for the end user.
The present study was conducted to identify the potential effectiveness of a non-invasive technology (EzeCheck) in anemia eradication through routine screening, among women of reproductive age, residing in Moradabad city, Uttar Pradesh. Since EzeCheck has been diagnostically validated as an effective screening tool over the invasive methods [Citation23] for hemoglobin estimation among masses, we have used EzeCheck for conducting this study.
Materials and methods
Design and setting
With permission from local administrators and competent state authorities, and ethical approval from KIMS (Kalinga Institute of Medical Sciences), we assessed the Hgb of individuals using EzeCheck- a non-invasive hemoglobin screening device which provides instant hemoglobin values in the range of 7–16 g/dL. A cross-sectional study was performed involving the ASHA workers who conducted several camps at different localities of the city to determine the hemoglobin levels of the women. The non-invasive tests were conducted monthly and were completely voluntarily. Women willing to take the test were verbally informed and the written consent was obtained prior to the initiation of the test process. In the case of minor girls (age < 18 years), appropriate written consent from their parent/guardian was obtained.
The number of females, who took the non-invasive tests for the first time, were asked to have a second time screening (within 1–6 months) as well to determine the effectiveness of the test process. The tests were conducted from Jan 2022 to February 2023.
Study population
We included women participants of reproductive age group starting from the age of 15 years to 49 years. We did not restrict individuals from participating in the assessment except for those who had tar, soot or mehndi applied on their left-hand ring fingertip or aged 50 years and above, and those who refused verbal consent were excluded.
Data collection
Initially, the basic information, such as age and disease profile, was captured for the consenting individuals and was recorded using the EzeCheck mobile app (connected with the EzeCheck device via Bluetooth). Once the basic details of the subjects were successfully entered, the device was positioned to capture the signal from the reflection of the LED light from the subject’s fingertip, for the estimation of Hgb levels. Then, the device ran a series of signal processing techniques at the backend with the machine learning algorithm and artificial intelligence, to generate the hemoglobin value for the subject taking the test, and the results were displayed on the connected mobile app. The whole process took around 45 s; the reading was then archived. Each of the participants was measured twice with a difference in the time of the second screening.
Data management and analysis
The Hgb levels of the participants were stored in the EzeCheck web application. The data were then exported in digital format and reported in MS Excel. Statistical analyses of the data were performed using MS Excel and Matplotlib 3.7.2, Plotly 5.16.1 libraries of Phyton.
We undertook descriptive analyses (frequency, percentage, and mean and standard deviation/median with range, as appropriate) to provide a profile of the samples used. For comparing the performance of EzeCheck, we categorized the Hgb (first and second screening) as ‘anemia’ and ‘no anemia’. We used the value-specific WHO criteria for anemia classification [Citation23] as cut-offs: Hgb value <12 g/dL as mild anemia, Hgb values between 8 and –10.9 g/dL as moderate anamia while Hgb values <8 g/dL as severe anemia.
Ethics
All potential women participants were explained about EzeCheck before the assessment. Verbal and written informed consent was obtained from all the participants before measuring their hemoglobin using EzeCheck. The participant’s name, address details or any other personal identifier was not collected. Only age and Hgb estimates were captured using the app and unique system-generated numeric IDs were used for analysis.
Results
A total of 203 women, aged 15–49 years, were screened twice with different time intervals (in months) for determining the hemoglobin values using the non-invasive device. No dropout cases were observed between the first and second screening since all the enrolled women were advised to continue the regular follow-up mechanism for the study and all of them participated in the second screening, enthusiastically. The entire population was categorized into four major categories depending on the observed hemoglobin values: women having Hgb value ≥12 g/dL as Normal, Hgb value between 11 and –11.9 g/dL as Mild anemic, Hgb values between 8 and –10.9 g/dL as Moderate anemic while women having, observed Hgb value as <8 g/dL, were categorized as Severe anemic. The mean age of the women involved in the study was 20.17 ± 7.23 years.
