ABSTRACT
Between-session work (BSW) acts as the vehicle to translate skills learnt in therapy sessions into adaptive changes in everyday life, a key goal in Cognitive Behavioural Therapies (CBT). Despite a well-established relationship between engagement with BSW and enhanced treatment outcomes, difficulties completing between-session tasks are common and factors affecting patient engagement with BSW are poorly understood. This mixed-methods systematic review and “best fit” framework synthesis explored predictors of engagement with BSW in CBT-based interventions. Comprehensive searches were conducted across five databases, identifying 59 eligible studies. This combined theory and empirical evidence approach depicted ten predictor themes related to between-session engagement, spanning individual, relational and contextual concepts. While ambiguous findings were generated by existing evidence, several factors emerged as relatively consistent predictors of engagement with BSW: positive patient beliefs regarding BSW and treatment such as perceived helpfulness, and practitioner competency in planning and reviewing BSW, including providing a rationale and addressing difficulties were associated with greater engagement. Conversely, patient in-session resistance, including counter change talk, was an indicator of disengagement between-sessions. The impact of patient symptomology, sociocultural environment, practitioner beliefs and the therapeutic relationship is unclear. The conceptual model presented offers a testable framework for researchers and a guideline for practitioners.
Introduction
Common mental health problems such as depression or anxiety are a leading cause of disease burden globally, negatively impacting individuals and society (Christensen et al., Citation2020; Collaborators, Citation2022). CBT is the recommended first-line treatment across disorders with extensive empirical support (David et al., Citation2018). Although CBT is an umbrella term for a family of therapies targeting dysfunctional thinking and maladaptive behaviour, a distinct commonality across treatments is the inclusion of between-session work (BSW).
BSW can be broadly defined as “activities that enable the client to gather information and generalise new learning from the therapeutic setting to the everyday life situations in which their problems occur” (Ryum et al., Citation2023, p. 2). Common examples include reading psychoeducational materials, self-monitoring activities such as recording negative automatic thoughts and implementing techniques such as exposure (Fehm & Mrose, Citation2008). Previous research on BSW in CBT has explored its relationship with treatment outcomes and several meta-analyses have consistently evidenced the use of, and engagement with BSW as a predictor of symptom improvement (Kazantzis et al., Citation2000, Citation2010, Citation2016; Mausbach et al., Citation2010; Wheaton & Chen, Citation2021). These findings hold when tested across different patient populations, clinical disorders, and types of between-session activities (Kazantzis, Citation2021). Disengagement between sessions has also been identified as an indicator of premature treatment termination (Cammin-Nowak et al., Citation2013).
Diverse measurement of BSW is apparent across studies, perhaps due to varied conceptualisation of between-session engagement (Kazantzis & Dattilio, Citation2010). Measures have predominantly centred however on assessment of the quantity of BSW completed, including the number of practices undertaken or amount of time spent on activities. Comparatively less studies have measured the quality of engagement such as skills acquired or cognitive change. Despite its identified value, lack of engagement between-sessions is reported as a common issue by CBT practitioners (Kazantzis & Shinkfield, Citation2007). When assessed by independent observers, Haller and Watzke (Citation2021) found difficulties completing BSW within 75% of the telephone-based CBT sessions. Previous research has explored factors which may influence patient engagement between-session (Dobson, Citation2021; Kazantzis & Shinkfield, Citation2007), however although a wide array of factors have been studied, findings remain inconclusive.
In view of the robust documented relationship between engagement with BSW and treatment success, it is concerning that predictors of between-session engagement are poorly understood. To our knowledge, no previous systematic review has synthesised predictors of engagement with CBT BSW across common mental health problems. A systematic review by Wheaton and Chen (Citation2021) explored the importance of BSW in exposure and response prevention (ERP) for obsessive—compulsive disorder (OCD), linking some factors to greater between-session engagement: OCD features (i.e. fewer hoarding symptoms and behavourial avoidance), patient beliefs (i.e. positive treatment expectancy) and therapeutic alliance (i.e. agreement with practitioner on therapy tasks). These findings however are specific to OCD/ERP and may not be representative of other disorders. Ryum et al. (Citation2023) reviewed the impacts of practitioner integration of BSW in psychotherapy, exploring outcomes such as symptom change, dropout, and between-session engagement. The findings provide us with some indication of practitioner behaviours which may promote BSW such as flexibility and collaboration in the design, planning and review of between-session tasks, however does not explore wider factors related to the practitioner (e.g. practitioner beliefs), or patient (e.g. problem severity), environmental (e.g. social support), task-related (e.g. perceived task difficultly) and intervention (e.g. intensity of practitioner support) characteristics. Ryum et al. (Citation2023) was also not specific to CBT-based interventions and was restricted to adult populations. Holistic identification of the predictors of engagement with BSW would enable targeted intervention, enhancing between-session engagement and thus treatment outcomes. The primary review objective was to:
• Explore predictors of engagement with BSW in CBT-based interventions.
A secondary objective was to:
• Explore variation in the engagement rates with BSW reported across studies and how these are measured.
Methods
Review reporting
The protocol for this mixed-methods review was prospectively registered with PROSPERO (CRD42021251551) guided by the Preferred Reporting Items for Systematic Review and Meta-analysis Protocols (PRISMA-P) statement (Moher et al., Citation2015). Since registration, several minor amendments were made to the protocol, detailed in Supplementary Material (S1). Reporting of methods and findings adheres to the PRISMA statement (Page et al., Citation2021).
Search strategy and eligibility
The search for primary studies used keywords and MeSH terms related to concepts of BSW and CBT. CBT terms built upon those used in a previous review (Fordham et al., Citation2021). Searches were undertaken from inception to 7th June 2023 on MEDLINE (OVID interface), Embase (OVID interface), PsycINFO (OVID interface), CINAHL (EBSCO interface) and Dissertations & Theses Global (ProQuest interface). No limits were applied to database searches. A specialist librarian from the University of Manchester was consulted during search strategy development and reviewed the finalised search strategies for all databases (S2). Eligibility criteria for primary studies are presented in . Reference lists and bibliographies of all shortlisted full texts were searched for relevant materials and forward citation index tracking of these articles was conducted. The reference lists of identified relevant systematic reviews were also searched for eligible articles.
Table 1. Eligibility criteria for primary studies.
Data management and screening
Search results were independently imported into the reference management software package EndNote version X9 and duplicates removed. References were then imported into the systematic review management tool Covidence (https://www.covidence.org/) whereby further duplicates not identified in Endnote were removed. Titles and abstracts of records retrieved, then full text articles, were screened independently by two reviewers (MB with either PB, AB, JC or KL). In instances where further information was required, the author was contacted. Disagreements were resolved by discussion across the review team.
Data extraction
Data extraction was performed in Microsoft Excel using structured tables aligned with recommendations from the Centre for Reviews and Dissemination (University of York, Citation2009) and the Joanna Briggs Institute (JBI) (Moola et al., Citation2024). Forms were piloted independently by two reviewers (MB, KL) using three included studies (one quantitative, one qualitative and one mixed-methods) to ensure all relevant information was captured. The first author (MB) extracted data from each included article, uncertainties were discussed with the review team. No assumptions regarding missing data were made and these were declared as “not reported” in the extraction table if data could not be located. When the same study or sample was reported in multiple articles, data was extracted from the most complete source.
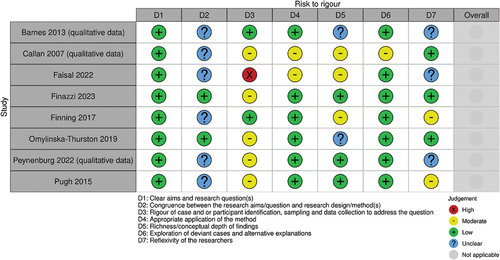
Quality assessment
Given the diversity of study designs across included studies, the JBI suite of checklists (https://jbi.global/critical-appraisal-tools), matched to study design, were used to assess six selected risk of bias domains in quantitative studies and seven risk to rigour domains in qualitative studies. Modelled from the Quality In Prognosis Studies (QUIPS) tool (Hayden et al., Citation2013), the domains prioritised for quantitative studies included 1) Selection bias, 2) Attrition bias, 3) Predictor measurement bias, 4) Outcome measurement bias, 5) Confounding bias and 6) Statistical analysis and reporting bias. Guided by the Cochrane Handbook (Noyes et al., Citation2022), domains assessed for included qualitative studies focused on the assessment of (1) Clear aims and research question(s), (2) Congruence between the research aims/question and research design/methodology/method(s), (3) Rigour of case and/or participant identification, sampling and data collection to address the question, (4) Appropriate application of the method, (5) Richness/conceptual depth of findings, (6) Exploration of deviant cases and alternative explanations and (7) Reflexivity of the researchers. The first author independently assessed all included studies for risk to bias or rigour with a second reviewer (EV) independently assessing a 25% sample (Cohen’s kappa κ = 0.725 (95% CI, 0.592 to 0.858), p < 0.001). Disagreements were resolved by a third independent reviewer (AB). For instance, in cases where discrepancies arose within a specific domain, such as one reviewer assessing a study with a moderate risk of outcome measurement bias while the other deemed it as low risk, AB independently determined the consensus judgment. Studies were not excluded due to risk of bias/rigour assessments, instead methodological limitations present across included studies are discussed in relation to the potential impacts on review findings.
