ABSTRACT
Exposure therapy is effective but widely underused. Numerous studies indicate therapist factors that might explain this pattern of underuse. This systematic review and meta-analysis synthesised those previous research findings, to identify which therapist factors are clearly associated with their intent to use exposure therapy. A systematic review and six random-effects meta-analyses synthesised studies identified in three databases (Scopus, PsychINFO, Web of Science) and through reference lists and citation searches. Most studies relied on a survey design, resulting in weak quality of research. Twenty-six eligible studies were included in the narrative synthesis, (including 5557 participants), while 21 studies yielded sufficient data to enter the meta-analysis. Medium to large pooled effect sizes indicated that therapists with more positive beliefs, a CBT orientation, and training in exposure therapy were significantly more likely to use exposure. Small pooled effect sizes indicated that older and more anxious therapists were less likely to use exposure. Therapist years of experience was not significantly associated with exposure use. There was no evidence of publication bias. Therapist characteristics clearly play a role in the use of exposure therapy, and future clinical and research work is required to address this limitation in the delivery of this effective therapy.
Exposure with response prevention (exposure therapy) is a well-established and highly effective approach to treatment of anxiety symptoms across a broad range of disorders and across the lifespan. It is recommended for use with anxiety disorders (e.g. panic disorder – Bouchard et al., Citation1996; phobias – Odgers et al., Citation2022 social anxiety – Kampmann et al., Citation2016), and for disorders where the core pathology is anxiety-based (e.g. obsessive-compulsive disorder – Ojalehto et al., Citation2020; post-traumatic stress disorder – McLean et al., Citation2022 eating disorders – Butler & Heimberg, Citation2020). It is also effective in addressing the anxiety features that arise from and that maintain a range of medical conditions (e.g. atrial fibrillation – Oser et al., Citation2021; pain– Körfer et al., Citation2020; chronic pain – Hedman-Lagerlöf et al., Citation2018 irritable bowel syndrome – Ljótsson et al., Citation2011). In most of these cases, it is a key element of cognitive-behavior therapy, though there is evidence for several disorders that the exposure element on its own can be as effective as when the broader cognitive elements are added (e.g. Ougrin, Citation2011). To summarise, exposure therapy has been found to be effective for numerous anxiety-based disorders, and has a relatively robust effect across populations (Carpenter et al., Citation2018).
However, despite the effectiveness of exposure therapy, it is underused by very many clinicians (Becker et al., Citation2004; Gunter & Whittal, Citation2010; Hipol & Deacon, Citation2013; Rosen et al., Citation2004). Furthermore, when exposure therapy is used, it is often adapted in line with the therapists’ clinical judgement, which can reduce treatment efficacy (Stobie et al., Citation2007). Many clinicians report finding exposure stressful to implement (Schumacher et al., Citation2015), and often opt for techniques such as progressive muscle relaxation or deep breathing over the use of exposure therapy (Deacon, Lickel, et al., Citation2013), despite the evidence that exposure is superior to these.
The phenomenon of clinicians choosing not to use evidence-based therapy (such as exposure) or deviating significantly from best practice protocols has been referred to as “therapist drift” (Waller, Citation2009). The reduced effectiveness of evidence-based therapy in practice in comparison to its efficacy in randomised control trials is often attributed to such therapist drift (Waller & Turner, Citation2016). Therapist factors such as anxiety, age and theoretical orientation have all been associated with a propensity to drift from empirically-supported treatments (Speers et al., Citation2022). However, it is also important to recognise that the therapist might not have sufficient knowledge of methods such as exposure to utilise them effectively. Whilst there are numerous examples of therapist drift leading to ineffective implementation of exposure therapy (Brosan et al., Citation2006), in many cases exposure is not used at all (Whiteside et al., Citation2016). Research has repeatedly shown that a significant proportion of clinicians do not use exposure therapy to treat anxiety-based disorders, even if the clinician is reportedly orientated towards the use of CBT (Becker et al., Citation2004). Freiheit et al. (Citation2004) found that even though 71% of their sample listed CBT as their theoretical orientation, only 12–38% of them used exposure to treat anxiety disorders.
There are numerous suggestions as to why clinicians might be less likely to use exposure therapy, despite the evidence base (Waller & Turner, Citation2016). These include: organisational issues (e.g. too few sessions provided to follow manualised treatment - Royal College of Psychiatrists, Citation2013); negative views towards manualised treatments (E. Addis & Krasnow, Citation2000); fear of negative outcomes when using exposure therapy (Deacon, Lickel, et al., Citation2013); and overvaluation of the therapeutic relationship as a method of change (Brown et al., Citation2013). While knowledge of protocols is a necessary element in therapy delivery, it is not sufficient in itself. Evidence-based therapies are still underutilised in clinician populations where awareness and knowledge of appropriate therapies is high (Simmons et al., Citation2008).
This pattern of differences in therapy delivery means that it is important to identify factors associated with a therapist’s intent to use exposure therapy. Such identification would allow the targeting of further training or supervision. Given the growing body of research into the relationship between therapist factors and their intent to use exposure therapy (e.g. Deacon, Farrell, et al., Citation2013), it is timely to undertake a systematic review to synthesise these findings, to identify any gaps in the literature, to direct future research, and to identify implications for clinical practice. Therefore, the current review aims to identify therapist variables that are associated with therapists’ intent to use exposure therapy, using both a systematic review and a meta-analytic approach to synthesise the existing research.
Method
The protocol for this review was pre-registered on Open Science Framework (https://osf.io/pwg3d/?view_only=1255a474841540e9a1855e2517bf4a13). The original registered plan was to undertake a narrative synthesis alone. However, this was adjusted to add a meta-analytic element, given the number of papers that were identified.
Inclusion and exclusion criteria
Studies were included if they investigated the use of exposure therapy in a mental health setting. Studies had to include as part of their analysis: at least one measure of therapist characteristics; an index of intent to use exposure therapy; and consideration of the relationship between these characteristics and exposure use. Studies investigating the use of exposure therapy in any population were included if they were quantitative and written in English. Grey literature, systematic reviews or meta-analyses, single case studies and studies not written in English were excluded. Studies investigating interventions to increase the use of exposure therapy were excluded due to a pre-existing meta-analysis (Trivasse et al., Citation2020).
Search strategy
A title, abstract and keyword search was conducted on the databases Scopus, PsychINFO and Web of Science on 13th September 2021, and updated on 8th August 2022. PsychINFO is considered the most comprehensive database in Psychology (Arnold et al., Citation2006), and Web of Science and Scopus both claim to be two of the largest databases covering multidisciplinary scientific literatures (Chadegani et al., Citation2013). Thus, it was deemed suitable to search these three databases for this review. As the Cochrane Library includes reviews only, it was decided not to search this database. Whilst Google Scholar has been found to return a large proportion of relevant articles compared to all other databases (Harari et al., Citation2020), it has some key limitations, which influenced the decision not to search it. Harari et al. (Citation2020) concluded that searching in Google Scholar is not reproducible due to its lack of a transparent ranking algorithm. It also has a search character limit, and it is not possible to limit the bibliographic fields being searched (Harari et al., Citation2020).
Keywords were “therapist”, “exposure therapy”, and “characteristics”. The following combination was used: (Therapist* OR “CBT therapist*” OR “cognitive behavio*ral therapist*” OR psychologist* OR “clinical psychologist*” OR clinician* OR psychotherapist*) W/3 (anxiet* OR characteristic* OR factor* OR belief* AND “exposure therap*”). The full syntax for the search strategy is presented in Appendix A.