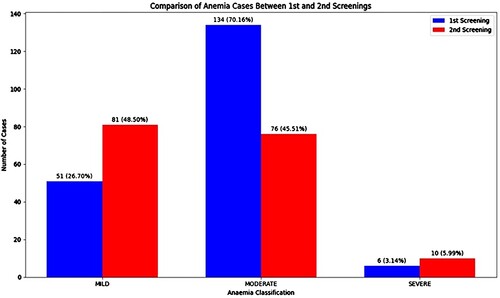
During the first screening, the prevalence of anemia observed among the women population was 94.1% (Mild: 25.13%, Moderate: 66.01% & Severe: 2.96%) while it reduced to 82.2% (Mild: 39.9%, Moderate: 37.4% and Severe: 4.9%) on second screening. The average time interval between the first and the second screening was 68.49 ± 50.84 days.
The difference in anemia prevalence on the first and second screening has been shown in for all three anemia categories (Mild, Moderate and Severe).
The mean (±SD) hamoglobin levels on the first and second screenings were 10.32 ± 1.15 g/dL and 10.93 ± 1.31 g/dL, respectively. The prevalence of Moderate class of anemia (Hgb value between 8 and –10.9 g/dL) was highest among the studied population during the first screening and the prevalence of mild anemia was highest during the second time screening.
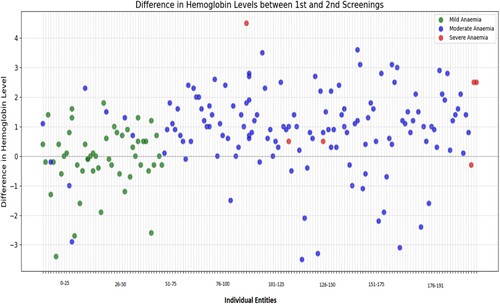
The difference in the Hgb values of both the first and second screening has been represented in , indicating a positive response (increase in the Hb levels on the second screening) of 76% in the studied anemic cases. Out of these, 38.21% of the anemic cases had a Hgb difference within 0–1 g/dL, 23.03% had a difference between 1.1 and –2 g/dL, 12.04% had a difference of 2.1–3 g/dL, while only 2.61% had a difference greater than 3 g/dL on their second screening. Out of 191 anemic cases observed during the first screening, the Hgb levels decreased for 46 women during the second screening i.e. the difference between the two Hgb values (second screening Hgb- first screening Hgb) was negative.
Figure 2. Scatter plot representing the effect of second time screening on the anemic population with respect to the observed difference in the Hgb values.
50.7% of the moderate anemic cases had either mild anemia or normal Hgb values, on their second screening. The percentage of anemic population (mild, moderate, and severe) present as per their range of difference values (second screening Hgb value – first screening Hgb value), has been represented in . Out of 191 anemic cases, 7 individuals (3 Mild and 4 Moderate anemic) had a difference greater than –2.5 g/dL between the two screenings; 8 individuals (Mild = 2 and Moderate = 6) had a range of difference of –2.5 g/dL to –1.5 g/dL; 14 individuals (Mild = 8 and Moderate = 6) had a range of difference of –1.5 g/dL to –0.5 g/dL; 52 individuals (Mild = 25, Moderate = 24 and Severe = 3) had a difference range of –0.5 g/dL to 0.5 g/dL; 66 cases (Mild = 11 and Moderate = 55) had a difference range of 0.5 g/dL to 1.5 g/dL; 31 cases (Mild = 2, Moderate = 27 and Severe = 2) had a range of difference of 1.5 g/dL to 2.5 g/dL while 13 individuals (Moderate = 12 and Severe = 1) had a difference >2.5 g/dL.
Figure 3. The bubble chart represents the anemia prevalence after obtaining the differences from both the first and second non-invasive screening.