Data synthesis
“Best fit” framework synthesis was chosen to accommodate quantitative and qualitative data and integrate relevant theory alongside eligible evidence (Carroll et al., Citation2013). “Best fit” synthesis involves using concepts from an existing conceptual model, theory or framework relevant to the health behaviour of interest as an a priori coding framework for retrieved primary studies. A novel theory-driven and evidence-based conceptual model is produced to describe or explain patient health behaviour and decision-making with the view of informing future research, clinical practice and service policy (Carroll et al., Citation2013).
To identify conceptual frameworks relevant to engagement with BSW in CBT-based interventions, we ran a second independent systematic search across MEDLINE, Embase, PsycINFO and CINAHL simultaneous to the primary studies search (see Figure 1 in Carroll et al., Citation2013 for process). Search strategies were constructed using the BeHEMoTH theory search approach (Booth & Carroll, Citation2015) (S3). Within this search for relevant frameworks, literature detailing theory relating to engagement with BSW in CBT was eligible if the proposed theoretical concepts were empirically tested and/or prompted by established classic behaviour change theories i.e. those widely used and subjected to external and internal validation across multiple settings and behaviours (Nilsen, Citation2015). Screening procedures followed the same process as the primary studies searches (see S4 for PRISMA flow diagram depicting model search).
Searches identified two frameworks which met the inclusion criteria (Kazantzis & Miller, Citation2022; Kazantzis et al., Citation2005). Common exclusion reasons for further reports included no inclusion of a conceptual framework (n = 60) or the framework presented was not in the context of engagement with BSW in CBT (n = 14). The combination of the two models was favoured over arbitrary selection of one model and sought to offer a more comprehensive framework overall (see S5 for a priori coding framework). As per previous examples (Carroll et al., Citation2013), the constituent concepts of both models were deconstructed using thematic analysis (Braun & Clarke, Citation2006). Theme definitions were generated from the original model reports, assisting the coding of the primary research data. New themes for primary study findings which did not map to the framework were generated and aspects of the a priori framework where there was neither corroborating nor opposing evidence remained in the final conceptual model to highlight knowledge gaps in the evidence base (Carroll et al., Citation2013; Russo et al., Citation2021). Iterations of the developing model were shared amongst the review team to seek consensus at each step of the process.
Meta-analyses of quantitative data could not be conducted due to clinical, methodological, and statistical heterogeneity across studies which made even exploratory meta-analyses involving arbitrary selection of specific study conditions unviable. Instead, quantitative findings were tabulated using a vote counting method based on direction of effect i.e. whether the predictor was found to have a positive or negative effect on engagement with BSW (McKenzie & Brennan, Citation2023). Direction of effect was extracted regardless of statistical significance to not discount possibly important effects deemed non-significant due to insufficient statistical power (McKenzie & Brennan, Citation2023) i.e. a non-significant effect with a positive direction was considered a positive effect. Qualitative data integrated into the model are reported in a summary table.
When the impact of the same predictor was examined via multiple statistical tests, only the most rigorous is reported in the synthesis, ordered as: multivariate analyses of predictor effects, univariate analyses, correlation analyses and difference in means.
Patient and public involvement (PPI)
An advisory panel of four individuals selected due to their experience of receiving CBT for anxiety/depression contributed to interpretation of review findings. Members were recruited with the aid of two PPI coordinators who shared opportunity forms with their networks’, interested applicants were screened for their experience of receiving CBT treatment and were recruited on a first come, first serve basis. While the content of the review findings did not change, discussions enabled the review team to highlight key areas of enquiry in an ongoing piece of research further interrogating the review findings. Members were also asked to contribute ideas regarding the dissemination of findings, identifying key strategies to optimally target stakeholder audiences.
Results
Study characteristics
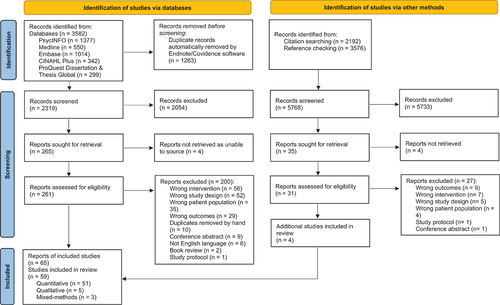
A total of 59 primary research studies were included in the review (see for PRISMA flow diagram depicting primary studies search). Study characteristics are presented in . The majority of studies were quantitative (n = 51; 86%), from the United States of America (USA) (n = 35; 59%) involving adult populations (n = 52; 88%). Sample sizes ranged from 7 to 521. Most quantitative studies employed observational study designs or included secondary analyses of RCT data, four were primary RCTs (Olatunji et al., Citation2015; Schneider, Citation2019; Simpson, Zuckoff, et al., Citation2010; Westra et al., Citation2009). Only two qualitative studies explicitly reported their applied methodology (Finazzi et al., Citation2023; Omylinska‐Thurston et al., Citation2019), data collection methods included semi-structured interviews (Barnes et al., Citation2013; Callan, Citation2007; Faisal & Masood, Citation2022; Finazzi et al., Citation2023; Finning et al., Citation2017; Omylinska‐Thurston et al., Citation2019) and open-ended questionnaires (Peynenburg et al., Citation2022; Pugh et al., Citation2015). Complete demographic information concerning either the mean sample age, gender or ethnicity proportion was not reported in 27 studies. Where these characteristics were reported, samples were predominately female and of White ethnicity (n = 26; 81%).
Table 2. Included studies characteristics.
Quality assessment
A summary of the risk of bias and risk to rigour judgments for included studies are presented in .
Figure 2. Risk of bias judgments.Footnote2
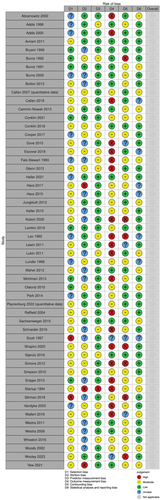
Risk of bias
Across quantitative studies the main concerns centred around selection bias, attrition bias and outcome measurement bias. Recruitment methods to identify samples within some studies included self-selecting participants or participants recruited via “gatekeepers” such as general practitioners. Some studies included only participants who had responded to BSW or had completed treatment in their analyses, with only some listing reasons for attrition or detailing differences between completers and non-completers. Only 30% of studies measuring BSW used one of three validated measures of engagement with BSW; the Homework Compliance Scale (HCS) (Primakoff et al., Citation1986), the Homework Rating Scale-Revised (HRS-II) (Kazantzis et al., Citation2005) and the Patient Exposure and Response Prevention Adherence Scale (PEAS) (Simpson, Maher, et al., Citation2010) for OCD samples.Footnote1
Validated tools were more frequently applied for predictor measurement. However, only 15 quantitative study designs (28%) pre-specified anticipated predictor effects for all examined predictors within their study and studies rarely referenced underpinning theory prompting the selection of predictor variables. Exploration of predictors ought to be theory or evidence driven to generate confirmatory results, enabling authors to state a priori hypotheses, contrasting to more ambiguous exploratory post hoc testing of predictors (Sun et al., Citation2012). Issues with incomplete reporting of predictor effects when results were non-significant was also common i.e. data from which direction of effect could be derived was not reported, impeding data extraction and interpretation. The extent to which confounding variables were accounted for in study design and/or analysis varied across studies.
Risk to rigour
Included qualitative designs detailed clear aims and research questions, yet there were uncertainties regarding the congruence between aims and methodologies as most did not declare the chosen qualitative approach. Further issues included an absence of reporting regarding how data saturation was determined.
Synthesis of findings
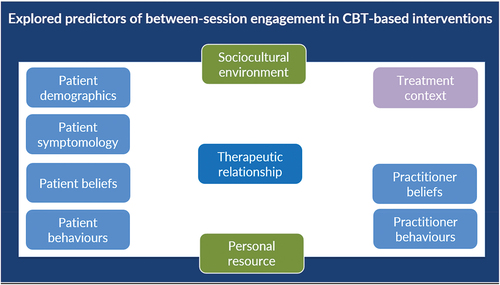
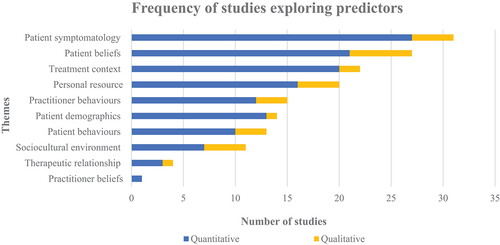
Conceptual model themes are represented in . Overall, data aligned adequately with themes derived from the theoretical frameworks. With the exception of the a priori theme—practitioner behaviours, evidence mapping most intimately to the a priori framework was predominantly qualitative and clustered around patient beliefs regarding BSW. Additions to the model (S6) were required largely for quantitative studies which most frequently focused on the influence of patient symptomology (see ). S7 displays quantitative data based on direction of effect. S8 reports qualitative findings across themes.
