Abstract
Introduction: Non-communicable diseases, especially cardiovascular diseases (CVD), have become more prevalent across the world, more so in developing countries. Novel methods in the management of CVD risks in patients with diabetes mellitus, type 2 (DM2) requires constant attention and an ever-evolving approach. The role of magnesium supplementation in the management of CVD has been described, but the relationship between serum magnesium (Mg) and the lipid subsets have had conflicting results in different population groups.
Methods: A cross-sectional study was performed by collecting data on patients with DM2 from a specialised diabetes clinic at Edendale Hospital, Pietermaritzburg, KwaZulu-Natal, South Africa, between July 1, 2015 and June 30, 2016. Lipid subsets (total cholesterol [TC], high-density lipoprotein cholesterol [HDL], low-density lipoprotein cholesterol [LDL] and triglycerides [TG]), age, sex and Mg were recorded for analysis.
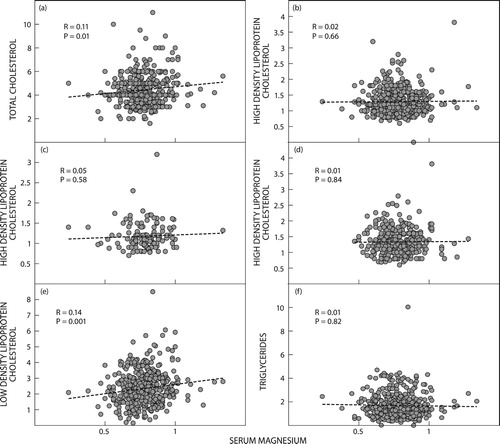
Results: A total of 495 clinical data sheets were analysed. The majority of participants were female (73.45%) with a mean age of 56.97 years. A statistically significant, positive, linear relationship was found between Mg and TC (R = 0.11; p = 0.01) as well as Mg and LDL R = 0.14; p = 0.001), but not between Mg and HDL (R = 0.02; p = 0.66) and Mg and TG (R = 0.01; p = 0.82).
Discussion: The results of this study are similar to findings by a group of researchers in China and differ when compared with studies observing Caucasian patients. It is plausible that intrinsic ethnic differences in lipid metabolism and the various ways in which magnesium requiring enzymatic processes are utilised may be responsible for the results found in the present study population versus those found in Caucasian study participants in other countries. More research is required to determine the effect of magnesium supplementation and CVD outcomes in the present study population.
Introduction
Non-communicable diseases (NCD) have become more prevalent as part of the so-called epidemiological shift.Citation1 More than two-thirds of deaths globally in 2012 were attributed to NCD.Citation2 Cardiovascular disease (CVD) accounted for 46% of these deaths, with diabetes mellitus (DM) linked to another 1.5 million deaths. This burden is experienced by individuals in developing countries at a high rate. The WHO estimates that low- and middle-income countries carry 83% of the burden of deaths due to NCDs. This makes it important to develop multifaceted approaches when managing these modifiable conditions.
Serum lipid subsets (low density lipoprotein cholesterol [LDL], high density lipoprotein cholesterol [HDL] and total cholesterol [TC] as well as triglycerides [TG]) have been implicated in the development of CVD. HDL shows an inverse relationship with CVD, while LDL has been shown to increase the risk of CVD and is a good predictor of CVD in patients with DM.Citation3,Citation4 A similar positive relationship exists between TG and CVD.Citation5
Relationship between plasma magnesium (Mg) levels and lipid profiles in patients with diabetes mellitus, type 2 (DM2) remains controversial.
Numerous studies have shown a relationship between Mg and the lipid subsets; however, the conclusions drawn from these studies differ markedly. In 2012 Huang et al. studied a population of individuals with DM2 to determine the correlation between Mg and metabolic parameters. They found a positive relationship between Mg and HDL and a negative correlation between Mg and TG.Citation6 Rasheed et al. found a significant relationship between Mg and HDL and a negative relationship between Mg and LDL and TC.Citation7 In 2016 Cao et al. found a positive relationship between Mg and all the lipid subsets.Citation8 Mirmiran et al., however, found no relationship at all between Mg and the lipid subsets.Citation9 Data in the African context remain scarce.