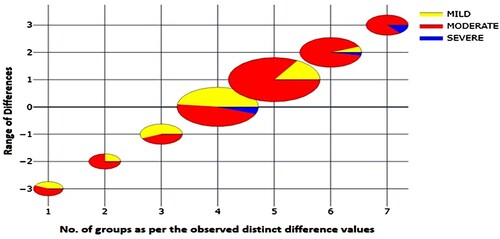
Most of the anemic population (61.25%) had a difference of 0 to +2 g/dL in their first- and second-time screening, indicating a positive response to the routine screening intervention.
Discussion
This study was conducted to investigate the prevalence of anemia among women in Moradabad city and assess the effectiveness of routine non-invasive hemoglobin monitoring in addressing this health concern. Despite various interventions, anemia remains a significant issue in several regions across India. The findings of this study highlight the persistent prevalence of anemia among women in Moradabad, indicating the need for targeted interventions.
The study revealed that conducting non-invasive hemoglobin tests at regular intervals, in conjunction with government initiatives, can play a crucial role in addressing anemia. Research has consistently shown that multiple factors contribute to anemia in young women, with iron deficiency being the most prevalent cause [Citation24–26]. Heavy menstrual bleeding is identified as a leading cause of iron deficiency in women of reproductive age, often compounded by inadequate dietary intake [Citation27,Citation28].
An analysis of data from 15 countries underscores the global burden of anemia, with India projected to have the highest prevalence by 2025. To achieve global targets for anemia reduction, it is essential to implement effective interventions and monitor progress regularly [Citation29]. In Moradabad, timely interventions were recommended for women identified with anemia during non-invasive screenings, including dietary modifications and lifestyle changes.
Digital health tools, such as the EzeCheck device, facilitated access to medical advice and support for women in Moradabad. The app's digital reporting feature enabled individuals to share hemoglobin reports with healthcare providers, overcoming barriers such as lack of transportation and access to medical facilities.
The study observed a reduction in moderate anemia cases during follow-up screenings, suggesting improvements in hemoglobin levels. However, challenges such as non-adherence to iron supplementation and side effects of iron supplements were identified as potential barriers to addressing severe anemia cases [Citation30–32]. Also, another study found that the tablet’s unappealing taste, smell, or color, nausea, difficulty in swallowing and form of injection/liquid were some of the major deciding factors for women to discontinue taking iron supplements [Citation33–37].
Routine non-invasive hemoglobin screening, coupled with targeted interventions, is proposed as a cost-effective approach to reducing anemia prevalence among women in developing countries like India. Addressing structural and non-structural factors contributing to anemia requires a comprehensive strategy, including adequate training for healthcare providers and the adoption of innovative digital solutions like EzeCheck.
While the study had limitations, such as a lack of data on iron supplementation and reasons for increased severe anemia cases, it underscores the positive impact of routine hemoglobin screening using non-invasive digital approaches in reducing anemia prevalence among women of reproductive age. Further research is warranted to explore the combined impact of iron supplementation and routine non-invasive testing on anemia prevalence.
Conclusion
For the expedient and efficient management of anemia, early diagnosis facilitated by the utilization of a Non-invasive digital hemoglobin screening device (EzeCheck) is imperative. EzeCheck is found to be easy to operate, cost-effective, eco-friendly, swift in providing results, and easy to set up across diverse geographical regions. Proper use of such non-invasive devices will help to effectively measure the hemoglobin levels at regular intervals of time.
Also, with the highly advanced digital feature of the device, one can effectively track the progress of various supplementation programs by regular (monthly basis) screening of the Hgb levels with digitalized record maintenance in the EzeCheck app.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Anaemia. https://www.who.int/data/nutrition/nlis/info/anaemia#:~:text = WHO%20defines%20anaemia%20in%20children,levels%20are%20easy%20to%20administer.
- Awasthi R, Srivastava A, Dixit AK, et al. Nutritional status of adolescent girls in urban slums of Moradabad: a cross sectional study. Int J Community Med Public Health. 2016;3(1):276–280. doi:10.18203/2394-6040.ijcmph20151576
- Girija PL. Anaemia among women and children of India. Anc Sci Life. 2008 Jul;28(1):33.
