Abstract
Background: The risk of complications from type 2 diabetes mellitus (T2DM) is high. Achieving targets reduces the morbidity and mortality. This study aims to assess whether patients at the Helen Joseph Hospital's Diabetic Clinic are meeting the 2012 SEMDSA targets for diabetes.
Methods: A retrospective clinical audit was carried out. The files of 321 patients with T2DM were reviewed. Glycated haemoglobin (HbA1c), blood pressure, abdominal circumference and lipograms were assessed.
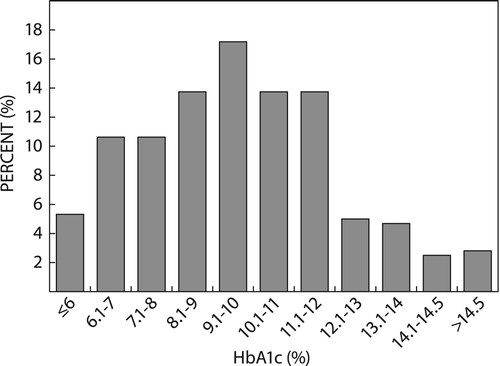
Results: The study population comprised majority black (n = 143; 44.6%) and coloured (n = 109; 34%) patients and was predominantly female (n = 200; 62.3%). The mean age was 59.4 years (SD 9.9 years). In total, 89.1% (n = 286) had hypertension, and 82.2% (n = 264) dyslipidaemia. The metabolic syndrome criteria were fulfilled by 266 (91.2%) patients. The majority did not exercise (n = 174; 56.3%). A small number smoked (n = 39; 12.5%) and used alcohol (n = 33; 10.6%). Mean HbA1c was 9.5% (SD 2.4; range 3.9–16.9%). Only 49 (15.3%) achieved the target HbA1c. Target blood pressure was achieved by 72 patients (25%). LDL target was achieved by 71 (22.6%) and abdominal circumference by 32 (11%) patients.
Conclusions: Despite adequate protocols and access to tertiary medical care, a very small percentage of patients are achieving proposed targets. The reasons for this are likely multi-fold and further analysis is required to assess these.
Introduction
The rapid rise in prevalence of diabetes mellitus (DM) in the last few decades has generated concern globally.Citation1,Citation2 The socio-economic concerns stemming from this disease and its complications are extensive, affecting all levels of society.Citation3,Citation4 Early recognition, diagnosis and implementation of treatment, continuous access to appropriate medications, treatment of concomitant medical problems and vigilant screening and recognition of complications is imperative in the management of DM. For this reason, Diabetic Societies worldwide have proposed guidelines to assist clinicians.Citation5,Citation6
The establishment of specialised diabetic clinics is an attempt to improve access to health care and a continuous supply of medication for all individuals.Citation5 At hospital level, diabetic clinics are referral centres for the complicated and often difficult to treat patients. Regular audits of these institutions allow management to assess systems and protocols and address areas of concern.Citation5
Audits of diabetic clinics, in South Africa and internationally, reveal that even with evidence-based guidelines only small numbers of patients are able to achieve set targets.Citation7,Citation8 In a 2009 audit of Charlotte Maxeke Academic Hospital, Helen Joseph Hospital and Chris Hani Baragwanth Hospital by Dr A. Klisiewicz assessing achievement of targets in diabetic patients, 30.7% of patients had a target glycated haemoglobin (HbA1c) of < 7%, 21.3% reached target SBP < 130 mmHg, 40.2% reached target DBP < 80 mmHg, 50.7% of patients achieved target LDL cholesterol of < 2mmol/l and 70.2% of patients were classified as overweight and obese with the majority having abdominal circumferences greater than the recommended values.Citation9
Pinchevsky et al. demonstrated a decline in percentage of patients achieving targets between the years 2009 and 2013 in their audit of the Charlotte Maxeke Johannesburg Academic Hospital diabetic clinic.Citation10 Target HbA1c of < 7% was achieved in 25.4% of the cohort in 2009 and 15.5% in 2013; BP target of < 140/90 mmHg in 35.9% in 2009 and 49.6% in 2013 and LDL cholesterol targets were achieved in 72.7% in 2013 as compared with 47.7% in 2009.Citation10
The South African cohort of the International Diabetes Management Practices Study also demonstrated very low target achievement rates in private South African hospitals, with patients on insulin therapy having higher mean HbA1c levels than those on oral hypoglycaemic agents.Citation11 International studies reveal only slightly better results with the greatest level of target achievement in resource-rich developed countries.Citation10,Citation12–15
This audit was designed to assess whether the patients at the Helen Joseph Diabetic Clinic are achieving the recommended targets set out by the Society for Endocrinology, Metabolism and Diabetes South Africa (SEMDSA) 2012 Guidelines for Diabetes Management. The results obtained in this study will be used to assess whether current treatment and education protocols are adequate and to identify areas where further research and interventions are required.