Following the search, duplicates were removed, and then title and abstracts were screened by the lead author. A second author (JB) independently screened 10% of the papers (randomly selected) to check agreement on the studies to be included in the review. These authors agreed fully on the papers to be included. Papers were excluded if they did not mention exposure therapy and therapist characteristics. No previous reviews were found with the same aims and methodology as the current review. If the title and abstract seemed relevant or it was unclear, the whole article was read to assess if it met the inclusion criteria. The references of papers that met the inclusion criteria were manually searched for other relevant articles. A citation search was conducted using Web of Science to assess whether papers that had cited the included papers also met the inclusion criteria.
Quality assessment
The Effective Public Health Practice Project (EPHPP, Citation2020) was utilised to assess the quality of studies that were included in the review. The EPHPP has been shown to have high levels of construct validity in relation to other highly-rated measures and has strong interrater reliability (Thomas et al., Citation2004).
The EPHPP rates quality indicators such as selection bias, study design, confounding variables, data collection methods, and withdrawal and dropout rate. The “blinding” component was removed for the current review as none of the studies were randomised control trials. Items are scored 1 = strong, 2 = moderate, and 3 = weak. A quality rating dictionary is supplied to assist the rating of every area of assessment (EPHPP, Citation2017). Specific criteria are provided for each area that should be met if the study is to be rated “strong”. A study was given an overall score of “strong” if none of the six items were rated as weak, “moderate” if one item was rated weak, and “weak” if two or more items were rated as weak.
Twenty-five percent of the papers included in the review were selected using a random number generator and quality assessed by an independent reviewer, and discrepancies were resolved through discussion between the reviewers. This criterion of reviewing 25% of full papers was chosen because it has been used in a number of systematic reviews and meta-analyses across various fields of research (e.g. Gosling et al., Citation2021; Merry et al., Citation2013; Nicholson et al., Citation2020; Ruffell et al., Citation2019; Veal et al., Citation2021). Cohen’s kappa was calculated to assess interrater reliability. There was a strong rate of agreement between the reviewers (K = 1, p = .014).
Data analysis
Six random effect meta-analyses were conducted using the statistical package Meta-Analysis via Shiny (Hamilton et al., Citation2017). Studies with sufficient statistical information to either convert to or calculate standardized effect sizes were included. In instances where studies only reported the standardised regression coefficients (β) and not correlation coefficients, authors of the papers (N = 3) were contacted. Two authors responded but no longer had access to the datasets, and the other did not respond. Thus, Pearson’s r was imputed using r = 98β + .05λ, where λ is an indicator variable that equals 1 when β is non-negative and 0 when β is negative (Peterson & Brown, Citation2005). The author of one study that did not include the data required to compute standardized effect sizes was contacted but did not respond, and thus the paper could not be included in the meta-analyses.
Fisher’s Z transformed r was calculated for correlational associations where continuous measures of therapist factors were used (beliefs, age, years of experience, anxiety), either by directly extracting Pearson’s r, or by converting to r from β, or by using Spearman’s rho as an approximation of r. Hedges g was calculated for dichotomous therapist factors (therapeutic orientation, training) to adjust for unequal sample sizes across groups. Heterogeneity was assessed using Cochran’s Q and I2 statistics (Higgins et al., Citation2003). Publication bias was assessed using a weight-function model (Vevea & Hedges, Citation1995), and calculation of the fail-safe N (Rosenthal, Citation1991). Sources of heterogeneity in the studies include the measures used to assess the frequency of exposure use, and the anxiety disorder(s) treated using exposure (e.g. anxiety, PTSD, phobia).
Results
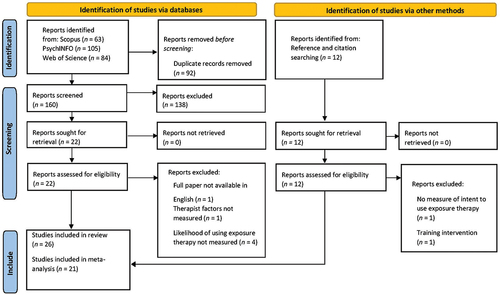
The search is summarised in a PRISMA flow diagram in . It yielded 252 papers. Following the removal of duplicates, there were 160 studies. After title and abstract screening, 16 papers met the inclusion criteria. A citation and reference search of these 16 papers yielded a further 10 papers that met inclusion criteria, resulting in a total of 26 papers that could be included in the narrative synthesis, as listed in . Of these, 21 yielded adequate data to allow effect sizes to be calculated (after some authors were approached for additional information for this purpose). Those 21 studies were included in the meta-analysis.
Table 1. Authors, key variables, and findings of included papers.
Characteristics of papers included
There were a total of 5557 participants. Of the 21 studies that reported gender demographics, a mean of 73% of participants were female. The most common therapist factors measured were beliefs about exposure (using the Therapist Beliefs about Exposure Therapy Scale [TBES]; Deacon, Farrell, et al., Citation2013), anxiety, therapeutic orientation, and demographics (age, gender, and years of experience).
Given that it is widely used, it is important to understand the TBES. The TBES measures therapists’ negative beliefs about the safety, tolerability, and ethicality of exposure therapy (Deacon, Farrell, et al., Citation2013). Twenty-one negative statements about exposure therapy are presented on a 5-point Likert scale rated from 0 = strongly disagree to 4 = strongly agree. The total score range is from 0 to 84, with higher scores indicating stronger negative beliefs about exposure therapy. The TBES has demonstrated excellent internal consistency (α = .90–.96; Deacon, Farrell, et al., Citation2013; N. Farrell et al., Citation2013; Meyer et al., Citation2014), test-retest reliability (r = .89; Deacon, Farrell, et al., Citation2013), and criterion validity (Deacon, Farrell, et al., Citation2013).
As the TBES is a continuous measure, Pearson’s correlations between beliefs and exposure use were commonly reported across the studies where the measure of intent/use of exposure therapy was also continuous (e.g. continuous measure of likelihood of using exposure therapy, number of sessions spent on exposure interventions). Studies not reporting Pearson’s r instead reported β, Odds Ratios, Cohen’s d, Tau Beta, or Spearman’s rho. Similarly, anxiety was assessed dimensionally, using five different continuous measures across the seven studies, whereby higher scores indicate greater levels of anxiety. The majority of studies therefore reported Pearson’s correlations between anxiety and exposure use, followed by β and Spearman’s rho.
Intent to use exposure therapy was measured either in response to a clinical vignette or by self-report from the therapists’ own practice. It should be noted that the majority of studies focused on the use of exposure in children with anxiety or in adults with PTSD, meaning that the generalizability of these findings to other clinical populations is limited. The key findings and quality assessments of papers (see Appendix B for full ratings) are presented in and explained below.
Quality of papers
All but one of the 26 papers received a global quality rating of “weak”, and the other received a rating of “moderate” (Scherr et al., Citation2015). All studies were retained to give an accurate view of the field and to identify areas for future research. The completed quality assessments can be found in Appendix B. Twenty-three studies used an exclusively survey-based design, while three studies used an experimental design with correlational elements (Hundt et al., Citation2016; Scherr et al., Citation2015; van Minnen et al., Citation2010).
