ABSTRACT
Background: Under- and over-nutrition during pregnancy are known risk factors for pregnancy complications and adverse pregnancy and infant outcomes. Understanding perceptions around nutrition in pregnancy can create culturally appropriate interventions for improved health outcomes.
Objective: A mixed-methods study was performed to explore local perceptions and practices of diet and physical activity in pregnancy in a marginalised population along the Myanmar–Thailand border.
Methods: From April to July 2017, a cross-sectional survey and focus group discussions were conducted with pregnant women reporting to antenatal care; in-depth interviews were conducted with senior midwives at participating organisations along the Myanmar–Thailand border.
Results: A total of 388 pregnant women were interviewed at two clinic sites along the Myanmar–Thailand border. A high proportion of women had limited knowledge of and poor dietary practices. Consuming a sweetened drink in the last 24 hours as well as being a non-teenage, multigravida woman was significantly associated with high body mass index (BMI) compared to normal BMI. Qualitative analysis combined focus group discussions (n = 66) and in-depth interviews (n = 4) summarising emergent themes: common foods eaten or avoided and rationale; benefits of nutrition; perceptions of overweight and weight gain during pregnancy; barriers to a healthy diet; and sources of diet information.
Conclusions: There is limited awareness about healthy diets and lifestyle in these marginalised, migrant communities along the Myanmar–Thailand border. This study suggests that simple, culturally appropriate messaging should be provided to women and communities with low health literacy to generate awareness about healthy lifestyles and their effects on pregnancy outcomes as an important element of a broader strategy to address maternal nutrition in this population. However, more studies to determine the effectiveness of a broad range of interventions in low- and middle-income countries (LMIC) are needed, especially in marginalised migrant populations.
Responsible Editor Jennifer Stewart Williams, Umeå University, Sweden
Background
The growing double burden of under- and over-nutrition in pregnant women in low- and middle-income countries (LMIC) has a direct impact on maternal, infant and child health [Citation1–Citation4]. Infant health and child development closely relate to maternal nutrition, with effects extending into adolescence and adulthood [Citation5–Citation7]. These impacts have important societal and economic implications, resulting in reduced human capital – a cycle of malnutrition with intergenerational effects most felt in (LMIC) [Citation8].
Among LMIC, Asian populations are disproportionally affected by the nutrition transition due to increased risk of morbidity from diet-related diseases of over-nutrition at lower BMI than non-Asians. These diseases of overweight coexist with persistently high rates of under-nutrition in Asia [Citation9–Citation13]. As the global poor bear the greatest burden of risk due to the nutrition transition [Citation14], migrant populations within Asia require special attention. In 2015, migrants numbered 244 million globally, after rapid increases in the preceding 15 years [Citation15,Citation16]. Along the Myanmar–Thailand border a large workforce of low-skilled labourers from Myanmar supports Thailand’s burgeoning professional and service industries [Citation17–Citation20]. In 2016, Myanmar made up 80% of all documented migrants in Thailand (1.43 million), with an additional estimated 1–2 million undocumented migrants in Thailand from Myanmar, Cambodia and Lao PDR [Citation21]. Migrants face significant constraints on their social well-being with particular concern for pregnant women who have limited options for appropriate care during pregnancy [Citation22–Citation25] and restricted access to healthy foods. Recent analyses of body mass index (BMI) and gestational weight gain (GWG) over the past 30 years among migrant and refugee pregnant women along the Myanmar–Thailand border mirror global trends in persistent under-nutrition with a rapid rise in overweight and obesity [Citation26].
Although nutrition is a key modifiable risk factor in pregnancy, little is known about the diet of pregnant women in LMIC and particularly pregnant migrants. Despite the 2009 Institute of Medicine (USA) guidelines on GWG, health workers in high-income countries (HIC) report difficulties in antenatal nutrition counselling [Citation27–Citation29]. These challenges are exacerbated in LMIC settings where poverty and poorly resourced health systems can perpetuate a lack of awareness about the importance of nutrition and physical activity amongst health workers and local communities [Citation30–Citation33]. Although rare in the literature, a focus on marginalised populations such as migrants and refugees from a region of economic inequality and armed conflict can provide insights into social, ethnic and cultural influences on maternal nutrition [Citation34,Citation35]. To inform the development of targeted interventions around maternal nutrition, a mixed-methods study was conducted to examine common perceptions and practices of diet and physical activity among pregnant women in a migrant population along the Myanmar–Thailand border.
Methods
Setting
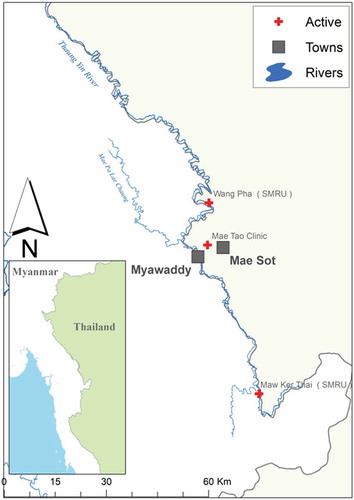
A cross-sectional survey and focus group discussions (FGD) with pregnant women were conducted at two antenatal care (ANC) clinics run by the Shoklo Malaria Research Unit (SMRU) in Maw Ker Thai (MKT) and Wang Pha (WPA), Thailand. SMRU has provided medical and obstetric services for migrants since 1998 in MKT and 2004 in WPA. In-depth interviews (IDI) were conducted with midwives from SMRU and Mae Tao Clinic (MTC). MTC has been providing care for migrant communities in urban border areas since 1989 (). This post-conflict region has emerged from more than five decades of civil unrest due to differences with the central government of Myanmar. Education systems have suffered and economic inequalities have prompted many to seek part-time residence along the border, where health services remain limited in rural and remote areas. SMRU and MTC have provided free maternal and child health services for decades to fill a gap otherwise unanswered by governments on either side of the border [Citation17–Citation20].
