ABSTRACT
Repetitive Negative Thinking (RNT) encompasses both worry and rumination and is a transdiagnostic process. A systematic review and meta-analysis were co-produced with individuals with lived experience of anxiety and depression. The objective was to examine the efficacy of RNT-specific psychological interventions. Inclusion criteria were mean age or range 10–24 years, and including a measure of worry, rumination, RNT, anxiety, depression, psychosis, self-harm, or suicide. The Cochrane Risk of Bias measure was used. PsycInfo, Medline/PubMed, Scopus and Embase databases were searched on 24 April 2023. There were 16 studies with 20 RNT interventions, N = 1,183 participants, 79% female, mean pooled age = 20.08 years. There was a small effect of RNT interventions on anxiety symptoms (g = −0.43 to −0.47, 95% CI = −0.23 to −0.70). There were small-to-medium effects on depressive symptoms (g = −0.40 to −0.52, 95% CI = −0.19 to −0.84), and RNT (g = −0.59 to −0.71, 95% CI = −0.41 to −1.01). Most studies indicated some concerns for risk of bias. Transdiagnostic interventions that target RNT are efficacious in reducing symptoms of anxiety, depression, and RNT in young people. Further research is required to address younger age groups, psychosis, and different cultural contexts.
Protocol Registration
PROSPERO (CRD42023408899).
Transdiagnostic approaches consider the role of processes maintaining multiple psychological disorders (Dalgleish et al., Citation2020). Worry and rumination are transdiagnostic processes (Ehring & Watkins, Citation2008; Zagaria et al., Citation2023), involved in anxiety, depression (Funk et al., Citation2022; McEvoy et al., Citation2018), psychosis (Hartley et al., Citation2014), suicidal ideation (Law & Tucker, Citation2018; Teismann et al., Citation2021) and self-harm (Dawkins et al., Citation2019). Worry involves thoughts about future problems, while rumination is past focused. Both worry and rumination are examples of “repetitive negative thinking” (RNT) (Stade & Ruscio, Citation2023). Definitions of RNT emphasise the tendency to get “stuck” in negative thinking (Ehring & Watkins, Citation2008). Given excessive RNT is a transdiagnostic process, it is an ideal target for early intervention for a range of psychological symptoms (Topper et al., Citation2010).
Interventions for RNT are based on addressing abstract styles of thinking and challenging metacognitions (e.g. Ehring & Behar, Citation2021; Ehring & Watkins, Citation2008; Wells, Citation2011). Metacognitions refer to positive and negative beliefs about thought processes and are theorised to maintain worry and rumination. For example, an individual may hold positive beliefs about worry as they think it can enable them to solve and avoid future problems, hence continue to worry as they think it is useful (Wells, Citation2011). Examples of RNT-specific interventions include rumination-focused Cognitive Behaviour Therapy (RFCBT; Watkins, Citation2016) and metacognitive therapy (MCT; Wells, Citation2011). MCT focuses on challenging the perceived benefits of RNT, and changing the process of thinking, including how intensely an individual engages with thoughts, rather than changing the content of thoughts. RFCBT also focuses on changing the process of thinking, through helping an individual learn to notice and change their thinking processes from an abstract style (e.g. “why am I such a failure?”) to a concrete style (e.g. “what exactly has led me to failing this time, what are the next steps I want to take?”). Interventions for RNT decrease psychological distress and improve quality of life with large effect sizes in adults (e.g. McEvoy et al., Citation2015).
The efficacy of RNT interventions in young people aged 14–24 years, with elevated symptoms of anxiety and depression, was examined by Bell et al. (Citation2023). This review included interventions categorised as RNT focused, compared to non-RNT focused. There were 21 randomised controlled trials (RCTs) categorised as RNT focused interventions, which demonstrated a significant impact favouring intervention versus control at post-treatment, on anxiety (g = −0.42) and depression (g = −0.47). Additionally, Bell et al. (Citation2023) concluded that interventions targeting RNT do not need to be long as higher treatment dose did not show better results. Bell et al.'s (Citation2023) review was useful in highlighting the appeal of RNT interventions as brief, effective transdiagnostic interventions in young people. However, closer inspection of the interventions categorised as RNT focused raises questions over the specificity of the interventions included. Only around half of the interventions Bell et al. (Citation2023) categorised as RNT focused appear to be RNT specific. The remaining studies classified as RNT focused were of standard or general psychological interventions not designed specifically to target RNT or based on a model of RNT as a maintaining mechanism of distress, such as eye movement desensitization (e.g. Lytle et al., Citation2002) and attention training to positive stimuli (e.g. Sass et al., Citation2017). Bell et al. (Citation2023) did not outline any specific criteria that were used to judge whether an intervention was RNT-focused or non-RNT focused. Examples of interventions that the authors judged as non-RNT focused included CBT for insomnia, and self-monitoring. Further, Bell et al. (Citation2023) did not report on insights from individuals with lived experience of anxiety and depression in their review.
Given previous reviews (Bell et al., Citation2023) did not report on insights from lived experience experts in their publication, it is important for a review to be co-produced with young people. It is imperative to integrate meaning from young people with lived experience of mental health problems through more extensive engagement consistent with co-production methods, including, for example, monthly meetings with lived experience experts over the course of a systematic review. Co-production with young people with lived experience of mental health problems is essential to produce a high-quality review of interventions for worry and rumination. Research in partnership with lived experience experts using co-production methods (Norton, Citation2021) is vital to inform best practice (Schleider, Citation2023). Co-produced research with individuals with lived experience of mental health problems can improve mental health service quality and delivery (Egan et al., Citation2023). Further, lived experience engagement is critical in improving intervention uptake (Schouten et al., Citation2022; Sunkel & Sartor, Citation2022).
The purpose of the current co-produced systematic review and meta-analysis was to examine the transdiagnostic efficacy of RNT interventions in young people aged 10–24 years. The four novel aspects of this review building on Bell et al. (Citation2023) are as follows: (1) age range lowered to 10 years to examine evidence for early intervention, (2) outcomes extended beyond anxiety and depression to self-harm, suicide and psychosis, (3) inclusion of individuals with a “sub-threshold” diagnosis (i.e. elevated symptoms), in addition to young people with low to high symptom severity, which may also include prevention studies, and (4) co-production of the review with people with lived experience of mental health problems. Another purpose of the review was to understand through examination of moderators in which contexts, and for whom, RNT interventions appear to work.
The overall aim was to co-produce with young people a systematic review and meta-analysis to understand the efficacy of RNT interventions as a transdiagnostic early intervention. It was hypothesised that RNT interventions would result in significant decreases in symptoms of anxiety, depression, psychosis, and measures of suicide and self-harm.