A meta-analysis of studies conducted worldwide (and published in English) in 2017 reported that magnesium supplementation in individuals with DM2 has a positive effect on their CVD outcomes.Citation10 The effects of the magnesium supplementation are likely multifactorial and the authors advised that larger RCTs be conducted. It is not clear whether African populations have been represented appropriately in the studies performed. This is important as magnesium handling, in conjunction with various other minerals such as calcium, differs between races where, for example, individuals of African descent have been found to excrete magnesium less readily than their Caucasian counterparts.Citation11 Lipid metabolism, too, differs depending on race. African American women have been shown to have a higher apoCIII level than Caucasian women, which affects the way HDL is handled.Citation12
With the differing relationships shown between Mg and the lipid subsets it is important to understand the relationship experienced by specific populations. This study hopes to add to the body of knowledge and assist the clinician in the decision to advise supplementation with magnesium.
Methods
A cross-sectional study was performed by collecting data on patients with DM2 from a specialised diabetes clinic at Edendale Hospital, Pietermaritzburg, KwaZulu-Natal, South Africa, between July 1, 2015 and June 30, 2016. Data were collected by reviewing information recorded on the standardised clinic tool used by this clinic.Citation13 The use of the data was approved by the University of KwaZulu-Natal Biomedical Research Ethics Committee (BCA 194/15).
The following data were recorded for analysis:
Lipid subsets (TC, HDL, LDL, TG)
Age
Sex
Mg
Normal lipid subset values (in mmol/l) were assumed at values below target value for patients with DM:Citation14,Citation15
TC < 4.5
LDL < 1.8
HDL > 1 (in males); >1.2 (in females)
TG < 1.7
Mg was measured using the Siemens Dimension clinical chemistry system (Siemens Healthcare Diagnostics Inc, Deerfield, IL, USA), which utilises a photometric method, a modified methylthymol blue (MTB) complexometric procedure. This is the commonest method used worldwide, with an assay range of 0.0–8.22mmol/l. The assigned coefficients are as follows: C0 −0.200 and C1 0.100. Tests were performed by the National Health Laboratory Service.
The data were analysed using the SOFA Statistics software (ver. 1.4.6) (http://www.sofastatistics.com/downloads.php) and Microsoft Excel (Microsoft Corp, Redmond, WA, USA). Univariate and multivariate analyses were performed. Results were deemed statistically significant at a p-value of < 0.05.
Results
The study reviewed 495 clinical data sheets. The mean age of the patients was 56.97 years (±SD 12.29 years). Male patients totalled 126 (25.45%), female patients totalled 364 (73.54%) and unrecorded sex totalled 5 (1.01%). The mean Mg was 0.78mmol/l (SD 0.12mmol/l).
Table 1: Multivariate analysis of the mean serum magnesium of, and its relationship with, the lipid subsets
a and e demonstrate significant, linear, positive relationships between Mg and TC and Mg and LDL, respectively. demonstrate the lack of significant relationships.
Figure 1: (a) Relationship between serum magnesium and total cholesterol. (b) Relationship between serum magnesium and high-density lipoprotein cholesterol. (c) Relationship between serum magnesium and high-density lipoprotein cholesterol (males). (d) Relationship between serum magnesium and high-density lipoprotein cholesterol (females). (e) Relationship between serum magnesium and low-density lipoprotein cholesterol. (f) Relationship between serum magnesium and triglycerides.