Aims
The primary aim of this study was to evaluate whether target HbA1c levels are achieved among patients attending the Diabetic Clinic. Secondary objectives were to determine whether targets for blood pressure, waist circumference and serum lipids were being achieved in these patients and, lastly, to determine the prevalence of obesity based on the WHO definition and the prevalence of the metabolic syndrome based on the harmonised definition of the metabolic syndrome.
Methods
Study design
A retrospective cross-sectional clinical audit of the Helen Joseph Academic Hospital Diabetic Clinic for the defined date range of the March 1, 2015–April 30, 2015 was conducted. Records of all patients attending the diabetic clinic were assessed. The records of all patients with type 2 diabetes mellitus (T2DM) for a period of greater than five years and who were on either insulin only therapy or insulin and metformin therapy were included in the study. The records of patients with type 1 diabetes (T1DM) and those patients with T2DM on only oral hypoglycaemic agents were excluded from the study. The reason for the exclusion of patients on oral hypoglycaemic agents alone was due to the fact that at Helen Joseph Hospital these patients are usually followed up at the hospital medical outpatients (MOPD) clinic and only referred to the Diabetic Clinic when insulin initiation is required. The records of 321 patients fulfilled the inclusion criteria and were entered into the data collection set.
Data collection
Demographics and other descriptive characteristics were obtained from institutional records. The list of medications prescribed at the last clinic visit was used. As per records, information on exercise, smoking and alcohol use are noted in a yes/no format without being quantified and was thus recorded as such.
Clinical parameters are measured by nursing staff on duty at every visit and inter-observer variability is possible. Height is measured using a standardised height metre. Weight using a standardised scale is measured with patients standing barefoot without support. Body mass index (BMI) is calculated from the patient’s weight and height using Quetelet's formula (weight (kg)/height (m) × height (m)). Abdominal circumference is measured using the International Diabetes Federation (IDF) measuring tape placed at 2 cm above the anterior superior iliac crest with the patient standing. Blood pressure (BP) is measured using the Mindray vs-800 calibrated automatic sphygmomanometer (Mindray, Shenzhen, PR China). An average of the last three measurements was used in order to compensate for the phenomenon of white coat hypertension.
As Helen Joseph Hospital is a public sector hospital, blood samples are processed by the National Health Laboratory Services (NHLS). The last recorded glycated haemoglobin (HbA1c) value and random serum lipograms were used for analysis.
Data were recorded on data sheets and then put into the Research Electronic Data Capture (REDCap: https://www.project-redcap.org/) web-based application. Once all data were recorded, a data report formed in REDCap was transferred to Microsoft Office Excel (Microsoft Corp, Redmond, WA, USA) for analysis.
Targets used in this study
The targets set out by 2012 SEMDSA guideline for the management of T2DM were used in this study.Citation5 Target HbA1c used for the purpose of this study was 7% or lower, which is the SEMDSA recommended guideline for the majority of patients.Citation5 The reason for this was that though the SEMDSA guidelines for target HbA1c differ according to age, prevalence of cardiovascular risk factors, hypoglycaemic unawareness and general overall prognosis, no clear outline of age range and prognosis is given.Citation5 Additionally, data collected during this study did not include patient factors that allow for a higher HbA1c, such as recurrent hypoglycaemic events, hypoglycaemic unawareness and the presence of target organ damage. The blood pressure target was set as < 140/90. Waist circumference target was taken to be < 80cm for females and ≤ 94cm for males. Targets for cholesterol are as follows: total cholesterol < 4.5mmol/l; triglycerides < 1.7mmol/l; HDL > 1.2mmol/l for women and > 1.0mmol/l for men; and an LDL cholesterol target of < 1.8mmol/l.