Model themes
Patient demographics
No clear associations to engagement with BSW were identified for gender, marital status, age, or education though potential trends suggesting greater socioeconomic status (Callan et al., Citation2019; Lukin, Citation2011; Maher et al., Citation2012; Woods et al., Citation2002) and White ethnicity possibly predicting greater between-session engagement were evident (Callan, Citation2007; Jungbluth & Shirk, Citation2013; Stirman et al., Citation2018; Woods et al., Citation2002) (see Callan et al. (Citation2019) STAR-D study group for exception).
Patient symptomology
Depression severity was the most explored predictor, including findings from 18 quantitative studies and four qualitative designs. Across quantitative studies, there was an almost even split amongst positive (n = 8) (Bryant et al., Citation1999, [pre-treatment depression severity]; Bryant et al., Citation1999 [depression severity at the time of the assignment]; Addis & Jacobson, Citation2000; Burns & Spangler, Citation2000; Callan, Citation2007, Cooper et al., Citation2017; Lukin, Citation2011; Stirman et al., Citation2018) and negative effects (n = 9) (Burns & Nolen-Hoeksema, Citation1992; Callan et al., Citation2019; Haller & Watzke, Citation2021; Jungbluth & Shirk, Citation2013; Maher et al., Citation2012; Mohlman, Citation2013; Park et al., Citation2014; Scott & Stradling, Citation1997; VanDyke, Citation2002). Direction of effect was uncertain for three analyses due to: insufficient reporting of non-significant result (Abramowitz et al., Citation2002), mixed direction of effect across included treatment groups (Callan et al., Citation2019) and mixed direction of effect across measurement tools accessing depression severity (Wallert et al., Citation2018). Qualitative studies corroborated depression as a barrier to BSW (Barnes et al., Citation2013; Callan, Citation2007; Finning et al., Citation2017; Omylinska‐Thurston et al., Citation2019) and indicated that the duration of depression may also be important, with longer durations hindering between-session engagement (Callan, Citation2007). Quantitative findings regarding duration were inconclusive (Bryant et al., Citation1999; Callan, Citation2007; Callan et al., Citation2019).
Anxiety related disorders were less frequently interrogated as predictive of between-session engagement; while OCD severity displayed a possible negative association to BSW (three available analyses, all depicting negative associations: Maher et al., Citation2012; Park et al., Citation2014; Wheaton et al., Citation2016), severity of generalised anxiety (Lamkin et al., Citation2019; Mohlman, Citation2013; Omylinska‐Thurston et al., Citation2019; Schneider, Citation2019; Wallert et al., Citation2018; Westra, Citation2011; Woods et al., Citation2002) and post-traumatic stress disorder (Keller, Citation2015; Scott & Stradling, Citation1997; Stirman et al., Citation2018; Woolley et al., Citation2023) produced inconsistent effects.
Quantitative studies testing the presence (Abramowitz et al., Citation2002; Callan et al., Citation2019; Keller, Citation2015; Lukin, Citation2011; Woods, Citation2002), number (Callan et al., Citation2019; Lukin, Citation2011; Maher et al., Citation2012) or severity of comorbidities (Callan et al., Citation2019) denote a slight positive relationship to between-session engagement (6 out of 10 obtainable analyses) tentatively suggesting greater engagement. Predictors mainly focused on psychological comorbidities, though Callan et al. (Citation2019) examined the influence of physical health, finding no effect. Qualitative data contradicts this overall positive trend, noting how another clinical problem interfered with BSW completion (Callan, Citation2007). Similarly, studies exploring the effect of the global severity of psychological difficulties generally found those more functionally impaired were less engaged between sessions (Callan et al., Citation2019; Lukin, Citation2011; Maher et al., Citation2012; VanDyke, Citation2002; Woods et al., Citation2002).
Due to scant evidence, inferences cannot be made regarding the effect of specific symptoms (Callan, Citation2007; Callan et al., Citation2019; Fals-Stewart & Lucente, Citation1993; Keller, Citation2015; Lamkin et al., Citation2019; Lukin, Citation2011; Maher et al., Citation2012; Park et al., Citation2014; Stirman et al., Citation2018; Wallert et al., Citation2018; Woods et al., Citation2002) or diagnoses as predictors of between-session engagement (Callan et al., Citation2019; Conklin et al., Citation2021; Woods et al., Citation2002).
Patient beliefs
Patient beliefs about self and coping/Patient beliefs about others
Quantitative evidence pertaining to these sub-themes were investigated only by single studies limiting meaningful interpretation. Qualitative evidence expressed fear of failure and lack of confidence as a barrier to BSW (Callan, Citation2007; Button, Citation2013; Finning et al., Citation2017; Omylinska‐Thurston et al., Citation2019).
Patient beliefs about BSW
Findings signified how positive beliefs regarding BSW facilitated between-session engagement while negative beliefs acted as a barrier to completion; for example, the perceived helpfulness (Cooper et al., Citation2017; Peynenburg et al., Citation2022; VanDyke, Citation2002; Woolley et al., Citation2023) or difficulty of tasks (Barnes et al., Citation2013; Callan, Citation2007; Finning et al., Citation2017; Omylinska‐Thurston et al., Citation2019; Peynenburg et al., Citation2022; Pugh et al., Citation2015). BSW which wasn’t tailored around specific needs or collaboratively designed was also harder to complete (Callan, Citation2007).
Negative consequences of engaging with BSW were described such as painful emotions (Callan, Citation2007; Finning et al., Citation2017; Pugh, Citation2015) and reduced self-efficacy (Callan, Citation2007; Omylinska‐Thurston et al., Citation2019). Noted in Omylinska‐Thurston et al. (Citation2019), experiencing difficulties with BSW fuelled further negative thoughts and feelings, creating a negative feedback loop, counteracting change, and leading to further disengagement. Conversely, patients disclosed positive consequences of engagement, including improvements in mood, empowerment over difficulties and a sense of progress in therapy (Finning et al., Citation2017; Pugh et al., Citation2015; Yew et al., Citation2021).
Patient beliefs about treatment
Overall, positive beliefs regarding treatment such as acceptance of the treatment rationale and commitment to CBT predicted greater between-session engagement (Abramowitz et al., Citation2002; Addis & Jacobson, Citation2000; Callan, Citation2007; Glenn et al., Citation2013; Maher et al., Citation2012; VanDyke, Citation2002). However, Snippe et al. (Citation2015) reported a negative relationship between treatment expectancy and between-session engagement, while Lewin et al. (Citation2011) and Lukin (Citation2011) observed mixed effects of treatment expectancy on engagement, varying across raters i.e. patient, parent, and practitioner.
Patient behaviours
In-session patient resistance emerged as a consistent predictor of disengagement between-sessions (Button, Citation2013; Hara et al., Citation2015; Jungbluth & Shirk, Citation2013; Sijercic et al., Citation2016 [opposition counter change talk]; Westra, Citation2011) with the exception of Sijercic et al. (Citation2016) [ambivalent counter change talk], where effect direction was mixed across patient and practitioner ratings of between-session engagement. Conversely, positive change talk (Button, Citation2013), in-session compliance (Abramowitz et al., Citation2002), early between-session engagement (Lax et al., Citation1992) and use of positive coping strategies pre-treatment fostered BSW completion. Several behaviours which hampered between-session engagement were reported, including procrastination and disorganisation (Callan, Citation2007; Omylinska‐Thurston et al., Citation2019; Peynenburg et al., Citation2022).
Practitioner beliefs
This was the least endorsed theme with only one corresponding finding; practitioner treatment expectancy, which was found to positively correlate with child between-session engagement for ERP therapy (Lewin et al., Citation2011).
Practitioner behaviours
General therapeutic and interpersonal skills
General practitioner skills such as agenda setting and application of cognitive-behavioural techniques elicited positive effects to BSW engagement, indicating greater practitioner competence facilitates greater patient response between sessions (Bryant et al., Citation1999; Callan, Citation2007). The only practitioner interpersonal skill examined as a predictor of between-session engagement was empathy; explored by two studies, both evidencing positive associations (Burns & Nolen-Hoeksema, Citation1992; Hara et al., Citation2015).
BSW-related behaviours
Aligned with theoretical considerations proposed within both models, data within this subtheme can be classified as practitioner competency when planning (i.e. specifying and providing a rationale for the task) and reviewing BSW (i.e. discussing tasks the following session and appraising engagement). Findings evidence practitioner BSW-related behaviours as a driving factor for between-session engagement, denoting a generally positive effect across quantitative (Bryant et al., Citation1999; Conklin et al., Citation2018; Haller & Watzke, Citation2021; Jungbluth & Shirk, Citation2013; Woolley et al., Citation2023; Yew et al., Citation2021) and qualitative evidence (Callan, Citation2007; Finazzi et al., Citation2023).
Therapeutic relationship
Mixed findings were expressed from the four studies coded to this theme; while Wheaton et al. (Citation2016) and Maher et al. (Citation2012) found positive effects overall, VanDyke (Citation2002) evidenced a negative effect. In the qualitative phase of Callan (Citation2007), barriers to BSW relating to lack of collaboration and the bond component of the therapeutic relationship were highlighted. Notably, the positive effects found by Wheaton et al. (Citation2016) were found only for the total score of the Working Alliance Inventory-Short form (Hatcher & Gillaspy, Citation2006) and the task agreement sub-scale, while negative associations were documented for the other two sub-scales representing the patient-practitioner bond and the extent of mutually agreed goals for treatment.