Synthesis of findings
Independent of clinician characteristics, it was commonly noted that exposure therapy is widely underused (Becker et al., Citation2004; De Jong et al., Citation2020; Kline et al., Citation2021; Reid et al., Citation2018). For example, Whiteside et al. (Citation2016) found that although 81% of participants endorsed a CBT orientation, only 25.7% of therapists said they often used exposure, and only 5.8% said they always used it to treat childhood anxiety disorders. The findings of the review will be synthesised using the most commonly identified therapist factors mentioned above—beliefs about exposure, anxiety, therapeutic orientation, and demographics.
Beliefs about exposure therapy
Negative beliefs about exposure therapy were associated with reduced use in all 14 studies that used the TBES (De Jong et al., Citation2020; Deacon, Farrell, et al., Citation2013; Kannis-Dymand et al., Citation2022; Keleher et al., Citation2020; Kline et al., Citation2021; Meyer et al., Citation2014, Citation2020; Pittig et al., Citation2019; Reid et al., Citation2018; Rowe & Kangas, Citation2020; Sars & van Minnen, Citation2015; Schumacher et al., Citation2018, Citation2019; Whiteside et al., Citation2016). The majority of studies found a medium to large effect size, though two studies yielded a small effect size (Pittig et al., Citation2019; Schumacher et al., Citation2019).
Therapeutic orientation
Seven studies reported on therapeutic orientation in relation to exposure use. Five found that those with a CBT orientation were more likely to use exposure therapy (De Jong et al., Citation2020; Jelinek et al., Citation2022; Keleher et al., Citation2020; Kline et al., Citation2021; Whiteside et al., Citation2016), with medium to large effect sizes. Another study found that this effect did not remain significant when other therapist factors were included in a regression model (Hundt et al., Citation2016). The final study found no relationship between therapeutic orientation and exposure use (Moses et al., Citation2021).
Therapist age
Eight studies examined the relationship between age and use of exposure therapy (De Jong et al., Citation2020; Hundt et al., Citation2016; Jelinek et al., Citation2022; Kannis-Dymand et al., Citation2022; Kline et al., Citation2021; Meyer et al., Citation2020; Scherr et al., Citation2015; Schumacher et al., Citation2019). Most found that older therapists were less likely to use exposure therapy, though two found no such association (Hundt et al., Citation2016; Kline et al., Citation2021). Effect sizes ranged between low and medium.
Therapist years of experience
Seven studies examined the relationship between years of experience and use of exposure, none of which found a significant relationship (Becker-Haimes et al., Citation2017; Hundt et al., Citation2016; Jelinek et al., Citation2022; Keleher et al., Citation2020; Kline et al., Citation2021; Moses et al., Citation2021; Whiteside et al., Citation2016).
Therapist anxiety
Seven studies measured the relationship between therapist anxiety and use of exposure. Two studies found no relationship (De Jong et al., Citation2020; Reid et al., Citation2018), but five found that therapists with higher anxiety were less likely to use exposure therapy (Levita et al., Citation2016; Meyer et al., Citation2014; Pittig et al., Citation2019; Scherr et al., Citation2015; Z. Parker & Waller, Citation2019), with small to medium effect sizes.
Professional background and education
Eleven studies investigated the relationship between professional background or education and use of exposure. Studies did not state how they operationalised “professional background”. “Professional background” was stated as a variable in each of the studies investigating its relationship with exposure, and studies typically listed the professions (e.g. clinical psychologist, psychiatrist, support worker, marriage and family therapist). There was some indication that exposure therapy might be more likely to be used by clinical psychologists than other professions (Keleher et al., Citation2020; Meyer et al., Citation2014; Moritz et al., Citation2019). Seven studies found a positive relationship between years of education and use of exposure (De Jong et al., Citation2020; Keleher et al., Citation2020; Kline et al., Citation2021; Meyer et al., Citation2014; Moritz et al., Citation2019; Sars & van Minnen, Citation2015; Whiteside et al., Citation2016), with moderate effect sizes. Four studies found no relationship between education and use of exposure therapy (Reid et al., Citation2018; Rowe & Kangas, Citation2020; Schumacher et al., Citation2019; Stewart et al., Citation2016).
Training in exposure therapy
All six studies that investigated the relationship between specific training in exposure and the use of exposure therapy found a positive relationship, with small to large effect sizes (Becker et al., Citation2004; Hundt et al., Citation2016; Kannis-Dymand et al., Citation2022; Kline et al., Citation2021; Moses et al., Citation2021; Reid et al., Citation2018).
Meta-analyses
Six random-effects meta-analyses were conducted using effect sizes from 21 studies to examine the associations between therapist factors and intent to use exposure therapy. It was not possible to conduct meta-analyses for therapist professional background or education, due to the different methodologies and comparisons used.
The results of the meta-analyses are shown in , and illustrated in . Cochran’s Q test revealed significant heterogeneity among the samples in each meta-analysis, with I2 statistics ranging from 58.7% to 89.5%, indicating a moderate to large degree of heterogeneity in the samples. The weight‐function model likelihood ratio test did not indicate evidence of significant publication bias across any of the meta-analyses. Therapists with more positive beliefs about exposure therapy were significantly more likely to use it. Those with a CBT orientation or training in exposure therapy were significantly more likely to use exposure, or to have more positive beliefs about it. Older and more anxious therapists were less likely to use exposure therapy, or had less positive beliefs about it. In each case, a large number of non-significant findings would have been needed to negate the conclusion. In contrast, therapist years of experience did not show a significant association with use of exposure (p = .334). These results support the conclusions of the narrative synthesis, making them more robust.
Table 2. Random-effects meta-analyses: Therapist factors associated with the use of, or beliefs about the use of, exposure therapy for anxiety disorders.
Discussion
Exposure therapy is one of our most effective psychological therapies, but is used far less than the evidence base would suggest should be the case (Whiteside et al., Citation2016). This review has considered the range of therapists’ characteristics that contribute to their intent to use exposure therapy. Overall, the quality of the studies was weak, mostly because of a reliance on survey methodology and a lack of randomised controlled trials.
The most widely reported finding was that therapists with negative beliefs about exposure therapy were less likely to use it. This finding was consistent across a range of professionals in several countries. The studies focused mostly on adults with PTSD and children with anxiety, which could limit the generalizability of the findings to other populations. The TBES has demonstrated good reliability and validity (Deacon, Farrell, et al., Citation2013), is widely used, and has been translated into several languages. Therefore, despite the limitations associated with self-report (e.g. social desirability bias), it seems likely that the association between negative beliefs about exposure therapy and the reduced use of exposure therapy is reliable and valid.
As might be expected, therapists with a CBT therapeutic orientation were more likely to use exposure therapy than those who favoured other modalities. As most studies did not blind participants to the aims of their research and relied on self-selected samples, it is likely that therapists with a CBT orientation and familiarity with exposure were overrepresented in the sample. Furthermore, some studies only included participants who identified as trauma or anxiety experts or excluded participants from the sample if they did not use exposure (van Minnen et al., Citation2010). Therefore, there might not be sufficient representation from other orientations to make the findings generalizable.
While it is highly likely that there is a significant positive correlation between age and experience as a therapist, only age was associated (negatively) with intent to use exposure therapy. Hence, it can be concluded that older therapists are less likely to use exposure therapy, independent of their years of experience as a therapist. This conclusion has also been reached elsewhere (De Jong et al., Citation2020). Various potential explanations for this link have been advanced in the literature. For example, older therapists might have received more training in other theoretical orientations earlier on in their career before learning CBT (De Jong et al., Citation2020; Scherr et al., Citation2015). Alternatively, perhaps older therapists have more confidence than younger therapists, thus relying more heavily on their clinical judgement and/or on the interventions they learnt earlier on in their career, resulting in drift from CBT protocols (Scherr et al., Citation2015; Waller et al., Citation2012). However, it should be stressed that these are clinical hypotheses at present, and research is needed to understand why older therapists appear to be less likely to use exposure therapy.