Method
Co-production with young people with lived experience of mental health problems
Consistent with reviews highlighting the importance of young people co-producing reviews of interventions (e.g. Breen et al., Citation2023; Egan et al., Citation2022), collaboration included lived experience leads (SR, ST, GK) and a lived experience Youth Advisory Committee (YAC). The YAC comprised seven young people (19–29 years; gender 43% female, 29% male, 14% non-binary, 14% not reported) from Kenya (n = 2), India (n = 2), Australia (n = 2), and the United Kingdom (UK; n = 1). Lived experience leads identified young people for the committee, led YAC meetings, synthesised insights, and conducted key aspects of the research such as defining search terms, judging the degree of specific RNT content of interventions, and writing the publication. Individuals in the YAC signed consent forms prior to the first meeting, and the research was approved by the Curtin University Human Research Ethics Committee (HRE2023–0154). The YAC shared their insights into how worry and rumination were relevant to their lived experience of anxiety, depression, and psychosis. The YAC guided all stages of the research, for example, helping to create the search strategy and protocol, lay summary, infographic and video for dissemination.
Search strategy and selection criteria
PsycINFO, Medline/PubMed, Scopus, Embase were searched on 24 April 2023, using the following search terms: depress* OR anxiety OR self-injury OR self-harm OR psychosis AND repetitive negative thinking OR negative thoughts OR worry OR rumination OR repetitive thinking OR perseverative cognitionFootnote1 AND RCT OR randomised control trial. There were no date restrictions.
Articles were screened according to the following inclusion criteria: (a) peer-reviewed journal publication in English or German; (b) a controlled trial of worry/rumination/RNT intervention comparing to any form of control condition (including wait-list, no-treatment, placebo or active treatment comparison), (c) intervention(s) were focused specifically on worry, rumination or RNT (see for definition), including both internet delivered and face-to-face interventions, (d) included a validated psychometric measure of worry, rumination or RNT and anxiety, depression, suicide, self-harm or psychosis, (e) participant mean age between 10 and 24 years (if mean age was not specified, an age range within these years), and (f) ethical approval and ascertainment of written informed consent in the published article. The exclusion criteria were as follows: (a) an intervention which is general, or another psychological approach not specifically stated as a treatment for worry/rumination/RNT (e.g. general cognitive behaviour therapy), and (b) open trials, qualitative studies, grey literature, dissertations, and unpublished studies.
Table 1. Definition of specific Repetitive Negative Thinking (RNT) interventions.
The reference list of Bell et al. (Citation2023) was screened to identify any RNT-specific interventions that met our inclusion criteria which were not located by the database search. This resulted in 12 of the 21 articles included in the previous review being included in the current review according to our definition of an RNT-specific intervention (see and supplementary materials).
Procedure
The systematic review was registered with PROSPERO (CRD42023408899) on 28 March 2023. The primary rater (TC) screened 100% of titles/abstracts, with a random 30% screened independently by a secondary rater (TB), resulting in substantial agreement (Cohen’s k = 0.66; Landis & Koch, Citation1977). All full-text articles were screened by TC, with a random 30% screened independently by TB, which resulted in substantial agreement (Cohen’s k = 0.79; Landis & Koch, Citation1977). Consensus on final article inclusion was provided by SE and DG.
The YAC met in five online meetings. Young people co-produced the research including the proposal, search terms and registration, and dissemination outputs. In addition, young people were asked the following questions: “do you see worry and rumination as relevant to your experience of, for example, anxiety and depression?” and “do you see an intervention for worry/rumination as relevant to you, would you be interested in doing it?”. Further, young people discussed their interpretation of the findings from the systematic review and meta-analysis. They were invited to provide feedback via email when not able to attend meetings. YAC members received AUD$100 for each meeting.
Risk of bias
The Cochrane Risk-of-Bias Tool V.2 (Sterne et al., Citation2019) was used due to following PRISMA guidelines (Page et al., Citation2021) which recommend this is assessed. The five domains were as follows: randomisation process, deviations from the intended interventions, missing outcome data, measurement of the outcome, and selection of the results. Categories are “low risk”; low risk for all domains; “some concerns”; some concerns in at least one domain; “high risk”; high risk in one domain or some concerns for multiple domains.
Data analysis
Inter-rater reliability was calculated with Kappa coefficients in SPSS (Version 28; IBM Corp., 2021). The ranges are 0 = no agreement, .10–.20 = slight agreement, .21–.40 = fair agreement, .41–.60 = moderate agreement, .61–.80 = substantial agreement, .81–.99 = near perfect agreement, and 1 = perfect agreement (Landis & Koch, Citation1977).
Young people’s views expressed in the YAC meetings were summarised by SE using techniques of content analysis (Hsieh & Shannon, Citation2005), following a similar procedure to another co-designed review (Breen et al., Citation2023). Consensus was provided by SR and ST.
The data were analysed in a meta-analysis of between-groups effect sizes for the outcomes of worry, rumination, RNT, anxiety and depression. A Hunter-Schmidt Random Effects Model was used to pool effect sizes across studies for the primary outcomes of worry, rumination, RNT and psychological symptoms, due to significant variation across studies. To support the results of the random effects model we ran a Robust Bayesian meta-analysis (RoBMA) where we averaged across a set of 12 models to more accurately account for publication bias (see Maier et al., Citation2023). We assessed publication bias using Bayes factors and interpreted these based on the assumption that Bayes factors higher than one suggest evidence for publication bias. This method is superior to traditional methods such as Egger’s et al. (Citation1997) test, which cannot distinguish between lack of publication bias and lack of evidence for publication bias (Bartoš et al., Citation2022). Several Robust Bayesian meta-analysis models account for publication bias, where the predictive utility of the two competing (i.e. effect vs null effect) hypotheses are judged using Bayes factors (BF10; van Doorn et al., Citation2021). Bayes factors should be considered on a continuum but for ease of understanding there are some general rules of thumb. First, a Bayes factor larger than one is considered supportive of the alternative hypothesis (i.e. an effect) and a Bayes factor less than one is supportive of the null hypothesis. Second, the level of evidence can be judged as follows: Bayes factors between 1 and 3 (or 1/3 to 1) are considered weak evidence, Bayes factors between 3 and 10 (or 1/10 to 1/3) are considered moderate evidence, and Bayes factors of 10 or larger (or smaller than 1/10) are considered strong evidence in favour (or against) a hypothesis (Jeffreys, Citation1961).
Heterogeneity was assessed via I2 statistics and Bayes factors. I2 estimates suggest the percentage of variance in effect sizes due to heterogeneity, and were categorized as low (0–40%), medium (41–60%), or high (61–100%; Moher et al., Citation2009). Bayes factors for heterogeneity were assessed, where Bayes factors larger than one indicate evidence in favour of heterogeneity. We anticipated heterogeneity to be substantial across studies for all outcomes due to different types of interventions, different duration, and format. Subgroups included: dose, experimental design versus multi-session intervention, outcome measure (i.e. worry, repetitive negative thinking, rumination), and type of intervention (therapist-led or self-help). The number of sessions and session duration was used to classify dose as short (<2 hours), medium (3–6 hours), or long (7+ hours) in total.