The WHO Classification for obesity and the harmonised criteria for the clinical diagnosis of the metabolic syndrome was used to classify the patients.Citation16
Statistical and data analysis
Data analysis was performed by a statistician and carried out using SAS version 9.4 for Windows (SAS Institute, Cary, NC USA). Descriptive analysis of the data was carried out as follows. Categorical variables were summarised by frequency and percentage tabulation, and illustrated by means of bar charts. Continuous variables were summarised by the mean, standard deviation, median and interquartile range, and their distribution illustrated by means of histograms. The prevalence of patients who met each of the treatment goals was estimated, together with 95% confidence intervals. The association between target achievement and insulin regimen was analysed by means of a chi-square test. The 5% significance level was used throughout.
Results
Demographics
The study population comprised 321 patients aged 30–88 years old, with a mean age of 59.4 years (SD 9.9). Complete demographic data can be seen in . The cohort compromised majority black (n = 143; 44.6%) and coloured (n = 109; 34%) patients. This sample was predominantly female (n = 200, 62.3%). The year of diagnosis ranged between 1973 and 2010. The majority of patients had a sedentary lifestyle: 174 patients (56.3%) did not exercise. In addition, a small number of patients in this study population smoked (n = 39; 12.5%) and used alcohol (n = 33; 10.6%).
Table 1: Demographic data
A large proportion of patients had concomitant hypertension (n = 286; 89.1%) and dyslipidaemia (n = 264; 82.2%). More than half of the patients were classified as obese according to the WHO classification. A staggering 91.2% (n = 266) fulfilled the criteria for diagnosis of the metabolic syndrome.
The following insulin regimens were used: NPH insulin only 11.2% (n = 36), pre-mix 30/70 insulin (30% short acting/70% NPH insulin) 73.2% (n = 235), basal-bolus (NPH and short-acting insulin) 4.6% (n = 47) and pre-mix 30/70 plus short-acting insulin combination 0.9% (n = 3). Analysis of the small number of patients in the pre-mix 30/70 plus short-acting insulin combination group would not have revealed any significant results, therefore this group was excluded from further analysis.
Metformin was used in 72.5% (n = 228) of patients. Of note, the majority of patients were being treated with statins, aspirin and angiotensin converting enzyme inhibitors. A complete list of medications used can be found in .
Table 2: Medications used
Achievement of targets
shows detailed analysis of each variable. and depict the percentage of patients achieving targets.
Figure 1: Percentage of patients who met targets. SBP = systolic blood pressure; DBP = diastolic blood pressure, HDL = high-density lipoprotein; LDL = low-density lipoprotein.
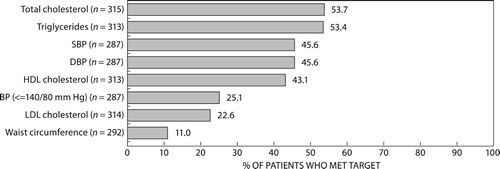
Table 3: Analysis of variables
Table 4: Patients who meet targets
Anthropometric measurements
The mean average systolic BP was 144 mmHg (SD 20; range 98–245 mmHg) and the mean average diastolic BP was 81 mmHg (SD 11; range 53–112 mmHg). Only 72 patients achieved the target BP of < 140/90mmHg (25.1%; 95% CI = 20.2–30.5). Mean waist circumference was found to be 109 cm for females (SD 16 cm; range 72–160 cm) and 106 cm for male (SD 15 cm; range 55–157 cm) and only 32 patients (11%; 95% CI 7.9–15.1) had a waist circumference measurement that did not meet criteria for central obesity.
Blood results
The mean HbA1c in this study population was 9.5% (SD 2.4; range 3.9–16.2%). Only 49 (15.3%; 95% CI 11.5–19.7) achieved the target HbA1c of 7% or less. depicts the range of HbA1c. There was no significant association between patients with HbA1c at target and insulin regimen used (p = 0.85). illustrates the relationship between insulin regimen and HbA1c. There was, however, a higher mean HbA1c level amongst patients on basal bolus than those using other regimens, even when controlling for co-morbidities.