Anxiety was negatively related to clinicians’ use of exposure. It was measured using a range of tools and constructs in the different studies, and hence it is not clear whether some facets of anxiety are better predictors of exposure usage than others. It is possible that the relationship between anxiety and exposure use might be mediated by another variable that was not routinely measured. For example, it is possible that with good supervision and a well-resourced organisation (e.g. lower caseloads, resulting in more time to do the work), more anxious therapists might still be willing to use exposure therapy.
Higher levels of training and education were also clearly associated with use of exposure therapy. However, this relationship is difficult to interpret, as the individual papers did not always specify what sort of training was given (e.g. was exposure-specific training needed to establish such a link? – Reid et al., Citation2018). It is not known how training might have its effect, as such mechanisms are not routinely measured. For example, does such education and training influence anxiety (e.g. by building confidence), beliefs about exposure, or simple levels of compliance with supervision?
It is possible that more years of education gives professionals increased opportunity to learn about exposure. Learning about exposure therapy might increase confidence and thus reduce anxiety about using it. Increased education might also provide the opportunity to develop more positive beliefs about exposure therapy. However, it is difficult to draw conclusions here, as this mechanism was not directly explored in the studies reported in this review. Furthermore, many studies did not separate the effects of training in exposure from years of education, making it impossible to disentangle the effects of the two.
Similarly, studies did not state how they operationalized “professional background”. Some studies reported professions such as clinical psychologists, nurses, and support workers (e.g. Keleher et al., Citation2020), whereas others reported the education levels associated with that profession, such as doctoral level psychologists or masters degree counsellors (e.g. Whiteside et al., Citation2016). This omission makes it difficult to know whether it was the clinicians’ profession (e.g. current job role) or the education level and training length associated with it that was related to use of exposure. Further research is necessary to explore the relationships between professional background, education, and use of exposure.
Strengths and limitations of the current review
The current review and meta-analysis had numerous strengths. There was a comprehensive and replicable search strategy, using three databases and forward and backwards citation searches. The quality rating showed strong interrater reliability. Data for the majority of papers permitted their inclusion in the meta-analysis.
The review also had a number of limitations. Western countries were over-represented. Including samples recruited from a wider range of countries would make the findings more generalizable. Whilst the databases searched (Scopus, PsychINFO, Web of Science) include key databases for Psychology-related research, searching only three databases potentially limits the identification of studies suitable for inclusion, and other databases (e.g. Pubmed) could be used in future reviews of this sort. Furthermore, while the grey literature was not included to ensure that the research that was included was of appropriate quality, that could mean that key data were not included. However, the meta-analyses revealed that the number of null findings needed to counter the conclusions would be high. The inclusion of only English language papers was also a potential limitation, as it might have resulted in fewer non-significant findings being included and fewer non-western clinical practices being represented.
Strengths and limitations of studies included
A strength of the studies included is that the majority used reliable and validated measures for therapist characteristics, such as the TBES (Deacon, Farrell, et al., Citation2013). However, there was variable measurement of clinician use of exposure, with some using vignettes (enhancing validity but limiting generalizability—e.g. van Minnen et al., Citation2010). Others addressed self-reported use of exposure therapy (e.g. Schumacher et al., Citation2019), where self-report can be inflated by social desirability bias and limited by poor recall and different clinician caseloads.
A further limitation of the studies included in the review was a reliance on cross-sectional survey designs, which allow for the recruitment of large samples, but lead to a lack of causal evidence. It is possible that only those who were confident in using exposure therapy responded to recruitment calls. Furthermore, it was not possible to identify response rates and withdrawal from most of the research.
Finally, the majority of research focused either on the use of exposure in children with anxiety, or in adults with PTSD. This pattern indicates a particular need for research into the intent to use exposure in a wider range of anxiety-based disorders, and across the patient age range. Furthermore, there was an imbalance in the number of males to females in the samples, with 73% of the total sample (where gender data were available) being female. There was no research focusing on the use of exposure with older adults or people with learning disabilities. Consequently, these findings are only generalizable to populations of young people and adults, rather than to other clinical populations. They indicate the need for research that is more representative of the wider population.
Implications for future research
A critical implication is that studies are needed that address causality more robustly and in a more clinically generalizable way. For example, the link between intent to use exposure therapy and actual clinical practice could be monitored in real-life clinical settings or using filmed sessions, where clinicians’ other characteristics are also monitored more carefully (e.g. the quality of training, and its impact on exposure use during and after the training). Furthermore, more representative samples of clinicians should be recruited, as the self-selection element of this study is likely to mean that the findings cannot be generalized.
It will also be important to determine whether service-level issues impact on the delivery of exposure therapy (or vice versa). An example is clinician caseload, where there is some evidence that indicates that higher caseload is associated with less use of exposure therapy (Becker-Haimes et al., Citation2017; Sars & van Minnen, Citation2015), though the causal direction would need to be monitored longitudinally. For example, while it is possible that having a high caseload results in clinicians not having the time to deliver exposure therapy, it is also possible that not delivering effective therapies such as exposure results in keeping patients much longer, and building up a larger caseload as a result.
It may also be important to consider how to support clinicians to put aside older practices that have since been found to be detrimental to exposure therapy, such as the parallel use of relaxation techniques. It could be assumed that learning new evidence-based techniques (e.g. inhibitory learning approaches to exposure—Craske et al., Citation2014) reduces the use of outdated methods, but this might not be the case, particularly if teachers or supervisors are using out of date methods. Effective ways of supporting clinicians to transition to newer evidence-based practice could warrant future research (Niven et al., Citation2015).
Another area that clearly merits further research attention is whether additional training and supervision could result in clinicians whose anxiety and negative beliefs about delivering exposure therapy are less prominent (e.g. N. Farrell et al., Citation2013). However, Trivasse et al. (Citation2020) have pointed out the importance of determining whether such attitudinal and emotional changes are translated into behavioural change on the part of clinicians.
Implications for clinical practice
Both clinicians and patients report that CBT is offered sub-optimally, including limited use of exposure therapy (e.g. Cowdrey & Waller, Citation2015; Mulkens et al., Citation2018). The key clinical implications of this research centre on whether changes in clinicians’ practice can be brought about. Selection of clinicians based on their characteristics (anxiety-proneness, beliefs about exposure, age, etc.) is unlikely to be viable or helpful. It is also clear that training alone has limited impact on clinicians’ implementation of exposure therapy (Trivasse et al., Citation2020). However, it is possible that those characteristics could be used to guide post-qualification training and supervision (e.g. supervisors assisting more anxious clinicians to undertake exposure activities with their patients, to overcome their own anxiety). Trivasse et al. (Citation2020) suggested supporting clinicians to develop implementation intentions, as this has been found to improve goal attainment even if the necessary action is anxiety-provoking. For example, clinicians could make an “if-then” plan to implement exposure strategies that they have learned.
A further possibility is that services that are commissioned to provide evidence-based therapies such as exposure therapy could be required to monitor whether it is delivered and whether it achieves the expected effectiveness. If the therapy is not delivered or does not achieve the expected outcomes, this could be because clinicians commonly overestimate their personal effectiveness (Walfish et al., Citation2012), and therefore might feel less compelled to use evidence-based therapy, particularly if they find the intervention challenging. Therefore, a focus on feeding back on outcomes might enable services to ensure that their clinicians take a more effective approach to treatment, using exposure therapy more often and with greater fidelity.
