ABSTRACT
Background: Studies examining how the capacity of health facilities affect implementation of free healthcare policies in low and middle-income countries are limited.
Objective: This study describes how the context and institutional capacity of health facilities influenced implementation of the free maternal and child health programme (FMCHP) in Enugu state, South-east Nigeria.
Methods: We conducted a qualitative case study at the state level and in two health districts (Isi-Uzo and Enugu Metropolis) in Enugu State. Data were collected through document review and semi-structured, in-depth interviews with policymakers (n = 16), healthcare providers (n = 16) and health facility committee leaders (n = 12) guided by an existing capacity framework and analysed using a thematic framework approach.
Results: The findings reveal that active health facility committees, changes in provider payment process, supportive supervision, drug revolving fund, availability of medical equipment, electronic data transmission and staff sanction system enhanced the capacity of health facilities to offer free healthcare. However, ineffective decentralisation, irregular supervision and weak citizen participation limited this capacity. Uncertain provider payment, evidence of tax payment policy and a co-existing fee-exempt scheme constrained health facilities in following the FMCHP guidelines. Poor recording and reporting skills and lack of support from district officials constrained providers’ adherence to claims’ submission timeline. Poor funding, weak drug supply system, inadequate infrastructure and lack of participatory decision-making constrained delivery of free healthcare. Insufficient trained workforce, mission-inconsistent postings and transfers, and weak staff disciplinary system limited the human resource capacity.
Conclusions: Effectiveness of FMCHP at the health facility level depends on the extent of decentralisation, citizen participation, concurrent and conflictive policies, timely payment of providers, organisation of service delivery and human resources practices. Attention to these contextual and institutional factors will enhance responsiveness of health facilities, sustainability of free healthcare policies and progress towards universal health coverage.
Responsible Editor Peter Byass, Umeå University, Sweden
Background
Many low and middle-income countries (LMICs) have adopted free healthcare policies to mitigate the negative impact of user fees on the poor, improve access to health services and accelerate progress towards universal health coverage and the sustainable development goals (SDGs) [Citation1–Citation3]. That notwithstanding, poor use of public health facilities and poor health indicators in low resource settings persist [Citation3]. Only 9.5% of the countries with maternal mortality ratios above 100 deaths per 100,000 live births in 1990 achieved the millennium development goal (MDG) target of three-quarter reduction in maternal mortality [Citation4]. Of the 104 LMICs, only about 23% attained the MDG4 target to reduce under-five mortality by two-thirds relative to 1990 levels [Citation4]. In Nigeria, despite adoption of free maternal and child healthcare policies in 2006 [Citation5], reduction in maternal and childhood mortality rates have been lower than expected [Citation6]. Although capacity of health facilities, referred to as ability to perform appropriate tasks effectively, efficiently and sustainably [Citation7,Citation8], affect the effectiveness of free healthcare policies, theory-driven studies examining the effect of capacity of health facilities on implementation of user fee removal policies are limited.
Growing evidence suggests that factors affecting the capacity of health facilities to implement free healthcare policies are context-sensitive. Use of service charters to curb informal payments to service providers [Citation9], active health facility committees (HFCs) including financial management [Citation10–Citation12], timely payment of providers [Citation13], regular and uninterrupted drug supply [Citation13], availability of clear guidelines on use of user fee replacement grants [Citation14], an effective staff sanction framework, which reduces health worker absenteeism [Citation15], have enabled health facilities to effectively implement free healthcare policies. In contrast, barriers to health facilities implementing free healthcare policies include weak decentralization [Citation10,Citation16–Citation18]; poor supervision and monitoring [Citation19,Citation20]; weak referral systems [Citation17]; absence of written implementation guidelines [Citation14,Citation21]; shortage of staff and inconsistent recording and reporting [Citation10,Citation20]; low social accountability and community involvement [Citation9,Citation22–Citation24]; delayed payment of providers [Citation12,Citation21,Citation25]; lack of adequate drug stock [Citation17,Citation18,Citation24,Citation26–Citation31]; mistrust between providers and patients [Citation19,Citation32–Citation34]; absenteeism [Citation10,Citation15,Citation20]; poorly motivated health workers [Citation18,Citation24]; lack of financial incentives [Citation35]; preference for urban postings [Citation19,Citation36]; funding inadequacy in health facilities [Citation16]; inadequate physical infrastructure [Citation18,Citation24,Citation36]; unavailability of guidelines for use of user fee replacement fund [Citation37] and unclear procedures for targeting beneficiaries [Citation3].
Enugu State adopted the free maternal and child healthcare programme (FMCHP) in 2007, which removed user fees at the point of service delivery for pregnant women and under-five children based on a minimum services package [Citation38]. The FMCHP, which is tax-funded through State and Local Government contributions, is delivered mainly through public primary and secondary health facilities. Basic child healthcare services including health education, growth monitoring, immunization, nutritional supplementation, de-worming and integrated management of childhood illnesses; basic ante-natal care, safe deliveries, post-natal care, family planning services, routine laboratory investigations and basic emergency obstetric care are provided across the two levels of care. Additionally, the cottage and district hospitals provide comprehensive maternity services and treat difficult childhood illnesses. The state teaching hospital provides only referral care.
The FMCHP is administered through a decentralized health system in which the State Ministry of Health (MOH) is organized into a Policy Development and Planning Directorate (PDPD) and State Health Board (SHB); and the state delineated into seven District Health Boards (DHBs) and 68 Local Health Authorities (LHAs) (). The PDPD, through a Steering Committee, governs the FMCHP and manages FMCHP funds. The SHB, through an Implementation Committee, oversees the DHBs and supervises district-level health workers, vets free care claims and pays health facilities for patients who receive free services. The DHBs monitor implementation of FMCHP at the LHAs and district hospitals; ensure regular and uninterrupted supply of FMCHP forms to health facilities; and collate facility claims from LHAs and submit them to the SHB. The LHAs monitor implementation of the FMCHP in all primary health facilities and cottage hospitals. LHAs support health facilities to prepare claims and submit completed claims to the DHBs. Health facilities are expected to provide responsive services, document all FMCHP expenditures, completely fill and promptly submit claim forms, track submitted claims, report major service delivery gaps to government and handle minor infrastructural gaps.