In the SMRU and MTC catchment areas, migrants residing on both sides of the border frequently move to and from Myanmar but the total population, estimated at 200,000, is relatively stable [Citation19,Citation36,Citation37]. In 2016, SMRU performed over 16,000 ANC consultations and over 1600 deliveries. MTC provided over 10,000 ANC consultations and 2500 deliveries in the same year [Citation38]. Pregnant women receiving care reflect the migrant populations along the border, who are predominantly Burman or Karen; commonly speak Burmese, and Sgaw and Pwo Karen; and represent Buddhists, Christians and Muslims [Citation37]. Average socio-economic status of women from SMRU WPA ANC is higher than MKT, but both communities have low literacy rates at around 45% [Citation39]. Women presenting to SMRU ANC have a median of 11 visits prior to delivery [Citation40].
Study design
A convergent parallel mixed-methods design was employed with quantitative (cross-sectional survey), and qualitative (FGD, IDI) components exploring pregnant women’s perceptions and behaviours regarding nutrition in pregnancy. The mixed-methods approach was chosen to enhance findings in quantifying behaviours and perceptions around nutrition and exercise with qualitative components exploring the rationale for these behaviours and perceptions. Prior to finalisation, cross-sectional survey and FGD and IDI guides were translated into Sgaw Karen and Burmese, back-translated to identify and correct errors in translation or meaning, and piloted with 20 pregnant women or SMRU staff.
Cross-sectional survey
All pregnant women presenting to ANC were approached individually and informed about the study. The aim was to conduct 200 surveys from each SMRU clinic as this approached the total number of monthly ANC consultations. Women presenting for delivery or pregnancy complications were excluded. Four study staff were trained at each site to administer the questionnaire in the patients’ preferred languages. Informal investigator observations informed the survey, which consisted of 12 questions evaluating women’s knowledge of appropriate GWG, their pre-pregnancy weight, if they returned to pre-pregnancy weight after prior delivery (for multigravida) and if they felt they knew what constitutes a healthy diet. Women were also asked if they perceived themselves to be active and about ‘healthy behaviours’ such as: ever having exercised and, if so, how often; most recent consumption of a snack or a sweetened beverage. Snacks (small amounts of food between larger meals) were recorded by interviewers and categorised as healthy or unhealthy; photographs of locally available sweetened beverages were shown to women to easily identify what they consumed.
Focus group discussions
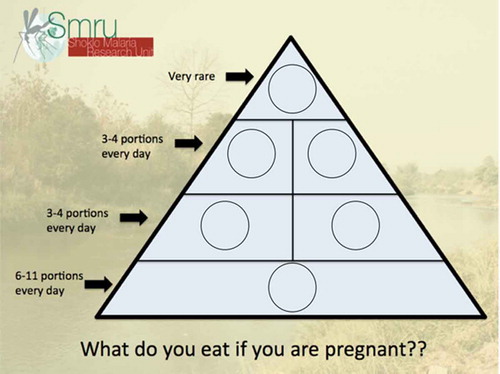
The FGD facilitator was trained and experienced in leading FGD, and fluent in Burmese, and Sgaw and Pwo Karen. When possible, an additional facilitator fluent in the three languages also helped with FGD and assisted in note-taking by the primary author. FGD were conducted in private counselling rooms, once participants consented to being audio-recorded. FGD began with women prompted to solve a food pyramid puzzle with photos of food groups according to their usual dietary preferences (Figure 2), followed by questions and probes as outlined in . Pregnant women presenting to ANC were approached, provided with information and, if expressing interest, these women were grouped according to age, parity, ethnicity and language. If groups of four to eight participants were possible among women presenting to ANC on a given day, these women provided consent and FGD were then conducted.
Table 1. Focus group discussion guide used with pregnant women at SMRU ANC in Maw Ker Thai and Wang Pha.
In-depth interviews
SMRU and MTC senior midwives (≥ 8 years of experience) were invited to participate in IDI to discuss changes seen in pregnant women nutrition over their careers. Questions explored midwives’ perceptions of nutrition and dietary habits of pregnant women; and changes in pregnant women nutritional status, GWG and access to healthy foods over time. Ideas about appropriate counselling measures or interventions for nutrition in pregnancy were also discussed. All midwives were provided with information on the study prior to consenting to participate, agreed to have IDI recorded and were interviewed in a private room at SMRU or MTC clinics.
Anthropometric measurements
Trained midwives collected maternal weight and height data at the first ANC visit in the first trimester and this was used to estimate pre-pregnancy BMI, if available [Citation41,Citation42]. A mechanical scale measured weight accurate to 0.5 kg. A stadiometer measured height with precision up to 1 mm. World Health Organization (WHO) standards for Asian populations were used to determine low (< 18.5 kg/m2), normal (18.5–23 kg/m2) and high (≥ 23 kg/m2) BMI.