Service users might also be encouraged to raise their concerns if they are not being offered appropriate treatment. Providing resources to services to ensure that clinicians feel skilled and confident to use exposure therapy could be matched with encouraging patients to ask for exposure therapy where it would be appropriate. Such an approach could improve the quality of care offered while reducing clinician burden, since exposure therapy can be a short and effective intervention when delivered appropriately (Kaczkurkin & Foa, Citation2015).
Conclusion
In summary, exposure therapy is effective but is seriously under-used (Becker et al., Citation2004; Gunter & Whittal, Citation2010; Hipol & Deacon, Citation2013; Rosen et al., Citation2004). This review and meta-analysis has shown that therapist factors that influence intent to use exposure therapy include age, training in exposure, education, CBT orientation, therapist anxiety, and attitudes towards exposure therapy. These findings have significant implications for patient care, given that exposure therapy is strongly recommended for anxiety disorders (NICE, Citation2013). Therefore, it will be necessary for future research to consider the gap between intention and behaviour when it comes to implementing exposure therapy, while considering the interaction between client, therapist, and organisational factors.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Aarons, A. (2004). Mental health provider attitudes toward adoption of evidence-based practice: The Evidence-Based Practice Attitude Scale (EBPAS). Mental Health Services Research, 6(2), 61–74. https://doi.org/10.1023/B:MHSR.0000024351.12294.65
- Addis, E., & Krasnow, D. (2000). A national survey of practicing psychologists’ attitudes toward psychotherapy treatment manuals. Journal of Consulting and Clinical Psychology, 68(2), 331–339. https://doi.org/10.1037/0022-006X.68.2.331
- Addis, M. E., & Carpenter, K. M. (1999). Why, why, why? Reason‐giving and rumination as predictors of response to activation‐and insight‐oriented treatment rationales. Journal of Clinical Psychology, 55(7), 881–894. https://doi.org/10.1002/-SICI-1097-4679-199907-55:7<881:AID-JCLP9>3.0.CO;2-E
- Arnold, S. J., Bender, V. F., & Brown, S. A. (2006). A review and comparison of psychology-related electronic resources. Journal of Electronic Resources in Medical Libraries, 3(3), 61–80. https://doi.org/10.1300/J383v03n03_04
- * Becker, C., Zayfert, C., & Anderson, E. (2004). A survey of psychologists’ attitudes towards and utilization of exposure therapy for PTSD. Behaviour Research and Therapy, 42(3), 277–292. https://doi.org/10.1016/S0005-7967(03)00138-4
- * Becker-Haimes, E., Okamura, K., Benjamin Wolk, C., Rubin, R., Evans, A., & Beidas, R. (2017). Predictors of clinician use of exposure therapy in community mental health settings. Journal of Anxiety Disorders, 49, 88–94. https://doi.org/10.1016/j.janxdis.2017.04.002
- Bond, W., Hayes, S. C., Baer, A., Carpenter, M., Guenole, N., Orcutt, K., Waltz, T., & Zettle, R. D. (2011). Preliminary psychometric properties of the acceptance and action questionnaire–II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy, 42(4), 676–688. https://doi.org/10.1016/j.beth.2011.03.007
- Bouchard, S., Gauthier, J., Laberge, B., French, D., Pelletier, M. -H., & Godbout, C. (1996). Exposure versus cognitive restructuring in the treatment of panic disorder with agoraphobia. Behaviour Research and Therapy, 34(3), 213–224. https://doi.org/10.1016/0005-7967(95)00077-1
- Brosan, L., Reynolds, S., & Moore, R. (2006). Factors associated with competence in cognitive therapists. Behavioural and Cognitive Psychotherapy, 35, 179–190. https://doi.org/10.1017/S1352465806003304
- Brown, A., Mountford, A., & Waller, G. (2013). An idea worth researching: Is the therapeutic alliance overvalued in the treatment of eating disorders? The International Journal of Eating Disorders, 46(8), 779–782. https://doi.org/10.1002/eat.22177
- Butler, R. M., & Heimberg, R. G. (2020). Exposure therapy for eating disorders: A systematic review. Clinical Psychology Review, 78, 101851. https://doi.org/10.1016/j.cpr.2020.101851
- Carleton, N., Norton, P., & Asmundson, G. (2007). Fearing the unknown: A short version of the Intolerance of Uncertainty Scale. Journal of Anxiety Disorders, 21(1), 105–117. https://doi.org/10.1016/j.janxdis.2006.03.014
- Carpenter, J., Andrews, L., Witcraft, S., Powers, M., Smits, J., & Hofmann, S. (2018). Cognitive behavioral therapy for anxiety and related disorders: A meta-analysis of randomized placebo-controlled trials. Depression and Anxiety, 35(6), 502–514. https://doi.org/10.1002/da.22728
- Chadegani, A. A., Salehi, H., Yunus, M. M., Farhadi, H., Fooladi, M., Farhadi, M., & Ebrahim, N. A. (2013). A comparison between two main academic literature collections: Web of science and Scopus databases. Asian Social Science, 9(5). https://doi.org/10.5539/ass.v9n5p18
- Connor, K. M., & Davidson, J. R. (2003). Development of a new resilience Scale: The Connor‐Davidson resilience Scale (CD‐RISC). Depression and Anxiety, 18(2), 76–82. https://doi.org/10.1002/da.10113
- Cowdrey, D., & Waller, G. (2015). Are we really delivering evidence-based treatments for eating disorders? How eating-disordered patients describe their experience of cognitive behavioral therapy. Behaviour Research and Therapy, 75, 72–77. https://doi.org/10.1016/j.brat.2015.10.009
- Craske, M. G., Treanor, M., Conway, C. C., Zbozinek, T., & Vervliet, B. (2014). Maximizing exposure therapy: an inhibitory learning approach. Behaviour Research and Therapy, 58, 10–23. https://doi.org/10.1016/j.brat.2014.04.006
- de Beurs, E., Van Dyck, R., Marquenie, L. A., Lange, A., & Blonk, R. W. B. (2001). Depression Anxiety and Stress Scales--Dutch Version (DASS, DASS-42, DASS-21) [ Database record]. APA PsycTests https://doi.org/10.1037/t69646-000.
- * De Jong, R., Lommen, M., van Hout, W., De Jong, P., & Nauta, M. (2020). Therapists’ characteristics associated with the (non-)use of exposure in the treatment of anxiety disorders in youth: A survey among Dutch-speaking mental health practitioners. Journal of Anxiety Disorders, 73, 1–8. https://doi.org/10.1016/j.janxdis.2020.102230
- * Deacon, B., Farrell, N., Kemp, J., Dixon, L. J., Sy, J. T., Zhang, A. R., & McGrath, P. B. (2013). Assessing therapist reservations about exposure therapy for anxiety disorders: The Therapist Beliefs about Exposure Scale. Journal of Anxiety Disorders, 27(8), 772–780. https://doi.org/10.1016/j.janxdis.2013.04.006
- Deacon, B., Lickel, J., Farrell, N., Kemp, J., & Hipol, L. (2013). Therapist perceptions and delivery of interoceptive exposure for panic disorder. Journal of Anxiety Disorders, 27(2), 259–264. https://doi.org/10.1016/j.janxdis.2013.02.004
- Deacon, B. J., Meyer, J. M., Kemp, J. J., Farrell, N. R., Blakey, S. M., Benito, K. G., & Whiteside, S. P. (2019). How do clinicians deliver exposure therapy for anxiety? Evidence for anxiety increasing and anxiety decreasing delivery styles and therapist clusters [ Unpublished manuscript].