Effect sizes (Hedge’s g or dkorr) were calculated using pre- and post-test means from the experimental and control groups. We used the method described by Klauer (Citation2001), where within-group effects are calculated for both the control and experimental groups and subtracted (i.e. intervention group effect-control group effect). Form three on the Psychometrica effect size calculators was used to compute dkorr (https://www.psychometrica.de/effect_size.html). A few studies only provided other statistics (e.g. f-values). For example, Pan et al. (Citation2020) did not provide means and SD pre- and post-test for control and experimental groups but did provide between-group effect sizes that were controlled for baseline differences. These were converted to hedges g and imputed into the meta-analysis. Effect sizes were interpreted according to Cohen (Citation1992), as small = 0.20–0.49, medium = 0.50–0.79, and large =>0.80, where a negative effect size indicates a decrease in psychological symptoms.
Results
Study characteristics
The search resulted in 3,527 studies after duplicate removal, of which 16 were included with 20 intervention groups (). The studies were predominately conducted in the UK and Europe (38%), followed by Australia (19%), USA (19%), Colombia (12%), Iran (6%) and China (6%). All interventions were rated by GK as RNT-specific with consensus by SE (see supplementary materials). Most interventions (25%) were RFCBT (Watkins, Citation2016), followed by RNT-specific CBT (25%), MCT (19%; Wells, Citation2011), working memory training (WMT) (19%), and RNT-specific Acceptance and Commitment Therapy (ACT) (12%). RFCBT and MCT were described in the Introduction. RNT specific CBT includes interventions targeting RNT, for example, worry journals where an individual record outcomes of worry events. RNT-specific ACT uses techniques for “defusing” from stuck thinking. WMT involves computer tasks to improve retention and manipulation of information in working memory. Participants were mainly female (79%), and most (81%) were young adults ( and ).
Table 2. Summary of characteristics across interventions.
Table 3. Study characteristics.
Risk of bias ratings
Most studies were categorised as having some concerns (93.75%), with the remainder as high risk (6.25%) (). There was moderate agreement (Cohen’s k = 0.55), between the primary (JF) and secondary rater (JKB) on risk of bias.
Efficacy of repetitive negative thinking interventions
Effects on worry, rumination and repetitive negative thinking
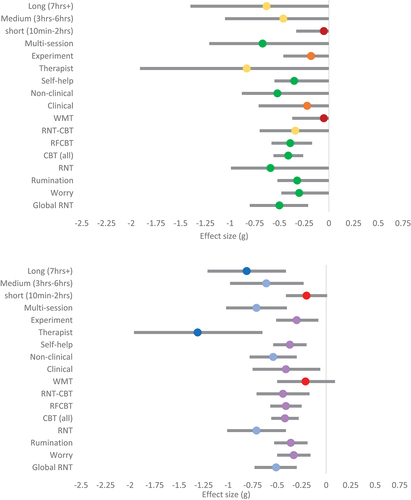
The output of the RoBMA showed strong support for small-to-medium effects of the efficacy of RNT interventions on rumination (g(hunter-schmidt) = −0.36; g(RoBMA) = −0.32; ) and worry (g(hunter-schmidt) = −0.33; g(RoBMA) = −0.30), and RNT (g(hunter-schmidt) = −0.71; g(RoBMA) = −0.59). The only noticeable difference between the random effects model and the RoBMA is on RNT, where the RoBMA gave a more conservative estimate. Random effects models suggested low to moderate-high heterogeneity (I2 = 20.86–64.08%), but RoBMA suggested we cannot be certain whether heterogeneity or publication bias is present (). There was strong evidence for the efficacy of RNT interventions on reducing global RNT, with a medium effect (g(hunter-schmidt) = −0.51; g(RoBMA) = −0.50). For global RNT, there was strong evidence for the presence of heterogeneity and moderate evidence for the absence of publication bias ().
Table 4. Pooled effects, heterogeneity, and publication bias results for all main analyses and sub-group analyses.
Considering specific forms of RNT interventions, the evidence for a small effect (g(hunter-schmidt) = −0.42 to −0.44; g(RoBMA) = −0.34 to −0.41) of CBT interventions on global RNT was strong (RFCBT) to moderate (RNT-CBT; ). Random effects models suggested low heterogeneity (I2 = 0.00%), but RoBMA suggested the evidence for the absence of heterogeneity with the current data is weak. There was weak to moderate evidence for the absence of publication bias across CBT intervention types. There was weak evidence in favour of a null effect of working memory training interventions on global RNT (g(hunter-schmidt) = −0.21; g(RoBMA) = −0.05), with little certainty as to whether heterogeneity or publication bias was present. There were not sufficient data points for MCT interventions to calculate a pooled effect, but two studies that tested MCT interventions and measured rumination support the efficacy of MCT on RNT (Modini & Abbott, Citation2018; Zemestani et al., Citation2016).
Self-help interventions had a small pooled effect on global RNT (g(hunter-schmidt) = −0.37; g(RoBMA) = −0.35), whereas therapist-led interventions produced a large effect (g(hunter-schmidt) = −1.31; g(RoBMA) = −0.83). However, there was strong evidence for the presence of heterogeneity among therapist-led interventions, indicating that particular therapist-led interventions might be more effective than others, but we cannot conclude which types.
There was weak evidence in favour of an effect of RNT experiments on global RNT, where the evidence for multi-session intervention on global RNT was strong (). Multi-session interventions produced a medium pooled effect on global RNT (g(hunter-schmidt) = −0.71; g(RoBMA) = −0.67), while experiments only produced a small effect (g(hunter-schmidt) = −0.30; g(RoBMA) = −0.18). Last, short interventions had little effect on reducing RNT (g(hunter-schmidt) = −0.20; g(RoBMA) = −0.05), whereas moderate and longer interventions had medium effects (g(hunter-schmidt) = −0.61 to − 0.81; g(RoBMA) = −0.46 to − 0.63; see ).
Figure 2. Forest plots for rumination.
Effects on anxiety
The output of the RoBMA showed strong support for the efficacy of RNT interventions on anxiety. The pooled effect was small (g(hunter-schmidt) = −0.47; g(RoBMA) = −0.43), with weak evidence for presence of heterogeneity and moderate evidence for the absence of publication bias. The random effects model demonstrated moderate–high levels of heterogeneity (I2 = 68.09%). Random effects models suggested MCT resulted in larger reductions in anxiety (g = −1.34), but RoBMA analysis suggested a more conservative, small effect (g = −0.42), with only weak evidence in favour of an effect. On closer inspection, one intervention (Zemestani et al., Citation2016) produced a very large effect that had a strong influence. Therefore, more studies with larger sample sizes are needed to confirm the efficacy of MCT on anxiety. The evidence for the efficacy of CBT interventions grouping together RFCBT and RNT specific CBT on anxiety was strong in favour of a small effect (g(hunter-schmidt) = −0.40; g(RoBMA) = −0.38). The evidence was less conclusive when considering RFCBT and RNT-CBT separately ().