Statistical analysis
Cross-sectional survey data were compared using Student’s t-test for continuous, normally distributed variables, and the Chi-squared test for categorical variables. Bonferroni correction was applied to baseline characteristics with multiple comparisons ().
Table 2. Demographic characteristics of all women participating in the cross-sectional survey and by BMI category (MKT = Maw Ker Thai ANC; WPA = Wang Pha ANC).
Cross-sectional survey responses were summarised for all women and for those who first presented to antenatal care in the first trimester (). BMI taken after the first trimester is no longer a proxy for pre-pregnancy BMI; therefore, only women enrolled in the first trimester were included (). Logistic regression was used to examine associations between BMI (low vs normal and high vs normal) and cross-sectional survey responses. Both models were adjusted for ethnicity (Burman, Karen or other). Age < 20 years (teenage) and gravidity demonstrated collinearity and a combination variable was used in the model: teenage and primigravida, teenage and/or primigravida, and neither teenage nor primigravida. Covariates that were significant at p < 0.10 were included in a multivariate logistic regression model where, using a stepwise approach, only those variables that were significant at p < 0.05 were retained in the final model and considered independent risk factors. Factors significantly associated with high BMI in the first trimester were reported as adjusted odds ratios (AOR) with 95% confidence intervals (95% CI). Data from the cross-sectional survey were analyzed using Stata v14.0 (StataCorp, College Station, Texas, USA) and SPSS v15.0 (IBM, Armonk, New York, USA).
Table 3. Responses to selected cross-sectional questions on perceptions and behaviours regarding nutrition in pregnancy at SMRU ANC.
The recordings of FGD and IDI were transcribed from Karen and directly to English by AHH working with translators fluent in Burmese and Sgaw and Pwo Karen. Line-by-line inductive coding was initially performed on full transcripts of FGD and IDI by AHH. Any outstanding questions, clarifications and confirmation of findings from the initial transcription and coding phases were discussed with AHH, MKP, SP and MCD until consensus was reached. Thematic analysis based on initial coding was used to identify emergent themes and triangulate the information collected [Citation43,Citation44] facilitated by NVivo for Mac v11.4.0 (QSR International, Melbourne, Australia). Finally, queries were performed on textual data to identify variations across pregnant women according to parity, ethnicity and site as well as for midwives. This inductive approach allowed for establishing links between research objectives and findings from raw data and developed deeper understanding of the underlying experiences and processes evident in emergent themes.
Results
Cross-sectional survey
A total of 388 pregnant women participated in cross-sectional surveys in MKT (n = 203) and WPA (n = 185; ). At each site, most pregnant women meeting inclusion criteria were included: 72.2% (203/281) in MKT and 59.9% (185/309) at WPA. Significant differences between BMI groups were observed in ethnicity, gravidity, age (and age < 20 years) and trimester of first ANC attendance (). Of the pregnant women who reported employment the majority 85.2% (167/196) were in unskilled jobs including daily manual labour, factory work and agricultural work.
Overall, pregnant women had limited knowledge and poor dietary practices (). A high proportion of women did not know what constitutes a healthy diet (43.6%; 169/388) and were unsure of an appropriate GWG (85.3%; 331/388), and nearly half (47.7%; 185/388) of the women did not know their pre-pregnancy weight. Three-quarters (77.1%; 299/388) perceived they were active but less than one-third (29.1%, 113/388) reported ever exercising. Most women (63.3%; 243/384) reported regularly eating unhealthy snacks, with almost half (47.9%; 186/388) of the women having consumed a sweetened beverage in the 24 hours prior to being surveyed. Of the 14% (55/388) of women who provided an estimate of appropriate GWG, the median weight nominated was 6 kg (range 0–20 kg).
The proportion of first antenatal care visits was highest for the first trimester than in the second or third trimesters (). In the sub-cohort of women with BMI measured in the first trimester, the proportion of women who had consumed sweetened beverages in the previous 24 hours was highest in the high BMI group (). Variables excluded in regression analysis were knowledge of GWG, pre-pregnancy weight, return to pre-pregnancy weight, women’s perception of activity, ever exercised, or knowledge of a healthy diet. Consuming a sweetened drink and age (teenager) with gravidity were initially included in the regression model with covariates for women consuming a snack in the prior 24 hours and eating unhealthy snacks. Consuming a sweetened drink in the last 24 hours as well as being a non-teenage, multigravid woman was significantly and independently associated with high BMI compared to normal BMI, and there was no association with consuming a snack in the prior 24 hours and/or eating unhealthy snacks after adjustment (). The proportion of women who did not know what constitutes a healthy diet was highest in the low BMI group but this was not statistically significant (). Amongst multigravida, the proportion of women self-reporting not returning to their pre-pregnancy weight was higher among women with high BMI than with normal BMI (62.1% vs. 22.4%, AOR 5.66, 95% CI 2.14–14.96; p = 0.001) ().
Qualitative findings
A total of 11 FGD of four to eight participants each were conducted with a total of 66 women; 38 from a total of 7 FGD from MKT and 28 women from a total of 4 FGD from WPA ranging in age from 18 to 39 and 18 to 40 years, respectively. Two FGD were conducted with Burman primigravida; and three FGD conducted with Karen primigravida, Karen multigravida and Burman multigravida each. IDI were conducted with four midwives; two from SMRU and two from MTC.