Treatment context
Evidence corresponding to variations in treatment such as type of CBT (Addis & Jacobson, Citation1996, Citation2000; Conklin et al., Citation2021; Faisal & Masood, Citation2022; Raffield, Citation2004) or BSW (Barnes et al., Citation2013; Cammin-Nowak et al., Citation2013; Keller, Citation2015; Lax et al., Citation1992; Peynenburg et al., Citation2022); e.g., thought challenging versus breathing exercises (Peynenburg et al., Citation2022) or in vivo exposure versus imaginal exposure (Keller, Citation2015), were too limited to draw conclusions.
Treatment augmentation
Two RCTs explored the effect of Motivational Interviewing (MI) adjuncts to CBT treatment for anxiety, both suggesting MI was influential in improving between-session engagement (Simpson, Zuckoff, et al., Citation2010; Westra et al., Citation2009). Although interpretations are limited due to minimal available evidence, data suggests psychotropic medication may foster engagement between-sessions (Lax et al., Citation1992; Park et al., Citation2014; Wallert et al., Citation2018). The value of incentivised treatment engagement (Schneider, Citation2019) and personalised written prompts relating to BSW (Lundie, Citation1998) were examined only by single studies.
Personal resource
Motivation
Participants conveyed a lack of motivation impeding BSW (Barnes et al., Citation2013; Callan, Citation2007; Omylinska‐Thurston et al., Citation2019; Pugh et al., Citation2015), sometimes linked to other aspects such as negative consequences of engaging with tasks as discussed previously (Pugh et al., Citation2015) or as a symptom of their depression (Barnes et al., Citation2013). Evidence expressed positive effects from measures of change readiness (Dove, Citation2015; Maher et al., Citation2012), however Schneider (Citation2019) found the relationship between participants’ self-reported readiness to change and between-session exposure differed across treatment conditions and Westra (Citation2011) evidenced the effect of patient motivation for therapy varied when BSW engagement was rated by either the patient or practitioner.
Psychological insight
Findings appear to indicate higher levels of patient CBT understanding and ability reflects better between-session engagement (Bryant et al., Citation1999; Callan, Citation2007; Callan et al., Citation2019; Escovar & Chavira, Citation2019; Glenn et al., Citation2013; Maher et al., Citation2012; Peynenburg et al., Citation2022; Raffield, Citation2004; Woods et al., Citation2002). Executive functioning skills appeared to be positively associated with BSW (Lukin, Citation2011; Maher et al., Citation2012) with the exception of non-verbal executive skills (Maher et al., Citation2012).
Practical obstacles
Participants described how the demands of other responsibilities such as childcare and work, subsequently leading to lack of time, hampered between-session engagement (Barnes et al., Citation2013; Callan, Citation2007; Haller & Watzke, Citation2021; Peynenburg et al., Citation2022; Pugh et al., Citation2015). Further obstacles such as the fear of others discovering BSW resulted in tasks being left until the end of the day (Barnes et al., Citation2013) which can particularly impact the quality of engagement considering completing activities later relies on memory recall.
Sociocultural environment
While findings point to a beneficial effect on BSW from social support (Barnes et al., Citation2013; Callan, Citation2007; Wallert et al., Citation2018), the influence of further predictors such as quality of life (Callan et al., Citation2019; Jungbluth & Shirk, Citation2013; Maher et al., Citation2012; Wallert et al., Citation2018) or parental factors in child and adolescent studies (Jungbluth & Shirk, Citation2013; Lewin et al., Citation2011; Lukin, Citation2011) had too few studies to discern patterns. Predictors relating to cultural aspects were not present across included data.
Rates of engagement with BSW
The measurement of between-session engagement within quantitative studies varied substantially meaning it was not possible to compare engagement rates across studies. To gain some indication, we examined included studies which employed the HRS-II (Kazantzis et al., Citation2005) (n = 4), a 12-item scale which assesses the quantity and quality of between-session engagement as well as perceived difficulties, where higher scores indicate greater levels of engagement or positive patient beliefs. Of studies which reported the total scale score (Hara et al., Citation2015, Citation2017; Sachsenweger et al., Citation2015), mean scores ranged from 27.93 to 33.05; low scores out of the maximum score of 48. Qualitative findings indicate experiencing difficulties during BSW completion as a sizeable issue, with Barnes et al. (Citation2013) expressing BSW was found to be the biggest challenge during therapy.
Discussion
Summary of findings
This systematic review synthesised quantitative and qualitative data to broadly examine predictors of engagement with BSW across clinical presentations, populations, CBT interventions and modalities. A combined theoretical and empirical evidence approach depicted ten predictor themes related to between-session engagement. Existing evidence yielded ambiguous findings, yet several factors emerged as relatively consistent predictors of between-session engagement. Specifically, the review emphasises the importance of positive patient beliefs regarding BSW and treatment, such as perceived helpfulness to secure engagement. Additionally, practitioner competency when planning and reviewing tasks, relating to specificity and troubleshooting difficulties was shown to foster greater engagement. Conversely, instances of patient in-session resistance, including counter change talk, were indicative of decreased engagement between sessions. Findings are less clear concerning the impact of patient symptomology, sociocultural environment, practitioner beliefs and the therapeutic relationship. Although heterogeneity prohibited a method of computing rates of between-session engagement across studies, findings suggest recurring challenges with task completion and a need to enhance engagement with BSW. Encouragingly, those factors emerging as the strongest predictors are modifiable variables and may represent important avenues for practice change.
Clinical recommendations
Adopting a holistic approach enabled the identification of patient, practitioner, and environmental predictors of BSW. Thus far, investigations have most frequently focused on patient characteristics, though a growing body of evidence has explored the impact of practitioner factors. The latter offers a fruitful opportunity for intervention as practitioners have the potential to modify the influence of patient and environmental predictors and enhance engagement with BSW. Consistent with previous expert recommendations (Beck, Citation1979; Kazantzis et al., Citation2005), engagement promoting practitioner actions include patient involvement in task design, clear task specification, pre-emptive problem solving to address potential barriers to completion, and ongoing task review. Findings show that enabling understanding of the rationale for BSW and how to accomplish it can secure engagement even if a task is perceived by the patient as difficult and/or painful to complete, counteracting unhelpful patient beliefs which can impede BSW.
Data appeared to suggest greater between-session engagement for patients of White ethnicity (Callan, Citation2007; Jungbluth & Shirk, Citation2013; Stirman et al., Citation2018; Woods et al., Citation2002). Although included empirical data does not offer explanations behind these ethnic disparities, the influence of cultural practices and beliefs such as those regarding help-seeking were featured in the a priori framework. It is potentially important to note that CBT is rooted in European-American principles, neglecting those of non-Western cultures (Fenn & Byrne, Citation2013; Naeem et al., Citation2019); concepts used in BSW may therefore not be recognised by patients from ethnic minority backgrounds (Faheem, Citation2023). With the support of supervision, practitioners are encouraged to adapt treatment and BSW accordingly (see Naeem et al., Citation2019 for practical framework to culturally adapt CBT). As a minimum, this may involve practitioners evaluating their awareness of cultural knowledge across different ethnic groups and facilitating the use of culturally sensitive language and materials.
Although evidence was limited, indicators of socioeconomic status were positively associated with BSW. This aligns with previous research which evidenced unemployment as a consistent predictor of treatment disengagement (Verbist et al., Citation2023). This appears counterintuitive to psychological services aiming to support people back into work, particularly initiatives like the UK National Health Service (NHS) Talking Therapies for Anxiety and Depression programme where improving productivity persists as a central economic argument for the scheme (Clark et al., Citation2009). Further investigations are warranted to understand why socioeconomic status may predict between-session engagement, perhaps linked to other sociocultural factors like housing instability or practical obstacles such as increased demands from other responsibilities. Practitioners should consider sociocultural influences to BSW and attend to any barriers through discussion or signposting to other agencies for practical support.
Patient in-session resistance including patient opposition with practitioner direction or counter change-talk was identified as a consistent indicator of reduced engagement between-sessions. Practitioners can work to minimise these adverse effects to between-session engagement by integrating MI components in practice (see Miller & Rollnick, Citation2012; Randall & McNeil, Citation2017). The review showed promising evidence for MI adjuncts (Simpson, Zuckoff, et al., Citation2010; Westra et al., Citation2009) with further studies demonstrating how patient motivation and readiness to change facilitated BSW (Callan, Citation2007; Dove, Citation2015; Maher et al., Citation2012; Pugh et al., Citation2015). This finding aligns with that of the previous OCD-specific review (Wheaton & Chen, Citation2021), adding weight to an argument for practitioner-led redress. Empathy is also a fundamental component of MI and was found to positively influence between-session engagement when rated by patients (Burns & Nolen-Hoeksema, Citation1992; Hara et al., Citation2017). Practitioners can convey empathy through active listening techniques, employing verbal (i.e. empathetic statements) and non-verbal cues (i.e. open body language, eye contact), demonstrating warmth and a genuine interest in understanding patients’ experiences.