Therapist-led RNT interventions appear to have a stronger effect on reducing anxiety (g(hunter-schmidt) = −1.28; g(RoBMA) = −0.49) compared to self-help interventions (g(hunter-schmidt) = −0.35; g(RoBMA) = −0.31). However, this comparison needs to be considered in light of RoBMA results suggesting that the current evidence is inconclusive for therapist-led interventions (BF10 = 1.64; ). There were only three data points for therapist-led interventions, and there is strong evidence for large heterogeneity. Therefore, more therapist-led RNT intervention studies with larger sample sizes are needed to confirm the comparative efficacy between self-help and therapist-led interventions. Experimental design interventions were less effective at reducing anxiety (g(hunter-schmidt) = −0.29; g(RoBMA) = −0.13) compared to multi-session interventions (g(hunter-schmidt) = −0.59; g(RoBMA) = −0.46). However, the evidence in favour of an effect for multi-session intervention was barely moderate (BF10 = 4.03) and there was strong evidence for heterogeneity. This suggests that specific types of multi-session RNT interventions are more effective than others, but there were not enough studies to make any conclusions. Last, it appears that longer interventions (g(hunter-schmidt) = −1.28; g(RoBMA) = −0.53) are more effective than medium (g(hunter-schmidt) = −0.28; g(RoBMA) = −0.20) and short interventions (g(hunter-schmidt) = −0.29; g(RoBMA) = −0.13). However, RoBMA results indicated evidence was inconclusive, and there was strong evidence for heterogeneity among longer interventions.
Effects on depression
The output of the RoBMA showed weak support for the efficacy of RNT interventions on depression. The pooled effect was small-medium (g(hunter-schmidt) = −0.52; g(RoBMA) = −0.40) with strong evidence for presence of heterogeneity (I2 = 80.27%) and moderate evidence for the absence of publication bias. However, there was stronger evidence for an effect of CBT focused interventions on depression (g(hunter-schmidt) = −0.43; g(RoBMA) = −0.41). There was weak evidence in favour of the absence of publication bias and heterogeneity for CBT interventions (). There were not sufficient data points for MCT or WMT interventions to calculate a pooled effect of their efficacy.
Therapist-led RNT interventions appear to have a stronger effect on depression (g(hunter-schmidt) = −1.34; g(RoBMA) = −0.49) compared to self-help interventions (g(hunter-schmidt) = −0.37; g(RoBMA) = −0.32). However, this comparison needs to be considered in light of RoBMA suggesting that the current evidence is inconclusive for therapist-led interventions (). There were only four data points for therapist-led interventions, and there is strong evidence for presence of heterogeneity among these effects. There were not enough data points to measure the effect of RNT experiments on depression. However, there was moderate evidence for an effect of multi-session RNT interventions in reducing depression. The pooled effect was medium (g(hunter-schmidt) = −0.66 g(RoBMA) = −0.53). There was strong evidence for the presence of heterogeneity and moderate evidence for the absence of publication bias. This suggests that specific types of multi-session RNT intervention might be more effective than others, but there were not enough studies to know which. Lastly, it appears that longer interventions (g(hunter-schmidt) = −1.21; g(RoBMA) = −0.48) are more effective than medium (g(hunter-schmidt) = −0.42; g(RoBMA) = −0.33) and short interventions (g(hunter-schmidt) = 0.05; g(RoBMA) = 0.01) in reducing depression. The evidence in favour of a null effect for short interventions is moderate, whereas the evidence in favour of an effect for medium and long interventions is moderate and weak, respectively. There is strong evidence for presence of heterogeneity in long interventions. See for a summary of all pooled effects.
Figure 3. Forest plots for anxiety.
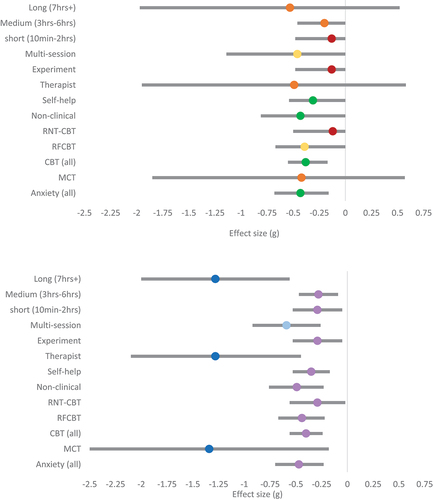
Figure 4. Forest plots for depression.

Young people’s views on worry and rumination
The YAC emphasised that worry and rumination were important to their lived experience of anxiety, depression, and psychosis. Young people commented about their experience saying, “It’s our mind playing games with us, worrying about the future, you get anxious” and “I feel like worrying is a part of situations where I become anxious”. Another young person said when they become aware they are worrying they think “I don’t want to go down that route, down the rabbit hole of getting stuck in thoughts”. Others said social media is an important part of their experience of worry and rumination, for example, “Constant looking at social media becomes repetitive and obsessive”. Some young people noted the difficulty in controlling repetitive thinking, for example, “I have insight into rumination, yet I can’t control it, that makes it worse, you attribute that lack of control to yourself … that leads to negative self-esteem”. Young people also talked about “overthinking”, e.g. “I overthink a lot”. Several people resonated with this, saying they engaged in “overthinking a lot”.
A discussion was also held about whether they would be interested in engaging in RNT interventions, and an example of MCT was discussed. All YAC members said they would be interested in treatments such as MCT for example, saying“I can definitely see the benefits of this intervention for worry for my own experiences and for others I have known”. One young person emphasised “the earlier the better”, and another said “I also feel like learning such tools very early on in life could help us a lot. As kids, we pick up things much faster and it’s easier to form a habit at a young age than older”. Another young person commented “I think early interception of worry and rumination can in fact help avoid the outcomes of depression, anxiety, suicidal thoughts. There are so many instances where I find myself jumping from one bad thought to another in a fraction of a second.” highlighting the importance of early intervention. Finally, young people said that treatments should be tailored according to cultural contexts saying, “we are diverse, the treatments should be different across countries”.
Discussion
The aim of this co-produced review was to examine the efficacy of interventions for RNT. We also aimed to understand the views of young people about the relevance of RNT. Young people were unanimous in their views that worry and rumination were relevant to their lived experience of anxiety, depression, and psychosis. These insights are consistent with qualitative studies in young people (Oliver et al., Citation2015; Sloan et al., Citation2021) and adults (Joubert et al., Citation2022), where individuals described worry and rumination as relevant to their mental health problems. The young people who co-produced our review underscored that they were interested in engaging in RNT-specific interventions, that early intervention was key, and that they recommended intervention may differ across cultural contexts. We found evidence for the efficacy of RNT-specific interventions in reduction of worry, rumination, RNT, anxiety, and depression in young people aged 14–24 years. No studies were located including samples with a mean age between 10 and 14 years, or measures of psychosis, self-harm, or suicide.