Foods eaten
Staple foods for pregnant women across all groups included rice, vegetables, fruits and milk. Common sources of protein included fish, chicken and eggs, but were often limited in pregnant women’s diets. Karen and primigravida women were more likely to mention protein sources in their diet. Women attributed limited intake of protein to preference, noting that the smell of raw or cooked meats was offensive and nauseating. Most milk consumed by women is processed and high in sugar and/or saturated fats. Burman women made more mention of curries in their diets, which often were served with rice. Oil, and in particular palm oil, was often included in the diet of women from WPA. Although many women desired soybean and other vegetable oils as they were considered healthier, palm oil was more often used due to cost and availability.
When asked about snacks, women mentioned regularly eating small amounts of food between meals, but also included beverages such as milk and other sweetened beverages (e.g. Sprite). Often women consumed cheap snacks purchased at local shops that are deep-fried, artificially sweetened, industrially or locally processed and/or high in sugar or salt content. Burman women and women from MKT spent the greatest amount of time discussing snacks, citing their inexpensiveness, ability to satiate a craving or hunger quickly and as an option when appetite is low as in the earlier stages of pregnancy:
Yes, I eat one time a day, but I cannot eat much so I eat only a little. I eat snacks meant for children – 1 packet for 5 baht [USD $0.15] – and cake [processed, sweetened].
I eat a little bit of rice, but more fruits. (Primigravida, Karen, MKT)
I eat rice only a little bit. Normally I drink milk and eat snacks. (Burman, Multigravida, MKT)
Benefits of nutrition
As a rationale for their diet, women commonly noted that they would ‘think’ that these were the appropriate foods. Many reported indulging cravings, which were often attributed to the developing foetus (‘the baby asks for it’). There was a commonly held belief that during pregnancy a woman was free to eat what she pleased as her appetite allowed:
‘During pregnancy, we can eat everything, because the baby asks for it. If I see it, I will buy and eat.’ (Primigravida, Karen MKT)
Few women mentioned direct benefits of maternal nutrition, but many seemed to understand that diet could have benefits for maternal and foetal health. Many made simplified assertions that women should eat certain foods to ‘give the baby strength’, ‘to give the mother strength’ or to have ‘good energy’. A minority of women mentioned that meats, vegetables and fruits were important for development of the ‘baby brain’ and for the ‘baby to grow tall’.
Foods avoided
The main foods avoided were chilli, coconut water, dogfruit (Archidendron pauciflorum), ‘hot foods’, daw kha tha (Oroxylum inidicum) and raw foods. Chilli was universally avoided in its raw form to avoid baby discomfort (e.g. ‘burn the baby’). This did not preclude women from eating spicy foods, particularly if they were prepared with dried chillies (e.g. nya oo htee [Karen] or nga pi [Burmese], a fish paste prepared with fish sauce, shrimp paste and dried chillies). Coconut water, especially in early pregnancy, was commonly associated with miscarriage and a ‘difficult delivery’. Dogfruit was also mentioned as a common food to avoid in all groups. Its strong smell and bitter taste could harm the baby or cause a difficult delivery. Food items categorised as ‘hot foods’ to be avoided to minimise mother and baby discomfort included chillies (raw), spicy foods, ginger, coconut water and betel nut.
A legume found along the border region, Oroxylum indicum (Karen: daw ka tha), was believed by Karen women to cause miscarriage. One mother asserted that even sitting beneath a daw ka tha tree may induce miscarriage.
Raw foods, such as raw vegetables (including eggplant, commonly eaten raw along the border) as well as meats, were thought to cause disease (e.g. ‘worm infections’) in the mother or infant.
Another category mentioned included ‘sticky foods’, such as sticky rice and ripe bananas, as potentially causing a ‘sticky placenta’ that would make delivery difficult. These foods were also thought to be related to the amount of vernix on the delivered infant.
Overweight or obesity and weight gain during pregnancy
Most women did not know of an effect of excessive GWG on maternal or foetal/infant health. Women were evenly divided between viewing overweight or ‘fat’ as beneficial or harmful in pregnancy:
If you eat more then you will put on weight. The baby will become strong and you will become fat. For people who don’t want to eat or don’t like eating because of a lack of appetite – then in such cases you cannot add weight. (Primigravida, Karen, MKT)
However, some women feared that overweight or obesity risked a large infant and difficult delivery. Many could state direct risks to maternal health: pre-eclampsia (‘high blood pressure’), diabetes (‘sweet blood’ or ‘sweet urine’) and atherosclerosis (‘veins can become clogged’). Even upon probing, however, many were unaware of any relation of overweight or excessive GWG to infant health.