While there was no support for higher levels of education predicting better response between-sessions, psychological insight and comprehension of therapeutic techniques did predict greater between-session engagement. This, like patient motivation, is modifiable and practitioners can seek to build patient capabilities around CBT principles. Similarly, patient fear of failure and diminished confidence appeared to be a pervasive barrier to between-session engagement. Practitioners can consider using relativity simple tasks early in treatment to enable “easy-wins” to increase patient self-efficacy and drive subsequent engagement (Dobson, Citation2021).
Future research recommendations
While the review highlights several factors important to between-session engagement, gaps and inconsistencies in the evidence base remain. To gain a more confident understanding of predictors and advance the research in this area, the following limitations must be addressed.
The review emphasises methodological issues inherent within quantitative inquiries of BSW and a failure to address limitations long since raised by previous authors (Kazantzis et al., Citation2004; Mausbach et al., Citation2010). The lack of standardised metric and methodology measuring BSW remains a persistent issue, despite recognition of biases associated with the source (i.e. patient, practitioner, or observer), nature (Likert scale, number of assignments completed), and assessment timing (retroactive or contemporaneous) (Mausbach et al., Citation2010). Despite repeated calls to include assessment of the quality of engagement alongside measures of the quantity of BSW completed (Kazantzis et al., Citation2004, Citation2016), this has not been reflected in the literature; only 40% (n = 21) of quantitative studies in the current review considered engagement quality. Devoting time or effort to complete BSW does not necessary reflect the level of skills acquisition attained from the exercise and previous findings have highlighted evaluating the quality of between-session engagement may better predict sustained treatment benefit in comparison to measures of quantity alone (Kazantzis et al., Citation2016). While we do not advocate that assessments of quantity should be eradicated, instead we urge engagement between-sessions be defined by both the quantity and quality of work completed and echo previous recommendations to move away from oversimplified single-item measures of compliance and adherence to multifaceted measures of engagement. Though further psychometric validation is required, Haller and Watzke (Citation2021) offer a comprehensive measure of BSW; the Global Homework Engagement Scale (GHES), spanning assessments of both engagement quantity and quality, as does the HRS-II (Kazantzis et al., Citation2005). Both also assess various predictor variables including difficulties faced during completion which may help to evaluate the value of these factors further.
Increased standardisation of measurement has been continually recommended (Dobson, Citation2021; Kazantzis et al., Citation2004), yet it appears further harmony is still required. In future, those using quantitative designs ought to state a priori hypotheses, employ validated measures of predictors and between-session engagement, assess at multiple time points, using multiple sources and report complete data regardless of statical significance. This would enable future teams to conduct meta-analyses to produce more precise estimates of predictor effects, something not viable in the current evidence base. Constrained by data quality, we applied the method of vote counting based on direction of effect regardless of statistical significance (McKenzie & Brennan, Citation2023). There are however limitations to this method as it provides no information regarding magnitude of effects nor does it account for differences in study sizes (Borenstien et al., Citation2009), limiting the extent to which we can ascertain practical relevance; issues which can be overcome when more sophisticated analytical methods are possible. However, to further assess the practical significance of the consistent predictors of BSW, additional quantitative data, including effect sizes, can be found in S9.
While all themes require further evaluation, there are several prime areas where evidence is lacking; predictors pertaining to the sociocultural environment, practitioner beliefs and the therapeutic relationship. To advance knowledge concerning sociocultural predictors, more research with underserved communities is required given the review consisted mainly of White Western depressed adults which is not representative of the patient population composition. While both theoretical models incorporated in the synthesis stress the influence of practitioner beliefs and the therapeutic relationship on BSW, assertions were not confidently reflected across included data and further corroborating evidence is required. Additionally, despite including data from 26 studies, the influence of patient symptomology was inconsistent. Given the individual nature of presentations, qualitative designs may be favoured to complement and guide quantitative measurement, generating exploratory knowledge as to how and why certain factors predict engagement. Uncertainties also remain concerning the impact of comorbidity on BSW as findings were contradictory. Given the commonality of physical-mental health comorbidity as well as comorbid depression and anxiety, the lack of evidence concerning these multimorbid conditions is striking.
Conclusion
While the adverse effects of between-session disengagement on treatment outcomes are well-established, engagement with BSW remains far from optimal. Current evidence provides an emerging but incomplete picture of the core predictors of between-session engagement with specific knowledge gaps. Findings underscore the potential of practitioner behaviours centred around detailed planning and review of BSW to influence patient and wider environmental factors identified as consistent predictors to between-session engagement. The conceptual model presented in this paper offers a foundational framework for further testing through robust research and practice application. The continued evaluation and translation of key predictors into facilitative engagement mechanisms will enable service providers to enhance engagement with BSW and maximise health change.
Supplemental Material
Download MS Word (134.5 KB)Acknowledgments
The authors would like to thank Janice Connell for support with article screening and Chunhu Shi for input regarding quantitative data extraction.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Available on request.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/16506073.2024.2369939.
Additional information
Funding
Notes
1. We adopted a conservation approach when defining validated measures; defined as psychometrically tested in the context of BSW in CBT in more than once instance.
2. The mixed-methods study (Barnes et al., Citation2013) did not supply quantitative data relevant to the review question so was therefore not included in the quantitative quality assessment.
References
- Abramowitz, J. S., Franklin, M. E., Zoellner, L. A., & DiBernardo, C. L. (2002). Treatment compliance and outcome in obsessive-compulsive disorder. Behavior Modification, 26(4), 447–463. https://doi.org/10.1177/0145445502026004001
- Addis, M. E., & Jacobson, N. S. (1996). Reasons for depression and the process and outcome of cognitive-behavioral psychotherapies. Journal of Consulting and Clinical Psychology, 64(6), 1417–1424. https://doi.org/10.1037/0022-006X.64.6.1417
- Addis, M. E., & Jacobson, N. S. (2000). A closer look at the treatment rationale and homework compliance in cognitive-behavioral therapy for depression. Cognitive Therapy and Research, 24(3), 313–326. https://doi.org/10.1023/A:1005563304265
- Aviram, A., & Alice Westra, H. (2011). The impact of motivational interviewing on resistance in cognitive behavioural therapy for generalized anxiety disorder. Psychotherapy Research, 21(6), 698–708. https://doi.org/10.1080/10503307.2011.610832
- Barnes, M., Sherlock, S., Thomas, L., Kessler, D., Kuyken, W., Owen-Smith, A., Lewis, G., Wiles, N., & Turner, K. (2013). No pain, no gain: Depressed clients’ experiences of cognitive behavioural therapy. British Journal of Clinical Psychology, 52(4), 347–364. https://doi.org/10.1111/bjc.12021
- Beck, A. T. (1970). Cognitive therapy: Nature and relation to behavior therapy. Behavior Therapy, 1(2), 184–200. https://doi.org/10.1016/S0005-7894(70)80030-2
- Beck, A. T. (1979). Cognitive therapy of depression. Guilford press.
- Booth, A., & Carroll, C. (2015). Systematic searching for theory to inform systematic reviews: Is it feasible? Is it desirable? Health Information & Libraries Journal, 32(3), 220–235. https://doi.org/10.1111/hir.12108
- Borenstein, M., Hedges, L., Higgins, J., & Rothstein, H. (2009). Introduction to meta-analysis. John Wiley & Sons, Ltd.
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa
- Bryant, M. J., Simons, A. D., & Thase, M. E. (1999). Therapist skill and patient variables in homework compliance: Controlling an uncontrolled variable in cognitive therapy outcome research. Cognitive Therapy and Research, 23(4), 381–399. https://doi.org/10.1023/A:1018703901116
- Burns, D. D., & Nolen-Hoeksema, S. (1991). Coping styles, homework compliance, and the effectiveness of cognitive-behavioral therapy. Journal of Consulting and Clinical Psychology, 59(2), 305. https://doi.org/10.1037/0022-006X.59.2.305
- Burns, D. D., & Nolen-Hoeksema, S. (1992). Therapeutic empathy and recovery from depression in cognitive-behavioral therapy: A structural equation model. Journal of Consulting and Clinical Psychology, 60(3), 441–449. https://doi.org/10.1037/0022-006X.60.3.441
- Burns, D. D., & Spangler, D. L. (2000). Does psychotherapy homework lead to improvements in depression in cognitive–behavioral therapy or does improvement lead to increased homework compliance? Journal of Consulting and Clinical Psychology, 68(1), 46. https://doi.org/10.1037/0022-006X.68.1.46
- Button, M. (2013). Using in-session change talk and counter-change talk to predict engagement in cognitive-behavioural therapy ( MS00059). https://manchester.idm.oclc.org/login?url=https://www.proquest.com/dissertations-theses/using-session-change-talk-counter-predict/docview/1510314016/se-2?accountid=12253
- Callan, J. A. (2007). Development of a scale: Barriers to CBT homework completion scale. University of Pittsburgh.