Evidence indicates that the initial improvement on service utilization has not been sustainable, out-of-pocket payments are common, and the FMCHP does not seem pro-poor nor does it improve use of the public health system [Citation39–Citation42]. The maternal mortality rate in Enugu is 645/100,000 live births [Citation43], higher than the national rate of 576/100,000 live births [Citation44]. Under-five mortality rate in South-east Nigeria, including Enugu State, is 131/1000 live births; slightly higher than national average of 128/100,000 live births [Citation44]. Only 45% of under-five children are fully vaccinated while 8.6% of the children have no vaccination at all in Enugu State [Citation44]. Delivery at public health facilities in Enugu State, though improved by 15.1% from 2008 to 2013, is still low at about 36.5% [Citation44]. Yet, little is known about facility-level factors affecting implementation of the FMCHP.
The purpose of this study was to examine how context and institutional capacity of health facilities affect implementation of FMCHP in Enugu, South-east Nigeria. Such evidence will help decision makers in Nigeria and similar settings to develop a governance model for strengthening the capacity of health facilities to offer free healthcare that contributes towards universal health coverage and the SDGs.
Methods
Conceptual framework
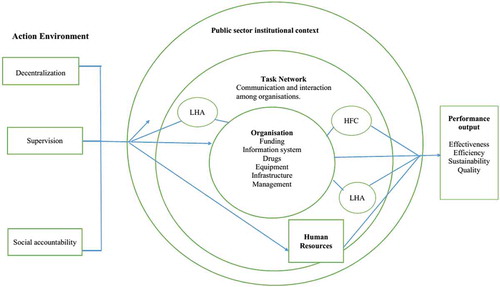
The study was guided by the Hilderbrand and Grindle (Citation1997) Capacity Framework [Citation45], comprising five dimensions – action environment, institutional context of public sector, task network, organisation and human resources – that impact on public service performance as shown in . Action environment focuses on the external context of health facilities such as decentralization, supervision and citizen participation. Institutional context of public providers deals with general rules, procedures and concurrent policies that shape performance of health facilities. Task network entails relations among actors involved in implementing FMCHP. Organisation encompasses structures and processes in health facilities that enhance service delivery including physical resources, information systems, drug delivery systems, and finances. Human resources comprise attraction and retention of individuals who work in public health facilities. Optimal capacity of health facilities would result in responsiveness of service delivery.
Study setting
This study, which is part of a doctoral thesis that assessed the governance of FMCHP in Enugu State, Nigeria [Citation46], took place at the MOH and in two districts (Isi-Uzo and Enugu Metropolis) of Enugu State, South-east Nigeria. In 2017, Isi-Uzo and Enugu Metropolis had 209,872 and 1,021,912 populations, respectively, out of which women of childbearing age constitute 42.8% and 46.9%, respectively [Citation44]. Children under five years represent 18.1% and 15.5%, respectively, of the population of Isi-Uzo and Enugu Metropolis [Citation44]. The two districts have, each, a DHB, four LHAs, a general hospital and a network of cottage hospitals and primary health facilities. Many health facilities have health facility committees (HFCs) allowing for community involvement in health facility management.
Research design
This study adopted a qualitative, case study design because experiences with implementation of the FMCHP are embedded in the context that formed the focus of inquiry [Citation47,Citation48]. The case is the FMCHP of Enugu State in South-east Nigeria. Two districts were selected as embedded case study sites. The phenomenon of inquiry is the implementation of the programme.
Study population and sampling strategy
We categorised the seven health districts into two groups of three well-performing and four less-well-performing districts using provider payment data over five years (2009–2014), which ranged from 2% to 26% with a median of 14% serving as the cut-off point [Citation46,Citation49]. We used provider payment data for the categorisation, because the health information management system does not disaggregate maternal and child health utilisation by user fee and fee-exempt. Enugu Metropolis and Isi-Uzo districts were each randomly selected from the well-performing and less-well-performing districts. The districts were selected to maximise the diversity of implementation experiences and understand how contextual and institutional factors influenced the capacity of health facilities to offer free MCH services in two contrasting settings. We purposively selected policymakers (n = 16), health care providers (n = 16) and health facility committees (HFC) leaders (n = 12) because of their positions, involvement in FMCHP implementation and willingness to participate in the study. In each district, healthcare providers were selected from the district hospital, the busiest cottage hospital and six primary health centres that have active HFCs. Key public officials at state and district levels were used as gatekeepers to identify participants.
Data collection methods
A semi-structured, in-depth interview guide, developed based on conceptual framework of this study, validated by two experts and adapted following analysis of pilot interviews, was used to conduct interviews. In total, 44 people were interviewed between February and September 2015 () using the same interview guide. The guide explored how decentralisation, monitoring and supervision, citizen participation, concurrent policies, provider payment procedures, and resource availability in health facilities affected implementation of FMCHP (Appendix 1). Appointments were sought by cell phone or personal visits. Participants were interviewed in their offices or health facilities. Interviews, which lasted about 60–90 min, were conducted in English, audiotaped, transcribed verbatim and transcripts sent back to participants to confirm the credibility of the transcripts [Citation50].
Table 1. Socio-demographic profile of the participants.
Additional data were collected through document review. Thirteen documents, relevant to the research questions, were identified in consultation with key government officials (Appendix 2). The documents reviewed included policy documents, programme reports and memoranda on FMCHP.