Midwives knew the ill effects of overweight and poor and/or excessive GWG to both mother and foetus. Midwives noted that overweight was of increasing concern compared to earlier years working in the region, when the primary concern was under-nutrition:
The mother has become too fat so it can be a problem when she comes to delivery. If there is too much fat it can lead to bad health. Over sweetness, diabetes. It can be that the fat closes the blood vessels. It can also cause joint pains. They can have sweet blood [diabetes] or high blood pressures. (Midwife, SMRU)
Social considerations and sources of information
Social factors impacting nutrition for pregnant women related to financial, food access and family considerations. Women most readily mentioned financial limitations, unprompted, especially among Karen women and women from MKT. Expense limited dietary choices such as meat, often consumed once or twice a week – corroborated by midwives. Often, finances fluctuated daily and women spent money on foods as it became available. Women often borrowed money for food from close relatives. Financial and logistic constraints commonly hampered access to foods, especially for those who lived far from urban areas. Family considerations were important: where household chores were shared with mothers, husbands, aunts or other family members, greater time was available for preparation of regular meals. Other members of the family may be responsible for the purchase of foods (e.g. the husband) or cooking (e.g. mothers or sisters). Some women, unable to work or prohibited from work, were dependent on other family members for their meals. Women and midwives mentioned gathering wild vegetables near one’s house to address financial constraints:
All of us who come here[,] none of us live in the towns, all of us live in different places and villages – country people. The foods that we are talking about … if people mentioned it, we can buy it to eat. But if they were not mentioned, then we cannot buy it. It doesn’t mean that we can afford everyday because we cannot. Where I live is now considered close to Koh Koh [near the SMRU WPA clinic, on the Myanmar side] but you have to take a motorcycle to get there and it costs 100 baht [USD $3.17]. So in order to eat all these things we have to travel some distance. For those who live far, far away it is out of the question. (Multigravida, Karen, WPA)
Midwives felt that better formal education and improved counselling by health workers were responsible for women having healthier diets than in the past:
‘Before, women were afraid of eating, but we have been teaching the women and now they have greater health awareness, fewer problems and the women are eating better’ (Midwife, MTC).
Commonly cited sources for information on foods to eat or avoid and nutritional benefits were elders within the community and family members. However, women frequently mentioned that their thoughts concerning appropriate foods for pregnant women came from no source at all (i.e. ‘I think by myself’), or that they ‘never heard’ about appropriate nutrition in pregnancy. Health professionals as a source of information were predominantly mentioned by multiparous women, likely reflecting more frequent contact with the health system:
For us, there are no specific things to eat, it is only if I think the food is nutritious for the baby, then I will try to eat it. (Multigravida, Burman, WPA)
For me, I have learned this information … whenever I heard it from the medic or health workers. When they talk about it, I try to pay attention and remember. (Multigravida, Burman, WPA)
Midwives and pregnant women agreed that information reflective of older traditions and beliefs circulates in communities, but that younger women often disregard such advice. Women appeared to consider information provided by community members to be less trustworthy than that of health professionals:
‘But [beliefs of the elders] are from before, and now we see that pregnant women eat everything, whatever they want to eat. These are the changes; they eat everything’ (Midwife, MTC).
Counselling considerations
The food pyramid game () helped assess what women ate and explored women’s knowledge and awareness, yielding insights about counselling. The instructions for the game were repeated up to three times in each FGD, with the pyramid described as relative frequency of food groups eaten, rather than portions of each food group per day. This is likely a reflection of low health literacy and numeracy among this population, as well as cultural differences in measurement or awareness of amounts of foods included in one’s diet. The vocabulary of pregnant women did not appear to allow for certain concepts; for example, photos depicting protein were often referred to as ‘meat’, although these photos included lentils and eggs.
When asked about how to improve pregnant women nutrition, midwives suggested clinic-based counselling, having noticed benefits of individual counselling using posters, flip charts and handouts. One midwife mentioned the potential benefits of group counselling:
‘Sometimes, we counsel the breastfeeding women in a group. We can do this type of counseling. We can explain, “How should women eat?” “What to eat?” ’ (Midwife, SMRU).
Two midwives shared reservations about their expertise on dietary recommendations for pregnant women. Two midwives noted limitations in time available for clinic-based counselling or funds to provide dietary supplements. Midwives were quick to suggest that women could eat nutritious foods, but that many lacked awareness, stating that most pregnant women would try to adhere to midwives’ recommendations, as financial constraints allowed:
We encourage them that if they have money they should buy the healthy foods, but if you cannot afford, you can try to pick vegetables in the forest that grow for free. There are plenty. We do counselling like this. (Midwife, MTC)
Discussion
This study examines perceptions and behaviours related to nutrition in pregnancy in a marginalised community along the Myanmar–Thailand border. Both the quantitative and qualitative findings suggest a dearth of awareness about nutrition. Among women with BMI available from the first trimester, the survey showed that being overweight was associated with consumption of sweetened beverages, being a non-teenage multigravida, and not returning to pre-pregnancy weight (among multigravida). Many women expressed a limited understanding of the link between maternal nutrition and foetal development. Although better informed, midwives lacked confidence in counselling pregnant women on appropriate nutrition. Considering the limitations of counselling by health workers in HIC, a feeling of inadequacy among local midwives is not surprising in this low-resource context with a rapidly changing burden of diet-related disease [Citation27,Citation28,Citation32].
Information on healthy and unhealthy foods was variable. Women mentioned social dietary taboos, which provide a cultural ‘awareness’ regarding specific ‘unhealthy’ local foods, intended to protect mother and child [Citation45,Citation46]. As in other Asian populations [Citation47], meat as a protein source was limited due to pregnant women’s preference and its cost, with health benefits largely unknown. Likewise, Karen and Burman women expressed concern over ‘hot’ and ‘cool’ foods – likely alluding to a perceived internal bodily balance [Citation46]. However, women often disregard dietary taboos [Citation46]. Perceptions of healthy and unhealthy foods change over time, as described elsewhere in South Asia; women now may consider eating fruits and vegetables to be healthy, whereas previously they avoided these foods as a means of ‘eating down’ [Citation48–Citation50].