- Callan, J. A., Kazantzis, N., Park, S. Y., Moore, C. G., Thase, M. E., Minhajuddin, A., Kornblith, S., & Siegle, G. J. (2019). A propensity score analysis of homework adherence-outcome relations in cognitive behavioral therapy for depression. Behavior Therapy, 50(2), 285–299. https://doi.org/10.1016/j.beth.2018.05.010
- Cammin-Nowak, S., Helbig-Lang, S., Lang, T., Gloster, A. T., Fehm, L., Gerlach, A. L., Strohle, A., Deckert, J., Kircher, T., Hamm, A. O., Alpers, G. W., Arolt, V., & Wittchen, H. (2013). Specificity of homework compliance effects on treatment outcome in CBT: Evidence from a controlled trial on panic disorder and agoraphobia. Journal of Clinical Psychology, 69(6), 616–629. https://doi.org/10.1002/jclp.21975
- Carroll, C., Booth, A., Leaviss, J., & Rick, J. (2013). “Best fit” framework synthesis: Refining the method. BMC Medical Research Methodology, 13(1), 37. https://doi.org/10.1186/1471-2288-13-37
- Christensen, M., Lim, C., Saha, S., Plana-Ripoll, O., Cannon, D., Presley, F., Weye, N., Momen, N., Whiteford, H., Iburg, K., & McGrath, J. J. (2020). The cost of mental disorders: A systematic review. Epidemiology and Psychiatric Sciences, 29. https://doi.org/10.1017/S204579602000075X
- Clark, D. M., Layard, R., Smithies, R., Richards, D. A., Suckling, R., & Wright, B. (2009). Improving access to psychological therapy: Initial evaluation of two UK demonstration sites. Behaviour Research and Therapy, 47(11), 910–920. https://doi.org/10.1016/j.brat.2009.07.010
- Collaborators, G. M. D. (2022). Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the global burden of disease study 2019. The Lancet Psychiatry, 9(2), 137–150. https://doi.org/10.1016/s2215-0366(21)00395-3
- Conklin, L. R., Curreri, A. J., Farchione, T. J., & Barlow, D. H. (2021). Homework compliance and quality in cognitive behavioral therapies for anxiety disorders and obsessive-compulsive disorder. Behavior Therapy, 52(4), 1008–1018. https://doi.org/10.1016/j.beth.2021.01.001
- Conklin, L. R., Strunk, D. R., & Cooper, A. A. (2018). Therapist behaviors as predictors of immediate homework engagement in cognitive therapy for depression. Cognitive Therapy and Research, 42(1), 16–23. https://doi.org/10.1007/s10608-017-9873-6
- Cooper, A. A., Kline, A. C., Graham, B., Bedard-Gilligan, M., Mello, P. G., Feeny, N. C., & Zoellner, L. A. (2017). Homework “dose,” type, and helpfulness as predictors of clinical outcomes in prolonged exposure for PTSD. Behavior Therapy, 48(2), 182–194. https://doi.org/10.1016/j.beth.2016.02.013
- David, D., Cristea, I., & Hofmann, S. G. (2018). Why cognitive behavioral therapy is the current gold standard of psychotherapy. Frontiers in Psychiatry, 9, 4. https://doi.org/10.3389/fpsyt.2018.00004
- De La Rosa, S., & Riva, M. T. (2021). Relationship variables in group psychotherapy for women sexual trauma survivors. International Journal of Group Psychotherapy, 71(1), 144–179. https://doi.org/10.1080/00207284.2020.1772072
- Dobson, K. S. (2021). A commentary on the science and practice of homework in cognitive behavioral therapy. Cognitive Therapy and Research, 45(2), 303–309. https://doi.org/10.1007/s10608-021-10217-5
- Dove, S. (2015). Adherence to treatment as a potential mediator of the relationship between readiness to change and treatment outcome in adolescent depression. Dissertation Abstracts International: Section B: The Sciences & Engineering, 77(2–B(E)), No Pagination Specified. https://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=psyc13&AN=2016-31154-065
- Ehring, T., Welboren, R., Morina, N., Wicherts, J. M., Freitag, J., & Emmelkamp, P. M. G. (2014). Meta-analysis of psychological treatments for posttraumatic stress disorder in adult survivors of childhood abuse. Clinical Psychology Review, 34(8), 645–657. https://doi.org/10.1016/j.cpr.2014.10.004
- Escovar, E. L., & Chavira, D. A. (2019). Engagement and premature dropout among latinx and non-latinx white patients in a cognitive-behavioral intervention for anxiety (22623559). https://manchester.idm.oclc.org/login?url=https://www.proquest.com/dissertations-theses/engagement-premature-dropout-among-latinx-non/docview/2309942092/se-2?accountid=12253.
- Faheem, A. (2023). ‘It’s been quite a poor show’ – Exploring whether practitioners working for Improving Access to Psychological Therapies (IAPT) services are culturally competent to deal with the needs of Black, Asian and Minority Ethnic (BAME) communities. The Cognitive Behaviour Therapist, 16. https://doi.org/10.1017/s1754470x22000642
- Faisal, K., & Masood, A. (2022). Efficacy of therapist guided internet based cognitive behavioural therapy for depression: A qualitative exploration of therapists and clients expEriences. Journal of Professional & Applied Psychology, 3(4), 453–468. https://doi.org/10.52053/jpap.v3i4.130
- Fals-Stewart, W., & Lucente, S. (1993). An MCMI cluster typology of obsessive—compulsives: A measure of personality characteristics and its relationship to treatment participation, compliance and outcome in behavior therapy. Journal of Psychiatric Research, 27(2), 139–154. https://doi.org/10.1016/0022-3956(93)90002-J
- Fehm, L., & Mrose, J. (2008). Patients’ perspective on homework assignments in cognitive-behavioural therapy. Clinical Psychology & Psychotherapy, 15(5), 320–328. https://doi.org/10.1002/cpp.592
- Fenn, K., & Byrne, M. (2013). The key principles of cognitive behavioural therapy. InnovAiT: Education and Inspiration for General Practice, 6(9), 579–585. https://doi.org/10.1177/1755738012471029
- Finazzi, E., MacLeod, E., MacBeth, A., & Triberti, S. (2023). Exploring service users experiences of remotely delivered CBT interventions in primary care during COVID-19: An interpretative phenomenological analysis. Public Library of Science ONE, 18(1), e0279263. https://doi.org/10.1371/journal.pone.0279263
- Finning, K., Richards, D. A., Moore, L., Ekers, D., McMillan, D., Farrand, P. A., O’Mahen, H. A., Watkins, E. R., Wright, K. A., Fletcher, E., Rhodes, S., Woodhouse, R., & Wray, F. (2017). Cost and outcome of behavioural activation versus cognitive behavioural therapy for depression (COBRA): A qualitative process evaluation. British Medical Journal Open, 7(4), e014161. https://doi.org/10.1136/bmjopen-2016-014161
- Fordham, B., Sugavanam, T., Edwards, K., Stallard, P., Howard, R., Das Nair, R., Copsey, B., Lee, H., Howick, J., Hemming, K., & Lamb, S. E. (2021). The evidence for cognitive behavioural therapy in any condition, population or context: A meta-review of systematic reviews and panoramic meta-analysis. Psychological Medicine, 51(1), 21–29. https://doi.org/10.1017/s0033291720005292
- Franks, C. M., & Wilson, G. (1976). Annual review of behavior therapy: Theory and practice (C. M. Franks & G. Terrence Wilson, Ed.). Brunner/Mazel Inc.