Table 5: Relationship between insulin regimen and HbA1c
Analysis of lipograms revealed unequally distributed data with: median total cholesterol of 4.4 mmol/l (IQR 3.6–5.2), median triglyceride level of 1.6 mmol/l (IQR 1.1–2.2), median LDL cholesterol of 2.4 mmol/l (IQR 1.9–3.0) and median HDL cholesterol level of 1.0 mmol/l (IQR 0.9–1.2) for males and 1.1 mmol/l (IQR 0.9–1.4) for females. Only 71 patients (22.6%; 95% CI 18.1–27.6%) had LDL cholesterol levels below the target. 61.3% (n = 192) and 46.6% (n = 146) of patients had low HDL cholesterol and high triglyceride levels respectively.
Discussion
The consequences of untreated and uncontrolled T2DM can be dire. Treatment of T2DM requires not only glycaemic control but control of other concomitant cardiovascular risk factors. The 2012 SEMDSA guidelines for the treatment of T2DM have set out targets for treatment that are evidence based and provide the necessary cardiovascular risk protection.Citation5 This audit of the Helen Joseph Hospital Diabetic clinic revealed sub-optimal management of T2DM patients with very low rates of targets attained in all areas.
The Diabetic Clinic at Helen Joseph Hospital is a referral clinic for the MOPD, the Polyclinic (a primary health care clinic based at the hospital), as well as the regional and district level clinics. Due to its nature as being a tertiary referral centre, most patients referred are either poorly controlled or have significant co-morbidities or complications. Once patients have achieved and maintained a good level of control, they are often stepped down back to their respective referral clinics. These factors could possibly explain the higher level of HbA1c and other cardiovascular risk factors found in this cohort.
Our cohort of 321 patients consisted mainly of black and coloured patients consistent with the South African demographic, the drainage area of the hospital and the individuals that reported using public healthcare facilities in the last South African Household Survey.Citation17 Female predominance is consistent with findings from Hilawe et al. and cohorts noted in other studies.Citation7,Citation18 Similarly the mean age of 59.4 years is in keeping with other cohorts.Citation13–15
Rates of smoking in this study population were found to be lower than the reported South African national average.Citation19 Use of alcohol was also noted in only a small percentage of patients. Though these rates are low, considering the fact that both smoking and excessive alcohol use confer additional risk in terms of cardiovascular disease and other complications, it is imperative that patients who require assistance with cessation of these risk activities be identified and helped.
The low numbers of patients with HIV/AIDS in this cohort is surprising, considering the high prevalence of HIV/AIDS in South Africa.Citation20 This is most likely due to a combination of underreporting by patients and under-screening by clinicians. Another reason may be that these patients are not being referred to the Diabetic Clinic (due to limited capacity) and are being treated at either the MOPD clinic or the HIV clinic. The interactions between HIV/AIDS and NCDs as well as their treatments have been well documented.Citation21–24 It is thus evident that further measures need to be taken within this diabetic clinic to ensure adequate screening and treatment for HIV/AIDS.
The high prevalence of obesity, hypertension and dyslipidaemia is reflective of the global rise in the metabolic syndrome.Citation16 Considering the higher risk of cardiovascular disease and other complications in patients diagnosed with the metabolic syndrome, this is disquieting. Even more perturbing is the very low rates of achievement of HbA1c, BP and lipid targets set by the SEMDSA diabetes guidelines.Citation25 Target attainment in this cohort includes HbA1c < 7% in 15.3%, BP < 140/90 in 25.1%, LDL-C < 1.8mmol/l in 53.4% and recommended waist circumference in 11%.
On comparison with other studies, both national and international, the Helen Joseph Diabetes Clinic is achieving much lower rates of attaining targets than other clinics. In a 2009 audit of Johannesburg teaching hospitals, Klisiewicz and Rahl found higher rates for attainment of HbA1c (30.7%) and BP (systolic BP 21.3%, diastolic BP 40.2%) targets, with a similar percentage of patients achieving LDL-C targets. Lower BP targets of < 130/80 and a higher LDL-C target of < 2.5mmol/l were used.Citation9
The 2013 Pinchevsky et al. audit of the Charlotte Maxeke Academic Hospital Diabetic Clinic revealed a similar percentage of patients attaining HbA1c targets (15.5%) to that in this study. However, a much higher percentage of patients attained BP target of < 140/90 (49.6%) and LDL-C of < 2.5mmol/l (72.7%).Citation10 Amod et al. demonstrated a 30% target HbA1c attainment in South African private hospitals and international diabetic clinics’ attainment of target HbA1c ranges between 30% and 60% as demonstrated in the meta-analysis by Pinchevsky et al. in 2015.Citation7,Citation11 The attainment of BP and LDL-C targets also show wide variability depending on countries’ income level and access to resources. Most studies omit waist circumference and BMI/obesity targets, which makes comparison with this population difficult.