The wider public health issue along the border is the ease of access to cheap, calorically dense, processed foods with adverse nutritional effects that exacerbate a lack of awareness and proclivity to indulge cravings [Citation13,Citation51–Citation53]. This becomes increasingly important in a context where women are restricted financially and geographically in accessing healthier foods. Pregnant women and midwives posited that women would make improved dietary choices, within their social constraints, if they were provided with appropriate information regarding nutrition. However, the reach of clinic-based care during pregnancy is far from comprehensive in this border region, with limitations in clinic-based programming for maternal nutrition [Citation24,Citation54,Citation55]. Awareness-raising at a community level should be considered to reach younger women whose diets may be tied to the choices of older members of the household.
Our findings suggest that simple, culturally appropriate counselling measures should be provided for women with low health literacy in LMIC settings [Citation30,Citation31,Citation34,Citation39]. The puzzle engaged women in discussion and identified gaps in knowledge about nutrition. Pictures are key in settings where numeracy and measurements for food frequency among pregnant women may be limited. Clear, broad prescriptions about foods high in sugar, salt or fats can help women make appropriate dietary choices when faced with easy access to processed foods. Such instructive measures lend themselves to group counselling in clinics or women’s groups at a community level [Citation56]. This requires developing the capacity of local health workers in effective counselling and should make use of older women equipped with appropriate information when possible [Citation57]. Continued research on pregnant women nutrition along the border could produce easy-to-understand, culturally and contextually specific information materials to counsel women presenting to ANC about healthy GWG [Citation26,Citation27,Citation58]. However, recent analyses suggest that such lifestyle measures are of modest benefit during pregnancy [Citation34,Citation59,Citation60] and change will likely require policy interventions to improve access to healthy foods along the border to influence pre-conception maternal nutrition [Citation61]. Similar upstream interventions should focus on accessing and educating women prior to conception, as pre-conception care is exceedingly rare in these communities [Citation55]. Such far-reaching public health interventions have the potential to break the intergenerational cycle of malnutrition and poverty.
The mixed-methods study design allowed quantitative measures of behaviours and potential impact on BMI to be further explained by qualitative methods [Citation62]. All methods allowed for triangulation of the main study findings. Study limitations include limited generalisability due to geographic and cultural specificity [Citation32], and lack of external validation of the cross-sectional survey. Regression analysis was limited to a small subset of women presenting in the first trimester, potentially obscuring significant associations, but baseline characteristics of women who attended in the first trimester were not significantly different to women who presented later. No validated questionnaire on diet and exercise in pregnancy currently exists [Citation63], and women’s self-report of exercise (often translated to ‘playing sport’ in Burmese and Karen) and activity in this study was subjective. These limitations were accepted at the study outset, as the primary aim was to develop a baseline understanding of perceptions of marginalised women toward nutritional status in pregnancy.
Conclusions
There is limited awareness about healthy diets and lifestyle in these marginalised, migrant communities along the Myanmar–Thailand border. This study suggests that simple, culturally appropriate messaging should be provided to women and communities with low health literacy to generate awareness about healthy lifestyles and their effects on pregnancy outcomes as an important element of a broader strategy to address maternal nutrition in this population. However, more studies to determine the effectiveness of a broad range of interventions in LMIC are needed, especially in marginalised migrant populations.
Ethics and consent
The Oxford Research Ethics Committee (OxTREC 509-17) and the Research Ethics Committee of Chiang Mai University Faculty of Medicine (FAM-2560-04604) approved this study in accordance with the Declaration of Helsinki. The Tak Province Community Advisory Board, a local ethics committee based along the Myanmar–Thailand border, also approved this study (TCAB-03/FEV/2017).
Paper context
Under- and over-nutrition during pregnancy risk adverse pregnancy and infant outcomes. Understanding perceptions around nutrition in pregnancy can create culturally appropriate interventions for improved health outcomes. This paper describes local perceptions toward nutrition during pregnancy in marginalised populations along the Myanmar–Thailand border. Simple, culturally appropriate messaging provided to women and communities with low health literacy can generate awareness about healthy lifestyles and their importance during pregnancy as part of a broader strategy to address maternal nutrition.
Acknowledgments
We would like to acknowledge the help and support of MTC, responsible for providing senior midwives who participated in this study. We also would like to acknowledge the pregnant women participating in this study and the SMRU study staff responsible for data collection.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
Notes on contributors
Ahmar H. Hashmi
All authors meet the International Committee of Medical Journal Editors requirements for authorship.
References
- Aune D, Saugstad OD, Henriksen T, et al. Maternal body mass index and the risk of fetal death, stillbirth, and infant death: a systematic review and meta-analysis. JAMA. 2014 Apr 16;311:1536–12.
- Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–451.
- Kiel DW, Dodson EA, Artal R, et al. Gestational weight gain and pregnancy outcomes in obese women: how much is enough? Obstet Gynecol. 2007;110:752–758.
- Nohr EA, Vaeth M, Baker JL, et al. Pregnancy outcomes related to gestational weight gain in women defined by their body mass index, parity, height, and smoking status. Am J Clin Nutr. 2009;90:1288–1294.