- EPHPP. (2017, May 24). Quality assessment dictionary. McMaster University. https://merst.ca/wp-content/uploads/2018/02/qualilty-assessment-dictionary_2017.pdf
- EPHPP. (2020, May 24). Quality assessment tool. McMaster University. https://merst.ca/wp-content/uploads/2018/02/quality-assessment-tool-2010.pdf
- Farrell, N., Deacon, B., Dixon, L., & Lickel, J. (2013). Theory-based training strategies for modifying practitioner concerns about exposure therapy. Journal of Anxiety Disorders, 27(8), 781–787. https://doi.org/10.1016/j.janxdis.2013.09.003
- Freiheit, S., Vye, C., Swan, R., & Cady, M. (2004). Cognitive-behavioral therapy for anxiety: Is dissemination working? The Behaviour Therapist, 27, 25–32.
- Gamez, W., Chmielewski, M., Kotov, R., Ruggero, C., & Watson, D. (2011). Development of a measure of experiential avoidance: The multidimensional experiential avoidance questionnaire. Psychological Assessment, 23(3), 692–713. https://doi.org/10.1037/A0023242
- Gosling, H., Pratt, D., Montgomery, H., & Lea, J. (2021). The relationship between minority stress factors and suicidal ideation and behaviours amongst transgender and gender non-conforming adults: A systematic review. Journal of Affective Disorders, 303, 31–51. https://doi.org/10.1016/j.jad.2021.12.091
- Griffin, D. W., & Bartholomew, K. (1994). Models of the self and other: Fundamental dimensions underlying measures of adult attachment. Journal of Personality and Social Psychology, 67(3), 430. https://doi.org/10.1037/0022-3514.67.3.430
- Gunter, R. W., & Whittal, M. L. (2010). Dissemination of cognitive-behavioral treatments for anxiety disorders: Overcoming barriers and improving patient access. Clinical Psychology Review, 30(2), 194–202. https://doi.org/10.1016/j.cpr.2009.11.001
- Hamilton, W. K., Aydin, B., Mizumoto, A., Coburn, K., & Zelinsky, N. (2017). Package ‘MAVIS’ (Version 1.1.3). http://kylehamilton.net/shiny/MAVIS/
- Harari, M. B., Parola, H. R., Hartwell, C. J., & Riegelman, A. (2020). Literature searches in systematic reviews and meta-analyses: A review, evaluation, and recommendations. Journal of Vocational Behavior, 118, 103377. https://doi.org/10.1016/j.jvb.2020.103377
- Hedman-Lagerlöf, M., Hedman-Lagerlöf, E., Axelsson, E., Ljótsson, B., Engelbrektsson, J., Hultkrantz, S., Lundbäck, K., Björkander, D., Wicksell, R. K., Flink, I., & Andersson, E. (2018). Internet-delivered exposure therapy for fibromyalgia: A randomized controlled trial. The Clinical Journal of Pain, 34(6), 532–542. https://doi.org/10.1097/AJP.0000000000000566
- Higgins, J. P., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta‐analyses. British Medical Journal, 327, 557–560. https://doi.org/10.1136/bmj.327.7414.557
- Hipol, L. J., & Deacon, B. J. (2013). Dissemination of evidence-based practices for anxiety disorders in Wyoming: A survey of practicing psychotherapists. Behavior Modification, 37(2), 170–188. https://doi.org/10.1177/0145445512458794
- * Hundt, N., Harik, J., Barrera, T., Cully, J., & Stanley, M. (2016). Treatment decision-making for posttraumatic stress disorder: The impact of patient and therapist characteristics. Psychological Trauma: Theory, Research, Practice, and Policy, 8(6), 728–735. https://doi.org/10.1037/tra0000102
- * Jelinek, L., Balzar, A., Moritz, S., Reininger, K., & Miegel, F. (2022). Therapists’ thought-action fusion beliefs predict utilization of exposure in obsessive-compulsive disorder. Behavior Therapy, 53(1), 23–33. https://doi.org/10.1016/j.beth.2021.05.004
- Kaczkurkin, A., & Foa, E. (2015). Cognitive-behavioral therapy for anxiety disorders: An update on the empirical evidence. Dialogues in Clinical Neuroscience, 17(3), 337–346. https://doi.org/10.31887/DCNS.2015.17.3/akaczkurkin
- Kampmann, I. L., Emmelkamp, P. M., Hartanto, D., Brinkman, W. -P., Zijlstra, B. J., & Morina, N. (2016). Exposure to virtual social interactions in the treatment of social anxiety disorder: A randomized controlled trial. Behaviour Research and Therapy, 77, 147–156. https://doi.org/10.1016/j.brat.2015.12.016
- * Kannis-Dymand, L., Grace, E., Mcdonald, L., & Chambers, R. (2022). Australian and New Zealand psychologists’ perceptions and use of therapist-guided exposure for panic disorder. The Clinical Psychologist, 26(1), 11–22. https://doi.org/10.1080/13284207.2022.2035651
- * Keleher, J., Jassi, A., & Krebs, G. (2020). Clinician-reported barriers to using exposure with response prevention in the treatment of paediatric obsessive-compulsive disorder. Journal of Obsessive-Compulsive and Related Disorders, 24, 1–7. https://doi.org/10.1016/j.jocrd.2019.100498
- * Kline, A., Klein, A., Bowling, A., & Feeny, N. (2021). Exposure therapy beliefs and utilization for treatment of PTSD: A survey of licensed mental health providers. Behavior Therapy, 52(4), 1019–1030. https://doi.org/10.1016/j.beth.2021.01.002
- Körfer, K., Schemer, L., Kube, T., & Glombiewski, J. A. (2020). An experimental analogue study on the “dose-response relationship” of different therapeutic instructions for pain exposures: The more, the better? Journal of Pain Research, 13, 3181–3193. https://doi.org/10.2147/JPR.S265709
- * Levita, L., Duhne, P., Girling, C., & Waller, G. (2016). *facets of clinicians’ anxiety and the delivery of cognitive behavioral therapy. Behaviour Research and Therapy, 77, 157–161. https://doi.org/10.1016/j.brat.2015.12.015
- Ljótsson, B., Hedman, E., Andersson, E., Hesser, H., Lindfors, P., Hursti, T., Rydh, S., Rück, C., Lindefors, N., & Andersson, G. (2011). Internet-delivered exposure-based treatment vs. stress management for irritable bowel syndrome: A randomized trial. The American Journal of Gastroenterology, 106(8), 1481–1491. https://doi.org/10.1038/ajg.2011.139
- McLean, C. P., Levy, H. C., Miller, M. L., & Tolin, D. F. (2022). Exposure therapy for PTSD: A meta-analysis. Clinical Psychology Review, 91, 102115. https://doi.org/10.1016/j.cpr.2021.102115
- Merry, L., Small, R., Blondel, B., & Gagnon, A. J. (2013). International migration and caesarean birth: A systematic review and meta-analysis. BMC Pregnancy and Childbirth, 13(1), 1–23. https://doi.org/10.1186/1471-2393-13-27