Data analysis
Data were analysed using a framework approach which involved coding the data, mapping and organising data under common themes, and interpretation [Citation51]. NVivo 11 software was used for coding and categorising the data. Codes were developed from the conceptual framework and reading the data. Coding was done by two persons guided by a coding framework, which enhanced validity and reliability of this study [Citation52]. Data analysis was piloted with six transcripts and all differences in coding were reconciled before full data analysis. The findings from different sources were compared for patterns of convergence and divergence. Furthermore, the findings of this study were discussed with study participants and key health systems stakeholders in a validation meeting.
Ethical considerations
The Health Research Ethics Committee of the University of Nigeria Teaching Hospital Enugu, Nigeria, approved this study. All participants provided written informed consent.
Results
Five themes emerged from the study, namely action environment (three sub-themes), institutional context of public providers (three sub-themes), task network (two sub-themes), organisation (four sub-themes) and human resources (three sub-themes). Each sub-theme is further divided into two categories (enabling factor and constraints) as shown in .
Table 2. Factors influencing capacity of health facilities to provide free maternal and child health services in Enugu State, Nigeria.
Action environment of providers
Decentralisation, supervision and accountability emerged as key themes in the action environment.
Decentralisation
Despite the existence of district health system (DHS) policy, most policymakers and providers identified dysfunctional District Health Boards (DHBs) and District FMCHP Committees as constraints to providers’ capacity to offer free health care. Meetings of DHBs were rarely held. Quarterly review meetings that provided opportunities for review of FMCHP implementation were no longer held since 2012 due to irregular funding (DR7, DR10). A few policymakers and providers observed that Local Government monitoring and evaluation officers by-pass the district information office in data transmission from health facilities to the MOH. Most HFC leaders do not know about the DHBs’ activities, nor the existence of the District FMCHP Committee.
Supervision
Most policymakers and providers mentioned that supervision is supportive and offers opportunity for on-the-job capacity building, but it is irregular. In Isi-Uzo, all HFC leaders revealed that supervision by government officials is poor. ‘One hardly sees supervisors from the local government. The occasional supervisors we see are those of SURE-P and PATHS2 (development partners)’ (HFC leader 4). Some HFC leaders in Enugu Metropolis mentioned that providers receive routine quarterly supervision. Conversely, some HFC leaders in Enugu Metropolis stated that ‘they (supervisors) do not even visit most of the health centres that are within accessible areas’ (HFC leader 11). Though vehicles were provided to districts to enhance supervision, the districts lack operating funds to conduct regular supervision (DR10).
Accountability
All categories of participants identified HFCs as the only functioning social accountability initiative in health facilities. HFCs effectively oversee the Drug Revolving Fund (DRF) and staff attendance. ‘We have been monitoring health workers. Their salaries were not paid until we endorsed their time book’ (HFC leader 6). HFCs are not involved in identifying eligible users of free care and managing free care refunds (DR9). HFCs lack the legislative framework for effective and efficient discharge of their functions (DR2). Some policymakers and HFC leaders noted that HFC Alliances exist but are ineffective. Most policymakers, providers and HFC leaders corroborated the findings that health facilities lacked service charters and complaint boxes (DR4, DR5). A few policymakers and providers observed that complaint boxes and service charters may not be useful because ‘people know their right…they are ready to bare their mind any time anywhere, even if it hurts you’ (Provider 8).
Institutional context of providers
Reimbursement standard, concurrent policies and poor remuneration emerged as key themes related to the institutional context of providers.
Reimbursement standard
Reimbursement was often delayed, health facilities were sometimes paid fractions of their claims, and health workers did not seem to understand the reimbursement procedure (DR2, DR3). Most policymakers and providers indicated that reimbursement of health facilities was poorly enforced in both districts. Many health facilities were not paid for over a year resulting in stoppage of free maternal and child health services in Isi-Uzo. In Enugu Metropolis, delayed reimbursement was compounded by under-payment of providers which resulted in interrupted free maternal and child health services. Delayed provider payment resulted in stock-outs and resumption of user fees (DR2, DR5, DR7, DR10, DR11, DR12). In both districts, most HFC leaders were not aware of the reimbursement process but a few HFC leaders corroborated policymakers’ and providers’ views that many providers no longer submitted claims for reimbursement.
“Ooh! There was a time the fund ceased for almost a year or two years…. the officers-in-charge lost hope, almost all of them lost hope. I do not even think that most providers are submitting their invoices now from this district” (Policymaker 14).
Concurrent policies
Evidence of tax payment was introduced as a proof of residence in the state but resulted in under-utilisation of free services (DR1, DR2). Most district-level policymakers and providers incorrectly interpreted evidence of tax payment as tax clearance or a salary slip of a ‘civil servant’ husband, payment of some money in lieu of tax clearance or Gen 35 (evidence of appointment) for civil servants. The evidence of tax payment policy was never implemented in Isi-Uzo but partially implemented in Enugu Metropolis. Most HFC leaders in both districts were not aware that evidence of tax payment was implemented in their facilities. Few HFC leaders observed that, other than civil servants, clients pay some money in lieu of tax in Enugu Metropolis.
Most providers and HFC leaders in Isi-Uzo stated that Subsidy Reinvestment Programme (SURE-P), a federal government scheme, provided an alternative to the failing state-owned FMCHP. ‘Many patients now prefer going to SURE-P centre for treatment and delivery, where they did not have to pay out-of-pocket. Since then we rarely had patients here’ (Provider 8). The SURE-P supported health facilities with free drugs, delivery kits, equipment, health workers and infrastructure. However, few HFC leaders noted that the health workers ‘came only when we had the SURE-P intervention’ (HFC leader 4).