Discussion
The epidemiological shift has seen a rise in the prevalence of NCD across the world.Citation1 New strategies need to be developed to curb the effects of NCD on the lives of millions. A meta-analysis published in 2017 suggested that magnesium supplementation has a positive effect on the outcome of CVD in patients with DM2.Citation10 The relationship between Mg and the lipid subsets differ from study to study, depending on the population studied. Studies analysing data obtained from individuals of African and Asian descent yield different results when compared with studies where the population consists mainly of Caucasian individuals.Citation16,Citation17 It is therefore important to understand the correlation between Mg and the lipid subsets in the local population to sensitise the clinician to the possible population-specific relationship. This study aimed to do that.
The sample population consisted mainly of females (73.54%) with a mean age of 56.97. The mean Mg level was 0.78 mmol/l. A statistically significant, positive relationship was found between Mg and TC (p = 0.01) as well as between Mg and LDL (p = 0.001). These findings are comparable to those published by Cao et al.8 There was no evidence of a relationship between Mg and HDL (0.66) or TG (0.82).
Intrinsic ethnic differences in lipid metabolisms is well known, with overweight Caucasian females having a higher visceral fat mass (VFM) compared with overweight African females.Citation18 This is significant as visceral fat and subcutaneous fat are metabolically different structures and respond to nutrients in varied ways.Citation19,Citation20 Although data pertaining to the differences in enzyme concentrations and their response to Mg are scarce, this may be a potential explanation for the findings of our study, compared with those of other researchers. Magnesium is an important rate-limiting factor in the biosynthesis of cholesterol in humans, where Mg acts by controlling the enzymatic activity of HMG CoA reductase (similar to statins), lecithin cholesterol acyl transferase and desaturase.Citation21 At the correct cellular concentration Mg acts by inhibiting calcium channels, modulating various cellular processes and hence CVD risk. If the cellular activity of these enzymes differs significantly in visceral vs. subcutaneous adipocytes, the effect of Mg will differ from population to population.
Dietary and lifestyle differences in different populations and the resultant effect on both Mg and the lipid subsets must be considered. The epidemiological shift of NCD, the burden of obesity affecting developing countries and ever-increasing rates of metabolic syndrome in sub-Saharan Africa and Asia could be a contributing factor in the differences observed.Citation22,Citation23
Many limitations have been identified. Being a cross-sectional study no causal relationship can be established. Information regarding body mass, co-morbidities (such as established deranged lipid profiles), the use of lipid or Mg altering drugs (such as statins), ethanol intake and daily dietary intake have not been recorded. It is recommended that in future studies these potentially confounding factors be considered.
The purpose of this study was to add to the body of knowledge regarding the relationship between Mg and the lipid subsets, as well as to sensitise clinicians to the potential impact of magnesium supplementation on lipids in patients with DM2.
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
JM Jansen van Vuuren http://orcid.org/0000-0002-7356-1824
S Pillay http://orcid.org/0000-0002-5604-645X
References
- Omran AR. The epidemiologic transition: a theory of the epidemiology of population change. Milbank Q. 2005;83(4):731–757. doi: 10.1111/j.1468-0009.2005.00398.x
- World Health Organization. Global status report on noncommunicable diseases 2014 [document on the Internet]. Geneva: World Health Organization; 2014. Available from: http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf?ua=1.