The RNT-specific interventions in our review included interventions where the protocol was based on RNT specific material, leading to the exclusion of other interventions, largely cognitive bias modification studies, that were included in Bell et al. (Citation2023). A strength of the current review was a stringent definition for what constituted an RNT-specific intervention, meaning conclusions can be drawn about interventions that are specifically designed to target RNT. Our findings of a small effect on anxiety (g = −0.43) were the same as Bell et al. (Citation2023). We also found converging evidence for small-medium effects on depression (g = −0.40 to g = −0.52), similar to Bell et al. (Citation2023) (g = −0.47). An important point to note when considering the small effects is that most studies included were in the context of prevention/early intervention, and most samples were non-clinical where smaller effect sizes are expected. However, examining prevention studies improves the generalisability of our results to young people in the community who are “sub-threshold” on psychological symptoms. Recent research has emphasised the promise of RNT interventions in prevention of mental health problems (Funk et al., Citation2023). Small effects in the context of prevention and early interventions have been argued to represent an important and effective outcome, where small effects can represent a large population benefit (O’Mara et al., Citation2023; Watson et al., Citation2016).
An important aspect of our review was an attempt to understand in which contexts, and for whom RNT interventions appear to work. We can conclude that short interventions of less than 2 hours duration are not recommended, as there was no impact on anxiety or depression. There was some evidence that interventions of a longer duration of 7 hours or more were more effective than medium length interventions. This result contrasts with Bell et al. (Citation2023), who did not find higher treatment dose to be associated with larger effects. There was some evidence from subgroup analyses that therapist-led interventions demonstrated stronger effects than self-help, consistent with the literature where guided interventions have stronger effects than unguided self-help (Andersson, Citation2016). However, the evidence for therapist-led versus self-help interventions was largely classified as weak due to the small number of studies included in the analysis. Any conclusions regarding comparative efficacy between these intervention modes should be tentative until there are further studies available. Future meta-analyses should examine mode of intervention. Reviews should also seek to examine differences in age, for example, high school versus university students. We had an insufficient number of studies to perform this sub-group analysis, with only three studies including high-school students. Hence, our findings apply mainly to university students.
Limitations and directions for future research
There were several limitations to our review. First, there were a relatively small number of studies, precluding examination of some moderators of change. We could not directly examine whether there were psychological mechanisms of change (e.g. change in metacognitive beliefs) that explained why RNT interventions resulted in reductions in anxiety and depression, as studies typically only reported symptom outcomes. However, given we observed medium reductions in RNT, the interventions did appear to target the proposed process. It is critical future treatment research examines causal reasons for how RNT interventions work, for example, which particular shared mechanisms, e.g. change in meta-cognitions, may be responsible for changes in RNT and symptoms across disorders. Consistent with previous reviews (Breen et al., Citation2023; Egan et al., Citation2022), we echo the need for examination of causal mechanisms underlying the efficacy of interventions. A further limitation was that no studies included measures of psychosis, self-harm, or suicide. Future research should broaden transdiagnostic outcomes beyond anxiety and depression, to include psychosis, self-harm, and suicide. It would also be useful to examine intervention at an earlier age, given most studies were in university students. A limitation to generalisability is most studies were conducted in high-income countries in the global North. More research is needed in low- and middle-income countries (LMICs) and different cultural contexts. This is especially relevant since young people from LMICs underscored the relevance of worry and rumination, but recommended treatments should be tailored across cultural contexts.
Future reviews could consider individual patient data meta-analysis to further understand the efficacy of RNT-specific interventions. Furthermore, many other interventions address transdiagnostic processes. Future research should investigate how efficacious RNT-specific interventions are compared to other transdiagnostic approaches. Future research should also examine which RNT-specific interventions are most efficacious for whom.
A final limitation is that while we decided to take a narrow approach to the definition of what constitutes an RNT intervention, with the rationale to provide a specific review of this mechanism, it is possible that in both our search terms and inclusion/exclusion criteria that some studies which may inform understanding of RNT interventions were missed. For example, one study we did not include and is relevant that showed promising results was a pilot feasibility trial based on the Laval model of Dugas et al. (Citation1998) of intolerance of uncertainty in adults applied to a child and adolescent sample (Perrin et al., Citation2019). Furthermore, there are a range of general CBT programs for anxiety (e.g. Cool Kids; Lyneham et al., Citation2003), which have been demonstrated in a review by Hudson et al. (Citation2015), which combined data from RCTs and uncontrolled trials, to result in a 58% remission rate for GAD in children and adolescents at follow-up. While we decided to take a narrow approach to examine what we considered to be RNT specific interventions to inform the effects of mechanism-specific interventions, future reviews could consider a broader approach and include all CBT interventions, where there is a substantial cognitive component, to determine the efficacy of a wider range of interventions than we included and compare to our findings. Partly, the findings of our review and Bell et al. (Citation2023) were similar, although a novel aspect of our review, besides a more selective and distinct definition of RNT-specific treatments, was reporting on the views of young people with lived experience of mental health challenges who guided our review. Our rationale for a selective definition of RNT interventions was that a distinct definition may help to inform understanding of specific mechanisms of change. However, it is an important question for future reviews to consider whether examining a wider range of interventions is a more informative approach than a specific focus of RNT interventions.
Conclusion
RNT-specific interventions are efficacious in reducing anxiety and depression in young people. Clinicians should consider delivery of RNT interventions for longer than 2 hours. Further research is required to examine the comparative efficacy between self-help and therapist-led interventions. Further research is also required with broader psychological outcomes and across cultural contexts.
Author contributors
SE, JKB, JF, PM, SR, ST, GK and DG designed the study. TC performed the literature search and screening of articles. TB conducted a secondary screening of articles. JF and JKB conducted risk of bias assessment. DG performed the statistical analysis. SE and DG judged final article inclusion. GK judged intervention content for studies. SR and ST led lived experience meetings. SE led the research, funding acquisition, co-ordinated all aspects of the research and wrote the first draft of the manuscript. All authors contributed to and have approved the final article.
Supplemental Material
Download MS Word (33.6 KB)Acknowledgments
We thank our lived experience Youth Advisory Committee for co-producing this review.
Disclosure statement
McEvoy and Ehring co-authored some of the randomised controlled trials of psychological interventions for worry/rumination included in the review.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/16506073.2024.2369936
Additional information
Funding
Notes
1. The inclusion of the search term “perseverative cognition” is an example of how our search strategy was coproduced with lived experience experts.