Poor remuneration in the public sector
Participants of all categories indicated that non-implementation of nationally approved health salary scales, discriminatory compensation for different cadres of health workers and unpaid salaries undermine staff motivation to implement FMCHP:
“Though doctors were paid with approved salary scale, other health workers were not. It is not possible that other health workers will wholeheartedly run the free maternal and child healthcare programme per guidelines” (Provider 11).
Task network of providers
Submission of claims and communication of service entitlements and obligations emerged as two main tasks of providers (). Most policymakers and providers stated that providers stopped submitting claims for reimbursement in Isi-Uzo, whereas providers in Enugu Metropolis delayed in submitting providers’ claims. Providers are not able to appropriately fill the claim forms and this was corroborated by document review (DR2, DR12). Few policymakers and most providers indicated that providers lacked support from district-level officials in preparation and submission of provider claims. ‘Our Local Health Authority does not support us very well. One will suffer, suffer and suffer before they sign claim form for one’ (Provider 2). The policymakers and providers stated that district-level officials withdrew from monitoring health facilities when health facilities were paid directly instead of through the district structures
Most HFC leaders in both districts said that they were not involved in claims preparation and submission. Only one HFC leader in Enugu Metropolis was aware of the reimbursement procedure. The HFC leader noted that providers were unable to correctly fill claims forms, and sometimes inflated their claims. Moreover, most policymakers, providers and HFC leaders agreed that providers do not sufficiently communicate service entitlements and obligations to users, which resulted in low awareness of the requirement for evidence of tax payment among users.
Organisational factors
Facility funding, health management information system, drugs, equipment, infrastructure and communication shaped provider capacity.
Facility funding
The FMCHP policy stipulates that 70% of health facilities’ claim for free services should be paid to the health facilities as operating cost (DR1). However, health facilities had poor access to the funds paid through the LHAs prior to 2010 when payment policy changed to direct facility funding (DR4, DR7, DR8). Most policymakers stated that the operating costs are paid directly to health facilities due to leakages at the LHAs. In Isi-Uzo, most district policymakers and providers observed that ‘health facilities no longer receive overhead from FMCHP due to cessation of reimbursement’ (Policymaker 14) and providers relied on funds from non-free services retained. One provider observed that ‘there was a time, health facilities received overhead, which was not regular, though. Within the preceding two years, I don’t think that there is anything like overhead for us’ (Provider 3). In Enugu Metropolis, most policymakers and providers indicated health facilities received insufficient reimbursements. The majority of HFC leaders in both districts indicated that they were signatories to health facilities’ account, but providers were unwilling to involve them in financial management.
Health management information system (HMIS)
The capacity of providers to record and report data is low (DR3). However, most policymakers and providers in both districts indicated that use of mobile phones facilitated data transmission to the State HMIS office. Few policymakers and providers in both districts observed that data collection and transmission are poorly funded. ‘It was agreed that M&E officer should be given N10,000 every month, but it has not been implemented’ (Policymaker 13). Most providers in both districts also stated that inadequate staffing and absence of data review meetings constrained providers’ capacity to report and use data for planning. Most HFC leaders stated that HFCs are not involved in data collection and reporting. Few HFC leaders noted that charts of maternal and child healthcare attendance are discussed in their HFC meetings.
Drugs, equipment and infrastructure
Existence of the drug revolving fund (DRF) scheme and procurement of drugs from the central medical stores enabled health facilities to offer free MCH services (DR2). Nonetheless, delayed payment of health facilities resulted in stock-outs (DR2, DR5, DR7, DR10, DR12). Most policymakers, providers and HFC leaders observed that providers’ DRF stocks were depleted due to delayed – or non-reimbursement of – FMCHP drug expenditure. Most policymakers and providers noted that many providers were supplied drugs beyond their level of care and drugs close to expiry. In both districts, most policymakers and few HFC leaders revealed that health workers dispensed private drugs in public health institutions. ‘The woman (provider) has resorted to buying drugs with her own money and selling them to those who come to the facility’ (HFC leader 4).
Most policymakers, providers and HFC leaders in both districts also stated that providers have equipment but lacked buildings to house equipment and support service delivery. Equipment were not always tailored to the scope of health facilities and staff received no training on how to operate and maintain them (DR2, DR3). Furthermore, in Isi-Uzo, few providers and HFC leaders highlighted the absence of a functional ambulance to support referral services. Even though ambulances were allocated to the district hospitals or the apex hospital in each local government (DR1), ambulances are usually used for other purposes and out of reach of the health facilities (DR3, DR10). In Enugu Metropolis, providers indicated that an insecure working environment led to incidence of thefts and sexual harassment of health workers on night shift. Many health facilities have dilapidated buildings, no perimeter fencing, poor electricity supply and poor water supply (DR2, DR3, DR5).
Providers-clients’ trust and communication
Despite policy stipulation that users be educated on service entitlements and obligations in FMCHP (DR1), users’ lack of confidence in public health facilities limit use of free services (DR13). Whereas some policymakers and providers claimed that providers ‘delivered services in a professional manner’ (Policymaker 15), other policymakers and providers said that users complain about poor attitudes of healthcare providers. ‘Last time, I met a woman who said that she would never go for free MCH services because if one went to the health centre, providers would be insulting one’ (Provider 10). Most HFC leaders in Isi-Uzo stated that providers were not courteous and responsive to clients’ expectations; and are not available for afternoon and night shifts. Conversely, most HFC leaders in Enugu Metropolis said that providers were approachable and treated clients with respect.
Human resources
Availability, posting and transfer, and weak disciplinary mechanisms emerged as sub-themes in human resources.