Importantly, we must note the heterogeneity of the study populations. Whilst this study focused on insulin-dependent T2DM patients, others comprise either a mix of patients with both T1DM and T2DM or all patients with T2DM, regardless of treatment regimen. Additionally, the majority of studies looking at similar outcomes have been carried out in primary health care settings as opposed to specialised diabetic clinics like the one at Helen Joseph Hospital. Still, the trend in many of these studies is lower levels of target achievement in individuals with T2DM who are on insulin-based therapy, as opposed to those receiving oral hypoglycaemic agents.Citation7
Numerous other factors for poor attainments of targets have been noted in other studies.Citation26 These reasons encompass patient, caregiver and system factors that influence outcomes. The most pertinent factors include education of diabetic clinic staff and patients; weight management focusing on nutrition and exercise; access to adequate, healthy food and appropriate medications; the ability to self-monitor glucose; and psychosocial factors relating to the patient's perceived burden of illness, fears of complications and treatment and depression. Further analysis is imperative in order to assess which of these barriers is prevalent in the Helen Joseph Hospital Diabetic Clinic, in order for appropriate intervention programmes to be designed.
This study has a number of limitations. The study cohort comprised only insulin-dependent T2DM patients at a referral centre for difficult to control patients and thus the very low levels of target attainment are not reflective of the general diabetic population. The cross-sectional design of the study does not allow assessment of whether patients referred to this clinic improve over time. A prospective study of these patients would provide more information in this regard and thus offer a better assessment of the current protocols. With the exception of HbA1c, the relationship of target achievement to the type and dose of medication was not assessed. Additionally, factors affecting HbA1c levels were not identified and individualised HbA1c targets were not applied to the patients in the cohort. Lastly, factors that affect the attainment of appropriate targets were not evaluated.
Conclusion
With current hospital protocols and access to tertiary medical care, only a very small percentage of patients at the diabetic clinic are achieving proposed targets. Other audits have revealed a range of reasons for poor control in their patients. More comprehensive analysis is required to assess the reasons in this clinic if we are to address the problem with the urgency it requires. Ultimately, the goal is to offer the best possible treatment to our ever-increasing diabetic population.
Ethics committee approval
The University of Witwatersrand Ethics Committee and the Helen Joseph Hospital Ethics Committee approved the study (Clearance certificate no: M151193).
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- World Health Organization. WHO: Global Action Plan for the prevention and control of non-communicable diseases 2013–2020. Geneva: World Health organisation; 2013.
- International Diabetes Federation. IDF Diabetes Atlas. 7th ed. Brussels: IDF; 2015.
- Bloom DE, Cafiero ET, Jane’-Llopis E, et al. The global economic burden of Noncommunicable Diseases. Geneva: World Economic Forum; 2011.
- Seuring T, Archangelidi O, Suhrcke M. The economic costs of Type 2 Diabetes: a global systematic review. Pharmacoeconomics. 2015;33(8):811–31. doi: 10.1007/s40273-015-0268-9
- Guideline Committee. The 2012 SEMDSA guideline for the management of Type 2 Diabetes (revised). JEMDSA. 2012;17(2 (supplement 1)):S1–95.
- American Diabetes Association. Standards of medical care in diabetes - 2017. Diabetes Care. 2017;40(Supplement 1):S1–2.
- Pinchevsky Y, Butkow N, Chirwa T, et al. Glycaemic, blood pressure and cholesterol control in 25 629 diabetics. Cardiovasc J Afr. 2015;26(4):188–92. doi: 10.5830/CVJA-2015-050
- Braga MFB, Casanova A, Teoh H, et al. Poor achievement of guidelines-recommended targets in type 2 diabetes: findings from a contemporary prospective cohort study. Int J Clin Pract. 2012;66(5):457–64. doi: 10.1111/j.1742-1241.2012.02894.x
- Klisiewicz AM, Raal FJ. Sub-optimal management of Type 2 Diabetes mellitus - a local audit. J Endocrinol Metab Diabetes South Afr. 2009;14(1):13–6. doi: 10.1080/22201009.2009.10872186
- Pinchevsky Y, Shukla V, Butlow N, et al. The achievement of glycaemic, blood pressure and LDL cholesterol targets in patients with type 2 diabetes attending a South African tertiary hospital outpatient clinic. JEMDSA. 2015;20(2):81–6.