- WHO. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: World Health Organization; 2016. Available from: https://apps.who.int/iris/handle/10665/250796.
- Cappellini MD, Santini V, Braxs C, et al. Iron metabolism and iron deficiency anemia in women. Fertil Steril. 2022 Sep 6;118(4):607–614.
- Ezzati M, Lopez AD, Rodgers AA, et al. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. World Health Organization; 2004.
- Harris-Fry H, Shrestha N, Costello A, et al. Determinants of intra-household food allocation between adults in South Asia–a systematic review. Int J Equity Health. 2017 Dec;16(1):1–21. doi:10.1186/s12939-017-0603-1
- Stevens GA, Finucane MM, De-Regil LM, et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: a systematic analysis of population-representative data. Lancet Glob Health. 2013 Jul 1;1(1):e16–e25. doi:10.1016/S2214-109X(13)70001-9
- Derman RJ, Patted A. Overview of iron deficiency and iron deficiency anemia in women and girls of reproductive age. Int J Gynaecol Obstet. 2023 Aug;162:78–82. doi:10.1002/ijgo.14950
- Munro MG, Critchley HO, Fraser IS. The flexible FIGO classification concept for underlying causes of abnormal uterine bleeding. In Seminars in reproductive medicine 2011 Sep (Vol. 29, No. 05, pp. 391-399). © Thieme Medical Publishers.
- Who C. Worldwide prevalence of anaemia 1993–2005. WHO Global Database on Anaemia; 2008.
- Killip S, Bennett JM, Chambers MD. Iron deficiency anemia. Am Fam Physician. 2007 Mar 1;75(5):671–678.
- Weatherall DJ. The inherited diseases of hemoglobin are an emerging global health burden. Blood J Am Soc Hematol. 2010 Jun 3;115(22):4331–4336.
- Daru J, Zamora J, Fernández-Félix BM, et al. Risk of maternal mortality in women with severe anaemia during pregnancy and post partum: a multilevel analysis. Lancet Glob Health. 2018 May 1;6(5):e548–e554. doi:10.1016/S2214-109X(18)30078-0
- Rosenthal J, Lopez-Pazos E, Dowling NF, et al. Folate and vitamin B12 deficiency among non-pregnant women of childbearing-age in Guatemala 2009–2010: prevalence and identification of vulnerable populations. Matern Child Health J. 2015 Oct;19:2272–2285. doi:10.1007/s10995-015-1746-6
- Child Health Epidemiology Reference Group; Kozuki N, Lee AC, Katz J. Moderate to severe, but not mild, maternal anemia is associated with increased risk of small-for-gestational-age outcomes. J Nutr. 2012 Feb 1;142(2):358–362. doi:10.3945/jn.111.149237
- Kalasuramath S, Kumar V, Kumar M, et al. Impact of anemia, iron defienciency on physical and cardiorespiratory fitness among young working women in India. Indian J Basic Appl Med Res. 2015;4:119–126.
- Roy SK. Factors affecting the work productivity of Oraon agricultural laborers of Jalpaiguri district, West Bengal. Am J Phys Anthropol. 2002 Mar;117(3):228–235.
- Edgerton VR, Gardner GW, Ohira Y, et al. Iron-deficiency anaemia and its effect on worker productivity and activity patterns. Br Med J. 1979 Dec 15;2(6204):1546–1549. doi:10.1136/bmj.2.6204.1546
- Hasan MM, Magalhaes RJ, Garnett SP, et al. Anaemia in women of reproductive age in low-and middle-income countries: progress towards the 2025 global nutrition target. Bull World Health Organ. 2022 Mar 3;100(3):196. doi:10.2471/BLT.20.280180
- https://www.amarujala.com/uttar-pradesh/moradabad/anemia-in-every-second-child-of-the-district-moradabad-news-mbd4193664121.