Availability of health workers
Health facilities lack the appropriate number and mix of human resources (DR2, DR3, DR6). Most policymakers and providers indicated that lack of qualified health workers hampered delivery of free maternal and healthcare services. ‘We cried out bitterly that trained health workers in the system were too small to carry out this laudable programme.’ (Policymaker 16). Some providers and few HFC leaders observed that SURE-P improved availability of staff in Isi-Uzo.
Posting and transfer
Participants of all categories supported the findings from document review that distribution of health workers was skewed in favour of urban districts (DR2, DR3, DR6). A few providers in Isi-Uzo observed that health workers were posted to health posts leaving busier health centres. In Enugu Metropolis, few providers stated that ‘some doctors were posted to less busy hospitals avoiding busier hospitals’ (Provider 12).
Weak disciplinary mechanisms
Most policymakers stated that district officials do not sanction primary health staff and heads of facilities are reluctant to implement staff disciplinary procedures because ‘higher authorities’ (Policymaker 11) do not act on their recommendations. Also, whereas the Local Government Service Commission (LGSC) is responsible for managing health workers, the district officials have only technical oversight of primary healthcare service delivery. In both districts, most providers and HFC leaders explained that heads of health facilities do not comply with staff disciplinary procedures because ‘heads of facilities do not want to be marked as the ones responsible for the ordeal of their co-workers’ (Provider 7) and due to political interference. ‘Most staff, who are truant, are people that you are unable to discipline. When you query them, a higher authority will query you’ (Provider 15). Most HFC leaders stated that ‘no head of facility has actually queried or reported staff for insubordination’ (HFC Leader, 4).
Discussion
This study has explored how the context and institutional capacity of health facilities affect implementation of the FMCHP. Evidence from this in-depth analysis could inform design of an improved governance model for strengthening the capacity of health facilities offering free maternal and child healthcare.
The study findings reveal that while decentralisation policy promoted integrated supportive supervision and monitoring of FMCHP in principle, ineffectual district FMCHP leadership resulted in poor provider performance monitoring, lack of support to frontline health workers and weak disciplinary mechanisms. These findings are consistent with results from previous studies [Citation10,Citation16–Citation20]. Decentralisation should encourage more use of local decision-making and building uniform institutional capacities across health districts through effective devolution of functions, power and resources to district-level FMCHP committees. In practice, organisational culture of public service bureaucracy constrained the constitution of district-level FMCHP committees, posting and transfer, staff disciplinary mechanisms and payment of salaries through the DHBs. There is a need to reinforce district FMCHP leadership and improve accountability between district-level officials and service providers through clarity of roles and responsibilities, clear rules and procedures, provider performance monitoring and need-based resource allocation [Citation16].
The study’s findings show that though citizen participation in management of health facilities implementing FMCHP enabled oversight of the drug revolving fund and staff attendance at work, HFCs did not play strong roles in FMCHP. Our findings are consistent with low citizen participation found in other studies [Citation9,Citation22–Citation24]. In contrast, in Nepal, Burkina Faso and Kenya, HFCs were actively involved in free care schemes including financial management [Citation10–Citation12]. The HFCs in this study could have played stronger roles to facilitate registration of beneficiaries with primary providers in their locality, endorse provider claims and ensure that rules for spending funds reimbursed to health facilities for free care were strictly adhered to. HFCs could have also established complaint boxes, displayed service charters and created awareness about usefulness of service charters in holding providers accountable. These gaps in the roles of HFCs provide insights into the potential of citizen participation for the improvement of free health services as has been argued in a previous study [Citation49]. It would be imperative to train and mentor HFCs and health care providers on the mandate of HFCs within the FMCHP policy to ensure that health facilities implement changes to the free care programme based on concerns raised by citizens [Citation53].
The study findings highlight the importance of providers’ use of discretion in modifying free healthcare policy and make services unresponsive [Citation54]. First, providers need to be paid at defined times. The findings indicate, as in several studies, that delayed reimbursement is a key implementation constraint [Citation12,Citation21,Citation25]. Regular and timely reimbursement of providers could reduce chances that providers may ration free services, resume charging of user fees or impose informal payments on users. Secondly, decision makers should avoid conflictive policies that produce a contradictory incentive environment for FMCHP implementation. The study findings indicate that providers used their discretion to interpret evidence of tax payment policy, which is inconsistent with intentions of the policy but influenced how they communicated the policy to consumers. Elsewhere, health workers have employed similar discretionary power to make changes to free healthcare policies during implementation [Citation21,Citation25]. Conversely, consumers in this study exploited information asymmetry, evaded evidence of tax payment policy, and used SURE-P providers, which offered alternative fee-exempt maternal and child health services in some districts.
Poor remuneration in the state public health sector created a weak incentive environment for providers of free care. This finding is consistent with findings in Nigeria [Citation24,Citation35], but is in contrast with evidence from Sierra Leone [Citation15]. Despite increased workload due to the free care policy, remuneration of health workers in Enugu State is at variance with nationally approved health salary scales for different cadres of health workers. This disparity in compensation, coupled with delayed payment of salaries of primary healthcare workers, is the most potent driver of poor motivation and exit of qualified health workers from Enugu’s health sector. Strategies to motivate and retain providers must take cognisance of public sector remuneration system as exemplified in Sierra Leone’s free health care initiative where salary uplift ensured that providers were adequately paid and motivated to manage increased workload without imposing informal charges on users [Citation15].
The findings further suggest that any provider performance monitoring system that excludes district and local health authority officials is structured to fail. Even though tools for FMCHP claims were available, the preparation of claim documents was problematic at the health facility level as is the case in Burkina Faso and Burundi [Citation10,Citation25]. In this study, the withdrawal of district-level officials from monitoring provider performance including reporting of claims is the singular most critical gap in the task network of providers; and is consistent with evidence from Burkina Faso, where lack support from district officials limited health workers’ recording and reporting [Citation10]. District-level officials withdrew from provider monitoring and supervision due to allegations of misappropriation of funds against them, unfavourable changes in reimbursement process and unpaid share of service charge. Consequently, providers lost the opportunity for on-the-job capacity building on and support for preparation and submission of claims.