- * Meyer, J., Farrell, N., Kemp, J., Blakey, S., & Deacon, B. (2014). Why do clinicians exclude anxious clients from exposure therapy? Behaviour Research and Therapy, 54, 49–53. https://doi.org/10.1016/j.brat.2014.01.004
- * Meyer, J., Kelly, P. J., & Deacon, B. J. (2020). Therapist beliefs about exposure therapy implementation. The Cognitive Behaviour Therapist, 13(10), 1–14. https://doi.org/10.1017/S1754470X20000112
- * Moritz, S., Külz, A., Voderholzer, U., Hillebrand, T., McKay, D., & Jelinek, L. (2019). “Phobie à deux” and other reasons why clinicians do not apply exposure with response prevention in patients with obsessive–compulsive disorder. Cognitive Behaviour Therapy, 48(2), 162–176. https://doi.org/10.1080/16506073.2018.1494750
- * Moses, K., Gonsalvez, C., & Meade, T. (2021). Utilisation and predictors of use of exposure therapy in the treatment of anxiety, OCD and PTSD in an Australian sample: A preliminary investigation. BMC Psychology, 9(1), 1–11. https://doi.org/10.1186/s40359-021-00613-7
- Mulkens, S., de Vos, C., de Graaff, A., & Waller, G. (2018). To deliver or not to deliver cognitive behavioral therapy for eating disorders: Replication and extension of our understanding of why therapists fail to do what they should do. Behaviour Research and Therapy, 106, 57–63. https://doi.org/10.1016/j.brat.2018.05.004
- NICE. (2013). Social anxiety disorder: Recognition, assessment and treatment. https://www.nice.org.uk/guidance/cg159/chapter/Recommendations#interventions-for-adults-with-social-anxiety-disorder-2
- Nicholson, E., McDonnell, T., De Brún, A., Barrett, M., Bury, G., Collins, C., Hensey, C., & McAuliffe, E. (2020). Factors that influence family and parental preferences and decision making for unscheduled paediatric healthcare–systematic review. BMC Health Services Research, 20(1), 1–23. https://doi.org/10.1186/s12913-020-05527-5
- Niven, J., Mrklas, J., Holodinsky, K., Straus, E., Hemmelgarn, R., Jeffs, P., & Stelfox, T. (2015). Towards understanding the de-adoption of low-value clinical practices: A scoping review. BMC Medicine, 13(1), 1. https://doi.org/10.1186/s12916-015-0488-z
- Odgers, K., Kershaw, K. A., Li, S. H., & Graham, B. M. (2022). The relative efficacy and efficiency of single- and multi-session exposure therapies for specific phobia: A meta-analysis. Behaviour Research and Therapy, 159, 104203. https://doi.org/10.1016/j.brat.2022.104203
- Ojalehto, H. J., Abramowitz, J. S., Hellberg, S. N., Buchholz, J. L., & Twohig, M. P. (2020). Adherence to exposure and response prevention as a predictor of improvement in obsessive-compulsive symptom dimensions. Journal of Anxiety Disorders, 72, 102210. https://doi.org/10.1016/j.janxdis.2020.102210
- Olatunji, O., Williams, L., Tolin, D. F., Abramowitz, J., Sawchuk, N., Lohr, M., & Elwood, S. (2007). The Disgust Scale: Item analysis, factor structure, and suggestions for refinement. Psychological Assessment, 19(3), 281–297. https://doi.org/10.1037/1040-3590.19.3.281
- Oser, M., Khan, A., Kolodziej, M., Gruner, G., Barsky, A. J., & Epstein, L. (2021). Mindfulness and interoceptive exposure therapy for anxiety sensitivity in atrial fibrillation: A pilot study. Behavior Modification, 45(3), 462–479. https://doi.org/10.1177/0145445519877619
- Ougrin, D. (2011). Efficacy of exposure versus cognitive therapy in anxiety disorders: Systematic review and meta-analysis. BMC Psychiatry, 11(1), 200. https://doi.org/10.1186/1471-244X-11-200
- Pacini, R., & Epstein, S. (1999). The relation of rational and experiential information processing styles to personality, basic beliefs, and the ratio-bias phenomenon. Journal of Personality and Social Psychology, 76(6), 972–987. https://doi.org/10.1037/0022-3514.76.6.972
- * Parker, Z., & Waller, G. (2019). Psychotherapists’ reports of technique use when treating anxiety disorders: Factors associated with specific technique use. The Cognitive Behaviour Therapist, 12(33), 1–13. https://doi.org/10.1017/S1754470X19000205
- Parker, Z. J., & Waller, G. (2017). Development and validation of the negative attitudes towards CBT Scale. Behavioural and Cognitive Psychotherapy, 45(6), 629–646. https://doi.org/10.1017/S1352465817000170
- Peterson, R. A., & Brown, S. P. (2005). On the use of beta coefficients in meta-analysis. The Journal of Applied Psychology, 90(1), 175. https://doi.org/10.1037/0021-9010.90.1.175
- * Pittig, A., Kotter, R., & Hoyer, J. (2019). The struggle of behavioral therapists with exposure: Self-reported practicability, negative beliefs, and therapist distress about exposure-based interventions. Behavior Therapy, 50(2), 353–366. https://doi.org/10.1016/j.beth.2018.07.003
- * Reid, A., Bolshakova, M., Guzick, A., Fernandez, A., Striley, C., Geffken, G., & McNamara, J. (2017). Common barriers to the dissemination of exposure therapy for youth with anxiety disorders. Community Mental Health Journal, 53(4), 432–437. https://doi.org/10.1007/s10597-017-0108-9
- * Reid, A., Guzick, A., Fernandez, A., Deacon, B., McNamara, J., Geffken, G., McCarty, R., & Striley, C. (2018). Exposure therapy for youth with anxiety: Utilization rates and predictors of implementation in a sample of practicing clinicians from across the United States. Journal of Anxiety Disorders, 58, 8–17. https://doi.org/10.1016/j.janxdis.2018.06.002
- Rosen, C. S., Chow, H. C., Finney, J. F., Greenbaum, M. A., Moos, R. H., Sheikh, J. I., & Yesavage, J. A. (2004). VA practice patterns and practice guidelines for treating posttraumatic stress disorder. Journal of Traumatic Stress, 17(3), 213–222. https://doi.org/10.1023/B:JOTS.0000029264.23878.53
- Rosenberg, M. (1965). Society and the adolescent self-image. Princeton University Press.
- Rosenthal, R. (1991). Meta‐ analytic procedures for social research. Sage Publications Inc. https://doi.org/10.4135/9781412984997
- * Rowe, C., & Kangas, M. (2020). The impact of Australian psychologists’ education, beliefs, theoretical understanding, and attachment on the use and implementation of exposure therapy. Behaviour Change, 37(3), 151–170. https://doi.org/10.1017/bec.2020.9
- Royal College of Psychiatrists. (2013). Report of the second round of the National Audit of Psychological Therapies (NAPT). Health Care Quality Improvement Partnership.