- Bellows AL, Kachwaha S, Ghosh S, et al. Nutrient adequacy is low among both self-declared lacto-vegetarian and non-vegetarian pregnant women in Uttar Pradesh. Nutrients. 2020 Jul 17;12(7):2126. doi:10.3390/nu12072126
- Sahoo KC, Sinha A, Sahoo RK, et al. Diagnostic validation and feasibility of a non-invasive haemoglobin screening device (EzeCheck) for'Anaemia Mukt Bharat'in India. Cureus. 2024 Jan 24;16(1).
- Donnez J, Carmona F, Maitrot-Mantelet L, et al. Uterine disorders and iron deficiency anemia. Fertil Steril. 2022 Oct 1;118(4):615–624. doi:10.1016/j.fertnstert.2022.08.011
- Jain V, Chodankar RR, Maybin JA, et al. Uterine bleeding: how understanding endometrial physiology underpins menstrual health. Nat Rev Endocrinol. 2022 May;18(5):290–308. doi:10.1038/s41574-021-00629-4
- Petraglia F, Dolmans MM. Iron deficiency anemia: impact on women’s reproductive health. Fertil Steril. 2022 Oct 1;118(4):605–606. doi:10.1016/j.fertnstert.2022.08.850
- Hentze MW, Muckenthaler MU, Galy B, et al. Two to tango: regulation of Mammalian iron metabolism. Cell. 2010 Jul 9;142(1):24–38. doi:10.1016/j.cell.2010.06.028
- Zhang Q, Ananth CV, Rhoads GG, et al. The impact of maternal anemia on perinatal mortality: a population-based, prospective cohort study in China. Ann Epidemiol. 2009 Nov 1;19(11):793–799. doi:10.1016/j.annepidem.2009.06.002
- De Benoist B, Cogswell M, Egli I, et al. Worldwide prevalence of anaemia 1993-2005. WHO Global Database of anaemia; 2008.
- Tessema J, Jefferds ME, Cogswell M, et al. Motivators and barriers to prenatal supplement use among minority women in the United States. J Am Diet Assoc. 2009 Jan 1;109(1):102–108. doi:10.1016/j.jada.2008.10.013
- Galloway R, Dusch E, Elder L, et al. Women's perceptions of iron deficiency and anemia prevention and control in eight developing countries. Soc Sci Med. 2002 Aug 1;55(4):529–544. doi:10.1016/S0277-9536(01)00185-X
- Jefferds MD. Concepts of iron deficiency anemia and public health measures in rural Costa Rica. Soc Sci Med. 2002 Oct 1;55(7):1143–1156. doi:10.1016/S0277-9536(01)00254-4
- Seck BC, Jackson RT. Determinants of compliance with iron supplementation among pregnant women in Senegal. Public Health Nutr. 2008 Jun;11(6):596–605. doi:10.1017/S1368980007000924
- Ejidokun OO. Community attitudes to pregnancy, anaemia, iron and folate supplementation in urban and rural Lagos, south-western Nigeria. Midwifery. 2000 Jun 1;16(2):89–95. doi:10.1054/midw.1999.0196
- Ghanekar J, Kanani S, Patel S. Toward better compliance with iron–folic acid supplements: understanding the behavior of poor urban pregnant women through ethnographic decision models in Vadodara, India. Food Nutr Bull. 2002;23(1):65–72. doi:10.1177/156482650202300109
- Wulff M, Ekström EC. Iron supplementation during pregnancy in Sweden: to what extent is the national recommendation followed? Acta Obstet Gynecol Scand. 2003 Jan 1;82(7):628–635. doi:10.1034/j.1600-0412.2003.00186.x
- Hyder SZ, Persson LÅ, Chowdhury AM, et al. Do side-effects reduce compliance to iron supplementation? A study of daily-and weekly-dose regimens in pregnancy. J Health Popul Nutr. 2002 Jun 1;20(2):175–179.