- Glenn, D., Golinelli, D., Rose, R. D., Roy-Byrne, P., Stein, M. B., Sullivan, G., Bystritksy, A., Sherbourne, C., & Craske, M. G. (2013). Who gets the most out of cognitive behavioral therapy for anxiety disorders? The role of treatment dose and patient engagement. Journal of Consulting and Clinical Psychology, 81(4), 639–649. https://doi.org/10.1037/a0033403
- Haller, E., & Watzke, B. (2021). The role of homework engagement, homework-related therapist behaviors, and their association with depressive symptoms in telephone-based CBT for depression. Cognitive Therapy and Research, 45(2), 224–235. https://doi.org/10.1007/s10608-020-10136-x
- Hara, K. M., Aviram, A., Constantino, M. J., Westra, H. A., & Antony, M. M. (2017). Therapist empathy, homework compliance, and outcome in cognitive behavioral therapy for generalized anxiety disorder: Partitioning within- and between-therapist effects. Cognitive Behaviour Therapy, 46(5), 375–390. https://doi.org/10.1080/16506073.2016.1253605
- Hara, K. M., Westra, H. A., Aviram, A., Button, M. L., Constantino, M. J., & Antony, M. M. (2015). Therapist awareness of client resistance in cognitive-behavioral therapy for generalized anxiety disorder. Cognitive Behaviour Therapy, 44(2), 162–174. https://doi.org/10.1080/16506073.2014.998705
- Hatcher, R. L., & Gillaspy, J. A. (2006). Development and validation of a revised short version of the working alliance inventory. Psychotherapy Research, 16(1), 12–25. https://doi.org/10.1080/10503300500352500
- Hayden, J. A., van der Windt, D. A., Cartwright, J. L., Côté, P., & Bombardier, C. (2013). Assessing bias in studies of prognostic factors. Annals of Internal Medicine, 158(4), 280–286. https://doi.org/10.7326/0003-4819-158-4-201302190-00009
- Hayes, S. C., & Hofmann, S. G. (2021). “Third‐wave” cognitive and behavioral therapies and the emergence of a process‐based approach to intervention in psychiatry. World Psychiatry, 20(3), 363–375. https://doi.org/10.1002/wps.20884
- Jungbluth, N. J., & Shirk, S. R. (2013). Promoting homework adherence in cognitive-behavioral therapy for adolescent depression. Journal of Clinical Child & Adolescent Psychology, 42(4), 545–553. https://doi.org/10.1080/15374416.2012.743105
- Kazantzis, N. (2021). Introduction to the special issue on homework in cognitive behavioral therapy: New clinical psychological science. Cognitive Therapy and Research, 45(2), 205–208. https://doi.org/10.1007/s10608-021-10213-9
- Kazantzis, N., & Dattilio, F. M. (2010). Definitions of homework, types of homework, and ratings of the importance of homework among psychologists with cognitive behavior therapy and psychoanalytic theoretical orientations. Journal of Clinical Psychology, 66(7), 758–773. https://doi.org/10.1002/jclp.20699
- Kazantzis, N., Deane, F. P., & Ronan, K. R. (2000). Homework assignments in cognitive and behavioral therapy: A meta-analysis. Clinical Psychology Science & Practice, 7(2), 189–202. https://doi.org/10.1093/clipsy.7.2.189
- Kazantzis, N., Deane, F. P., & Ronan, K. R. (2004). Assessing compliance with homework assignments: Review and recommendations for clinical practice. Journal of Clinical Psychology, 60(6), 627–641. https://doi.org/10.1002/jclp.10239
- Kazantzis, N., Deane, F. P., Ronan, K. R., & L’Abate, L. (2005). Using homework assignments in cognitive behavior therapy. Routledge. https://www.routledge.com/Using-Homework-Assignments-in-Cognitive-Behavior-Therapy/Kazantzis-Deane-Ronan-LAbate/p/book/9780415947732.
- Kazantzis, N., & Miller, A. R. (2022). A comprehensive model of homework in cognitive behavior therapy. Cognitive Therapy and Research, 46(1), 247–257. https://doi.org/10.1007/s10608-021-10247-z
- Kazantzis, N., & Shinkfield, G. (2007). Conceptualizing patient barriers to adherence with homework assignments. Cognitive and Behavioral Practice, 14(3), 317–324. https://doi.org/10.1016/j.cbpra.2006.08.003
- Kazantzis, N., Whittington, C., & Dattilio, F. (2010). Meta-analysis of homework effects in cognitive and behavioral therapy: A replication and extension. Clinical Psychology Science & Practice, 17(2), 144–156. https://doi.org/10.1111/j.1468-2850.2010.01204.x
- Kazantzis, N., Whittington, C., Zelencich, L., Kyrios, M., Norton, P. J., & Hofmann, S. G. (2016). Quantity and quality of homework compliance: A meta-analysis of relations with outcome in cognitive behavior therapy. Behavior Therapy, 47(5), 755–772. https://doi.org/10.1016/j.beth.2016.05.002
- Keller, S. M. (2015). Homework adherence in prolonged exposure for chronicposttraumatic stress disorder. Case Western Reserve University.
- Kobori, O., Dighton, G., & Hunter, R. (2020). Does perfectionism impact adherence to homework assignment? A preliminary pilot study of perfectionism and procrastination of CBT homework. Behavioural and Cognitive Psychotherapy, 48(2), 243–247.
- Lamkin, J., Hundt, N., Ahearn, E. P., Stanley, M., & Smith, T. L. (2019). Patterns of treatment disengagement and personality traits associated with posttraumatic stress disorder in recent-era U.S. veterans receiving cognitive processing therapy. Journal of Traumatic Stress, 32(4), 625–632. https://doi.org/10.1002/jts.22428
- Lax, T., Başoǧlu, M., & Marks, I. M. (1992). Expectancy and compliance as predictors of outcome in obsessive-compulsive disorder. Behavioural and Cognitive Psychotherapy, 20(3), 257–266. https://doi.org/10.1017/S0141347300017237
- Lewin, A. B., Peris, T. S., Bergman, R. L., McCracken, J. T., & Piacentini, J. (2011). The role of treatment expectancy in youth receiving exposure-based CBT for obsessive compulsive disorder. Behaviour Research and Therapy, 49(9), 536–543. https://doi.org/10.1016/j.brat.2011.06.001
- Lukin, K. (2011). Predictors and moderators of treatment adherence in depressed youths. Dissertation Abstracts International: Section B: The Sciences & Engineering, 72(12–B), 7691. https://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=psyc9&AN=2012-99120-132
- Lundie, E. M. (1998). The effects of written prompts on homework compliance and outcome in a cognitive behavioural treatment for depression and research portfolio. University of Glasgow.
- Maher, M. J., Wang, Y., Zuckoff, A., Wall, M. M., Franklin, M., Foa, E. B., & Simpson, H. B. (2012). Predictors of patient adherence to cognitive-behavioral therapy for obsessive-compulsive disorder. Psychotherapy and Psychosomatics, 81(2), 124. https://doi.org/10.1159/000330214
- Mausbach, B. T., Moore, R., Roesch, S., Cardenas, V., & Patterson, T. L. (2010). The relationship between homework compliance and therapy outcomes: An updated meta-analysis. Cognitive Therapy and Research, 34(5), 429–438. https://doi.org/10.1007/s10608-010-9297-z
- McKenzie, J. E., & Brennan, S. E. (2023). Chapter 12: Synthesizing and presenting findings using other methods. In J. P. T. Higgins, J. Thomas, J. Chandler, M. Cumpston, T. Li, M. J. Page, & V. A. Welch (Eds.), Cochrane handbook for systematic reviews of interventions version 6.4 (updated August 2023) (pp. 321–347). Cochrane www.training.cochrane.org/handbook
- Miller, W. R., & Rollnick, S. (2012). Motivational interviewing: Helping people change. Guilford press.
- Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., Shekelle, P., & Stewart, L. A. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews, 4(1), 1. https://doi.org/10.1186/2046-4053-4-1
- Mohlman, J. (2013). Executive skills in older adults with GAD: Relations with clinical variables and CBT outcome. Journal of Anxiety Disorders, 27(1), 131–139. https://doi.org/10.1016/j.janxdis.2012.12.001
- Moola, S., Munn, Z., Tufanaru, C., Aromataris, E., Sears, K., Sfetcu, R., Currie, M., Qureshi, R., Mattis, P., & Lisy, K. (2024). Chapter 7: Systematic reviews of etiology and risk. In E. Aromataris, C. Lockwood, K. Porritt, B. Pilla, & Z. Jordan (Eds.), JBI manual for evidence synthesis. https://doi.org/10.46658/JBIMES-24-06
- Naeem, F., Phiri, P., Rathod, S., & Ayub, M. (2019). Cultural adaptation of cognitive–behavioural therapy. BJPsych Advances, 25(6), 387–395. https://doi.org/10.1192/bja.2019.15
- National Institute for Health and Care Excellence. (2011). Common mental health problems: Identification and pathways to care [ Clinical guideline CG123]. https://www.nice.org.uk/guidance/cg123
- Nilsen, P. (2015). Making sense of implementation theories, models and frameworks. Implementation Science, 10(1). https://doi.org/10.1186/s13012-015-0242-0
- Noyes, J., Booth, A., Cargo, M., Flemming, K., Harden, A., Harris, J., Garside, R., Hannes, K., Pantoja, T., & Thomas, J. (2022). Chapter 21: Qualitative evidence. In J. Higgins, J. Thomas, J. Chandler, M. Cumpston, T. Li, M. Page, & V. Welch (Eds.), Cochrane handbook for systematic reviews of interventions (Version 6.3). www.training.cochrane.org/handbook
- Olatunji, O. B., Rosenfield, D., Monzani, B., Krebs, G., Heyman, I., Turner, C., Isomura, K., & Mataix‐Cols, D. (2015). Effects of homework compliance on cognitive‐behavioral therapy with d‐cycloserine augmentation for children with obsessive compulsive disorder. Depression & Anxiety, 32(12), 935–943. https://doi.org/10.1002/da.22423
- Omylinska‐Thurston, J., McMeekin, A., Walton, P., & Proctor, G. (2019). Clients’ perceptions of unhelpful factors in CBT in IAPT serving a deprived area of the UK. Counselling and Psychotherapy Research, 19(4), 455–464. https://doi.org/10.1002/capr.12249
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., Mcdonald, S., and Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. https://doi.org/10.1136/bmj.n71
- Park, J. M., Small, B. J., Geller, D. A., Murphy, T. K., Lewin, A. B., & Storch, E. A. (2014). Does d-cycloserine augmentation of CBT improve therapeutic homework compliance for pediatric obsessive–compulsive disorder? Journal of Child and Family Studies, 23(5), 863–871. https://doi.org/10.1007/s10826-013-9742-1
- Peynenburg, V., Wilhelms, A., Sapkota, R., Nugent, M., Owens, K., Titov, N., Dear, B., & Hadjisatvropoulos, H. (2022). Understanding client difficulties in transdiagnostic internet-delivered cognitive behaviour therapy: A qualitative analysis of homework reflections. Journal of Clinical Medicine, 11(14), 4226. https://doi.org/10.3390/jcm11144226
- Primakoff, L., Epstein, N., & Covi, L. (1986). Homework compliance: An uncontrolled variable in cognitive therapy outcome research. Behavior Therapy, 17(4), 433–446. https://doi.org/10.1016/S0005-7894(86)80073-9
- Pugh, E., Hadjistavropoulos, N., D, H., Hampton, A. J., Bowen, A., & Williams, J. (2015). Client experiences of guided internet cognitive behavior therapy for postpartum depression: A qualitative study. Archives of Women’s Mental Health, 18(2), 209–219. https://doi.org/10.1007/s00737-014-0449-0
- Raffield, T. J. (2004). A preliminary study of sociotropy/autonomy and brief cognitive therapy for depression [Health & mental health treatment & prevention 3300]. Dissertation Abstracts International: Section B: The Sciences & Engineering, 65(1–B), 449. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc5&NEWS=N&AN=2004-99014-087 ( Dissertation Abstracts International.