The study findings highlight a requirement for resource allocation to providers to be need-based. The policy of remitting 70% of FMCHP service refunds directly to health facilities while potentially effective in principle, was unpredictable in practice. Also, equipment donated by development partners enabled health facilities to offer free services. However, buildings are dilapidated, health facilities lack public utilities and functional ambulances to support referrals, equipment is stacked and not tailored to the scope of services provided by facilities, which are consistent with findings of several studies [Citation18,Citation24,Citation36]. Equally, the study found that donation of seed stock for the drug revolving fund and subsequent procurement through the central medical stores improved availability of quality-assured drugs in health facilities. However, some drugs donated by development partners failed to match the needs of health facilities. Some needed drugs were either expiring or not available due to delayed reimbursement, untimely replenishment of stocks and providers’ lack of funding for transport to collect drugs from the central medical store. These findings, which are consistent with evidence from several studies, partly explains health workers’ poor adherence to the free care policy and increased involvement in parallel drug supply systems [Citation12,Citation17,Citation26–Citation31].
Furthermore, the study findings indicate the need to fill gaps in staffing to meet service entitlements through recruitment and retention of appropriate cadres and mission-consistent postings and transfers especially in rural health facilities. Similarly, shortage of appropriate qualified health workers, worse in remote areas, constrained provision of maternal, neonatal and child health services in the Lao People’s Democratic Republic and three African countries, where health workers had preference for urban posts [Citation19,Citation36]. Though presence of SURE-P staff improved the availability of health workers, postings and transfers of health workers to less busy or urban health facilities limit responsiveness of health facilities and contribute to declining quality of care. It seems that health workers in the study setting choose less busy health facilities to enable them to cope with parallel engagements in the private sector and unauthorized continuing professional education.
Despite the existence of sanction procedures and HFCs’ monitoring of staff attendance, which could reduce rate of absenteeism among health workers, heads of health facilities are reluctant to invoke staff disciplinary measures because state-level officials do not act on recommendations of district officials, for fear of political interference in staff disciplinary processes and for sense of comradeship, similar to weak mechanisms of answerability and enforceability found in Zambia [Citation20]. Contrastingly, Sierra Leone has shown that absenteeism could reduce drastically when a staff sanction framework is implemented within the context of a free health care initiative [Citation15]. Improving human resource capacity will require a combination of performance-based funding to ensure that health workers are adequately motivated and enforcing sanction framework for holding providers accountable for delivery of quality services and adherence to guidelines and reporting timelines, and sanctions imposed, if specified outputs and outcomes are not delivered [Citation15,Citation55].
The use of case study design in this study enhanced identification of how provider factors can mediate implementation of the FMCHP. However, while sampling participants was informed by anticipated richness and relevance of information in relation to the study questions [Citation48], the views expressed by these participants may not be generalizable to other actors. Although the study was limited to two districts, use of qualitative pilots, member check, coding framework, validation meeting, triangulation of findings from multiple sources and the full descriptions of participants’ narratives have been helpful in providing evidence that is trustworthy, relevant and has utility for decision-making.
Conclusions
This study contributes to the scholarship and policy debate on implementation of user fee policies through its detailed analysis of Nigeria’s implementation experiences. Key lessons that should strengthen the capacity of health facilities to implement free healthcare policies include: ensure effective devolution of functions, powers and resources to district-level organisations; strengthen facility-based social accountability initiatives; harmonize concurrent and conflictive policies; ensure adequate and fair compensation of health workers, and timely reimbursement of providers; fill service delivery gaps in health facilities; and attract and retain appropriate mix of human resources. Overall, decision makers must pay attention to institutional designs and organisational practices shaping implementation of user fee removal policy at the facility level.
Ethics and consent
The study was approved by Health Research Ethics Committee of University of Nigeria Teaching Hospital Enugu, Nigeria. All participants provided written informed consent.
Paper context
Studies examining how capacity of health facilities affect implementation of free healthcare policies in low-resource settings are limited. This study describes how context and institutional factors affect the capacity of health facilities to implement a free maternal and child healthcare programme in Nigeria. Attention to decentralisation, citizen participation, concurrent policies, task network, organisation of service delivery and human resources will enhance the institutional capacity of health facilities to offer free health care.
Acknowledgments
We are grateful to all participants of this study and Prof Nkoli Ezuma for assisting with tool development and data analysis.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
Notes on contributors
Daniel C. Ogbuabor
DCO and OEO contributed to conceptualisation of the study. DCO conducted the field work. DCO and OEO analysed the data. All authors contributed to conceptualisation of the manuscript. DCO drafted the manuscript. All authors contributed to the intellectual content of the article. DCO finalised the article. All authors read and approved the final manuscript.
References
- Lagomarsino G, Garabrant A, Adyas A, et al. Moving towards universal health coverage: health insurance reforms in nine developing countries in Africa and Asia. Lancet. 2012;380:933–13.
- Yaogo M. Free versus subsidised healthcare: options for fee exemptions, access to care for vulnerable groups and effects on the health system in Burkina Faso. Health Res Policy Syst. 2017;15:58.
- Ridde V, de Sardan J-PO, Brouillet P, et al. Abolishing user fees for patients in West Africa: lessons for public policy. Paris (France): AFD, Agence française de développement; 2013.
- Ahmed SM, Rawal LB, Chowdhury SA, et al. Cross-country analysis of strategies for achieving progress towards global goals for women’s and children’s health. Bull World Health Organ. 2016;94:351–361.
- Okonofua F, Lambo E, Okeibunor J, et al. Advocacy for free maternal and child health care in Nigeria–results and outcomes. Health Policy. 2011;99:131–138.