References
- Andersson, G. (2016). Internet-delivered psychological treatments. Annual Review of Clinical Psychology, 12(1), 157–179. https://doi.org/10.1146/annurev-clinpsy-021815-093006
- Bartoš, F., Maier, M., Quintana, D. S., & Wagenmakers, E. J. (2022). Adjusting for publication bias in JASP and R: Selection models, PET-PEESE, and robust Bayesian meta-analysis. Advances in Methods and Practices in Psychological Science, 5(3), 25152459221109259. https://doi.org/10.1177/25152459221109259
- Bell, I. H., Marx, W., Nguyen, K., Grace, S., Gleeson, J., & Alvarez-Jimenez, M. (2023). The effect of psychological treatment on repetitive negative thinking in youth depression and anxiety: A meta-analysis and meta-regression. Psychological Medicine, 53(1), 6–16. https://doi.org/10.1017/S0033291722003373
- *Bernal-Manrique, K. N., García-Martín, M. B., & Ruiz, F. J. (2020). Effect of acceptance and commitment therapy in improving interpersonal skills in adolescents: A randomized waitlist control trial. Journal of Contextual Behavioral Science, 17, 86–94. https://doi.org/10.1016/j.jcbs.2020.06.008.
- Breen, L. J., Greene, D., Rees, C. S., Black, A., Cawthorne, M., & Egan, S. J. (2023). A co-designed systematic review and meta-analysis of the efficacy of grief interventions for anxiety and depression in young people. Journal of Affective Disorders, 335, 289–297. https://doi.org/10.1016/j.jad.2023.05.032
- Cohen, J. (1992). Statistical power analysis. Current Directions in Psychological Science, 1(3), 98–101. https://doi.org/10.1111/1467-8721.ep10768783
- *Cook, L., Mostazir, M., & Watkins, E. (2019). Reducing stress and preventing depression (RESPOND): Randomized controlled trial of a web-based rumination-focused cognitive behavioral therapy for high-ruminating university students. Journal of Medical Internet Research, 21(5), e11349. https://www.jmir.org/2019/5/e11349/.
- Dalgleish, T., Black, M., Johnston, D., & Bevan, A. (2020). Transdiagnostic approaches to mental health problems: Current status and future directions. Journal of Consulting and Clinical Psychology, 88(3), 179–195. https://doi.org/10.1037/ccp0000482
- Dawkins, J. C., Hasking, P. A., Boyes, M. E., Greene, D., & Passchier, C. (2019). Applying a cognitive-emotional model to nonsuicidal self-injury. Stress and Health, 35(1), 39–48. https://doi.org/10.1002/smi.2837
- De Voogd, E. L., Wiers, R. W., & Salemink, E. (2017). Online visual search attentional bias modification for adolescents with heightened anxiety and depressive symptoms: A randomized controlled trial. Behaviour Research and Therapy, 92, 57–67. https://doi.org/10.1016/j.brat.2017.02.006
- *Dereix-Calonge, I., Ruiz, F. J., Sierra, M. A., Pena-Vargas, A., & Ramirez, E. S. (2019). Acceptance and commitment training focused on repetitive negative thinking for clinical psychology trainees: A randomized controlled trial. Journal of Contextual Behavioral Science, 12, 81–88. https://doi.org/10.1016/j.jcbs.2019.02.005.
- DeVoogd, E. L., De Hullu, E., Burnett Heyes, S., Blackwell, S. E., Wiers, R. W., Salemink, E., & van Wouwe, J. P. (2017). Imagine the bright side of life: A randomized controlled trial of two types of interpretation bias modification procedure targeting adolescent anxiety and depression. PLOS ONE, 12(7), e0181147. https://doi.org/10.1371/journal.pone.0181147
- Dugas, M. J., Gagnon, F., Ladouceur, R., & Freeston, M. H. (1998). Generalized anxiety disorder: A preliminary test of a conceptual model. Behaviour Research and Therapy, 36(2), 215–216. https://doi.org/10.1016/S0005-7967(97)00070-3
- Egan, S. J., Neal, J., Ure, S., Callaghan, T., Ho, P., Shafran, R., & Wade, T. D. (2023). The development of co-designed parent-supported cognitive behaviour therapy for perfectionism in adolescents with eating disorders: Initial feasibility and acceptability. Journal of Eating Disorders, 11(1), 138. https://doi.org/10.1186/s40337-023-00860-6
- Egan, S. J., Rees, C. S., Delalande, J., Greene, D., Fitzallen, G., Brown, S., Webb, M., & Finlay-Jones, A. (2022). A review of self-compassion as an active ingredient in the prevention and treatment of anxiety and depression in young people. Administration and Policy in Mental Health and Mental Health Services Research, 49(3), 385–403. https://doi.org/10.1007/s10488-021-01170-2
- Egger, M., Davey Smith, G., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. British Medical Journal, 315(7109), 629–634. https://doi.org/10.1136/bmj.315.7109.629
- Ehring, T., & Behar, E. (2021). Transdiagnostic view on worrying and other negative mental content. In A. L. Gerlach & A. T. Gloster (Eds.), Generalized anxiety disorder and worrying: A comprehensive handbook for clinicians and researchers (pp. 43–68). Wiley-Blackwell.
- Ehring, T., & Watkins, E. R. (2008). Repetitive negative thinking as a transdiagnostic process. International Journal of Cognitive Therapy, 1(3), 192–205. https://doi.org/10.1521/ijct.2008.1.3.192
- Funk, J., Kopf-Beck, J., Watkins, E., & Ehring, T. (2023). Does an app designed to reduce repetitive negative thinking decrease depression and anxiety in young people? (RETHINK): A randomized controlled prevention trial. Trials, 24, 295. https://doi.org/10.1186/s13063-023-07295-2
- Funk, J., Takano, K., Schumm, H., & Ehring, T. (2022). The bi-factor model of repetitive negative thinking: Common vs. unique factors as predictors of depression and anxiety. Journal of Behavior Therapy and Experimental Psychiatry, 101781. https://doi.org/10.1016/j.jbtep.2022.101781
- *Grol, M., Schwenzfeier, A. K., Stricker, J., Booth, C., Temple McCune, A., Derakshan, N., Hirsch, C., Becker, E., & Fox, E. (2018). The worrying mind in control: An investigation of adaptive working memory training and cognitive bias modification in worry-prone individuals. Behaviour Research and Therapy, 103, 1–11. https://doi.org/10.1016/j.brat.2018.01.005.
- Hartley, S., Haddock, G., Sa, D. V. E., Emsley, R., & Barrowclough, C. (2014). An experience sampling study of worry and rumination in psychosis. Psychological Medicine, 44(8), 1605–1614. https://doi.org/10.1017/S0033291713002080
- Hsieh, H. F., & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. https://doi.org/10.1177/1049732305276687
- Hudson, J. L., Rapee, R. M., Lyneham, H. J., McLellan, L. T., Wuthrich, V. M., & Schniering, C. A. (2015). Comparing outcomes for children with different anxiety disorders following cognitive behavioral therapy. Behaviour Research and Therapy, 72(9), 30–37. https://doi.org/10.1016/j.brat.2015.06.007
- *Jacobs, R. H., Watkins, E. R., Peters, A. T., Feldhaus, C. G., Barba, A., Carbray, J., & Langenecker, S. A. (2016). Targeting ruminative thinking in adolescents at risk for depressive relapse: Rumination-focused cognitive behavior therapy in a pilot randomized controlled trial with resting state fMRI. PLOS ONE, 11(11), e0163952. https://doi.org/10.1371/journal.pone.0163952.