- Adair LS. Long-term consequences of nutrition and growth in early childhood and possible preventive interventions. International nutrition: achieving millennium goals and beyond. Vol. 78. Basel: Kargers Publishers; 2014. p. 111–120.
- Miller SL, Huppi PS, Mallard C. The consequences of fetal growth restriction on brain structure and neurodevelopmental outcome. J Physiol. 2016 Feb 15;594:807–823.
- Victora CG, De Onis M, Hallal PC, et al. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics. 2010;125:e473–e480.
- Victora CG, Adair L, Fall C, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet. 2008;371:340–357.
- Ee TX, Allen JC Jr., Malhotra R, et al. Determining optimal gestational weight gain in a multiethnic Asian population. J Obstet Gynaecol Res. 2014;40:1002–1008.
- Koh H, Ee TX, Malhotra R, et al. Predictors and adverse outcomes of inadequate or excessive gestational weight gain in an Asian population. J Obstet Gynaecol Res. 2013;39:905–913.
- Liu Y, Dai W, Dai X, et al. Prepregnancy body mass index and gestational weight gain with the outcome of pregnancy: a 13-year study of 292,568 cases in China. Arch Gynecol Obstet. 2012;286:905–911.
- Ota E, Haruna M, Suzuki M, et al. Maternal body mass index and gestational weight gain and their association with perinatal outcomes in Viet Nam. Bull World Health Organ. 2011 Feb 01;89:127–136.
- Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012 Jan;70:3–21.
- Popkin BM, Gordon-Larsen P. The nutrition transition: worldwide obesity dynamics and their determinants. Int J Obes Relat Metab Disord. 2004 Nov;28:S2–S9.
- United Nations Department of Economic and Social Affairs. International migration report 2015: highlights. New York: United Nations; 2015.
- Urquia ML, Gagnon AJ. Glossary: migration and health. J Epidemiol Community Health. 2011 May;65:467–472.
- Chantavanich S. Labor migration in the Greater Mekong Sub-region: thailand policies towards migrant workers from Myanmar. Bangkok: Mahidol University; 2006.
- Hugo G. Migrants and their integration: contemporary issues and implications. Paris: UNESCO; 2003.
- Huguet JW, Chamratrithirong A Thailand migration report 2011. Bangkok: International Organization for Migration; 2011.
- Sciortino R, Punpuing S. International migration in Thailand. Vol. 2009. Bangkok: International Organization for Migration; 2009.
- International Organization for Migration. Thailand migration profile. Bangkok: International Organization for Migration; 2016.
- Belton S. Borders of fertility: unplanned pregnancy and unsafe abortion in Burmese women migrating to Thailand. Health Care Women Int. 2007 Apr;28:419–433.
- Low S, Tun KT, Mhote NP, et al. Human resources for health: task shifting to promote basic health service delivery among internally displaced people in ethnic health program service areas in eastern Burma/Myanmar. Glob Health Action. 2014;7:24937.
- Mullany LC, Lee CI, Yone L, et al. Access to essential maternal health interventions and human rights violations among vulnerable communities in Eastern Burma. PLoS Med. 2008;5:12.
- Parmar PK, Barina CC, Low S, et al. Health and human rights in eastern Myanmar after the political transition: a population-based assessment using multistaged household cluster sampling. PLoS One. 2015;10:e0121212.
- Hashmi A, Solomon N, Lee SJ, et al. Nutrition in transition: historical cohort analysis of trends in under- and over-nutrition among pregnant women in a marginalized population along the Thailand-Myanmar border from 1986 to 2016. BMC Pregnancy Childbirth. Submitted.
- McDonald SD, Pullenayegum E, Taylor VH, et al. Despite 2009 guidelines, few women report being counseled correctly about weight gain during pregnancy. Ajog. 2011;205:e1–e6.
- Nikolopoulos H, Mayan M, MacIsaac J, et al. Women’s perceptions of discussions about gestational weight gain with health care providers during pregnancy and postpartum: a qualitative study. BMC Pregnancy Childbirth. 2017 Mar 24;17:97.
- Institute of Medicine. Weight gain during pregnancy: reexamining the guidelines. Washington, DC: Institute of Medicine; 2009.
- Aung MN, Lorga T, Srikrajang J, et al. Assessing awareness and knowledge of hypertension in an at-risk population in the Karen ethnic rural community, Thasongyang, Thailand. Int J Gen Med. 2012;5:553–561.
- Lorga T, Srithong K, Manokulanan P, et al. Public knowledge of diabetes in Karen ethnic rural residents: a community-based questionnaires study in the far north-west of Thailand. Int J Gen Med. 2012;5:799–804.
- Raman S, Nicholls R, Ritchie J, et al. Eating soup with nails of pig: thematic synthesis of the qualitative literature on cultural practices and beliefs influencing perinatal nutrition in low and middle income countries. BMC Pregnancy Childbirth. 2016 Jul 28;16:192.
- Scorgie F, Blaauw D, Dooms T, et al. “I get hungry all the time”: experiences of poverty and pregnancy in an urban healthcare setting in South Africa. Glob Health. 2015;25:37.
- Poston L, Caleyachetty R, Cnattingius S, et al. Preconceptional and maternal obesity: epidemiology and health consequences. Lancet Diabetes Endocrinol. 2016;4:1025–1036.
- Kavle JA, Landry M. Addressing barriers to maternal nutrition in low- and middle-income countries: A review of the evidence and programme implications. Matern Child Nutr. 2017:e12508.