- Ruffell, B., Smith, D. M., & Wittkowski, A. (2019). The experiences of male partners of women with postnatal mental health problems: A systematic review and thematic synthesis. Journal of Child and Family Studies, 28(10), 2772–2790. https://doi.org/10.1007/s10826-019-01496-4
- * Sars, D., & van Minnen, A. (2015). On the use of exposure therapy in the treatment of anxiety disorders: A survey among cognitive behavioural therapists in the Netherlands. BMC Psychology, 3(26). https://doi.org/10.1186/s40359-015-0083-2
- * Scherr, S., Herbert, J., & Forman, E. (2015). The role of therapist experiential avoidance in predicting therapist preference for exposure treatment for OCD. Journal of Contextual Behavioral Science, 4(1), 21–29. https://doi.org/10.1016/j.jcbs.2014.12.002
- Schumacher, S., Miller, R., Fehm, L., Kirschbaum, C., Fydrich, T., & Strohle, A. (2015). Therapists’ and patients’ stress responses during graduated versus flooding in vivo exposure in the treatment of specific phobia: A preliminary observational study. Psychiatry Research, 230(2), 668–675. https://doi.org/10.1016/j.psychres.2015.10.020
- * Schumacher, S., Schopka, N. M., Heinrich, M., & Knaevelsrud, C. (2019). The German adaptation of the Therapist Beliefs about Exposure Scale. Behavioural and Cognitive Psychotherapy, 47, 164–180. https://doi.org/10.1017/S1352465818000371
- * Schumacher, S., Weiss, D., & Knaevelsrud, C. (2018). Dissemination of exposure in the treatment of anxiety disorders and post‐traumatic stress disorder among German cognitive behavioural therapists. Clinical Psychology & Psychotherapy, 25(6), 856–864. https://doi.org/10.1002/cpp.2320
- Shafran, R., Thordarson, D. S., & Rachman, S. (1996). Thought-action fusion in obsessive compulsive disorder. Journal of Anxiety Disorders, 10(5), 379–391. https://doi.org/10.1016/0887-6185(96)00018-7
- Sharp, R., Herbert, D., & Redding, E. (2008). The role of critical thinking skills in practising clinical psychologists’ choice of intervention technique. The Scientific Review of Mental Health Practice, 6(1), 21–30.
- Simmons, A., Milnes, S., & Anderson, D. (2008). Factors influencing the utilization of empirically supported treatments for eating disorders. Eating Disorders: The Journal of Treatment & Prevention, 16(4), 342–354. https://doi.org/10.1080/10640260802116017
- Speers, A., Bhullar, N., Cosh, S., & Wootton, B. (2022). Correlates of therapist drift in psychological practice: A systematic review of therapist characteristics. Clinical Psychology Review, 93, 102–132. https://doi.org/10.1016/j.cpr.2022.102132
- * Stewart, E., Frank, H., Benito, K., Wellen, B., Herren, J., Skriner, L. C., & Whiteside, S. P. H. (2016). Exposure therapy practices and mechanism endorsement: A survey of specialty clinicians. Professional Psychology, Research and Practice, 47(4), 303–311. https://doi.org/10.1037/pro0000094
- Stobie, B., Taylor, T., Quigley, A., Ewing, S., & Salkovskis, P. (2007). “Contents may vary”: A pilot study of treatment histories of OCD patients. Behavioural and Cognitive Psychotherapy, 35(3), 273–282. https://doi.org/10.1017/S135246580700358X
- Stumpf, E., Higa McMillan, K., & Chorpita, F. (2009). The implementation of evidence-based services for youth: Assessing provider knowledge. Behavior Modification, 33(1), 48–65. https://doi.org/10.1177/0145445508322625
- Taylor, S., Zvolensky, J., Cox, B., Deacon, B. J., Heimberg, R. G., Ledley, D. R., Abramowitz, J. S., Holaway, R. M., Sandin, B., Stewart, S. H., Coles, M., Eng, W., Daly, E. S., Arrindell, W. A., Bouvard, M., & Cardenas, S. J. (2007). Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment, 19(2), 196–188. https://doi.org/10.1037/1040-3590.19.2.176
- Thomas, B. H., Ciliska, D., Dobbins, M., & Micucci, S. (2004). A process for systematically reviewing the literature: Providing the research evidence for public health nursing interventions. Worldviews on Evidence-Based Nursing, 1(3), 176–184. https://doi.org/10.1111/j.1524-475X.2004.04006.x
- Trivasse, H., Webb, T., & Waller, G. (2020). A meta-analysis of the effects of training clinicians in exposure therapy on knowledge, attitudes, intentions, and behavior. Clinical Psychology Review, 80, 80. https://doi.org/10.1016/j.cpr.2020.101887
- * van Minnen, A., Hendriks, L., & Olff, M. (2010). When do trauma experts choose exposure therapy for PTSD patients? A controlled study of therapist and patient factors. Behaviour Research and Therapy, 48(4), 312–320. https://doi.org/10.1016/j.brat.2009.12.003
- Veal, R., Critchley, C., Luebbers, S., Cossar, R., & Ogloff, J. R. (2021). Factor structure of the psychopathy checklist: Screening Version (PCL: SV): A systematic review using narrative synthesis. Journal of Psychopathology and Behavioral Assessment, 43(3), 565–582. https://doi.org/10.1007/s10862-021-09877-0
- Vevea, J. L., & Hedges, L. V. (1995). A general linear model for estimating effect size in the presence of publication bias. Psychometrika, 60(3), 419–435. https://doi.org/10.1007/BF02294384
- Walfish, S., McAlister, B., O’donnel, P., & Lambert, M. (2012). An investigation of self-assessment bias in mental health providers. Psychological Reports, 110(2), 1–6. https://doi.org/10.2466/02.07.17.PR0.110.2.639-644
- Waller, G. (2009). Evidence-based treatment and therapist drift. Behaviour Research and Therapy, 47(2), 119–127. https://doi.org/10.1016/j.brat.2008.10.018
- Waller, G., Stringer, H., & Meyer, C. (2012). What cognitive behavioral techniques do therapists report using when delivering cognitive behavioral therapy for the eating disorders? Journal of Consulting and Clinical Psychology, 80(1), 171. https://doi.org/10.1037/a0026559
- Waller, G., & Turner, H. (2016). Therapist drift redux: Why well-meaning clinicians fail to deliver evidence-based therapy, and how to get back on track. Behaviour Research and Therapy, 77, 129–137. https://doi.org/10.1016/j.brat.2015.12.005
- Weersing, R., Weisz, J., & Donenberg, G. (2002). Development of the therapy procedures checklist: A therapist-report measure of technique use in child and adolescent treatment. Journal of Clinical Child & Adolescent Psychology, 31(2), 168–180. https://doi.org/10.1207/S15374424JCCP3102_03
- * Whiteside, S., Deacon, B., Benito, K., & Stewart, E. (2016). Factors associated with practitioners’ use of exposure therapy for childhood anxiety disorders. Journal of Anxiety Disorders, 40, 29–36. https://doi.org/10.1016/j.janxdis.2016.04.001
Appendices Appendix A
Search strategy (original data search 13th September 2021, updated 8th August 2022)
Scopus
(Therapist* OR “CBT therapist*” OR “cognitive behavio*ral therapist*” OR psychologist* OR “clinical psychologist*” OR clinician* OR psychotherapist*) W/3 (anxiet* OR characteristic* OR factor* OR belief*)
AND
“exposure therap*”
Psycinfo
((therapist* or “CBT therapist*” or “cognitive behavio*ral therapist*” or psychologist* or “clinical psychologist*” or clinician* or psychotherapist*) adj3 (anxiet* or characteristic* or factor* or belief*))
AND
Exp Exposure therapy
Web of Science
((therapist* OR “CBT therapist*” OR “cognitive behavio*ral therapist*” OR psychologist* OR “clinical psychologist*” OR clinician* OR psychotherapist*) NEAR/3 (anxiet* OR characteristic* OR factor* OR belief*))
AND
“exposure therap*”
Appendix B
Quality Rating Table
Appendix C
Funnel Plots for all Meta-Analyses