- Jeffreys, H. (1961). Theory of probablity (3rd ed.). Oxford University Press.
- Joubert, A. E., Moulds, M. L., Werner-Seidler, A., Sharrock, M., Popovic, B., & Newby, J. M. (2022). Understanding the experience of rumination and worry: A descriptive qualitative survey study. British Journal of Clinical Psychology, 61(4), 929–946. https://doi.org/10.1111/bjc.12367
- Klauer, K. J. (Ed.). (2001). Handbuch kognitives training [Handbook of cognitive training]. Hogrefe.
- Kocovski, N. L., Fleming, J. E., Blackie, R. A., MacKenzie, M. B., & Rose, A. L. (2019). Self-help for social anxiety: Randomized controlled trial comparing a mindfulness and acceptance-based approach with a control group. Behavior Therapy, 50(4), 696–709. https://doi.org/10.1016/j.beth.2018.10.007
- *LaFreniere, L. S., & Newman, M. G. (2016). A brief ecological momentary intervention for generalized anxiety disorder: A randomized controlled trial of the Worry Outcome Journal. Depression and Anxiety, 33(9), 829–839. https://doi.org/10.1002/da.22507.
- Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics Bulletin, 33(1), 159–174. https://doi.org/10.2307/2529310
- Law, K. C., & Tucker, R. P. (2018). Repetitive negative thinking and suicide: A burgeoning literature with need for further exploration. Current Opinion in Psychology, 22, 68–72. https://doi.org/10.1016/j.copsyc.2017.08.027
- Lyneham, H. J., Abbott, M. J., Wignall, A., & Rapee, R. M. (2003). The cool kids anxiety treatment program. MUARU, Macquarie University.
- Lytle, R. A., Hazlett-Stevens, H., & Borkovec, T. D. (2002). Efficacy of eye movement desensitization in the treatment of cognitive intrusions related to a past stressful event. Journal of Anxiety Disorders, 16(3), 273–288. https://doi.org/10.1016/S0887-6185(02)00099-3
- Maier, M., Bartoš, F., & Wagenmakers, E.-J. (2023). Robust Bayesian meta-analysis: Addressing publication bias with model-averaging. Psychological Methods, 28(1), 107–122. https://doi.org/10.1037/met0000405
- *McDermott, K. A., & Cougle, J. R. (2021). Disengagement training for the treatment of pathological worry: A preliminary test. Behavior Therapy, 52(1), 86–98. https://doi.org/10.1016/j.beth.2020.02.005.
- McEvoy, P. M., Erceg-Hurn, D. M., Anderson, R. A., Campbell, B. N. C., Swan, A., Saulsman, L. M., Summers, M., & Nathan, P. R. (2015). Group meta-cognitive therapy for repetitive negative thinking in primary and non-primary generalized anxiety disorder: An effectiveness trial. Journal of Affective Disorders, 175(1), 124–132. https://doi.org/10.1016/j.jad.2014.12.046
- *McEvoy, P. M., Graville, R., Hayes, S., Kane, R. T., & Foster, J. K. (2017). Mechanisms of change during attention training and mindfulness in high trait-anxious individuals: A randomized controlled study. Behavior Therapy, 48(5), 678–694. https://doi.org/10.1016/j.beth.2017.04.001.
- McEvoy, P. M., Hyett, M. P., Ehring, T., Johnson, S. L., Samtani, S., Anderson, R., & Moulds, M. L. (2018). Transdiagnostic assessment of repetitive negative thinking and responses to positive affect: Structure and predictive utility for depression, anxiety, and mania symptoms. Journal of Affective Disorders, 232, 375–384. https://doi.org/10.1016/j.jad.2018.02.072
- McEvoy, P. M., Thibodeau, M. A., & Asmundson, G. J. G. (2014). Trait repetitive negative thinking: A brief transdiagnostic assessment. Journal of Experimental Psychopathology, 3(3), 382–398. https://doi.org/10.5127/jep.037813
- McIndoo, C. C., File, A. A., Preddy, T., Clark, C. G., & Hopko, D. R. (2016). Mindfulness-based therapy and behavioral activation: A randomized controlled trial with depressed college students. Behaviour Research & Therapy, 77, 118–128. https://doi.org/10.1016/j.brat.2015.12.012
- McIntosh, C., & Crino, R. (2013). Towards a unified worry exposure protocol for generalised anxiety disorder: A pilot study. Behaviour Change, 30(3), 210–225. https://doi.org/10.1017/bec.2013.19
- *Modini, M., & Abbott, M. J. (2017). Negative rumination in social anxiety: A randomised trial investigating the effects of a brief intervention on cognitive processes before, during and after a social situation. Journal of Behavior Therapy and Experimental Psychiatry, 55, 73–80. https://doi.org/10.1016/j.jbtep.2016.12.002.
- *Modini, M., & Abbott, M. J. (2018). Banning pre-event rumination in social anxiety: A preliminary randomized trial. Journal of Behavior Therapy and Experimental Psychiatry, 61, 72–79. https://doi.org/10.1016/j.jbtep.2018.06.009.
- *Mogoaşe, C., Brăilean, A., & David, D. (2013). Can concreteness training alone reduce depressive symptoms? A randomized pilot study using an internet-delivered protocol. Cognitive Therapy and Research, 37(4), 704–712. https://doi.org/10.1007/s10608-012-9514-z.
- Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & PRISMA group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ, 21(339) b2535. https://doi.org/10.1136/bmj.b2535
- Norton, M. J. (2021). Co-production within child and adolescent mental health: A systematic review. International Journal of Environmental Research and Public Health, 18(22), 11897. https://doi.org/10.3390/ijerph182211897
- O’Mara, M., Greene, D., Watson, H. J., Shafran, R., Kenworthy, I., Cresswell, C., & Egan, S. J. (2023). The efficacy of randomised controlled trials of guided and unguided self-help interventions for the prevention and treatment of eating disorders in young people: A systematic review and preliminary meta-analysis. Journal of Behavior Therapy and Experimental Psychiatry, 78, 101777. https://doi.org/10.1016/j.jbtep.2022.101777
- Oliver, J., Smith, P., & Leigh, E. (2015). ‘All these negative thoughts come flooding in’: How young people with depression describe their experience of rumination. The Cognitive Behaviour Therapist, 8, e15. https://doi.org/10.1017/S1754470X15000306
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hrobjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., & Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372(71). http://dx.doi.org/10.1136/bmj.n71
- *Pan, D., Hoid, D., Gu, R., & Li, X. (2020). Emotional working memory training reduces rumination and alters the EEG microstate in anxious individuals. Neuro Image Clinical, 28, 102488. https://doi.org/10.1016/j.nicl.2020.102488
- Perrin, S., Bevan, D., Payne, S., & Bolton, D. (2019). GAD-specific cognitive behavioral treatment for children and adolescents: A pilot randomized controlled trial. Cognitive Therapy and Research, 43(6), 1051–1064. https://doi.org/10.1007/s10608-019-10020-3
- *Roberts, H., Mostazir, M., Moberly, N. J., Watkins, E. R., & Adlam, A. L. (2021). Working memory updating training reduces state repetitive negative thinking: Proof-of-concept for a novel cognitive control training. Behaviour Research and Therapy, 142, 103871. https://doi.org/10.1016/j.brat.2021.103871.