- Carrara VI, Lwin KM, Phyo AP, et al. Malaria burden and artemisinin resistance in the mobile and migrant population on the Thai-Myanmar border, 1999–2011: an observational study. PLoS Med. 2013;10:e1001398.
- Parker DM, Carrara VI, Pukrittayakamee S, et al. Malaria ecology along the Thailand-Myanmar border. Malar J. 2015;05:388.
- Mae Tao Clinic. Mae Tao Clinic annual report 2016: working together. Mae Sot, Thailand: Mae Tao Clinic; 2017.
- Carrara VI, Hogan C, Pree CD, et al. Improved pregnancy outcome in refugees and migrants despite low literacy on the Thai-Burmese border: results of three cross-sectional surveys. BMC Pregnancy Childbirth. 2011;11:45.
- Moore KA, Simpson JA, Paw MK, et al. Safety of artemisinins in first trimester of prospectively followed pregnancies: an observational study. Lancet Infect Dis. 2016;16:576–583.
- Moore KA, Simpson JA, Thomas KH, et al. Estimating gestational age in late presenters to antenatal care in a resource-limited setting on the Thai-Myanmar border. PLoS One. 2015;10:e0131025.
- Krukowski RA, West DS, DiCarlo M, et al. Are early first trimester weights valid proxies for preconception weight? BMC Pregnancy Childbirth. 2016;16(1):357.
- Malterud K. Qualitative research: standards, challenges, and guidelines. Lancet. 2001;358:483–488.
- Patton MQ. Enhancing the quality and credibility of qualitative analysis. Health Serv Res. 1999;34(5):1189–1208.
- Arzoaquoi SK, Essuman EE, Gbagbo FY, et al. Motivations for food prohibitions during pregnancy and their enforcement mechanisms in a rural Ghanaian district. J Ethnobiol Ethnomed. 2015;17:59.
- Meyer-Rochow VB. Food taboos: their origins and purposes. J Ethnobiol Ethnomed. 2009 Jun;29:18.
- Chatterjee N, Fernandes G. ‘This is normal during pregnancy’: a qualitative study of anaemia-related perceptions and practices among pregnant women in Mumbai, India. Midwifery. 2014 Mar;30:e56–e63.
- Christian P, Srihari SB, Thorne-Lyman A, et al. Eating Down in pregnancy: exploring food-related beliefs and practices of pregnancy in rural Nepal. Ecol Food Nutr. 2006;45:253–278.
- Harding KL, Matias SL, Mridha MK, et al. Eating down or simply eating less? The diet and health implications of these practices during pregnancy and postpartum in rural Bangladesh. Public Health Nutr. 2017;20:1928–1940.
- Hutter I. Reduction of food intake during pregnancy in rural South India. Trop Med Int Health. 1996;1:399–405.
- Dans A, Ng N, Varghese C, et al. The rise of chronic non-communicable diseases in southeast Asia: time for action. Lancet. 2011;377:680–689.
- Angkurawaranon C, Jiraporncharoen W, Chenthanakij B, et al. Urban environments and obesity in Southeast Asia: a systematic review, meta-analysis and meta-regression. PLoS One. 2014;9:e113547.
- Kosulwat V. The nutrition and health transition in Thailand. Public Health Nutr. 2002 Feb;5:(1A):183–9.
- Mullany LC, Lee TJ, Yone L, et al. Impact of community-based maternal health workers on coverage of essential maternal health interventions among internally displaced communities in eastern Burma: the MOM project. PLoS Med. 2010 Aug 3;7:e1000317.
- Stevens A, Gilder MET, Moo P, et al. Folate supplementation to prevent birth abnormalities: evaluating an intervention among refugees and migrant workers on the Thai-Myanmar border. Public Health. In press.
- Prost A, Colbourn T, Seward N, et al. Women’s groups practising participatory learning and action to improve maternal and newborn health in low-resource settings: a systematic review and meta-analysis. Lancet. 2013;381:1736–1746.
- Aubel J, Toure I, Diagne M. Senegalese grandmothers promote improved maternal and child nutrition practices: the guardians of tradition are not averse to change. Soc Sci Med. 2004 Sep;59:945–959.
- Lee SJ, Hashmi A, Carrara VI, et al. Nutrition in transition: optimal gestational weight gain according to body mass index to reduce adverse perinatal outcomes in a marginalized population along the Myanmar-Thailand border. In Preparation.
- Hanson M, Barker M, Dodd JM, et al. Interventions to prevent maternal obesity before conception, during pregnancy, and post partum. Lancet Diabetes Endocrinol. 2017;5:65–76.
- Catalano P, De Mouzon SH. Maternal obesity and metabolic risk to the offspring: why lifestyle interventions may have not achieved the desired outcomes. Int J Obes (Lond). 2015 Apr;39:642–649.
- Hunter-Adams J, Rother HA. Pregnant in a foreign city: A qualitative analysis of diet and nutrition for cross-border migrant women in Cape Town, South Africa. Appetite. 2016 Aug;01:403–410.
- Peters DH, Adam T, Alonge O, et al. Implementation research: what it is and how to do it. BMJ. 2014;48:731–736.
- Lennox J, Petrucka P, Bassendowski S. Eating practices during pregnancy: perceptions of select Maasai women in Northern Tanzania. Glob Health Res Policy. 2017;2:9.