- Kana MA, Doctor HV, Peleteiro B, et al. Maternal and child health interventions in Nigeria: a systematic review of published studies from 1990 to 2014. BMC Public Health. 2015;15:334.
- Grindle MS. Good enough governance revisited. Dev Policy Rev. 2011;29:s199–s221.
- Grindle MS, Hilderbrand ME. Building sustainable capacity in the public sector: what can be done? Public Admin Develop. 1995;15:441–463.
- Atela M, Bakibinga P, Ettarh R, et al. Strengthening health system governance using health facility service charters: a mixed methods assessment of community experiences and perceptions in a district in Kenya. BMC Health Serv Res. 2015;15:539.
- Belaid L, Ridde V. An implementation evaluation of a policy aiming to improve financial access to maternal health care in Djibo district, Burkina Faso. BMC Pregnancy Childbirth. 2012;12:143.
- Opwora A, Kabare M, Molyneux S, et al. Direct facility funding as a response to user fee reduction: implementation and perceived impact among Kenyan health centres and dispensaries. Health Policy Plann. 2010;25:406–418.
- Sato M, Gilson L. Exploring health facilities’ experiences in implementing the free health-care policy (FHCP) in Nepal: how did organizational factors influence the implementation of the user-fee abolition policy? Health Policy Plann. 2015;30:1272–1288.
- Witter S, Khadka S, Nath H, et al. The national free delivery policy in Nepal: early evidence of its effects on health facilities. Health Policy Plann. 2011;26:ii84–91.
- Abuya T, Njuki R, Warren CE, et al. A policy analysis of the implementation of a Reproductive Health Vouchers Program in Kenya. BMC Public Health. 2012;12:540.
- Witter S, Wurie H, Bertone MP. The free health care initiative: how has it affected health workers in Sierra Leone? Health Policy Plann. 2016;31:1–9.
- Khim K, Annear PL. Strengthening district health service management and delivery through internal contracting: lessons from pilot projects in Cambodia. Soc Sci Med. 2013;96:241–249.
- Lang’at E, Mwanri L. Healthcare service providers’ and facility administrators’ perspectives of the free maternal healthcare services policy in Malindi District, Kenya: a qualitative study. Reprod Health. 2015;12:59.
- Mkoka DA, Mahiti GR, Kiwara A, et al. “Once the government employs you, it forgets you”: health workers’ and managers’ perspectives on factors influencing working conditions for provision of maternal health care services in a rural district of Tanzania. Hum Resour Health. 2015;13:77.
- Prytherch H, Kagone M, Aninanya GA, et al. Motivation and incentives of rural maternal and neonatal health care providers: a comparison of qualitative findings from Burkina Faso, Ghana and Tanzania. BMC Health Serv Res. 2013;13:149.
- Topp SM, Chipukuma JM, Hanefeld J. Understanding the dynamic interactions driving Zambian health centre performance: a case-based health systems analysis. Health Policy Plann. 2015;30:485–499.
- Agyepong IA, Nagai RA. “We charge them; otherwise we cannot run the hospital” front line workers, clients and health financing policy implementation gaps in Ghana. Health Policy. 2011;99:226–233.
- Mafuta EM, Dieleman MA, Hogema LM, et al. Social accountability for maternal health services in Muanda and Bolenge Health Zones, Democratic Republic of Congo: a situation analysis. BMC Health Serv Res. 2015;15:514.
- McMahon SA, George AS, Chebet JJ, et al. Experiences of and responses to disrespectful maternity care and abuse during childbirth; a qualitative study with women and men in Morogoro Region, Tanzania. BMC Pregnancy Childbirth. 2014;14:268.
- Onwujekwe O, Obi F, Uzochukwu B. Assessment of the NHIS-MDG free maternal and child health program and the prospects of reactivation/scale-up using the basic health care provision fund in Nigeria. Enugu (Nigeria): Health Policy Research Group, University of Nigeria; Sept 2016. (Research Summary 7).
- Nimpagaritse M, Bertone MP. The sudden removal of user fees: the perspective of a frontline manager in Burundi. Health Policy Plann. 2011;26:ii63–ii71.
- Mkoka DA, Goicolea I, Kiwara A, et al. Availability of drugs and medical supplies for emergency obstetric care: experience of health facility managers in a rural District of Tanzania. BMC Pregnancy Childbirth. 2014;14:108.
- Topp SM, Chipukuma JM. A qualitative study of the role of workplace and interpersonal trust in shaping service quality and responsiveness in Zambian primary health centres. Health Policy Plann. 2016;31:192–204.
- Chuma J, Musimbi J, Okungu V, et al. Reducing user fees for primary health care in Kenya: policy on paper or policy in practice? Int J Equity Health. 2009;8:15.
- Ameur AB, Ridde V, Bado AR, et al. User fee exemptions and excessive household spending for normal delivery in Burkina Faso: the need for careful implementation. BMC Health Serv Res. 2012;12:412.
- Fafchamps M, Minten B. Public service provision, user fees and political turmoil. J Afr Econ. 2007;16:485–518.
- Nabyonga-Orem J, Karamagi H, Atuyambe L, et al. Maintaining quality of health services after abolition of user fees: a Uganda case study. BMC Health Serv Res. 2008;8:102.
- Campbell J, Oulton JA, McPake B, et al. Increasing access to ‘free’ health services: are health workers not a missing link? Int J Clin Pract. 2011;65:12–15.
- Ridde V, Diarra A. A process evaluation of user fee abolition for pregnant women and children under five years in two districts in Niger (West Africa). BMC Health Serv Res. 2009;9.
- Ganle JK, Parker M, Fitzpatrick R, et al. A qualitative study of health systems barrier to accessibility and utilization of maternal and newborn healthcare services in Ghana after user fee abolition. BMC Pregnancy Childbirth. 2014;14:1.