- Sass, S. M., Evans, T. C., Xiong, K., Mirghassemi, F., & Tran, H. (2017). Attention training to pleasant stimuli in anxiety. Biological Psychology, 122, 80–92. https://doi.org/10.1016/j.biopsycho.2016.03.003
- Schleider, J. L. (2023). The fundamental need for lived experience perspectives in developing and evaluating psychotherapies. Journal of Consulting and Clinical Psychology, 91(3), 119–121. https://doi.org/10.1037/ccp0000798
- Schouten, S. E., Kip, H., Dekkers, T., Deenik, J., Beerlage de Jong, N., Ludden, G. D., & Kelders, S. M. (2022). Best-practices for co-design processes involving people with severe mental illness for eMental health interventions: A qualitative multi-method approach. Design for Health, 6(3), 316–344. https://doi.org/10.1080/24735132.2022.2145814
- *Skodzik, T., Adelt, M. H., Nossek, V. A., Kuck, S. T., & Ehring, T. (2018). Does a novel training in mental imagery reduce pathological worry? Behaviour Research and Therapy, 109, 56–67. https://doi.org/10.1016/j.brat.2018.07.005.
- Sloan, E., Moulding, R., Weiner, C., Dowling, R. M., & Hall, K. (2021). A qualitative examination of the relationship between rumination, distress, and dysregulated behaviors in vulnerable young people. Psychology and Psychotherapy, 94(2), 322–340. https://doi.org/10.1111/papt.12297
- Stade, E. C., & Ruscio, A. M. (2023). A meta-analysis of the relationship between worry and rumination. Clinical Psychological Science, 11(3), 552–573. https://doi.org/10.1177/21677026221131309
- Sterne, J. A., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., Cates, C. J., Cheng, H.-Y., Corbett, M. S., Eldridge, S. M., Emberson, J. R., Hernán, M. A., Hopewell, S., Hróbjartsson, A., Junqueira, D. R., Jüni, P., Kirkham, J. J., Lasserson, T., Li, T., McAleenan, A., Reeves, B. C., Shepperd, S., Shrier, I., Stewart, L. A., Tilling, K., White, I. R., Whiting, P. F., & Higgins, J. P. T. (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ: British Medical Journal, 366, l4898. https://doi.org/10.1136/bmj.l4898
- Sunkel, C., & Sartor, C. (2022). Perspectives: Involving persons with lived experience of mental health conditions in service delivery, development and leadership. BJPsych Bulletin, 46(3), 160–164. https://doi.org/10.1192/bjb.2021.51
- Teismann, T., Forkmann, T., Michalak, J., & Brailovskaia, J. (2021). Repetitive negative thinking about suicide: Associations with lifetime suicide attempts. Clinical Psychology in Europe, 3(3), e5579. https://doi.org/10.32872/cpe.5579
- Teng, M. H., Hou, Y. M., Chang, S. H., & Cheng, H. J. (2019). Home-delivered attention bias modification training via smartphone to improve attention control in sub-clinical generalized anxiety disorder: A randomized, controlled multi-session experiment. Journal of Affective Disorders, 246, 444–451. https://doi.org/10.1016/j.jad.2018.12.118
- Topper, M., Emmelkamp, P. M. G., & Ehring, T. (2010). Improving prevention of depression and anxiety disorders: Repetitive negative thinking as a promising target. Applied and Preventive Psychology, 14(1–4), 57–71.
- *Topper, M., Emmelkamp, P. M., Watkins, E., & Ehring, T. (2017). Prevention of anxiety disorders and depression by targeting excessive worry and rumination in adolescents and young adults: A randomized controlled trial. Behaviour Research and Therapy, 90, 123–136. https://doi.org/10.1016/j.brat.2016.12.015.
- van Doorn, J., van den Bergh, D., Böhm, U., Dablander, F., Derks, K., Draws, T., Etz, A., Evans, N. J., Gronau, Q. F., Haaf, J. M., Hinne, M., Kucharsky, S., Ly, A., Marsmen, M., Matzke, D., Komarlu Narenda Gupta, A., Sarafoglou, A., Stefan, A., Voelkel, J. G., & Wagenmakers, E. J. (2021). The JASP guidelines for conducting and reporting a Bayesian analysis. Theoretical Review, 28, 813–826. https://doi.org/10.3758/s13423-020-01798-5
- Vrijsen, J. N., Dainer-Best, J., Witcraft, S. M., Papini, S., Hertel, P., Beevers, C. G., Becker, E. S., & Smits, J. A. (2019). Effect of cognitive bias modification-memory on depressive symptoms and autobiographical memory bias: Two independent studies in high-ruminating and dysphoric samples. Cognition and Emotion, 33(2), 288–304. https://doi.org/10.1080/02699931.2018.1450225
- Watkins, E. R. (2016). Rumination-focused cognitive-behavioral therapy for depression. Guilford.
- Watson, H. J., Joyce, T., French, E., Willan, V., Kane, R. T., Tanner-Smith, E. E., McCormack, J., Dawkins, H., Hoiles, K. J., & Egan, S. J. (2016). Prevention of eating disorders: A systematic review of randomized controlled trials. The International Journal of Eating Disorders, 49, 833–862. https://doi.org/10.1002/eat.22577
- Wells, A. (2011). Metacognitive therapy for anxiety and depression. Guilford.
- Yang, W., Zhang, J. X., Ding, Z., & Xiao, L. (2016). Attention bias modification treatment for adolescents with major depression: A randomized controlled trial. The Journal of the American Academy of Child & Adolescent Psychiatry, 55(3), 208–218. https://doi.org/10.1016/j.jaac.2015.12.005
- Zagaria, A., Ballesio, A., Vacca, M., & Lombardo, C. (2023). Repetitive negative thinking as a central node between psychopathological domains: A network analysis. International Journal of Cognitive Therapy, 16(2), 143–160. https://doi.org/10.1007/s41811-023-00162-4
- *Zemestani, M., Davoodi, I., Honarmand, M. M., Zargar, Y., & Ottaviani, C. (2016). Comparative effects of group metacognitive therapy versus behavioural activation in moderately depressed students. Journal of Mental Health, 25(6), 479–485. https://doi.org/10.3109/09638237.2015.1057326