- Boden WE. High-density lipoprotein cholesterol as an independent risk factor in cardiovascular disease: assessing the data from Framingham to the veterans affairs high--density lipoprotein intervention trial. Am J Cardiol. 2000;86(12A):19–22. doi: 10.1016/S0002-9149(00)01464-8
- Howard BV, Robbins DC, Sievers ML, et al. LDL cholesterol as a strong predictor of coronary heart disease in diabetic individuals with insulin resistance and low LDL: the strong heart study. Arterioscler Thromb Vasc Biol. 2000;20(3):830–835. doi: 10.1161/01.ATV.20.3.830
- Miller M, Stone NJ, Ballantyne C, et al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circ. 2011;123(20):2292–2333. doi: 10.1161/CIR.0b013e3182160726
- Huang JH, Lu YF, Cheng FC, et al. Correlation of magnesium intake with metabolic parameters, depression and physical activity in elderly type 2 diabetes patients: a cross-sectional study. Nutr J. 2012;11:41. doi: 10.1186/1475-2891-11-41
- Rasheed H, Elahi S, Ajaz H. Serum magnesium and atherogenic lipid fractions in type II diabetic patients of Lahore, Pakistan. Biol Trace Elem Res. 2012;148(2):165–169. doi: 10.1007/s12011-012-9361-5
- Cao Y, Wang C, Guan K, et al. Association of magnesium in serum and urine with carotid intima-media thickness and serum lipids in middle-aged and elderly Chinese: a community-based cross-sectional study. Eur J Nutr. 2016;55(1):219–226. doi: 10.1007/s00394-015-0839-8
- Mirmiran P, Shab-Bidar S, Hosseini-Esfahani F, et al. Magnesium intake and prevalence of metabolic syndrome in adults: Tehran lipid and glucose study. Public Health Nutr. 2012;15(4):693–701. doi: 10.1017/S1368980011002941
- Verma H, Garg R. Effect of magnesium supplementation on type 2 diabetes associated cardiovascular risk factors: a systematic review and meta-analysis. J Hum Nutr Diet. 2017;30(5):621–633. doi: 10.1111/jhn.12454
- Palacios C, Wigertz K, Braun M, et al. Magnesium retention from metabolic-balance studies in female adolescents: impact of race, dietary salt, and calcium. Am J Clin Nutr. 2013;97(5):1014–1019. doi: 10.3945/ajcn.112.039867
- Wang L, Sacks FM, Furtado JD, et al. Racial differences between African-American and white women in insulin resistance and visceral adiposity are associated with differences in apoCIII containing apoAI and apoB lipoproteins. Nutr Metab. 2014;11(1):56. doi: 10.1186/1743-7075-11-56
- Pillay S, Aldous C. Introducing a multifaceted approach to the management of diabetes mellitus in resource-limited settings. S Afr Med J. 2016;106(5):42–43.
- Klug E. South African dyslipidaemia guideline consensus statement. S Afr Med J. 2012;102(3 Pt 2):178–187. doi: 10.7196/SAMJ.5502
- Amod A, Motala A, Levitt N, et al. The 2012 SEMDSA guideline for the management of type 2 diabetes. J Endocrinol Metab Diab S Afr. 2012;17(1):S1–S94.
- Kao WH, Folsom AR, Nieto FJ, et al. Serum and dietary magnesium and the risk for type 2 diabetes mellitus: the atherosclerosis risk in communities study. Arch Intern Med. 1999;159(18):2151–2159. doi: 10.1001/archinte.159.18.2151
- Nanri A, Mizoue T, Noda M, et al. Magnesium intake and type II diabetes in Japanese men and women: the Japan public health center-based prospective study. Eur J Clin Nutr. 2010;64(10):1244–1247. doi: 10.1038/ejcn.2010.138
- Punyadeera C, van der Merwe MT, Crowther NJ, et al. Ethnic differences in lipid metabolism in two groups of obese South African women. J Lipid Res. 2001;42(5):760–767.
- Wajchenberg BL. Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocr Rev. 2000;21(6):697–738. doi: 10.1210/edrv.21.6.0415
- Einstein FH, Atzmon G, Yang XM, et al. Differential responses of visceral and subcutaneous fat depots to nutrients. Diab. 2005;54(3):672–678. doi: 10.2337/diabetes.54.3.672
- Rosanoff A, Seelig MS. Comparison of mechanism and functional effects of magnesium and statin pharmaceuticals. J Am Coll Nutr. 2004;23(5):501S–505S. doi: 10.1080/07315724.2004.10719389
- Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3–21. doi: 10.1111/j.1753-4887.2011.00456.x
- Misra A, Khurana L. Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab. 2008;93(11_supp_1):s9–s30. https://doi.org/10.1210/jc.2008-1595