- Galadanci HS, Idris SA, Sadauki HM, et al. Programs and policies for reducing maternal mortality in Kano State, Nigeria: a review. Afr J Reprod Health. 2010;14:31–36.
- Sychareun V, Phommachanh S, Soysouvanh S, et al. Provider perspectives on constraints in providing maternal, neonatal and child health services in the Lao People’s democratic republic: a qualitative study. BMC Pregnancy Childbirth. 2013;13:243.
- Cheelo C, Chama C, Pollen G, et al. Do user fee revenues matter: assessing the influences of removal of user fees on health financial resources in Zambia. Lusaka (Zambia): Department of Economics, The University of Zambia; Feb 2010.
- State Ministry of Health [SMOH]. The guidelines for implementation of free maternal and under-5 child health programme. Enugu (Nigeria): Enugu State Ministry of Health; 2013.
- Ekwueme OC. Health consumer’s perception on increasing primary health care services utilization and quality enhancement at the primary health centres in Enugu, Enugu State, Nigeria. Open Access Sci Rep [Internet]. 2012;1(11):530.
- Nwala KE, Ebunoha GN, Ugwu UC. Consumer knowledge and availability of maternal and child health services: a challenge for achieving MDG 4 and 5 in Southeast Nigeria. BMC Health Serv Res. 2013;13:53.
- Onwujekwe O, Hanson K, Uzochukwu B. Are the poor differentially benefiting from provision of priority public health services? A benefit incidence analysis in Nigeria. Int J Equity Health. 2012;11:70.
- Uzochukwu B, Okwuosa C, Ezeoke O, et al. Free maternal and child healt services in Enugu State, South-east, Nigeria: experiences of the community and health care providers. Int J Med Health Sci Res. 2015;2:158–170.
- Ezugwu EC, Agu PC, Nwoke MO, et al. Reducing maternal deaths in a low resource setting in Nigeria. Niger J Clin Pract. 2014;17:62–66.
- National Population Commission [NPC]. Nigeria 2013 demographic and health survey. Abuja (Nigeria): National Population Commission; 2014.
- Hilderbrand ME, Grindle MS. Building sustainable capacity in the public sector: what can be done? In: Grindle MS, editor. Getting good government: capacity building in the public sectors of developing countries. Havard: Havard University Press; 1997; p. 30-61.
- Ogbuabor D. Achieving universal health coverage: governance analysis of the free maternal and child healthcare programme in Enugu State, South-east Nigeria [PhD Thesis]. Department of Health Administration and Management, University of Nigeria Nsukka; 2017.
- Gilson L. Health policy and systems research: A methodological reader. Geneva (Switzerland): Alliance for Health Policy and Systems Research, World Health Organization; 2012.
- Yin RK. Qualitative research from start to finish. New York (NY): Guilford Press; 2011.
- Ogbuabor DC, Onwujekwe OE. The community is just a small circle: citizen participation in the free maternal and child healthcare programme of Enugu State, Nigeria. Glob Health Action. 2018;11:1421002.
- Mero-Jaffe I. ‘Is that what I said?’ Interview transcript approval by participants: an aspect of ethics in qualitative research. Int J Qual Methodol. 2011;10:231–247.
- Gale NK, Heath G, Cameron E, et al. Using the framework method for the analysis of qualitative data in multidisciplinary health research. BMC Med Res Methodol. 2013;13:117.
- Gibbert M, Ruigrok W, Wicki B. What passes as a rigorous case study? Strategic Manage J. 2008;29:1465–1474.
- Lodenstein E, Dieleman M, Gerretsen B, et al. Health provider responsiveness to social accountability initiatives in low- and middle-income countries: a realist review. Health Policy Plann. 2017;32:125–140.
- Gilson L, Elloker S, Olckers P, et al. Advancing the application of systems thinking in health: South African examples of a leadership of sensemaking for primary health care. Health Res Policy Syst. 2014;12:30.
- Lewis M, Pettersson G. Governance in health care delivery: raising performance. Washington (DC): World Bank; 2009. (Report No.: 5074).
Appendix 1.
In-Depth Interview Guide
Appendix 2.
List of documents Reviewed
Enugu state 2013 guidelines for implementation of free maternal and u-5 child health programme. (DR1).
PATHS2 consultancy report on revision of FMCH policy and implementation guidelines in Enugu State. (DR2).
Enugu state 2013 policy on free maternal and child health services in Enugu State. (DR3).
Development of facility health committees to strengthen voice and accountability in Enugu State. PATHS2 Strategy Report. (DR4)
PATHS2 report of rapid assessment of 76 health facilities in six local government areas for implementation of essential systems and service packages. (DR5).
Annual performance review of Enugu state health sector. (DR6).
Implementation of the Enugu State free maternal and child healthcare programme: the concept, operations, challenges and prospects. Memo by former permanent secretary SMOH to Enugu State House Committee on Health (DR7).
Memo on FMCHP by Executive Secretary, Enugu State Planning Commission to Enugu State House Committee on Health (DR8).
Memo on FMCHP implementation by Facility Health Committees’ Alliance to Enugu State House Committee on Health (DR9).
FMCHP: Prospects, challenges and recommendations. Memo by the Chief Executive Officers of District Health Boards to Enugu State House Committee on Health (DR10).
Enugu State free maternal and child healthcare programme: overview, considerations and recommendations for improvement. Memo by State Health Board to Enugu State House Committee on Health (DR11).
An in-depth enquiry into state and local government contribution to FMCHP fund management and re-imbursement of health facilities. Memo by Local Government Service Commission to Enugu State House Committee on Health (DR12).
Enugu State free maternal and child healthcare programme implementation committee report, 2008. (DR13).