- Amod A, Riback W, Schoeman HS. Diabetes guidelines and clinical practice: is there a gap? The South African cohort of the International Diabetes Management Practices Study. JEMDSA. 2012;17(2):85–90.
- Stone MA, Charpentier G, Doggen K, et al. Quality of care of people with type 2 diabetes in eight European countries: findings from the guideline adherence to enhance care (GUIDANCE) study. Diabetes Care. 2013;36(9):2628–38. doi: 10.2337/dc12-1759
- Tanamas SK, Magliano DJ, Lynch B, et al. Ausdiab 2012. The Australian diabetes, obesity and lifestyle study. Melbourne: Baker IDI Heart and Diabetes Institute; 2013.
- Al-Rowais NA. Glycemic control in diabetic patients in King Khalid University Hospital (KKUH) – Riyadh – Saudi Arabia. Saudi Pharm J. 2014;22(3):203–6. doi: 10.1016/j.jsps.2013.06.008
- de Brito Gomes M, Gianella D, Faria M, et al. Prevalence of Type 2 Diabetic patients within the targets of care guidelines in daily clinical practice: a multi-center study in Brazil. Rev Diabet Stud. 2006;3(2):82–7. doi: 10.1900/RDS.2006.3.82
- Alberti KGMM, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome. Circ. 2009;120(16):1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644
- Stats SA Library Cataloguing -in-Publication Data. Use of health facilities and levels of selected health conditions in South Africa: Findings from the General Household Survey; 2011 [Internet]. Statistics South Africa; 2013. Available from: www.statssa.gov.za
- Hilawe EH, Yatsuya H, Kawaguchi L, et al. Differences by sex in the prevalence of diabetes mellitus, impaired fasting glycaemia and impaired glucose tolerance in sub-Saharan Africa: a systematic review and meta-analysis. Bull World Health Organ. 2013;91:671–82. doi: 10.2471/BLT.12.113415
- Reddy P, Zuma K, Shisana O, et al. Prevalence of tobacco use among adults in South Africa: results from the first South African national health and nutrition examination survey. South Afr Med J. 2015;105(8):648–55. doi: 10.7196/SAMJnew.7932
- StatsInBrief [Internet]. 2016. Available from: http://www.statssa.gov.za/publications/StatsInBrief/StatsInBrief2016.pdf
- Quin J. Diabetes and HIV. Clin Med. 2014;14(6):667–9. doi: 10.7861/clinmedicine.14-6-667
- Brown TT, Tassiopoulos K, Bosch RJ, et al. Association between systemic inflammation and incident diabetes in HIV-Infected patients after initiation of antiretroviral therapy. Diabetes Care. 2010;33(10):2244–9. doi: 10.2337/dc10-0633
- Wit SD, Sabin CA, Weber R, et al. Incidence and risk factors for New-Onset Diabetes in HIV-infected patients: the data collection on adverse events of Anti-HIV drugs (D:A:D) study. Diabetes Care. 2008;31(6):1224–9. doi: 10.2337/dc07-2013
- Young F, Critchley JA, Johnstone LK, et al. A review of co-morbidity between infectious and chronic disease in Sub Saharan Africa: TB and Diabetes Mellitus, HIV and metabolic syndrome, and the impact of globalization. Glob Health. 2009 Sep 14;5:9. doi: 10.1186/1744-8603-5-9
- SEMDSA Type 2 Diabetes Guidelines Expert Committee. SEMDSA 2017 guidelines for the management of Type 2 diabetes mellitus. JEMDSA. 2017;22(1 (Supplement 1)):S1–196.
- Skovlund SE, Peyrot M. The diabetes attitudes, wishes, and needs (DAWN) program: a new approach to improving outcomes of diabetes care. Diabetes Spectr. 2005;18(3):136–42. doi: 10.2337/diaspect.18.3.136