- Randall, C. L., & McNeil, D. W. (2017). Motivational interviewing as an adjunct to cognitive behavior therapy for anxiety disorders: A critical review of the literature. Cognitive and Behavioral Practice, 24(3), 296–311. https://doi.org/10.1016/j.cbpra.2016.05.003
- Roth, A. D., & Pilling, S. (2008). A competence framework for the supervision of psychological therapies. Retrieved August 18, 2011.
- Russo, G., Silva, T. J., Gassasse, Z., Filippon, J., Rotulo, A., & Kondilis, E. (2021). The impact of economic recessions on health workers: A systematic review and best-fit framework synthesis of the evidence from the last 50 years. Health Policy and Planning, 36(4), 542–551. https://doi.org/10.1093/heapol/czaa180
- Ryum, T., Bennion, M., & Kazantzis, N. (2023). Integrating between-session homework in psychotherapy: A systematic review of immediate in-session and intermediate outcomes. Psychotherapy Theory, Research, Practice, Training, 60(3), 306–319. https://doi.org/10.1037/pst0000488
- Sachsenweger, M. A., Fletcher, R. B., & Clarke, D. (2015). Pessimism and homework in CBT for depression. Journal of Clinical Psychology, 71(12), 1153–1172. https://doi.org/10.1002/jclp.22227
- Schneider, R. L. (2019). Values-Versus monetary reward-enhanced exposure therapy for the treatment of social anxiety in emerging adulthood. University of Colorado at Boulder.
- Scott, M. J., & Stradling, S. G. (1997). Client compliance with exposure treatments for posttraumatic stress disorder [behavior therapy & behavior modification 3312]. Journal of Traumatic Stress, 10(3), 523–526. https://doi.org/10.1002/jts.2490100315
- Shafran, R., Myles-Hooton, P., Bennett, S., & Öst, L.-G. (2021). The concept and definition of low intensity cognitive behaviour therapy. Behaviour Research and Therapy, 138, 103803. https://doi.org/10.1016/j.brat.2021.103803
- Sijercic, I., Button, M. L., Westra, H. A., & Hara, K. M. (2016). The interpersonal context of client motivational language in cognitive-behavioral therapy. Psychotherapy Theory, Research, Practice, Training, 53(1), 13–21. https://doi.org/10.1037/pst0000017
- Simons, A. D., Marti, C. N., Rohde, P., Lewis, C. C., Curry, J., & March, J. (2012). Does homework “matter” in cognitive behavioral therapy for adolescent depression? Journal of Cognitive Psychotherapy, 26(4), 390–404. https://doi.org/10.1891/0889-8391.26.4.390
- Simpson, H. B., Maher, M., Page, J. R., Gibbons, C. J., Franklin, M. E., & Foa, E. B. (2010). Development of a patient adherence scale for exposure and response prevention therapy. Behavior Therapy, 41(1), 30–37. https://doi.org/10.1016/j.beth.2008.12.002
- Simpson, H. B., Zuckoff, A. M., Maher, M. J., Page, J. R., Franklin, M. E., Foa, E. B., Schmidt, A. B., & Wang, Y. (2010). Challenges using motivational interviewing as an adjunct to exposure therapy for obsessive-compulsive disorder. Behaviour Research and Therapy, 48(10), 941–948. https://doi.org/10.1016/j.brat.2010.05.026
- Snippe, E., Schroevers, M. J., Annika Tovote, K., Sanderman, R., Emmelkamp, P. M., & Fleer, J. (2015). Patients’ outcome expectations matter in psychological interventions for patients with diabetes and comorbid depressive symptoms. Cognitive Therapy and Research, 39(3), 307–317. https://doi.org/10.1007/s10608-014-9667-z
- Startup, M., & Edmonds, J. (1994). Compliance with homework assignments in cognitive-behavioral psychotherapy for depression: Relation to outcome and methods of enhancement. Cognitive Therapy and Research, 18(6), 567–579.
- Stirman, S. W., Gutner, C. A., Suvak, M. K., Adler, A., Calloway, A., & Resick, P. (2018). Homework completion, patient characteristics, and symptom change in cognitive processing therapy for PTSD. Behavior Therapy, 49(5), 741–755. https://doi.org/10.1016/j.beth.2017.12.001
- Sun, X., Briel, M., Busse, J. W., You, J. J., Akl, E. A., Mejza, F., Bala, M. M., Bassler, D., Mertz, D., Diaz-Granados, N., Vandvik, P. O., Malaga, G., Srinathan, S. K., Dahm, P., Johnston, B. C., Alonso-Coello, P., Hassouneh, B., Walter, S. D., and Guyatt, G. H. (2012). Credibility of claims of subgroup effects in randomised controlled trials: Systematic review. BMJ, 344, e1553. https://doi.org/10.1136/bmj.e1553
- Systematic Reviews. (2009). CRD’s guidance for undertaking reviews in health care. Centre for Reviews and Dissemination, University of York.
- VanDyke, M. M. (2002). Contribution of working alliance to manual-based treatment of social anxiety disorder. The University of Nebraska-Lincoln.
- Verbist, I. L., Fabian, H., Huey, D., Brooks, H., Lovell, K., & Blakemore, A. (2023). Exploring access and engagement with Improving Access to Psychological Therapies (IAPT) services, before, during, and after the COVID-19 lockdown: A service evaluation in the Northwest of England. Psychotherapy Research, 34(2), 216–227. https://doi.org/10.1080/10503307.2023.2184285
- Wallert, J., Gustafson, E., Held, C., Madison, G., Norlund, F., von Essen, L., & Olsson, E. M. G. (2018). Predicting adherence to internet-delivered psychotherapy for symptoms of depression and anxiety after myocardial infarction: Machine learning insights from the U-CARE heart randomized controlled trial. Journal of Medical Internet Research, 20(10), e10754. https://doi.org/10.2196/10754
- Westra, H. A. (2011). Comparing the predictive capacity of observed in-session resistance to self-reported motivation in cognitive behavioral therapy. Behaviour Research and Therapy, 49(2), 106–113. https://doi.org/10.1016/j.brat.2010.11.007
- Westra, H. A., Arkowitz, H., & Dozois, D. J. (2009). Adding a motivational interviewing pretreatment to cognitive behavioral therapy for generalized anxiety disorder: A preliminary randomized controlled trial. Journal of Anxiety Disorders, 23(8), 1106–1117. https://doi.org/10.1016/j.janxdis.2009.07.014
- Wheaton, M. G., & Chen, S. R. (2021). Homework completion in treating obsessive–compulsive disorder with exposure and ritual prevention: A review of the empirical literature. Cognitive Therapy and Research, 45(2), 236–249. https://doi.org/10.1007/s10608-020-10125-0
- Wheaton, M. G., Huppert, J. D., Foa, E. B., & Simpson, H. B. (2016). How important is the therapeutic alliance in treating obsessive-compulsive disorder with exposure and response prevention? An empirical report. Clinical Neuropsychiatry, 13(6), 88.
- Woods, C. M., Chambless, D. L., & Steketee, G. (2002). Homework compliance and behavior therapy outcome for panic with agoraphobia and obsessive compulsive disorder. Cognitive Behaviour Therapy, 31(2), 88–95. https://doi.org/10.1080/16506070252959526
- Woolley, M. G., Smith, B. N., Micol, R. L., Farmer, C. C., & Galovski, T. E. (2023). Evaluating the relative contribution of patient effort and therapist skill in integrating homework into treatment for posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, & Policy. https://doi.org/10.1037/tra0001459
- Yew, R. Y., Dobson, K. S., Zyphur, M., & Kazantzis, N. (2021). Mediators and moderators of homework–outcome relations in CBT for depression: A study of engagement, therapist skill, and client factors. Cognitive Therapy and Research, 45(2), 209–223. https://doi.org/10.1007/s10608-019-10059-2